Abstract
Left ventricular diameter (LVEDD) increases with systematic endurance training but also in various cardiac diseases. High exercise capacity associates with favorable outcomes. We hypothesized that peak work rate (Wpeak) indexed to LVEDD would carry prognostic information and aimed to evaluate the association between Wpeak/LVEDDrest and cardiovascular mortality. Wpeak/LVEDDrest (W/mm) was calculated in patients with an echocardiographic examination within 3 months of a maximal cycle ergometer exercise test. Low Wpeak/LVEDDrest was defined as a value below the sex- and age-specific 5th percentile among lower-risk subjects. The association with cardiovascular mortality was evaluated using Cox regression. In total, 3083 patients were included (8.0 [5.4–11.1] years of follow-up, 249 (8%) cardiovascular deaths). Wpeak/LVEDDrest (W/mm) was associated with cardiovascular mortality (adjusted hazard ratio (HR) 0.28 [0.22–0.36]), similar to Wpeak in % of predicted, with identical prognostic strength when adjusted for age and sex (C-statistics 0.87 for both). A combination of low Wpeak/LVEDDrest and low Wpeak was associated with a particularly poor prognosis (adjusted HR 6.4 [4.0–10.3]). Wpeak/LVEDDrest was associated with cardiovascular mortality but did not provide incremental prognostic value to Wpeak alone. The combination of a low Wpeak/LVEDDrest and low Wpeak was associated with a particularly poor prognosis.
Similar content being viewed by others
Introduction
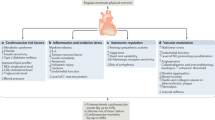
The left ventricle (LV) has adaptive properties in response to external demands, both in athletes and healthy individuals who develop increased LV dimensions as their exercise capacity and total heart volume increases1,2,3,4. However, LV dimensions may also increase due to cardiac disease (such as myocardial infarction, dilated cardiomyopathy and aortic or mitral regurgitation)5.
Peak oxygen consumption (peak VO2) measured during cardiopulmonary exercise testing (CPET) has been shown to be strongly related to cardiac dimensions6,7,8,9. In healthy individuals, larger cardiac dimensions are thus expected with higher peak VO2, or vice versa10,11. The absence of such a relation, i.e. increased cardiac dimensions but low peak VO2, is instead suggestive of cardiac disease, e.g. with left ventricular (LV) dilatation as an adaptation to pathological conditions2. Prior studies on the relation between cardiac dimensions and exercise capacity has been performed with CPET, i.e. with breathing gas analysis, cardiovascular magnetic resonance imaging/or echocardiography2,6. Given the strong relation between peak VO2 and peak work rate (Wpeak), cycle ergometer exercise testing could be used as a surrogate for CPET, offering a more widely available method for assessment of this relation12. No prior study has addressed the potential prognostic value of an abnormal relationship between Wpeak and LV size.
Measures of exercise capacity are strongly associated with cardiovascular (CV) morbidity and mortality, both in patients with established CV disease and in those without13,14,15,16,17,18,19,20,21. We hypothesized that by combining the prognostic information of exercise capacity and LV dimensions, by indexing Wpeak to LV end-diastolic diameter (LVEDD), a stronger association with CV mortality would emerge, compared to that for Wpeak alone, in particular in patients who are affected by both a low Wpeak and a large LVEDD. The aim of the current study was to evaluate if Wpeak/LVEDDrest predicted CV mortality better than Wpeak only.
Methods
We performed a retrospective analysis of consecutive patients aged 18 years or older who were referred for a clinical cycle ergometer exercise test at the department of Clinical Physiology at Kalmar County Hospital, Sweden between 31 May 2005 and 31 Oct 2016. The exercise stress test database has been described in detail elsewhere, and forms the basis for the Swedish national recommendations for grading of exercise capacity during standardized exercise stress testing13,22,23,24,25. Within this database, patients who had performed an echocardiographic examination within 3 months from the date of the exercise stress test were included. Patients who did not reach a peak rating of perceived exertion (RPE) of 17/20, and patients with missing data on Wpeak or LVEDDrest were excluded. A flowchart of patient inclusion and exclusion is presented in Fig. 1.
