Abstract
Postmenopausal status is a risk factor for distal sensory polyneuropathy—the most common type of peripheral neuropathy. We aimed to investigate associations between reproductive factors and history of exogenous hormone use with distal sensory polyneuropathy among postmenopausal women in the United States using data from the National Health and Nutrition Examination Survey 1999–2004, and to explore the modifying effects of ethnicity on these associations. We conducted a cross-sectional study among postmenopausal women aged ≥ 40 years. Women with a history of diabetes, stroke, cancer, cardiovascular disease, thyroid disease, liver disease, weak or failing kidneys, or amputation were excluded. Distal sensory polyneuropathy was measured using a 10-g monofilament test, and a questionnaire was used to collect data on reproductive history. Multivariable survey logistic regression was used to test the association between reproductive history variables and distal sensory polyneuropathy. In total, 1144 postmenopausal women aged ≥ 40 years were included. The adjusted odds ratios were 8.13 [95% confidence interval (CI) 1.24–53.28] and 3.18 (95% CI 1.32–7.68) for age at menarche < 11 years and time since menopause > 20 years, respectively, which were positively associated with distal sensory polyneuropathy; adjusted odds ratios were 0.45 for the history of breastfeeding (95% CI 0.21–0.99) and 0.41 for exogenous hormone use (95% CI 0.19–0.87) were negatively associated. Subgroup analysis revealed ethnicity-based heterogeneity in these associations. Age at menarche, time since menopause, breastfeeding, and exogenous hormone use were associated with distal sensory polyneuropathy. Ethnicity significantly modified these associations.
Similar content being viewed by others
Introduction
Distal sensory polyneuropathy (DSP) is a neurological disorder that is commonly encountered by family physicians and neurologists. It is characterized by symmetric distal foot or toe numbness, tingling, with/without neuropathic pain, or loss of sensation1. Some patients may only experience mild paresthesia or negative symptoms; however, it is challenging to reverse established neuropathy2. Moreover, ignoring these signs could eventually put patients at risk for various diseases or may be life-threatening3. Approximately 28% of American adults with diabetes suffer from DSP, which accounts for approximately $10.91 billion in healthcare expenditure in the United States (US)4,5,6. Among the non-diabetic population, prediabetes and metabolic syndrome components, such as obesity and hypertension, have been reported as common causes of cryptogenic sensory peripheral neuropathy2. In addition, cytostatic drugs, nutritional deficiency, alcoholism, smoking, and cardiovascular disease could also result in DSP7,8,9. Nevertheless, sometimes the neurologist is unable confirm the particular cause despite careful history and exclusive assessment10. Approximately 5–8 million Americans are affected by idiopathic (unknown cause) peripheral neuropathy10.
Several studies reported that women exhibited a 1.5 to twofold greater risk of DSP than men9. The sex differences in the prevalence of peripheral neuropathy may be due to women's longer lifespan and the reduced estrogen levels following menstrual transition among postmenopausal women11,12,13. The prevalence of DSP among Egyptian women was reported to peak in the 45–54 age group14. Women undergo menopause around this age, ending their reproductive phase15. Postmenopausal status has consistently been a risk factor for polyneuropathy in non-diabetic obese individuals16. Peripheral neuropathy always coexists with central nervous system diseases17,18. The widely fluctuating hormone levels during each reproductive stage and the cumulative lifetime estrogen exposure have a substantial impact on women’s central nervous system later in life13. Moreover, aging nerves are sensitive to exogenous estrogen in animal studies19,20. Nevertheless, there are no reports in the literature regarding whether reproductive factors and a history of exogenous hormone use are associated with the prevalence of peripheral neuropathy among postmenopausal women.
This cross-sectional study was designed to explore the associations between DSP and reproductive history factors, including age at menarche, pregnancy, breastfeeding, age at menopause, total reproductive lifespan, time since menopause, and history of exogenous hormone use among non-diabetic postmenopausal women using publicly published data from the National Health and Nutrition Examination Survey (NHANES) 1999–2004. As the prevalence of PN was reported to be different by racial/ethnic groups21, we also explored the modifying effect of ethnicity of these associations.
Materials and methods
Study participants
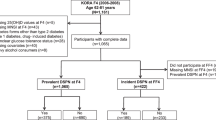
We extracted the data of postmenopausal women aged ≥ 40 years from the NHANES 1999–200422. Women with self-reported medical history of diabetes, stroke, cancer, cardiovascular disease, thyroid disease, liver disease, and weak/failing kidneys were excluded, because these diseases are common causes of peripheral neuropathy3. Women with amputation or insufficient information regarding their eligibility and outcome were also excluded. Finally, 1144 eligible postmenopausal women were included in the study (Fig. 1). Our study followed the reporting guidelines of the RECORD statement23.
