Abstract
To quantify the pooled rate and risk ratio of seroconversion following the uncomplete, complete, or booster dose of COVID-19 vaccines in patients living with HIV. PubMed, Embase and Cochrane library were searched for eligible studies to perform a systematic review and meta-analysis based on PRIMSA guidelines. The pooled rate and risk ratio of seroconversion were assessed using the Freeman-Tukey double arcsine method and Mantel–Haenszel approach, respectively. Random-effects model was preferentially used as the primary approach to pool results across studies. A total of 50 studies involving 7160 patients living with HIV were analyzed. We demonstrated that only 75.0% (56.4% to 89.9%) patients living with HIV achieved a seroconversion after uncomplete vaccination, which improved to 89.3% (84.2% to 93.5%) after complete vaccination, and 98.4% (94.8% to 100%) after booster vaccination. The seroconversion rates were significantly lower compared to controls at all the stages, while the risk ratios for uncomplete, complete, and booster vaccination were 0.87 (0.77 to 0.99), 0.95 (0.92 to 0.98), and 0.97 (0.94 to 0.99), respectively. We concluded that vaccine doses were associated with consistently improved rates and risk ratios of seroconversion in patients living with HIV, highlighting the significance of booster vaccination for patients living with HIV.
Similar content being viewed by others
Introduction
Patients living with HIV are at high risk for severe coronavirus disease 2019 (COVID-19), with higher rates of hospitalization and mortality due to immunosuppression, other comorbidities, or social determinants of health1,2,3,4. COVID-19 vaccines have been found to be the main measure of reducing the severity and mortality of COVID-19 patients in clinical trials and real-world populations5,6,7,8. Therefore, patients living with HIV were an early priority group for vaccine eligibility. However, the fact that patients living with HIV have a reduced serological response to multiple vaccines, such as hepatitis B and seasonal influenza vaccines, compared to HIV-negative individuals has raised concerns about the efficacy of COVID-19 vaccination for patients living with HIV9,10.
A growing number of studies have reported serological responses between HIV-infected and non-HIV-infected patients. However, the conclusions were not consistent. For example, Madhi et al. showed that patients living with HIV achieved similar immunogenicity compared to healthy controls after uncomplete, and complete COVID-19 vaccine11. Bergman et al. demonstrated that SARS-CoV-2-naive patients living with HIV had attenuated humoral immune responses to COVID-19 vaccine compared with HIV-negative vaccine counterparts12. A meta-analysis has been performed to compare the serological response between HIV-infected and non-HIV-infected patients after a second dose of COVID-19 vaccine, but the analyses on uncompleted and booster doses of COVID-19 vaccine, as well as the exact seroconversion rate in patients living with HIV, were not further evaluated13. To a large extent, there is a sparsity of evidence on the serological response following COVID-19 vaccines in patients living with HIV.
Therefore, it is necessary to perform a meta-analysis of available evidence to quantify the pooled rate and risk ratio of seroconversion following the uncomplete, complete, or booster dose of COVID-19 vaccines in patients living with HIV.
Methods
Search strategy
This systematic review and meta-analysis was based on the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRIMSA) guidelines14 and was registered on PROSPERO with the registration number CRD42022359603. PubMed, Embase and Cochrane Library databases were searched from inception to 13th, September 2022 using the following terms: “COVID-19” OR “SARS-Cov-2” AND “vaccines” AND “HIV”. The full details of search strategies were provided in Supplementary Table S1.
Inclusion and exclusion criteria
Study selection was conducted in three steps: removing the initial de-duplication, screening titles and abstracts, and reviewing the full text for eligible articles. Two researchers (Q.Z and F.Z.) independently evaluated eligibility, and discrepancies were solved by a third investigator (G.D.). Studies were included for analysis if they are cohort studies or randomized controlled trials that reported the seroconversion rate following the uncomplete, complete, or booster dose of COVID-19 vaccines in patients living with HIV; or provided risk ratios (RRs) for seroconversion and antibody titers following the uncomplete, complete, or booster dose of COVID-19 vaccines between HIV-infected and non-HIV-infected patients. Cohort studies were defined as those that sampled participants based on exposure, followed-up participants over time, and ascertained the outcomes15. The definition of seroconversion differed across studies, and Supplementary Table S2 provides the corresponding definition for each study. Uncomplete vaccination was defined as one dose of an mRNA vaccine (BNT162b2 or mRNA-1273), inactivated vaccine (BBIBP-CorV, Corona Vac, or Sinopharm), adenovirus vaccine (ChA-dOx1 nCoV-19), or recombinant protein vaccine (NVX-CoV2373). Complete vaccination was defined as two doses of an mRNA vaccine (BNT162b2 or mRNA-1273), inactivated vaccine (BBIBP-CorV, Corona Vac, or Sinopharm), or adenovirus vaccine (ChA-dOx1 nCoV-19), recombinant protein vaccine (NVX-CoV2373), or a single dose of adenovirus vaccine (Ad.26.COV2.S). Booster vaccination was defined as an additional shot after complete vaccination scheme. Studies on non-comparative cohorts with less than 10 participants were excluded. Case reports, case series, and studies with data inaccessible from the corresponding author were excluded. For multiple articles that reported identical outcomes from the same cohort, we selected those with the largest and most up-to-date studies.