To obtain survival status for each subject until study census date, the database was cross-linked with the mandatory Swedish Causes of Death Register (until 31 Dec 2019). Data on comorbidities, medications and hospital admission data were obtained through cross-linkage with the mandatory Swedish National Patient Register (until 31 Dec 2019)26. Definitions and diagnosis codes (International Classification of Diseases-10 (ICD-10)) are presented in Supplements (Table A). CV death was defined as death with an underlying cause within the ICD-10 chapter of CV disease (IX).
Exercise testing
Exercise testing was performed using a standardized protocol on an electrically braked computer-controlled, regularly calibrated cycle ergometer (Rodby Inc, Karlskoga, Sweden). A 12-lead electrocardiogram was recorded during rest, exercise and recovery. Systolic blood pressure was measured in the supine position before and after exercise, seated on the bicycle before exercise, and every 2 min during exercise. RPE was reported every 2 min during exercise. Work rate was started at 40–100 W (men) or 30–50W (women), depending on the expected exercise capacity, with an incremental increase of 10–20 W/min27. Patients were encouraged to exercise until exhaustion. The test was terminated at the patient’s will or if predefined termination criteria were fulfilled (severe chest pain, ST depression ≥ 0.4 mV, decreasing systolic blood pressure or any malignant dysrhythmia). In order to take the effect of different work load increments on the achieved absolute Wpeak, into account, the achieved Wpeak was re-calculated, if necessary, to a standard protocol with an increment of 15 W/min (men) and 10 W/min (women) by the following formula28: females: Wpeak × (incremental workload used/10)1/6); males: Wpeak × (incremental workload used/15)1/6. The re-calculated exercise capacity was then related to the Swedish reference material for standardized exercise stress testing (% of predicted Wpeak, which is adjusted for age, gender and height)25. ST-segment amplitudes were measured 60 ms following the J-point (ST60). Significant ST depression was defined as horizontal or down-sloping ST depression ≥ 0.1 mV in V5 during exercise or during the recovery phase. Heart rate recovery was defined as the difference in heart rate between the maximal heart rate and the heart rate 2 min after cessation of exercise15,29. If a patient had performed more than one test, only the most recent test was included.
Echocardiography
Two-dimensional transthoracic resting echocardiography was performed using commercially available echocardiographic equipment. At end-diastole, LVEDDrest (mm), septal and posterior wall thickness (IVS and PWT, mm) were obtained either from M-mode or 2D images in the parasternal long axis view. LV mass was calculated according to the Cube formula (LV mass (g) = 0.8 × 1.04 ([IVS + LVEDD + PWT]3 − LVEDD3) + 0.6) and presented after adjustment to body-surface (BSA)30. Left ventricular ejection fraction (LVEF) was reported either based on the Simpson biplane method, from M-mode data (Teichholtz formula), or by visual estimation31.
Aortic, mitral or tricuspid regurgitation were graded as none, mild, moderate or severe. Moderate aortic stenosis was defined as either an aortic valve (AV) maximal velocity by continuous Doppler ≥ 3.1–4.0 m/s or an AV mean gradient of 20–40 mm Hg, while severe aortic stenosis corresponded to an AV maximal velocity ≥ 4.0 m/s or an AV mean gradient ≥ 40 mm Hg. Early (E) and late (A) diastolic velocity over the mitral valve were measured using pulsed Doppler and the E/A ratio was calculated. Pulsed tissue Doppler imaging with a 2-mm sample volume placed in the myocardium at the septal and lateral mitral annulus (apical four-chamber view) was used to determine the average early diastolic myocardial velocity (e’), in order to calculate the E/e’ ratio. Wpeak/LVEDDrest (W/mm) was calculated as the peak work rate at exercise stress testing divided by the end-diastolic LV diameter during resting echocardiography.
Statistical analysis
Continuous variables were described using mean and standard deviation (SD). Comparisons of group means were performed using Student’s t test. Differences between groups were assessed using the χ2 test. The correlation between Wpeak and LVEDD was analyzed using Pearson’s r and visualized using scatter plots, separately for all patients, lower-risk subjects, patients with moderate/severe left-sided valvular regurgitation, and for patients with heart failure.
