Abstract
Micronutrient deficiency has serious consequences across all ages worldwide, particularly in sub-Saharan Africa. Poor micronutrient (MN) consumption among children remains a major public health concern in many countries. Low literacy, poor diets, a lack of access to healthcare, and insufficient agricultural productivity made proper micronutrient consumption difficult, despite numerous interventions. Thus, this research aimed to determine the adequate intake of MNs among 6–23 months of age children in sub-Saharan Africa. Initially, a two-stage stratified sampling technique was applied for the selected recent demographic and health survey data. The data source was the (2015–2020) standard demographic and health surveys (DHS) among 20 Sub-Saharan African countries. Micronutrient intake status (the outcome variable) was determined using either food rich in Vitamin A or iron consumed within the previous 24 hr or multiple micronutrient powder or iron supplementation within the previous 07 days or vitamin A supplementation or deworming within 06 months. A generalized linear mixed model based on Modified Poisson regression and robust error variance was used to identify factors associated with children’s adequate micronutrient intake. An adjusted Prevalence Ratio (aPR) with a 95% confidence interval was used to identify factors, strength and direction of the association. The total samples of 65,187 children aged 6–23 months were included. Of all, 73.99% (95% CI: 73.65, 74.32) of children had adequate intake of micronutrients. Maternal education (primary (aPR = 1.04, 95% CI: 1.02, 1.06) and secondary (aPR = 1.07, 95% CI: 1.04, 1.09)), father’s education (primary (aPR = 1.03, 95% CI: 1.01, 1.05) and secondary (aPR = 1.04, 95% CI: 1.02, 1.06)), occupational status of the mother (aPR = 1.04, 95% CI: 1.02, 1.06), pregnancy interval (aPR = 0.97, 95% CI: 0.95, 0.99), exclusive breastfeeding status (aPR = 0.83, 95% CI: 0.82, 0.85), birthweight (average (aPR = 1.03, 95% CI: 1.01, 1.05) and larger than average (aPR = 1.04, 95% CI: 1.02, 1.06)), multiple/twin at birth (aPR = 0.94, 95% CI: 0.91, 0.98), child age (aPR = 1.22, 95% CI: 1.19, 1.25), number of children in home (aPR = 1.02, 95% CI: 1.01, 1.03), ANC utilization (aPR = 1.20, 95% CI: 1.15, 1.27), place of birth (AOR = 0.93, 95% CI: 0.91, 0.95), rich households (aPR = 1.03, 95% CI: 1.01, 1.05), and countries from Central (aPR = 1.07, 95% CI: 1.04, 1.09), South Africa (aPR = 1.07, 95% CI: 1.03, 1.11), and West African (aPR = 0.95, 95% CI: 0.92, 0.99) were associated with level of micronutrients intake status. The prevalence of adequate intake of MN was considerable. Variables at the child, family and community levels were associated with adequate intake of micronutrients. Consequently, stakeholders’ involvement is required in healthcare and community settings.
Similar content being viewed by others
Introduction
One in two under-five children suffers from hidden hunger (micronutrient deficiency), which accounts for more than 340 million cases1 and is associated with the highest burden of diseases in Africa2. As a result, significant numbers of deaths were contributed by both micro and macronutrient deficiencies3. So, adequate nutrition during childhood is critical for optimal growth, health and development. Falling to meet the body requirement due to inadequate intake, highest losses and increased demand will lead to growth faltering, micronutrient deficiencies and common childhood illnesses4,5. Globally, micronutrient malnutrition is very prevalent6 and significantly contributes to child morbidity and mortality7. A billion individuals were predicted to be deficient in essential micronutrients (vitamins and minerals) like vitamin A, iodine and zinc8. Mostly in Africa, millions of vulnerable groups like children face one form of Micronutrient Deficiency9 regardless of different micronutrient deficiency prevention strategy the implementation10.