Data abstraction and quality assessment
Two investigators (Q.Z and F.Z) independently extracted data based on a predetermined proforma in Microsoft Excel. The following information was collected, including first author, publication year, country, study type, data source, patient number, control number, age, sex, vaccine type, vaccine dose, antiretroviral therapy, COVID-19 history, duration of follow-up, immunoassay, threshold for positive response, antibody titers, and adjustment parameters. We assessed risk of bias using two domain-based tools, including the Risk of Bias in Nonrandomized Studies of Interventions tool for comparative cohort studies, and the Cochrane Risk of Bias 2 tool for randomized controlled studies. For the Risk of Bias in Nonrandomized Studies of Interventions (ROBINS-I) tool16, risk of bias judgement per study is noted as low risk when all domains are judged as low risk of bias, moderate risk when one domain is judged as moderate risk of bias, serious risk when one domain is judged as serious risk of bias, or critical risk of bias when one domain is judged as critical risk of bias. For the Risk of Bias in the Cochrane Risk of Bias 2 tool, risk of bias judgement per study is noted as low risk when all domains are judged as low risk of bias, some concerns when one or more domains are judged as some concerns, or high risk when at least one domain is judged as high risk of bias, or when multiple domains are judged as some concerns. Risk of bias for non-comparative cohort studies was regarded as high risk of bias.
Outcomes of interest
The primary outcomes were the seroconversion rate following the uncomplete, complete, or booster dose of COVID-19 vaccines in patients living with HIV. The secondary outcomes were the risk ratios for seroconversion following the uncomplete, complete, or booster dose of COVID-19 vaccines between HIV-infected and non-HIV-infected patients.
Statistical analysis
All the analyses were performed and visualized with R statistic software (3.6.3). The principal summary measures used were pooled rate and risk ratio with 95% confidential interval (CI) of seroconversion following COVID-19 vaccination. χ2 test and I2 statistic were performed to evaluate the statistical heterogeneity of the results in the included studies. We considered heterogeneity to be significant when the P value by χ2 test was < 0.1 or the I2 statistic was ≥ 50%. The pooled seroconversion rate was assessed using the Freeman-Tukey double arcsine method. The pooled risk ratios were combined by the Mantel–Haenszel approach. Random-effects model was preferentially used as the primary approach to pool results across studies due to underlying clinical heterogeneity (eg, basic characteristics of the patients, COVID-19 history, adjustment for confounders).
Subgroup analyses were conducted following the complete dose of COVID-19 vaccines according to year of publication (2021 vs. 2022), study location (Europe vs. North America vs. South Africa vs. Asia vs. South America), study design (retrospective vs. prospective), source of data (multi-center vs. single-center), sample size (< 100 vs. ≥ 100), follow-up duration (< 2 months vs. ≥ 2 months), adjustment (yes vs. no), antiretroviral therapy (yes vs. not available), COVID-19 history (might be enrolled vs. none), and vaccine type (mRNA vs. adenovirus vs. inactivated vs. other vaccines). Meta-regression analyses were conducted to explore the potential effect of these parameters on the outcomes. The regression coefficient was calculated to describe the change of outcomes with explanatory variables (potential effect modifiers). Sensitivity analyses were conducted where the outcomes were recalculated by omitting one study at a time. Publication bias was evaluated by examining funnel plots (≥ 10 included studies) in combination with Egger’s test. If publication bias existed (funnel plot asymmetry, or Egger’s test P < 0.1), trim-and-fill analyses were performed to adjust for publication bias and further evaluate the stability of the pooled results. P value < 0.05 was considered statistically significant.
Result
Study selection, characteristics and quality assessment
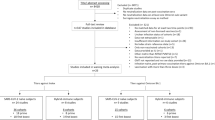
We identified 1592 citations through the literature search, excluded 1357 after initial title and abstract screening, and assessed the full text of 63 studies for eligibility. Another 13 studies were further removed for failing to report seroconversion (n = 6), cross-sectional studies (n = 5), reviews (n = 2) (File S1). Finally, 50 studies with a total of 7160 patients living with HIV were included in our meta-analysis11,12,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64, 30 studies were included for qualitative analysis of serological antibody titers (Supplementary Tables S3–S5); 46 studies11,12,17,18,19,20,21,22,23,24,25,27,28,29,30,31,32,34,35,36,37,38,39,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,58,59,60,61,62,63,64 were included for quantitative analysis of pooled seroconversion rate; 34 studies11,12,17,18,19,20,23,24,25,27,31,35,36,38,39,41,42,43,44,45,46,48,49,50,51,53,55,56,59,60,61,62,63,64 were used for quantitative analysis of pooled risk ratios for seroconversion following the uncomplete, complete, or booster dose of COVID-19 vaccines between patients living with HIV and HIV-negative vaccine counterparts (Fig. 1).
The main characteristics and clinical outcomes of the studies for quantitative analysis were summarized in Table 1 and Supplementary Table S2. The included studies were published between 2021 and 2022. Of these studies, 21 were from Europe, 11 from Asia, 9 from North America, 3 from South Africa and 2 from South America. The studies comprised 31 prospective studies and 15 retrospective studies. 19 studies were multicenter and 27 were single-center. The number of patients living with HIV in 18 studies was above 100; the follow-up duration in 15 studies was more than 2 months; only 11 studies had adjusted for potential confounders; the patients living with HIV in 40 studies received antiretroviral therapy; the patients living with HIV in 35 studies were not infected with COVID-19 prior to vaccination. In terms of vaccination type, mRNA vaccines were used in 26 studies; adenovirus vaccines were used in 3 studies; inactivated vaccines were used in 10 studies; and another 7 studies involved two or more vaccines or other types of vaccines. Supplementary Table S2 presents demographic characteristics, immunoassay and threshold for positive response. Supplementary Table S6 shows the detailed risk of bias for each study, and most of studies were regarded as critical or high risk of bias.