The association between Wpeak/LVEDDrest and CV mortality, and the association between Wpeak in % of predicted, was analyzed using Cox proportional hazard regression models. Models were evaluated unadjusted; adjusted for age and sex; and adjusted for age, sex, peak systolic blood pressure, presence of ST depression, heart rate recovery, peak heart rate, LVEF, E/e’, heart failure, hypertension, previous myocardial infarction, diabetes mellitus, hyperlipidemia, and peripheral arterial disease. The choice of confounding variables was based on directed acyclic graphs and previous literature knowledge. The assumption of proportional hazards was confirmed using Schoenfeld’s residuals. Results are presented as hazard ratios (HR) with 95% confidence intervals (CI) and C statistics for the continuous Wpeak/LVEDDrest and Wpeak.
We also present HR for combinations of low/normal (Wpeak/LVEDDrest and low/normal Wpeak). Since no reference values for Wpeak/LVEDDrest exist, an approximate age- and sex-specific lower limit of normal (LLN) for Wpeak/LVEDDrest was defined among a subgroup of lower-risk subjects in this cohort, including only non-obese (BMI < 30 kg/m2) subjects with normal LVEF (≥ 55%), absence of moderate/severe valvular heart disease, without CV medications or known CV, renal, respiratory, or malignant disease. A low Wpeak was defined as Wpeak in % of predicted below the LLN according to the validated, Swedish reference material for exercise capacity13,25.
Natural cubic spline modelling was used to characterize the risk associated with Wpeak/LVEDDrest and Wpeak as a continuum, using four knots placed at the 5th, 25th, 75th and 95th percentiles.
Statistical significance was defined as a two-tailed p-value < 0.05. Statistical analysis was performed using R v. 3.5.3 (R Core Team (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria (https://www.R-project.org/), example packages: Survival v. 3.1-12rms v. 6.3.0).
Ethical approval
The study complies with the Declaration of Helsinki and was approved by the Swedish Ethical Review Authority (Dnr 2012/379-31; 2018/141-31 and 2020/00352). Informed consent was waived by the Swedish Ethical Review Authority.
Permissions
The manuscript does not contain any reproduced material from other sources.
Results
A total of 3083 patients (mean age 60 ± 16 years, 55% male) were included. During a median follow-up of 8.0 [IQR 5.4–11.1] years, 592 (19%) patients died of whom 249 (8%) died due to a CV cause. Baseline characteristics are presented in Table 1. An echocardiographic examination was performed within 0 [0–1] days from the exercise stress test.
The mean Wpeak/LVEDDrest was 3.1 ± 1.2 W/mm in the whole study group. Males had higher Wpeak/LVEDDrest compared to females (3.6 ± 1.2 W/mm vs. 2.6 ± 0.8 W/mm, p < 0.001). Wpeak/LVEDDrest was lower in older age groups among both sexes (Supplemental Fig. A).
Mean Wpeak/LVEDDrest in HF patients was 2.6 ± 1.1 W/mm, 2.6 ± 0.9 W/mm in patients with at least moderate mitral or aortic regurgitation, and 3.3 ± 1.1 W/mm in patients with neither HF nor mitral or aortic regurgitation (p < 0.001 for both comparisons).
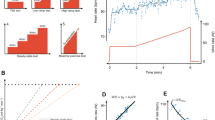
A total of 460 patients (15%) met the definition as lower-risk subjects. Among these, Wpeak was moderately correlated with LVEDDrest (r = 0.61, p < 0.001) (Fig. 2), while there was no clinically significant correlation between Wpeak and LVEDDrest among patients with HF or valvular heart disease (r = 0.06, p = 0.31 and r = 0.22, p < 0.001 respectively). A low Wpeak/LVEDDrest, defined as less than age- and sex specific 5th percentile of the lower-risk subgroup (Table 2), was found in 1,362 patients (44.2%). Compared to subjects with Wpeak/LVEDDrest above this threshold, patients with a low Wpeak/LVEDDrest had a higher prevalence of low LVEF < 50% (14.2% vs. 3.5%, p < 0.001), while they had greater E/e’ and LV mass (12 vs. 9, p < 0.001; 109 g/m2 vs. 92 g/m2, p < 0.001 respectively), Table 1.
The relation between peak work rate and left ventricular size in all subjects (n = 3083) (upper left panel, red), in low-risk patients (n = 460) (upper right panel, blue), patients with at least moderate mitral or aortic regurgitation (n = 346) (lower left panel, orange), and in heart failure patients (n = 309) (lower right panel, purple).