Nowadays, according to our knowledge, there is no database to show adequate intake of micronutrients worldwide including sub-Saharan African (SSA) countries. But there are pocket studies in including sub-Saharan African (SSA) countries to show the magnitude of components of micronutrient intake. In Ethiopia, 37.3% of children aged 6–23 months had not received any recommended micronutrients (MNs) sources11. Another systematic review (four countries: Ethiopia, Nigeria, Kenya, and South Africa) found that inadequate intakes varied from 51 to 99% for zinc, 13 to 100% for iron, and 1 to 100% for vitamin A, with households consuming iodized salt at rates ranging from 2 in Kenya to 96% in Ethiopia12. In addition, a study in South Africa shows that preschool children and their caregivers consumed a diet deficient in most of the essential micronutrients; due to poor quality of the diet with low vitamin A and iron status, one-fifth of the children had linear growth retardation13. Furthermore, a study in the pastoralist community of Kenya suggests that the highest probability of inadequacies for vitamins A, B12, and C and this is associated with different individual and household level factors14.
The most common contributors for inadequate micronutrient intakes are difference in residency area and geography11, racial differences, lower education and self-reported economic-related food insecurity15, monotonous diet, low bioavailability, seasonal variations and eating phytate foods as staple foods8,16. On the other hand, lack of availability and access to health care facilities, trained personnel and poor health care set-ups were also a factor that hinder the adequate services4.
The problem is escalating in developing countries due to a lack of consumption of the recommended sources of micronutrients like grains, roots and tubers, legumes and nuts, dairy products, flesh foods (meat, fish, poultry, and organ meats), eggs, vitamin A rich fruits and vegetables, and other fruits and vegetables consumed within the previous 24 h17. Hence, to address the scarcity of literature on the significant effect of individual and/or community level factors on adequate intake of micronutrients in SSA, this study utilized a multilevel modified Poisson regression model. As a result, this study sought to identify the individual and/or community-level factors associated with adequate micronutrient intake in children aged 6 to 23 months in sub-Saharan African countries.
Methods
Data sources
The data source was the recent (2015–2020) standard demographic and health survey (DHS) among 20 sub-Saharan African countries. The data were obtained from the DHS program (http://www.dhsprogram.com/) after a formal written request. A nationally representative standard DHS was used to estimate the pooled magnitude of micronutrient intake status among children 6–23 months of age in sub-Saharan Africa. The data were collected through a multistage stratified cluster sampling technique for each country. The nature of the data is hierarchal since the individuals are nested in regions and nations.
From all SSA countries, 17 countries datasets (namely: Benin, Burundi, Cameroon, Ethiopia, Gambia, Guinea, Liberia, Mali, Malawi, Nigeria, Rwanda, Sierra Leone, Tanzania, Uganda, South Africa, Zambia, and Zimbabwe) were included for this study. All other countries' data sets were excluded due to the absence of dataset, old dataset, and no denominator and numerator variables according to the guide to DHS statistics version 7.218.
Study population
For this study, all children 6–23 months of age with their mothers’ or caregivers’ records or data were the study population.
Study variables
In this study, the outcome variable is micronutrient intake status. Micronutrient intake status was determined using either food rich in Vitamin A or iron consumed within the previous 24 hr or multiple micronutrient powder or iron supplementation within the previous 07 days or vitamin A supplementation or deworming within 06 months18.
Individual or community level, or both factors, affected the micronutrient intake status of children aged 6 to 23 months.
Individual-level variables
Both maternal (socio-demographic and maternal health service utilization from pregnancy to postnatal time) and child-related variables have been included at this stage.
Community-level variables
As community-level variables, the place of residence, economic region, and the country was included.
Data processing and analysis
After obtaining the data set for each country from DHS programs, the data analysis was explored using Stata 16/MP (Stata Corporation IC., TX, USA) for Windows. The wealth index is obtained directly from the dataset that ranges from poorest to richest. Due to the hierarchical nature of DHS data, the observation of the data violates the assumption of independence. To assess the variation among the cluster, we estimated the Intra-class Correlation Coefficient (ICC) and deviance values. The outcome variable (adequate intake of MNs) was determined according to DHS statistics guide 7.2 using the following variables: foods rich in vitamin A and iron, supplementation of multiple micronutrient powder (MNP), iron, vitamin A and or deworming.