Seroconversion rate after uncomplete, complete, and booster vaccination
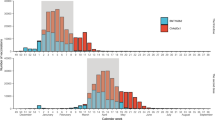
16 studies, 42 studies, and 6 studies evaluated the seroconversion rate of patients living with HIV after uncomplete, complete, and booster vaccination, respectively. As shown in Fig. 2a, the seroconversion rate was 75.0% (95% CI 56.4% to 89.9%) after uncomplete vaccination, 89.3% (95% CI 84.2% to 93.5%) after complete vaccination, and 98.4% (95% CI 94.8% to 100%) after booster vaccination. Significant heterogeneity was seen for the pooled seroconversion rate after uncomplete vaccination (I2 > 50%, P < 0.10) (Supplementary Fig. S1a). The funnel plot and Egger’s test (P = 0.47) did not detect the existence of publication bias in these studies (Supplementary Fig. S1b). The sensitivity analysis performed by using the “leave-one-out” did not markedly change our results (Supplementary Fig. S1c). Also, there is significant heterogeneity for the pooled seroconversion rate after complete vaccination (I2 > 50%, P < 0.10) (Supplementary Fig. S2). The funnel plot and Egger’s test (P < 0.01) suggested the existence of publication bias in these studies (Supplementary Fig. S3a). After 10 studies were filled, the funnel plot showed the relative symmetry (Supplementary Fig. S3b), and Egger’s test showed no evidence of significant publication bias (P = 0.49). The pooled seroconversion rate turned to be 96.6% (95% CI 92.6% to 99.2%) after complete vaccination. The sensitivity analysis did not significantly change our results (Supplementary Fig. S3c). As for the pooled seroconversion rate after booster vaccination, moderate heterogeneity was observed (I2 = 44%, P = 0.11) (Supplementary Fig. S4a), and the funnel plot showed the relative symmetry (Supplementary Fig. S4b), and Egger’s test showed no evidence of significant publication bias (P = 0.63). The results were stable after sensitivity analysis (Supplementary Fig. S4c).
Seroconversion compared with controls after uncomplete, complete, and booster vaccination
10 studies, 31 studies, and 3 studies compared the seroconversion with HIV-negative vaccine counterparts after uncomplete, complete, and booster vaccination. As suggested in Fig. 2b, the risk ratios were 0.87 (95% CI 0.77 to 0.99) after uncomplete vaccination, 0.95 (95% CI 0.92 to 0.98) after complete vaccination, and 0.97 (95% CI 0.94 to 0.99) after booster vaccination. Significant heterogeneity was seen for the pooled risk ratios for seroconversion after uncomplete vaccination (I2 > 50%, P < 0.10) (Supplementary Fig. S5a). The funnel plot and Egger’s test (P < 0.01) suggested the existence of publication bias in these studies (Supplementary Fig. S5b). After 5 studies were filled, the funnel plot showed relative symmetry (Supplementary Fig. S5c), and Egger’s test showed no evidence of significant publication bias (P = 0.89). The pooled risk ratios for seroconversion changed to 1.01 (95% CI 0.95 to 1.09) after uncomplete vaccination. The sensitivity analysis performed by using the “leave-one-out” did not markedly change our results except omitting Feng’s, Netto’s or Wong’s study (Supplementary Fig. S5d). Moreover, there is significant heterogeneity for the pooled seroconversion rate after complete vaccination (I2 > 50%, P < 0.10) (Supplementary Fig. S6). The funnel plot and Egger’s test (P < 0.01) suggested the existence of publication bias in these studies (Supplementary Fig. S7a). After 13 studies were filled, the funnel plot showed relative symmetry (Supplementary Fig. S7b), and Egger’s test showed no evidence of significant publication bias (P = 0.78). The pooled seroconversion rate turned to be 1.00 (95% CI 0.98 to 1.03) after complete vaccination. The sensitivity analysis did not significantly change our results (Supplementary Fig. S7c). Besides, there was minimal heterogeneity for seroconversion after booster vaccination (I2 = 7%, P = 0.34) (Supplementary Fig. S8a), and the funnel plot showed relative symmetry (Supplementary Fig. S8b), and Egger’s test showed no evidence of significant publication bias (P = 0.37). The results were stable after sensitivity analysis except omitting Vergori’s study (Supplementary Fig. S8c).
Meta-regression and subgroup analysis for seroconversion rate after complete vaccination
To examine whether the observed heterogeneity could be contributed by possible moderators for the pooled seroconversion rate after complete vaccination, univariate meta-regression was performed and suggested that study location and vaccine type were possible significant moderators (Supplementary Table S7). Subgroup analyses were further performed to evaluate the potential mediators for the pooled seroconversion rate after complete vaccination (Fig. 3, Supplementary Figs. S9–S18). Subgroup analysis according to year of publication demonstrated that the rate was lower in studies published in 2022, compared with studies published in 2021 (87.7% vs. 97.6%, P < 0.01). Subgroup analysis on basis of study location suggested that the rate was lowest in South America (59.1%), compared with Asia (73.1%), South Africa (74.7%), North America (93.9%), Europe (96.0%) (P < 0.01). Subgroup analysis stratified by vaccine type showed that the rate was lowest with inactivated vaccine (59%), compared with adenovirus vaccine (92.8%), mRNA vaccine (96.1%) or other vaccines (88.4%) (P < 0.01). There was no significant heterogeneity among all subgroup comparisons (all P > 0.05) when subgroup analyses were based on study design, source of data, sample size, follow-up duration, adjustment, antiretroviral therapy, or COVID-19 history.