Higher Wpeak/LVEDDrest was associated with reduced CV mortality (unadjusted HR: 0.26 [0.22–0.31] per 1 W/mm), Table 3, Fig. 4. C-statistics were numerically higher for Wpeak/LVEDDrest than for Wpeak in % of predicted (0.80 [0.78–0.82] vs. 0.78 [0.75–0.81], p = 0.15). C-statistics were identical after adjusting for age and sex (C-statistics 0.87 [0.85–0.89] in both). Indexing Wpeak to LVEDD/body surface area did not improve its performance (C-statistic 0.76 [0.73–0.79]).
The relative risk of CV mortality increased exponentially with lower Wpeak/LVEDDrest, as well as with lower Wpeak, Fig. 3. The combination of low Wpeak/LVEDDrest and a low Wpeak was associated with a particularly poor prognosis (adjusted HR 6.4 [4.0–10.3]) in reference to patients with normal Wpeak/LVEDDrest and normal Wpeak), Fig. 4. In reference to those with a low Wpeak/LVEDDrest but a normal Wpeak, the risk was three folded increased for those with both low Wpeak/LVEDDrest and low Wpeak (HR 3.1 [2.0–4.6]. Results for all-cause mortality are presented in Supplements (Table B, Figures A and B).
Impact of decreasing Wpeak/LVEDDrest and Wpeak alone on the risk of cardiovascular death. The hazard ratios (95% confidence intervals) were calculated using Cox regression and modelled with natural cubic splines with four knots (percentiles: 5th, 25th, 75th, 95th) and presented as unadjusted estimates (left panels) and adjusted for age and sex (right panels). Wpeak/LVEDDrest showed a substantial risk increase with low values both for adjusted and unadjusted estimates.
Time-to-event analysis for the combination normal/low Wpeak/LVEDDrest and normal/low Wpeak 3083 patients experiencing 249 events (cardiovascular death) over a median of 8.0 [IQR: 5.5, 11.1] years. A low Wpeak/LVEDDrest as well as a low Wpeak was defined as a value below the sex- and age-specific 5th percentile of lower-risk subjects.
Discussion
In a large consecutive cohort of patients undergoing clinical cycle ergometer exercise testing and an echocardiogram within 3 months, Wpeak/LVEDDrest was a strong predictor of CV mortality, similar to Wpeak in % of predicted, with identical prognostic strength when adjusted for age and sex.
We hypothesized that patients with a low exercise capacity and an enlarged LV would be at higher risk of cardiovascular death than patients with a low exercise capacity but a normally sized LV. While we did not find Wpeak/LVEDDrest to provide incremental value to Wpeak alone, we found that a low Wpeak/LVEDDrest in combination with a low Wpeak was associated with a particularly poor prognosis. A combination of a low Wpeak/LVEDDrest and a low Wpeak increased the risk of cardiovascular death by more than 600% (adjusted HR 6.4 [4.0–10.3])), in reference to those with normal Wpeak/LVEDDrest and a low Wpeak. The risk of cardiovascular death increased exponentially with lower Wpeak/LVEDDrest. Therefore, it is possible that the Wpeak/LVEDDrest could have a potential value in risk stratification of patients with heart failure in settings where more advanced markers for risk assessment are unavailable, e.g. cardiovascular magnetic resonance imaging or cardiopulmonary exercise stress testing with breathing-gas analysis33,34.
When describing the relation between exercise capacity and LV size, neither Wpeak nor LVEDD were indexed to body size or age. When determining whether exercise capacity is reduced or not, Wpeak should be related to anthropometric data (including sex and age)13,18. Reference values for exercise capacity using standardized cycle ergometer exercise test in Sweden has been published, in which age, sex and height, but not weight, are included in the regression equation25. In this study, we aimed to test the hypothesis that if exercise capacity was not increased in parallel to cardiac dimensions, the risk of cardiovascular death would increase. Since both exercise capacity and LVEDD are expected to be higher in larger individuals, this hypothesis does not require for any of the measures to be adjusted to body size. Previous studies have applied a similar strategy, i.e. assessing absolute values for peak VO2 and total heart volume or left ventricular dimension instead of indexing to body size2,35.