We were forced to use a generalized linear mixed model with Poisson regression (modified) and the robust error of variance to identify factors associated with micronutrient intake in SSA because the outcome variable, MN intake status among children 6–23 months of age, is (73.99%). Then, we have fitted four models: the null model (without independent variables), the model I (only individual-level variables (child and maternal sociodemographic variables)), model II (only community-level variables (residence and region)), and model III (both the individual and community level variables). Model III had the smallest deviance (-2LL) value of all models and was chosen as the best-fitted model for the discussion of this study result.
Before building all these models, a bi-variable generalized linear mixed (GLM) effect model using modified Poisson regression with the robust error of variance was employed to identify candidate variables for multivariable analysis in each category. Finally, a multivariable multilevel GLM effect model using Modified Poisson regression with the robust error of variance analysis was done for variables with a p-value < 0.25 during the bi-variable analysis (for initial assessment/screening). We have calculated the unadjusted and adjusted prevalence ratios (aPR) with 95% CI. We declare the statistical significance of variables and the degree of strength of the effect size by estimating the Confidence Intervals.
Parameter estimation method
In this study, parameters were estimated as follows:
-
Intra-class correlation Coefficient (ICC) was calculated as; ICC = \(\frac{\left({\mathrm{\sigma \mu }}^{2}\right)}{\upsigma {\upmu }^{2}+\upsigma {\mathrm{e}}^{2}}\) , where σμ2 is the variance of the group level; and σe2 denotes the variance of the individual level19.
-
Proportional change in variance (PCV) was calculated as; PCV \(=\frac{\left({V}_{0}-{V}_{x}\right)*100}{{V}_{0}}\), where V0 is the variance of the null model and Vx is each the variance of each model at each level with variables19.
-
Prevalence median ratio (PMR) was calculated as; PMR = exp \(\sqrt{2{\upsigma }^{2}*{\Phi }^{-1}(3/4)]}\), where σ2 is the variance of each model and Φ−1 is inverse of the standard normal cumulative distribution function20
Ethical consideration
The International Review Board of Demographic and Health Surveys (DHS) program data archivists were allowed to download and use the datasets for this study. Also, the data was handled according to the Helsinki Declaration of the World Medical Association.
Results
Sociodemographic characteristics of the participants
This report included 65,187 children aged 6 to 23 months from each nation (17 SSA countries). The mean ± SD of the children’s age was 12.79 ± 6.43 months. The mean ± SD of the mother’s/caregivers age was 27.96 ± 6.82 years. Of all, 70.96% of the mothers/caregivers found between 20 and 34 years of age. More than one-third and one-fourth of the mothers in sub-Saharan Africa have not attended any formal education and no formal work, correspondingly (Table 1).
Reproductive health-related characteristics
Of all, 44,667 (68.52%) respondents were < 20 years of age at their first pregnancy. According to this pooled data, the magnitude of institutional delivery for the index child was 46,628 (71.53%). Only one-third of the respondents were starting ANC follow-up before the end of the first trimester. One fourth of the mothers did not exclusively breastfeed their children (Table 2).
Cluster variation analysis
The measure of variation was measured for each model through Intra Class Correlation (ICC), Median Prevalence Ratio (MPR), and deviance. In the null model, the value of ICC was 10.67% (95% CI: 8.68, 13.06), which shows the presence of heterogeneity of micronutrient intake status among regions (clusters), as also indicated by the MPR with a value of 1.11. It means that, if we randomly select a child, a child in the regions with higher micronutrient intake status was 1.11 times higher as compared to a child in regions with lower micronutrient intake status.
Of all models that measure variations, model III has the lowest MPR and the deviance value, which was 1.04 and 34,163.07, respectively. So, model III was selected as the best-fitted model for this analysis (Table 3).