Meta-regression and subgroup analysis for seroconversion compared with controls after complete vaccination
Univariate meta-regression was further performed to explore the origin of heterogeneity for seroconversion compared with controls after complete vaccination, and results showed that study location and vaccine type were also possible significant moderators (Supplementary Table S8). Subgroup analyses were further performed to evaluate the potential mediators for the pooled seroconversion compared with controls after complete vaccination (Fig. 4, Supplementary Figs. S19–S28). Subgroup analysis according to year of publication demonstrated that the risk ratio was lower in studies published in 2022, compared with studies published in 2021 (0.92 vs. 0.99, P < 0.01). Subgroup analysis on basis of source data suggested that the risk ratio was lower in single-center studies (0.93), compared with multi-center studies (0.99) (P = 0.03). Subgroup analysis stratified by vaccine type showed that the risk ratio was lowest with inactivated vaccine (0.73), compared with mRNA vaccine (0.98), adenovirus vaccine (1.03), or other vaccines (0.92) (P < 0.01). There was no significant heterogeneity among all subgroup comparisons (all P > 0.05) when subgroup analyses were based on study location, study design, sample size, follow-up duration, adjustment, antiretroviral therapy, or COVID-19 history.
Grading the quality of evidence
According to the GRADE approach, the quality of evidence was very low for seroconversion rate after uncomplete or complete vaccination, and the quality of evidence was low for overall seroconversion rate after booster vaccination (Supplementary Table S9a). The quality of evidence was low for seroconversion compared with controls after uncomplete or complete vaccination, and the quality of evidence was moderate for seroconversion compared with controls after booster vaccination (Supplementary Table S9b). Supplementary Table S9 provided the detailed criteria to down- or up- grade the level certainty.
Discussion
COVID-19 pandemic has ravaged across the globe, claiming the lives of more than 6 million people65. COVID-19 vaccines have been found to be the main measure of reducing the severity and mortality of COVID-19 patients5,6. Increasing studies indicated impaired serological response following vaccination in immunocompromised patients with cancer66,67,68, immune-mediated inflammatory disorders69,70,71, or organ transplant72,73,74. However, data are scarce on COVID-19 vaccination responses in patients living with HIV.
In this meta-analysis, we analyzed 50 studies with a total of 7160 patients living with HIV. We demonstrated that only 75.0% patients living with HIV achieved a seroconversion after uncomplete vaccination, which improved to 89.3% after complete vaccination, and 98.4% after booster vaccination. The seroconversion rates were significantly lower compared to controls at all the stages, while the risk ratios for uncomplete, complete, and booster vaccination were 0.87, 0.95, and 0.97, respectively, suggesting the urgent need for booster vaccination in patients living with HIV.
In the meta-regression and subgroup analysis, we found that year of publication, study location and vaccine type were possible significant moderators for the pooled rate and risk ratio for seroconversion after complete vaccination. As for year of publication, the seroconversion rate was lower in studies published in 2022, compared with studies published in 2021. A possible explanation is that virus variation weakens the effectiveness of the vaccine over time75,76,77. Regarding study location, the seroconversion rate was the lowest in South America, followed by Asia, South Africa, North America, and Europe. These location-specific differences were partly because of different vaccine types in these regions78,79. Moreover, Liu et al. previously predicted SARS-CoV-2 has different peptide-HLA hits for MHC class I and MHC class II peptides in white, black and Asian ancestry80, which could cause the difference in these regions. It is also worth noting that vaccine types affected the seroconversion in patients living with HIV, and the seroconversion rate was lowest with inactivated vaccine, followed by adenovirus vaccine, and mRNA vaccine. Kwok et al. and Peng et al. previously demonstrated that compared with mRNA vaccine, the antibody level of inactivated CoronaVac-vaccinees wane quickly and patients after the vaccine face a higher risk of breakthrough infection81,82. Besides, Alhinai et al. performed longitudinal analyses of publicly accessible epidemiological, clinical, virological, vaccine-related, and other public health data from 41 eligible countries, and found that the real-world effectiveness of inactivated virus vaccines might be inferior to mRNA and/or adenovirus-vectored vaccines83. Our results further validated previous findings, and provided solid evidence through comprehensively analyzing all the published papers. However, the subgroup differences we found highlight the need for high quality studies on these differences, specifically the improvement in the design of studies, greater geographical representation and comparison of vaccine types.
Admittedly, our study has several limitations. First, notable heterogeneity was found in some comparisons, which may be attributed to various immunoassay kits, threshold for seroconversion, and immune status at the time of COVID-19 vaccination in patients living with HIV29,31,84. However, sensitivity analysis, subgroup analysis and trim-and-fill analysis were used for meta-analysis, suggesting the stability of the results. Second, significant publication bias was observed in some comparisons, partly because most of studies enrolled were on mRNA vaccines, which could cause some bias in the results. Thirdly, here we failed to explore the effect of CD4 T cell absolute counts on the seroconversion of COVID-19 vaccines in HIV patients. This gap was filled by our other study showing that CD4 T cell count is positively correlated with seroconversion among COVID-19 vaccinated patients with HIV85. Finally, the rate of seroconversion was pooled after the uncomplete, complete, and booster vaccination. However, seroconversion rate is just an indicator of vaccine immune response and surrogate endpoints for the vaccine's impact on infection rates and the severity of COVID-1986,87,88. Data on clinical efficacy endpoints, such as COVID-19 infection rates in vaccinated patients living with HIV, are still lacking89.
Conclusion
Our meta-analysis summarized the pooled seroconversion rate and the pooled risk ratios following the uncomplete, complete, or booster dose of COVID-19 vaccines in patients living with HIV. We concluded that vaccine doses were associated with consistently improved seroconversion rates and risk ratios in patients living with HIV. Our study provides solid evidence that booster vaccination is necessary for patients living with HIV.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Geretti, A. M. et al. Outcomes of coronavirus disease 2019 (COVID-19) related hospitalization among people with human immunodeficiency virus (HIV) in the ISARIC World Health Organization (WHO) Clinical Characterization Protocol (UK): A prospective observational study. Clin. Infect. Dis. 73, e2095–e2106. https://doi.org/10.1093/cid/ciaa1605 (2021).