Wpeak correlated with LVEDDrest in the subgroup of lower-risk subjects, similar to previous reports in healthy subjects1,3,4,36. It has been shown previously that intensive endurance training leads to an increase in LV-volume in healthy subjects, as a cardiac morphological adaptation4, and Meyer et al. showed that patients with a low peak work rate tended to have smaller left ventricles. Our study showed no meaningful correlation between LV size and peak work rate in patients with HF or valvular heart disease. This is not unexpected since the underlying cause of LV remodeling in response to endurance training is different than, for example, after myocardial infarction or with valvular heart disease. In contrast, among lower risk subjects, the association between LV size and Wpeak was stronger. In that way, an LV dilatation which is disproportionate to Wpeak is a sign of LV disease, in our study represented by a low Wpeak/LVEDDrest2. Although this could not be elucidated in the present study, the potential role of Wpeak/LVEDDrest in the discrimination of LV remodeling in response to exercise, i.e. athlete’s heart, and cardiac disease could warrant future studies.
Limitations
Firstly, as we included patients with a clinical referral to exercise stress testing and echocardiography, there is a selection bias, limiting broad generalization of our findings. Secondly, LV volumes were not available, and may have provided better assessment of LV dilatation than LVEDD. It is also possible that including measures of both ventricles and atria may be a better way to index the peak work rate to cardiac size, since physiological cardiac adaptation generally affects all four cardiac chambers2.
Thirdly, echocardiographic data were obtained from clinical records and not by a standardized, study-specific protocol.
Since this is a retrospective analysis, we have no data on reproducibility of the LVEDD values.
Conclusions
Wpeak/LVEDDrest was associated with cardiovascular mortality but did not provide incremental prognostic value to Wpeak alone. However, the combination of having a low Wpeak/LVEDDrest and low Wpeak was associated with a particularly poor prognosis.
Data availability
The data that support the findings of this study are available upon reasonable request to the corresponding author.
References
Nixon, J. V., Wright, A. R., Porter, T. R., Roy, V. & Arrowood, J. A. Effects of exercise on left ventricular diastolic performance in trained athletes. Am. J. Cardiol. 68, 945–949. https://doi.org/10.1016/0002-9149(91)90414-g (1991).
Engblom, H. et al. Peak oxygen uptake in relation to total heart volume discriminates heart failure patients from healthy volunteers and athletes. J Cardiovasc Magn Reson 12, 74. https://doi.org/10.1186/1532-429x-12-74 (2010).
Meyer, M., McEntee, R. K., Nyotowidjojo, I., Chu, G. & LeWinter, M. M. Relationship of exercise capacity and left ventricular dimensions in patients with a normal ejection fraction: An exploratory study. PLoS ONE 10, e0119432. https://doi.org/10.1371/journal.pone.0119432 (2015).
Arbab-Zadeh, A. et al. Cardiac remodeling in response to 1 year of intensive endurance training. Circulation 130, 2152–2161. https://doi.org/10.1161/circulationaha.114.010775 (2014).
Gaasch, W. H. & Zile, M. R. Left ventricular structural remodeling in health and disease: With special emphasis on volume, mass, and geometry. J. Am. Coll. Cardiol. 58, 1733–1740. https://doi.org/10.1016/j.jacc.2011.07.022 (2011).
Steding, K. et al. Relation between cardiac dimensions and peak oxygen uptake. J. Cardiovasc. Magn. Reson. 12, 8. https://doi.org/10.1186/1532-429x-12-8 (2010).
Saltin, B. & Calbet, J. A. Point: in health and in a normoxic environment, VO2 max is limited primarily by cardiac output and locomotor muscle blood flow. J. Appl. Physiol. (Bethesda, MD) 100, 744–745. https://doi.org/10.1152/japplphysiol.01395.2005 (2006).
Hammond, H. K., White, F. C., Bhargava, V. & Shabetai, R. Heart size and maximal cardiac output are limited by the pericardium. Am. J. Physiol. 263, H1675-1681. https://doi.org/10.1152/ajpheart.1992.263.6.H1675 (1992).
Stray-Gundersen, J. et al. The effect of pericardiectomy on maximal oxygen consumption and maximal cardiac output in untrained dogs. Circ. Res. 58, 523–530. https://doi.org/10.1161/01.res.58.4.523 (1986).