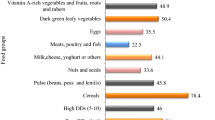
The pooled magnitude of micronutrient intake status in sub-Saharan Africa
The overall magnitude of adequate micronutrient intake status among children 6 – 23 months of age in sub-Saharan Africa was (73.99%, 95% CI 73.65, 74.32). The highest micronutrient intake status was found in Burundi (85.53%) and Rwanda (85.48%) followed by Malawi (82.18%) while the lowest was found in Ethiopia (59.10%) followed by Guinea (60.05%) as shown in the table below (Table 4). In sub-Saharan Africa, the proportion of recommended MNs consuming Vitamin A rich foods, Iron-rich foods, MMPs, Iron supplementation, Vitamin A supplementation, and deworming was (35,934 (55.12%), (22,568 (34.62%)), (2247 (3.45%)), (8670 (13.30%)), (33,497 (51.39%)), and (20,939 (32.12%)), respectively.
Factors associated with micronutrient intake status
Initially, a bi-variable multilevel GLM model using Poisson regression with robust error variance was used to identify factors associated with adequate micronutrient intake status of children 06 – 23 months of age in sub-Saharan African Countries. A separate model for individual, community, or both (community and individual level) factors were employed. From all models, the fourth model, which contained both individual and community level factors were identified as the best fit model with the lowest negative likelihood ratios (− 34,163.07(AIC = 68,388.14)) or deviance (68,326.14) values.
During bi-variable analysis; Age of the respondent, maternal educational status, father's educational status, maternal occupational status, father's occupational status, family size, age at first pregnancy, pregnancy interval, exclusive breastfeeding status, the weight of the child at birth, plurality, age of the child, mode of delivery, number of children, ANC Utilization, time to start ANC follow up, place of delivery, media exposure, residence, wealth Index, and economic regions of SSA countries were the significant variables.
All these variables were fitted into a multivariable multilevel GLM model using Poisson regression with the robust error of variance analysis. Finally, maternal educational status, father's educational status, maternal occupational status, pregnancy interval, exclusive breastfeeding, the weight of the child at birth, plurality, age of the child, number of children, ANC Utilization, time to start ANC follow-up, place of delivery, wealth index, and economic regions of SSA countries were the associated factors with adequate intake of micronutrients (MNs) status among 06 – 23 months of age children (Table 5).
Children from a mother with primary and secondary education were 4% (aPR = 1.04, 95% CI: 1.02, 1.06) and 7% (aPR = 1.07, 95% CI: 1.04, 1.09) higher prevalence of adequate intake of MNs as compared to those who were from mothers without any formal education. Children from a father with primary and secondary education were 3% (aPR = 1.03, 95% CI: 1.01, 1.05) and 1.04 (aPR = 1.04, 95% CI: 1.02, 1.06) more prevalence of adequate intake of MNs as compared to those who were from a father without any formal education.
Children who were from a mother with any job had a 4% (aPR = 1.04, 95% CI: 1.02, 1.06) higher prevalence of adequate intake of MNs as compared to their counterparts. Also, children born with a pregnancy interval of fewer than 23 months were a 3% (aPR = 0.97, 95% CI: 0.95, 0.99) lower prevalence of adequate intake of MNs as compared to their counterparts. Also, no exclusive breastfeeding children had a 17% (aPR = 0.83, 95% CI: 0.82, 0.85) lower prevalence of adequate intake of MNs as compared to those who have exclusive breastfeeding.
Similarly, children born with average and larger than average were 3% (aPR = 1.03, 95% CI: 1.01, 1.05) and 4% (aPR = 1.04, 95% CI: 1.02, 1.06) higher prevalence of adequate MNs as compared to children born as smaller than average. Also, children born multiple/twin were had 6% (aPR = 0.94, 95% CI: 0.91, 0.98) lower prevalence of adequate intake of MNs as compared to children born single.