Western Cape Department of Health in collaboration with the National Institute for Communicable Diseases, S. A. Risk factors for coronavirus disease 2019 (COVID-19) death in a population cohort study from the Western Cape Province, South Africa. Clin. Infect. Dis. 73, e2005–e2015. https://doi.org/10.1093/cid/ciaa1198 (2021).
Tesoriero, J. M. et al. COVID-19 outcomes among persons living with or without diagnosed HIV infection in New York State. JAMA Netw. Open 4, e2037069. https://doi.org/10.1001/jamanetworkopen.2020.37069 (2021).
Bhaskaran, K. et al. HIV infection and COVID-19 death: A population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet HIV 8, e24–e32. https://doi.org/10.1016/S2352-3018(20)30305-2 (2021).
Polack, F. P. et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl. J. Med. 383, 2603–2615. https://doi.org/10.1056/NEJMoa2034577 (2020).
Dagan, N. et al. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N. Engl. J. Med. 384, 1412–1423. https://doi.org/10.1056/NEJMoa2101765 (2021).
Xu, H. et al. Effectiveness of inactivated COVID-19 vaccines against mild disease, pneumonia, and severe disease among persons infected with SARS-CoV-2 Omicron variant: Real-world study in Jilin Province, China. Emerg. Microb. Infect. https://doi.org/10.1080/22221751.2022.2149935 (2022).
Mallory, R. M. et al. Safety and immunogenicity following a homologous booster dose of a SARS-CoV-2 recombinant spike protein vaccine (NVX-CoV2373): A secondary analysis of a randomised, placebo-controlled, phase 2 trial. Lancet Infect. Dis. 22, 1565–1576. https://doi.org/10.1016/S1473-3099(22)00420-0 (2022).
Catherine, F. X. & Piroth, L. Hepatitis B virus vaccination in HIV-infected people: A review. Hum. Vaccin. Immunother. 13, 1–10. https://doi.org/10.1080/21645515.2016.1277844 (2017).
Pallikkuth, S. et al. Impact of aging and HIV infection on serologic response to seasonal influenza vaccination. AIDS 32, 1085–1094. https://doi.org/10.1097/QAD.0000000000001774 (2018).
Madhi, S. A. et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 in people living with and without HIV in South Africa: An interim analysis of a randomised, double-blind, placebo-controlled, phase 1B/2A trial. Lancet HIV 8, e568–e580. https://doi.org/10.1016/S2352-3018(21)00157-0 (2021).
Bergman, P. et al. Safety and efficacy of the mRNA BNT162b2 vaccine against SARS-CoV-2 in five groups of immunocompromised patients and healthy controls in a prospective open-label clinical trial. EBioMedicine 74, 103705. https://doi.org/10.1016/j.ebiom.2021.103705 (2021).
Lee, A. et al. Efficacy of covid-19 vaccines in immunocompromised patients: systematic review and meta-analysis. BMJ 376, e068632. https://doi.org/10.1136/bmj-2021-068632 (2022).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71. https://doi.org/10.1136/bmj.n71 (2021).
Dekkers, O. M., Egger, M., Altman, D. G. & Vandenbroucke, J. P. Distinguishing case series from cohort studies. Ann. Intern. Med. 156, 37–40. https://doi.org/10.7326/0003-4819-156-1-201201030-00006 (2012).
Sterne, J. A. et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355, i4919. https://doi.org/10.1136/bmj.i4919 (2016).
Frater, J. et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 in HIV infection: A single-arm substudy of a phase 2/3 clinical trial. Lancet HIV 8, e474–e485. https://doi.org/10.1016/S2352-3018(21)00103-X (2021).
Levy, I. et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in people living with HIV-1. Clin. Microbiol. Infect. 27, 1851–1855. https://doi.org/10.1016/j.cmi.2021.07.031 (2021).
Portillo, V. et al. Impact on HIV-1 RNA levels and antibody responses following SARS-CoV-2 vaccination in HIV-infected individuals. Front. Immunol. 12, 820126. https://doi.org/10.3389/fimmu.2021.820126 (2021).
Rahav, G. et al. BNT162b2 mRNA COVID-19 vaccination in immunocompromised patients: A prospective cohort study. EClinicalMedicine 41, 101158. https://doi.org/10.1016/j.eclinm.2021.101158 (2021).
Ruddy, J. A. et al. Safety and antibody response to two-dose SARS-CoV-2 messenger RNA vaccination in persons with HIV. AIDS 35, 2399–2401. https://doi.org/10.1097/QAD.0000000000003017 (2021).
Ruddy, J. A. et al. Safety and antibody response to the first dose of severe acute respiratory syndrome coronavirus 2 messenger RNA vaccine in persons with HIV. AIDS 35, 1872–1874. https://doi.org/10.1097/qad.0000000000002945 (2021).
Antinori, A. et al. Humoral and cellular immune response elicited by mRNA vaccination against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in people living with human immunodeficiency virus receiving antiretroviral therapy based on current CD4 T-lymphocyte count. Clin. Infect. Dis. 75, e552–e563. https://doi.org/10.1093/cid/ciac238 (2022).
Ao, L. et al. Safety and immunogenicity of inactivated SARS-CoV-2 vaccines in people living with HIV. Emerg. Microb. Infect. 11, 1126–1134. https://doi.org/10.1080/22221751.2022.2059401 (2022).
Balcells, M. E. et al. Reduced immune response to inactivated severe acute respiratory syndrome coronavirus 2 vaccine in a cohort of immunocompromised patients in Chile. Clin. Infect. Dis. 75, e594–e602. https://doi.org/10.1093/cid/ciac167 (2022).