Solal, A. C., Chabernaud, J. M. & Gourgon, R. Comparison of oxygen uptake during bicycle exercise in patients with chronic heart failure and in normal subjects. J. Am. Coll. Cardiol. 16, 80–85. https://doi.org/10.1016/0735-1097(90)90460-7 (1990).
Arts, F. J. & Kuipers, H. The relation between power output, oxygen uptake and heart rate in male athletes. Int. J. Sports Med. 15, 228–231. https://doi.org/10.1055/s-2007-1021051 (1994).
Ren, C. et al. Comparison between treadmill and bicycle ergometer exercises in terms of safety of cardiopulmonary exercise testing in patients with coronary heart disease. Front Cardiovasc Med. 9, 864637. https://doi.org/10.3389/fcvm.2022.864637 (2022).
Lindow, T., Brudin, L., Elmberg, V. & Ekström, M. Long-term follow-up of patients undergoing standardized bicycle exercise stress testing: New recommendations for grading of exercise capacity are clinically relevant. Clin Physiol Funct Imaging 40, 83–90. https://doi.org/10.1111/cpf.12606 (2020).
Myers, J. et al. Exercise capacity and mortality among men referred for exercise testing. N. Engl. J. Med. 346, 793–801. https://doi.org/10.1056/NEJMoa011858 (2002).
Sipila, K. et al. Combination of low blood pressure response, low exercise capacity and slow heart rate recovery during an exercise test significantly increases mortality risk. Ann Med 51, 390–396. https://doi.org/10.1080/07853890.2019.1684550 (2019).
Bourque, J. M. & Beller, G. A. Value of exercise ECG for risk stratification in suspected or known CAD in the era of advanced imaging technologies. JACC Cardiovasc. Imaging 8, 1309–1321. https://doi.org/10.1016/j.jcmg.2015.09.006 (2015).
Snader, C. E. et al. Importance of estimated functional capacity as a predictor of all-cause mortality among patients referred for exercise thallium single-photon emission computed tomography: Report of 3400 patients from a single center. J Am Coll Cardiol 30, 641–648. https://doi.org/10.1016/s0735-1097(97)00217-9 (1997).
Yasui, Y. et al. Prognostic significance of peak workload-to-weight ratio by cardiopulmonary exercise testing in chronic heart failure. Am. J. Cardiol. 193, 37–43. https://doi.org/10.1016/j.amjcard.2023.01.052 (2023).
Hämäläinen, H. et al. Prognostic value of an exercise test one year after myocardial infarction. Ann. Med. 21, 447–453. https://doi.org/10.3109/07853898909149237 (1989).
Karlson, B. W., Sjölin, M., Lindqvist, J., Caidahl, K. & Herlitz, J. Ten-year mortality rate in relation to observations at a bicycle exercise test in patients with a suspected or confirmed ischemic event but no or only minor myocardial damage: Influence of subsequent revascularization. Am. Heart J. 141, 977–984. https://doi.org/10.1067/mhj.2001.115437 (2001).
Lindgren, M. et al. Cardiorespiratory fitness and muscle strength in late adolescence and long-term risk of early heart failure in Swedish men. Eur. J. Prev. Cardiol. 24, 876–884. https://doi.org/10.1177/2047487317689974 (2017).
Lindow, T., Brudin, L., Elmberg, V. & Ekstrom, M. Long-term follow-up of patients undergoing standardized bicycle exercise stress testing: New recommendations for grading of exercise capacity are clinically relevant. Clin Physiol Funct Imaging https://doi.org/10.1111/cpf.12606 (2019).
Lindow, T. et al. Typical angina during exercise stress testing improves the prediction of future acute coronary syndrome. Clin Physiol Funct Imaging 41, 281–291. https://doi.org/10.1111/cpf.12695 (2021).
Hedman, K., Lindow, T., Elmberg, V., Brudin, L. & Ekström, M. Age- and gender-specific upper limits and reference equations for workload-indexed systolic blood pressure response during bicycle ergometry. Eur. J. Prev. Cardiol. 2047487320909667, https://doi.org/10.1177/2047487320909667 (2020).