Children 12 to 23 months of age were a 22% (aPR = 1.22, 95% CI: 1.19, 1.25) higher prevalence of adequate intake of MNIS as compared to children 6 to 11 months of age. An index child with more than 4 children at home have 2% (aPR = 1.02, 95% CI: 1.01, 1.03) higher prevalence of adequate intake of MNs as compared to children from less than four. The prevalence of having adequate MNs were 20% (aPR = 1.20, 95% CI: 1.15, 1.27) higher than children born from mothers without ANC utilization.
Children born at home were a 7% (AOR = 0.93, 95% CI: 0.91, 0.95) lower prevalence of having an adequate intake of MNs as compared to children born in health institutions. Also, children from rich households were a 3% (aPR = 1.03, 95% CI: 1.01, 1.05) higher prevalence of adequate intake of MNs as compared to children born in poor households.
Besides these, children born from the economic regions of Central and South Africa were a 7% (aPR = 1.07, 95% CI: 1.04, 1.09) and 7% (aPR = 1.07, 95% CI: 1.03, 1.11) higher prevalence of adequate intake of MNs as compared to East African countries respectively. On the other hand, children from West African countries were a 5% (aPR = 0.95, 95% CI: 0.92, 0.99) lower prevalence of adequate intake of MNs as compared to East African countries.
Discussion
Adequate intakes of micronutrients have a significant role in the optimal health, growth and development of a child. But there is no pooled data related to this and its contributing factors in SSA. Therefore, this study helps to fill this gap by generating evidence among children 6 – 23 months of age.
The overall magnitude of adequate micronutrient intake status among children 6 – 23 months of age in sub-Saharan Africa was (73.99%, 95% CI: 73.65, 74.32) that ranges from 59.1% in Ethiopia to 85% in Burundi and Rwanda. This finding is higher than a study conducted in Ethiopia (63.7%)11, South Africa (< 50% of the RDA)13 and Bangladesh21. Similarly, different studies elsewhere using one of the components to measure micronutrient intake status shows that the intake is less than the recommended shows due to low intake of animal food sources, and the highest tubers and cereals consumption in Africa22,23. The possible justification might be variation across regions; the dietary intake is varying across regions due to cultural, availability, accessibility and religious differences. Also, the type of staple food varies in each geographic region as per their beliefs, traditions, food insecurity and literacy.
The intake of adequate micronutrients by the children was more likely among households who had parents (mothers and fathers) with the educational status primary and secondary, while we compared the children from parents/caregivers without any formal education. This finding is in agreement with other studies22,23,24,25. The higher odds of adequate consumption of micronutrients in children from educated parents might be due to better exposure to media, change in knowledge and behaviors, and increasing purchasing power of different food items.
Likewise, children who had a mother with any job had a higher prevalence of adequate intake of MNs as compared to their counterparts which is in line with other different studies3,26,27, the possible justification might be the strong association between job and income; a mother with regular income may have purchasing capacity of varieties of food regularly and may be linked with literacy level and exposure to media, which is increasing access to information about feeding practices and consumption of adequate intake of micronutrients.
Also, children who had a pregnancy interval of less than 23 months, born at home and without exclusive breastfeeding had a low level of adequate intake of MNs as compared to their counterparts. Likewise, different studies show that children from mothers/caregivers who were adhering to reproductive health services/issues were more likely to have an adequate intake of MNs, dietary diversity and meal frequency as compared to their counterparts11,22,26,28. It is a known fact that women with adequate follow-up will know appropriate infant and child feeding practices due to repeated counselling, which intern helps to improve frequent and diversified foods consumption.
Similarly, children born with average and larger than average were 3% (aPR = 1.03, 95% CI: 1.01, 1.05) and 4% (aPR = 1.04, 95% CI: 1.02, 1.06) higher prevalence of adequate MNs as compared to children born as smaller than average, which is in line with the study conducted in South Africa13. Because children's linear growth will be reflected by maternal inadequate intake of nutrients from preconception to date due to lack of variety of foods. This indicates that inadequate nutrients that affect the linear growths were persisting as a problem.