Bessen, C. et al. Impact of SARS-CoV-2 vaccination on systemic immune responses in people living with HIV. Front. Immunol. 13, 1049070. https://doi.org/10.3389/fimmu.2022.1049070 (2022).
Brumme, Z. L. et al. Humoral immune responses to COVID-19 vaccination in people living with HIV receiving suppressive antiretroviral therapy. npj Vaccines https://doi.org/10.1038/s41541-022-00452-6 (2022).
Chan, D. P. C., Wong, N. S., Wong, B. C. K., Chan, J. M. C. & Lee, S. S. Three-dose primary series of inactivated COVID-19 vaccine for persons living with HIV, Hong Kong. Emerg. Infect. Dis. https://doi.org/10.3201/eid2810.220691 (2022).
Corma-Gómez, A. et al. Severe immunosuppression is related to poorer immunogenicity to SARS-CoV-2 vaccines among people living with HIV. Clin. Microbiol. Infect. https://doi.org/10.1016/j.cmi.2022.05.018 (2022).
Cossu, M. V. et al. Does the co-morbidity burden contribute to suboptimal immunological responses to COVID-19 vaccination in people living with HIV?. J. Infect. Dis. https://doi.org/10.1093/infdis/jiac286 (2022).
Feng, Y. et al. Immunogenicity of an inactivated SARS-CoV-2 vaccine in people living with HIV-1: A non-randomized cohort study. EClinicalMedicine 43, 101226. https://doi.org/10.1016/j.eclinm.2021.101226 (2022).
Gianserra, L. et al. Immunogenicity and safety of BNT162b2 homologous booster vaccination in people living with HIV under effective cART. Vaccines https://doi.org/10.3390/vaccines10081243 (2022).
Gidari, A. et al. BNT162b2 elicited an efficient humoral response against different strains of SARS-CoV-2 in people living with HIV. Curr. HIV Res. https://doi.org/10.2174/1570162x20666220729143949 (2022).
Gonzalez de Aledo, M. et al. Safety and immunogenicity of SARS-CoV-2 vaccines in people with HIV. AIDS 36, 691–695. https://doi.org/10.1097/QAD.0000000000003161 (2022).
Haidar, G. et al. Prospective evaluation of coronavirus disease 2019 (COVID-19) vaccine responses across a broad spectrum of immunocompromising conditions: The COVID-19 vaccination in the immunocompromised study (COVICS). Clin. Infect. Dis. 75, e630–e644. https://doi.org/10.1093/cid/ciac103 (2022).
Han, X. et al. Safety and immunogenicity of inactivated COVID-19 vaccines among people living with HIV in China. Infect. Drug Resist. 15, 2091–2100. https://doi.org/10.2147/idr.S353127 (2022).
Hassold, N. et al. Impaired antibody response to COVID-19 vaccination in advanced HIV infection. AIDS 36, F1-f5. https://doi.org/10.1097/qad.0000000000003166 (2022).
Heftdal, L. D. et al. Humoral response to two doses of BNT162b2 vaccination in people with HIV. J. Intern. Med. 291, 513–518. https://doi.org/10.1111/joim.13419 (2022).
Hensley, K. S. et al. Immunogenicity and reactogenicity of SARS-CoV-2 vaccines in people living with HIV in the Netherlands: A nationwide prospective cohort study. PLoS Med 19, e1003979. https://doi.org/10.1371/journal.pmed.1003979 (2022).
Jedicke, N. et al. Humoral immune response following prime and boost BNT162b2 vaccination in people living with HIV on antiretroviral therapy. HIV Med. 23, 558–563. https://doi.org/10.1111/hiv.13202 (2022).
Khan, K. et al. Immunogenicity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and Ad26.CoV2.S vaccination in people living with human immunodeficiency virus (HIV). Clin. Infect. Dis. 75, e857–e864. https://doi.org/10.1093/cid/ciab1008 (2022).
Lapointe, H. R. et al. People with HIV receiving suppressive antiretroviral therapy show typical antibody durability after dual COVID-19 vaccination, and strong third dose responses. J. Infect. Dis. https://doi.org/10.1093/infdis/jiac229 (2022).
Lombardi, A. et al. Anti-spike antibodies and neutralising antibody activity in people living with HIV vaccinated with COVID-19 mRNA-1273 vaccine: A prospective single-centre cohort study. Lancet Reg. Health. Eur. 13, 100287. https://doi.org/10.1016/j.lanepe.2021.100287 (2022).
Loubet, P. et al. One-month humoral response following two or three doses of messenger RNA coronavirus disease 2019 vaccines as primary vaccination in specific populations in France: First results from the Agence Nationale Recherche contre le Sida (ANRS)0001S COV-POPART cohort. Clin. Microbiol. Infect. https://doi.org/10.1016/j.cmi.2022.10.009 (2019).
Lv, Z. et al. Inactivated SARS-CoV-2 vaccines elicit immunogenicity and T-cell responses in people living with HIV. Int. Immunopharmacol. 102, 108383. https://doi.org/10.1016/j.intimp.2021.108383 (2022).
Madhi, S. A. et al. Immunogenicity and safety of a SARS-CoV-2 recombinant spike protein nanoparticle vaccine in people living with and without HIV-1 infection: a randomised, controlled, phase 2A/2B trial. Lancet HIV 9, e309–e322. https://doi.org/10.1016/S2352-3018(22)00041-8 (2022).
Milano, E. et al. Immunogenicity and safety of the BNT162b2 COVID-19 mRNA vaccine in PLWH: A monocentric study in Bari, Italy. J. Med. Virol. 94, 2230–2236. https://doi.org/10.1002/jmv.27629 (2022).