Brudin, L., Jorfeldt, L. & Pahlm, O. Comparison of two commonly used reference materials for exercise bicycle tests with a Swedish clinical database of patients with normal outcome. Clin Physiol Funct Imaging 34, 297–307. https://doi.org/10.1111/cpf.12097 (2014).
Brooke, H. L. et al. The Swedish cause of death register. Eur. J. Epidemiol. 32, 765–773. https://doi.org/10.1007/s10654-017-0316-1 (2017).
Jorfeldt, L. & Pahlm, O. Kliniska arbetsprov: Metoder för diagnos och prognos. 1. uppl. edn, (Studentlitteratur, 2013).
Wallin, L. & Brudin, L. H. Physical working capacity determined by different types of bicycle exercise tests. Clin Physiol 8, 529–537 (1988).
Cole, C. R., Blackstone, E. H., Pashkow, F. J., Snader, C. E. & Lauer, M. S. Heart-rate recovery immediately after exercise as a predictor of mortality. N. Engl. J. Med. 341, 1351–1357. https://doi.org/10.1056/nejm199910283411804 (1999).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 16, 233–270. https://doi.org/10.1093/ehjci/jev014 (2015).
Baumgartner, H. et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 38, 2739–2791. https://doi.org/10.1093/eurheartj/ehx391 (2017).
Marwick, T. H. Ejection fraction pros and cons: JACC state-of-the-art review. J. Am. Coll. Cardiol. 72, 2360–2379. https://doi.org/10.1016/j.jacc.2018.08.2162 (2018).
Guazzi, M. et al. 2016 focused update: Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Eur. Heart J. 39, 1144–1161. https://doi.org/10.1093/eurheartj/ehw180 (2018).
van Woerden, G. et al. The clinical and prognostic value of late Gadolinium enhancement imaging in heart failure with mid-range and preserved ejection fraction. Heart Vessels 37, 273–281. https://doi.org/10.1007/s00380-021-01910-2 (2022).
Letnes, J. M. et al. Indexing cardiac volumes for peak oxygen uptake to improve differentiation of physiological and pathological remodeling: from elite athletes to heart failure patients. Eur. Heart J. Cardiovasc. Imag. https://doi.org/10.1093/ehjci/jead034 (2023).
Nambiar, L., Li, A., Howard, A., LeWinter, M. & Meyer, M. Left ventricular end-diastolic volume predicts exercise capacity in patients with a normal ejection fraction. Clin. Cardiol. 41, 628–633. https://doi.org/10.1002/clc.22928 (2018).
Spin, J. M. et al. The prognostic value of exercise testing in elderly men. Am J Med 112, 453–459. https://doi.org/10.1016/s0002-9343(02)01065-3 (2002).
Leeper, N. J. et al. Exercise capacity is the strongest predictor of mortality in patients with peripheral arterial disease. J. Vasc. Surg. 57, 728–733. https://doi.org/10.1016/j.jvs.2012.07.051 (2013).
Al Saadi, T. et al. Coenzyme Q10 for heart failure.
Bourque, J. M., Holland, B. H., Watson, D. D. & Beller, G. A. Achieving an exercise workload of > or = 10 metabolic equivalents predicts a very low risk of inducible ischemia: Does myocardial perfusion imaging have a role?. J Am Coll Cardiol 54, 538–545. https://doi.org/10.1016/j.jacc.2009.04.042 (2009).
Gulati, M. et al. Exercise capacity and the risk of death in women: The St James Women Take Heart Project. Circulation 108, 1554–1559. https://doi.org/10.1161/01.cir.0000091080.57509.e9 (2003).
Funding
Open access funding provided by Lund University. CEG and TL received funding’s from the Department of Research and Development, Region Kronoberg, Sweden; ME was supported by an unrestricted grant from the Swedish Research Council (Dnr: 2019-02081).
Author information
Authors and Affiliations
Contributions
C.E.G. performed the data analysis, prepared the figures and wrote the initial manuscript draft. M.E., M.U., L.B., A.C., K.H. and T.L. contributed substantially to the study design, data analysis and interpretation, and the writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Eklund Gustafsson, C., Ekström, M., Ugander, M. et al. Prognostic value of peak work rate indexed by left ventricular diameter. Sci Rep 13, 8806 (2023). https://doi.org/10.1038/s41598-023-35976-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-35976-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.