The other socio-demographic factors associated with a lower level of adequate intake of MNs are children who are twins and have more than 4 (four) children at home. Similarly, studies have shown that family size influences children’s dietary intake29,30,31. The possible justification might be the significant associations between food groups consumed. As the family size increase, the portion/meal size, nutrient density, quality of diet and affect the purchasing power of the households, which may affect the level of adequate intake of nutrients. Usually, what is observed is that a greater number of children in the house increases the risk of less adequacy of micronutrients intake.
Like a study in LMICs32 and East Africa23, this study, children from rich households had an adequate intake of MNs as compared to children born in poor households. This might be due to the purchasing power of households will be associated with overall healthier dietary patterns. Individuals with the highest socioeconomic status (SES) are more likely to consume healthy foods (rich in micronutrients) but not for children belong from low SES.
Children 12 to 23 months of age were a 22% (aPR = 1.22, 95% CI: 1.19, 1.25) higher magnitude of adequate intake of MNIS as compared to children 6 to 11 months of age, which is revealed by the studies conducted East Africa23 and Ethiopia33. This might be due to the late introduction of complementary feeding, caregivers' perception towards feeding a variety of food for age and beliefs, taboos and practices.
The prevalence of having adequate MNs were 20% (aPR = 1.20, 95% CI: 1.15, 1.27) higher than children born from mothers without ANC utilization. Likewise, a pooled study of young child feeding practices in the East African Region23 and iron-rich food consumption27 shows the link between maternal health care follow-up and adequate intake of nutrients. The possibility of receiving health information on child nutrition from health care providers during ANC and PNC services may help to change their behaviours and increase appropriate feeding practices, which is a clear indication to promote and offer universal ANC and PNC for mothers in SSA countries to improve micronutrient consumptions.
Besides these, children born from the economic regions of Central and South Africa were more adequate intake level MNs as compared to East African countries, likewise, children from West African countries had a lower level of adequate intake of MNs. Like this, a systematic review reveals that adequate intake of MNs varies across the region including developed countries and Nepal24 similarly. This systematic review shows that the existence of shows limited intake of micronutrients in Central and Eastern Europe than in other European countries25,34. The association between geographical region/location and adequate intake of MNs will be seasonal variability and type of food sources. Also, it might be due to the variations in education, occupation and income levels across regions. Furthermore, different socioeconomic positions within these countries may exist in greater social inequalities, diversity in food costs, access and availability.
This study's strength is that it attempts to pool adequate micronutrient intake in children aged 6–23 months at the SSA level using a large representative sample. As a result, it is generalizable. It also assessed the impact of individual and community-level variables on MN intake using reliable methods. Furthermore, the study is limited by the cross-sectional nature of the survey, affected recall bias during the interview, time between the survey and deworming medication intake, deworming was used in the last 6 months as an indirect indicator of the adequacy of micronutrients in the diet, a lack of bioavailability data, and an inability to determine the quantity and quality of dietary sources.
Conclusion
The overall magnitude of adequate intake of micronutrients in the sub-Saharan region among children 06 – 23 months of age is high. Both individual (maternal educational status, father's educational status, maternal occupational status, pregnancy interval, exclusive breastfeeding, weight of the child at birth, plurality, age of the child, number of children, ANC Utilization, time to start ANC follow-up, place of delivery) and community-level (wealth index, and economic regions of SSA countries) variables were associated with the adequate intake of micronutrients (Supplementary Information).
To strengthen further, health care workers at health institutions and community settings shall give attention to promoting means of adequate micronutrient intake. Also, governments shall have to follow the progress activities and strategies related to adequate intake of micronutrients by children routinely.
Data availability
The compiled dataset is available from the authors upon reasonable request from corresponding author and with permission of The DHS Program.