Nault, L. et al. Covid-19 vaccine immunogenicity in people living with HIV-1. Vaccine 40, 3633–3637. https://doi.org/10.1016/j.vaccine.2022.04.090 (2022).
Netto, L. C. et al. Safety and immunogenicity of CoronaVac in people living with HIV: a prospective cohort study. Lancet HIV 9, e323–e331. https://doi.org/10.1016/s2352-3018(22)00033-9 (2022).
Oyaert, M. et al. Evaluation of humoral and cellular responses in SARS-CoV-2 mRNA vaccinated immunocompromised patients. Front. Immunol. 13, 858399. https://doi.org/10.3389/fimmu.2022.858399 (2022).
Polvere, J. et al. B cell response after SARS-CoV-2 mRNA vaccination in people living with HIV. Commun. Med. (Lond) 3, 13. https://doi.org/10.1038/s43856-023-00245-5 (2023).
Pourcher, V. et al. High seroconversion rate and SARS-CoV-2 Delta neutralization in people with HIV vaccinated with BNT162b2. AIDS 36, 1545–1552. https://doi.org/10.1097/qad.0000000000003300 (2022).
Schmidt, K. G. et al. Characterization of serum and mucosal SARS-CoV-2-antibodies in HIV-1-infected subjects after BNT162b2 mRNA vaccination or SARS-CoV-2 infection. Viruses https://doi.org/10.3390/v14030651 (2022).
Speich, B. et al. Antibody response in immunocompromised patients after the administration of SARS-CoV-2 vaccine BNT162b2 or mRNA-1273: A randomised controlled trial. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciac169 (2022).
Spinelli, M. A. et al. Differences in post-mRNA vaccination severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) immunoglobulin G (IgG) concentrations and surrogate virus neutralization test response by human immunodeficiency virus (HIV) status and type of vaccine: A matched case-control observational study. Clin. Infect. Dis. 75, e916–e919. https://doi.org/10.1093/cid/ciab1009 (2022).
Tan, Y. et al. Early efficacy and safety of the third dose inactivated COVID-19 vaccine among people living with HIV. J. Acquir. Immune Defic. Syndr. 1999(90), e1–e3. https://doi.org/10.1097/qai.0000000000002953 (2022).
Tau, L. et al. SARS-CoV-2 humoral and cellular immune responses of patients with HIV after vaccination with BNT162b2 mRNA COVID-19 vaccine in the Tel-Aviv Medical Center. Open Forum Infect. Dis. 9, ofac089. https://doi.org/10.1093/ofid/ofac089 (2022).
Tuan, J. J. et al. Qualitative assessment of anti-SARS-CoV-2 spike protein immunogenicity (QUASI) after COVID-19 vaccination in older people living with HIV. HIV Med. 23, 178–185. https://doi.org/10.1111/hiv.13188 (2022).
Vergori, A. et al. SARS-CoV-2 omicron variant neutralization after third dose vaccination in PLWH. Viruses https://doi.org/10.3390/v14081710 (2022).
Woldemeskel, B. A. et al. The BNT162b2 mRNA vaccine elicits robust humoral and cellular immune responses in people living with human immunodeficiency virus (HIV). Clin. Infect. Dis. 74, 1268–1270. https://doi.org/10.1093/cid/ciab648 (2022).
Wong, N. S. et al. Surrogate neutralization responses following severe acute respiratory syndrome coronavirus 2 vaccination in people with HIV: Comparison between inactivated and mRNA vaccine. AIDS 36, 1255–1264. https://doi.org/10.1097/qad.0000000000003237 (2022).
Xu, X., Vesterbacka, J., Aleman, S. & Nowak, P. High seroconversion rate after vaccination with mRNA BNT162b2 vaccine against SARS-CoV-2 among people with HIV - but HIV viremia matters?. AIDS 36, 479–481. https://doi.org/10.1097/qad.0000000000003135 (2022).
Zeng, G. et al. IgG antibody responses and immune persistence of two doses of BBIBP-CorV vaccine or CoronaVac vaccine in people living with HIV (PLWH) in Shenzhen, China. Vaccines https://doi.org/10.3390/vaccines10060880 (2022).
Zou, S. et al. Immune response and safety to inactivated COVID-19 vaccine: A comparison between people living with HIV and HIV-naive individuals. AIDS Res. Ther. 19, 33. https://doi.org/10.1186/s12981-022-00459-y (2022).
World Health Organization, Coronavirus (COVID-19) Dashboard WHO Coronavirus (COVID-19) Dashboard with Vaccination Data, https://covid19.who.int/.
Massarweh, A. et al. Evaluation of seropositivity following BNT162b2 messenger RNA vaccination for SARS-CoV-2 in patients undergoing treatment for cancer. JAMA Oncol. 7, 1133–1140. https://doi.org/10.1001/jamaoncol.2021.2155 (2021).
Bird, S. et al. Response to first vaccination against SARS-CoV-2 in patients with multiple myeloma. Lancet Haematol. 8, e389–e392. https://doi.org/10.1016/S2352-3026(21)00110-1 (2021).
Roeker, L. E. et al. COVID-19 vaccine efficacy in patients with chronic lymphocytic leukemia. Leukemia 35, 2703–2705. https://doi.org/10.1038/s41375-021-01270-w (2021).
Reuken, P. A. et al. T Cell response after SARS-CoV-2 vaccination in immunocompromised patients with inflammatory Bowel disease. J. Crohns Colitis 16, 251–258. https://doi.org/10.1093/ecco-jcc/jjab147 (2022).