Abbreviations
- ANC:
-
Antenatal care
- aPR:
-
Adjusted prevalence ratio
- CI:
-
Confidence interval
- DHS:
-
Demographic and health survey
- ICC:
-
Intra-class correlation coefficient
- LLR:
-
Log-likelihood ratio
- MNs:
-
Micronutrients
- MPR:
-
Median odds ratio
- PCV:
-
Proportion of coefficient of variations
- SSA:
-
sub-Saharan Africa
- SVD:
-
Spontaneous vaginal delivery
- WHO:
-
World health organization
References
UNICEF. The State of the World’s Children 2019 [Internet]. https://www.unicef.org/reports/state-of-worlds-children-2019 (Accessed 18 August 2022).
Vos, T. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390(10100), 1211–1259 (2017).
Black, R. E. et al. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 371(9608), 243–260 (2008).
Tzioumis, E., Kay, M. C., Bentley, M. E. & Adair, L. S. Prevalence and trends in the childhood dual burden of malnutrition in low- and middle-income countries, 1990–2012. Public Health Nutr. 19(8), 1375–1388 (2016).
Adelekan, D. A. Multiple micronutrient deficiencies in developing countries. Nutrition 19(5), 473–474 (2003).
Bhutta, Z. A., Salam, R. A. & Das, J. K. Meeting the challenges of micronutrient malnutrition in the developing world. Br. Med. Bull. 106, 7–17 (2013).
WHO. Assessing the iron status of populations: including literature reviews [Internet]. https://www.who.int/publications-detail-redirect/9789241596107 (Accessed 18 August 2022).
WHO. Preventing and controlling micronutrient deficiencies in populations affected by an emergency: multiple vitamin and mineral supplements for pregnant and lactating women, and for children aged 6 to 59 months [Internet]. https://www.who.int/publications/m/item/WHO-WFP-UNICEF-statement-micronutrients-deficiencies-emergency (Accessed 19 August 2022).
WHO. The African Regional Health Report [Internet]. WHO | Regional Office for Africa. https://www.afro.who.int/sites/default/files/2017-06/african_regional_health_report2006_0.pdf (Accessed 19 August 2022).
WHO. 2012–2013 biennium report: Department of Nutrition for Health and Development: evidence and programme guidance [Internet]. World Health Organization; 2014. Report No.: WHO/NMH/NHD/EPG/14.1. https://apps.who.int/iris/handle/10665/101179 (Accessed 19 August 2022).
Gebremedhin, T., Aschalew, A. Y., Tsehay, C. T., Dellie, E. & Atnafu, A. Micronutrient intake status and associated factors among children aged 6–23 months in the emerging regions of Ethiopia: A multilevel analysis of the 2016 Ethiopia demographic and health survey. PLoS One 16(10), e0258954 (2021).
Harika, R. et al. Are low intakes and deficiencies in iron, vitamin A, zinc, and iodine of public health concern in Ethiopian, Kenyan, Nigerian, and South African children and adolescents?. Food Nutr. Bull. 38(3), 405–427 (2017).
Faber, M., Jogessar, V. B. & Benadé, A. J. S. Nutritional status and dietary intakes of children aged 2–5 years and their caregivers in a rural South African community. Int. J. Food Sci. Nutr. 52(5), 401–11 (2001).
Iannotti, L. & Lesorogol, C. Dietary intakes and micronutrient adequacy related to the changing livelihoods of two pastoralist communities in Samburu, Kenya. Curr. Anthropol. 55(4), 475–482 (2014).
Brunst, K. J. et al. Racial/ethnic and sociodemographic factors associated with micronutrient intakes and inadequacies among pregnant women in an urban US population. Public Health Nutr. 17(9), 1960–1970 (2014).
Gegios, A. et al. Children consuming cassava as a staple food are at risk for inadequate zinc, iron, and vitamin A intake. Plant Foods Hum. Nutr. 65, 64–70 (2010).
FAO. Guidelines for measuring household and individual dietary diversity [Internet]. https://www.fao.org/3/i1983e/i1983e00.htm (Accessed 18 August 2022).
Croft, T. N. et al. Guide to DHS Statistics 645 (Rockv ICF, 2018).
Hesketh, S. R. & Skrondal, A. Multilevel and Longitudinal Modeling using Stata (STATA press, 2021).
Goldstein, H. Multilevel Statistical Models Vol. 922 (Wiley, 2011).
Ahmed, F., Prendiville, N. & Narayan, A. Micronutrient deficiencies among children and women in Bangladesh: Progress and challenges. J. Nutr. Sci. 5, e46 (2016).
Arimond, M. & Ruel, M. T. Dietary diversity is associated with child nutritional status: Evidence from 11 demographic and health surveys. J. Nutr. 134(10), 2579–2585 (2004).
Gewa, C. A. & Leslie, T. F. Distribution and determinants of young child feeding practices in the East African region: Demographic health survey data analysis from 2008–2011. J. Health Popul. Nutr. 34(1), 6 (2015).
Baek, Y. & Chitekwe, S. Sociodemographic factors associated with inadequate food group consumption and dietary diversity among infants and young children in Nepal. PLoS One 14(3), e0213610 (2019).
Novaković, R. et al. Review article socio-economic determinants of micronutrient intake and status in Europe: A systematic review. Public Health Nutr. 17(5), 1031–1045 (2014).
Serra-Majem, L. et al. Determinants of nutrient intake among children and adolescents: Results from the enKid study. Ann. Nutr. Metab. 46(1), 31–38 (2002).
Akalu, Y. et al. Iron-rich food consumption and associated factors among children aged 6–23 months in sub-Saharan Africa: A multilevel analysis of demographic and health surveys. PLoS One 16(6), e0253221 (2021).
Na, M., Aguayo, V. M., Arimond, M. & Stewart, C. P. Risk factors of poor complementary feeding practices in Pakistani children aged 6–23 months: A multilevel analysis of the demographic and health survey 2012–2013. Matern. Child Nutr. 13(S2), e12463 (2017).
Magallanes, J. M. Human nutrition: The impact of family size and income on dietary intake. Philipp. Soc. Rev. 32(1/4), 69–79 (1984).
Zuercher, J. L., Wagstaff, D. A. & Kranz, S. Associations of food group and nutrient intake, diet quality, and meal sizes between adults and children in the same household: A cross-sectional analysis of U.S. households. Nutr. J. 10(1), 131 (2011).
Baek, Y. J., Paik, H. Y. & Shim, J. E. Association between family structure and food group intake in children. Nutr. Res. Pract. 8(4), 463–468 (2014).
Mayén, A. L., Marques-Vidal, P., Paccaud, F., Bovet, P. & Stringhini, S. Socioeconomic determinants of dietary patterns in low- and middle-income countries: A systematic review. Am. J. Clin. Nutr. 100(6), 1520–1531 (2014).
Tassew, A. A., Tekle, D. Y., Belachew, A. B. & Adhena, B. M. Factors affecting feeding 6–23 months age children according to minimum acceptable diet in Ethiopia: A multilevel analysis of the Ethiopian Demographic Health Survey. PLoS One 14(2), e0203098 (2019).
Novaković, R. et al. Micronutrient intake and status in Central and Eastern Europe compared with other European countries, results from the EURRECA network. Public Health Nutr. 16(5), 824–840 (2013).
Acknowledgements
The authors extend our deepest thanks to the Demographic and Health Survey (DHS) data archivist that allows accessing the dataset.
Author information
Authors and Affiliations
Contributions
M.T.E. and S.A.T. were involved in this study from the data acquisition, inception to design, data cleaning, data analysis, and interpretation and drafting and revising of the manuscript. A.D.G., D.T., Y.F., B.K., A.T.W. and M.T. were involved in the interpretation and revising of the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Engidaw, M.T., Gebremariam, A.D., Tiruneh, S.A. et al. Micronutrient intake status and associated factors in children aged 6–23 months in sub-Saharan Africa. Sci Rep 13, 10179 (2023). https://doi.org/10.1038/s41598-023-36497-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-36497-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.