Haberman, R. H. et al. Methotrexate hampers immunogenicity to BNT162b2 mRNA COVID-19 vaccine in immune-mediated inflammatory disease. Ann. Rheum. Dis. 80, 1339–1344. https://doi.org/10.1136/annrheumdis-2021-220597 (2021).
Seyahi, E. et al. Antibody response to inactivated COVID-19 vaccine (CoronaVac) in immune-mediated diseases: a controlled study among hospital workers and elderly. Rheumatol. Int. 41, 1429–1440. https://doi.org/10.1007/s00296-021-04910-7 (2021).
Grupper, A. et al. Kidney transplant recipients vaccinated before transplantation maintain superior humoral response to SARS-CoV-2 vaccine. Clin. Transplant. 35, e14478. https://doi.org/10.1111/ctr.14478 (2021).
Miele, M. et al. Impaired anti-SARS-CoV-2 humoral and cellular immune response induced by Pfizer-BioNTech BNT162b2 mRNA vaccine in solid organ transplanted patients. Am. J. Transplant. 21, 2919–2921. https://doi.org/10.1111/ajt.16702 (2021).
Peled, Y. et al. BNT162b2 vaccination in heart transplant recipients: Clinical experience and antibody response. J. Heart Lung Transplant. 40, 759–762. https://doi.org/10.1016/j.healun.2021.04.003 (2021).
Li, X. et al. Long-term variations and potency of neutralizing antibodies against Omicron subvariants after CoronaVac-inactivated booster: A 7-month follow-up study. J. Med. Virol. https://doi.org/10.1002/jmv.28279 (2022).
Liang, H. Y. et al. SARS-CoV-2 variants, current vaccines and therapeutic implications for COVID-19. Vaccines https://doi.org/10.3390/vaccines10091538 (2022).
World Health Organization. SARS-CoV-2 variants, working definitions and actions taken, https://www.who.int/activities/tracking-SARS-CoV-2-variants (2022).
Abdelhafiz, A. S. et al. Sinopharm’s BBIBP-CorV vaccine and ChAdOx1 nCoV-19 vaccine are associated with a comparable immune response against SARS-CoV-2. Vaccines https://doi.org/10.3390/vaccines10091462 (2022).
France 24 Egypt Plans to Make 1 Billion Sinovac Vaccines a Year, https://www.france24.com/en/live-news/20210901-egypt-plans-to-make-1-billion-sinovac-vaccines-a-year.
Liu, G., Carter, B. & Gifford, D. K. Predicted cellular immunity population coverage gaps for SARS-CoV-2 subunit vaccines and their augmentation by compact peptide sets. Cell Syst. 12, 102-107.e104. https://doi.org/10.1016/j.cels.2020.11.010 (2021).
Peng, Q. et al. Waning immune responses against SARS-CoV-2 variants of concern among vaccinees in Hong Kong. EBioMedicine 77, 103904. https://doi.org/10.1016/j.ebiom.2022.103904 (2022).
Kwok, S. L. et al. Waning antibody levels after COVID-19 vaccination with mRNA Comirnaty and inactivated CoronaVac vaccines in blood donors, Hong Kong, April 2020 to October 2021. Euro Surveill https://doi.org/10.2807/1560-7917.ES.2022.27.2.2101197 (2022).
Alhinai, Z., Park, S., Choe, Y. J. & Michelow, I. C. A global epidemiological analysis of COVID-19 vaccine types and clinical outcomes. Int J Infect Dis 124, 206–211. https://doi.org/10.1016/j.ijid.2022.09.014 (2022).
Avelino-Silva, V. I. et al. CD4/CD8 ratio and KT ratio predict yellow fever vaccine immunogenicity in hiv-infected patients. PLoS Negl. Trop. Dis. 10, e0005219. https://doi.org/10.1371/journal.pntd.0005219 (2016).
Zhou, Q. et al. Correlation between CD4 T-cell counts and seroconversion among COVID-19 vaccinated patients with HIV: A meta-analysis. Vaccines https://doi.org/10.3390/vaccines11040789 (2023).
Jin, P., Li, J., Pan, H., Wu, Y. & Zhu, F. Immunological surrogate endpoints of COVID-2019 vaccines: The evidence we have versus the evidence we need. Signal Transduct. Target Ther. 6, 48. https://doi.org/10.1038/s41392-021-00481-y (2021).
Earle, K. A. et al. Evidence for antibody as a protective correlate for COVID-19 vaccines. Vaccine 39, 4423–4428. https://doi.org/10.1016/j.vaccine.2021.05.063 (2021).
Garcia-Beltran, W. F. et al. COVID-19-neutralizing antibodies predict disease severity and survival. Cell 184, 476-488.e411. https://doi.org/10.1016/j.cell.2020.12.015 (2021).
Coburn, S. B. et al. Analysis of postvaccination breakthrough COVID-19 infections among adults with HIV in the United States. JAMA Netw. Open 5, e2215934. https://doi.org/10.1001/jamanetworkopen.2022.15934 (2022).
Funding
This research is supported by the National Natural Science Foundation of China (nos. 82102803, 82103183, 82272849), and Natural Science Foundation of Hunan province (nos. 2021JJ40976, 2022JJ40767).
Author information
Authors and Affiliations
Contributions
Concept and design: G.D. and H.L. Acquisition and interpretation of data: Q.Z. and F.Z. Drafting of the manuscript: F.Z. and Q.Z. Critical revision of the manuscript: G.D., Q.Z., Y.M. and Y.L. Final approval: All authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhou, Q., Zeng, F., Meng, Y. et al. Serological response following COVID-19 vaccines in patients living with HIV: a dose–response meta-analysis. Sci Rep 13, 9893 (2023). https://doi.org/10.1038/s41598-023-37051-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-37051-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.