The protocols of NHANES were approved by the Institutional Review Board of the Centers for Disease Control and Prevention, and all participants provided informed consent. We downloaded, generated, and cleaned the data from different NHANES cycles to build a dataset for this study. Our study was exempted by the Institutional Review Board of the Faculty of Medicine, Chulalongkorn University (No. 0422/65). All research was performed in accordance with the Declaration of Helsinki. Data from NHANES could be downloaded online. The datasets generated and analyzed during the current study are available from the first author.
Outcomes
DSP was identified as possessing at least one insensate site on either foot by a 10-g monofilament test, a binary variable: DSP and non-DSP24. Participants were asked to lie on the exam table to undergo the sensation of the touch test. Well-trained technicians applied slight pressure to the plantar-first metatarsal head, plantar-fifth metatarsal head, and plantar-hallux of each participant’s foot, without sequential order. An insensate site was defined when participants were unable to respond correctly to the filament pressure. The total number of insensate areas ranged from zero to six for both feet. DSP was defined as ≥ 1 insensate area, which has been reported as a significant predictor for ulcers and amputation, with moderately high sensitivity (∼85%) and specificity (∼80%)25.
Exposure
Self-reported reproductive factors and history of exogenous hormone use were analyzed in this study. Age at menarche was defined as the first menstrual period (≤ 11 and > 11 years). Gravidity was defined as the total number of pregnancies, including current pregnancies, live births, miscarriages, stillbirths, tubal pregnancies, and abortions (< 4 or ≥ 4). Breastfeeding was defined as having ever breastfed by any of their children (never or ever). Postmenopausal status was defined as both ovaries removed (representing the surgical menopause) or having last period at 12 or more months ago with the reason of “going-gone through menopause (representing natural menopause). Age at menopause was defined as the age at the last menstrual period (< 45; 46–55; ≥ 56 years). The total reproductive lifespan was defined as the time from the onset of menarche to the onset of menopause (≤ 35 and > 35 years). Time since menopause was defined as the duration between the age at interview and the age at last menstrual period (≤ 20 and > 20 years). A history of exogenous hormone use was defined as the use of contraceptives, including birth control pills and contraceptive injection, or any type of menopause hormone therapy, including pills, cream, patches, and injectables (never or ever).
Covariates
The demographic characteristics included age (40–70 and > 70 years), ethnicity (Mexican American and other Hispanic as Hispanic, and Non-Hispanic White, Black and Others as Non-Hispanic), education (less than high school and high school or above), income (prescribed investor rate [PIR] ≤ 2.00 and > 2.00, the sample median cutoff value for PIR is 2), and insurance (covered and not covered). Health-related lifestyle variables included smoking (never or ever) and alcohol consumption (never or ever). Smoking was defined as smoking at least 100 cigarettes in life or being a current smoker at the time of interview. Alcohol use was defined as at least 12 drinks of any type of alcohol throughout life (one drink was 2 oz. beer, a 4 oz. glass of wine, or an ounce of liquor). Health condition-related variables, including hypertension and body mass index (BMI), were also evaluated. Hypertension (yes or no) was defined as the presence of at least one of the following conditions: an average systolic blood pressure ≥ 140 mmHg, an average diastolic blood pressure ≥ 90 mmHg, or self-reported current use of prescribed antihypertensive medication22. BMI was calculated as weight in kilograms divided by height in meters squared: underweight/normal (< 25 kg/m2) and overweight/obese (≥ 25 kg/m2)26.
Statistical analysis
The missing values for each variable in the final analysis are shown in Table 1. Codebook of each variable could be found from Supplementary Table S1. We used the complete case analysis after data management and cleansing. Proportions with 95% confidence interval (CI) and medians with interquartile ranges (Q1 and Q3) were reported for categorical and numerical data, respectively. Binary logistic regression was conducted to determine the association between reproductive factors and exogenous hormone use with DSP, using the purposeful selection of covariate strategy27,28. The significant interaction term of ethnicity and menarche (p = 0.03) was fitted into the final multivariable logistic regression model based on both clinical and statistical considerations. We investigated whether ethnicity modifies the association between reproductive factors and DSP using the final multivariable model in the primary analysis (except for ethnicity and the interaction term) for subgroup analysis. Multicollinearity and goodness-of-fit were evaluated for each model. The results are presented as odds ratios (ORs) with 95% confidence intervals (CIs). Statistical significance was set at a two-sided p-value < 0.05. Survey weights, clusters, and strata were considered to account for the complex survey design in all statistical analyses using Stata software version 15.1.
Ethics declarations
NHANES is a publicly released de-identified dataset. The protocols of NHANES were approved by the Institutional Review Board of the Centers for Disease Control and Prevention, and all participants provided informed consent. We downloaded, generated, and cleaned the data from different NHANES cycles to build a dataset for this study. Our study was exempted by the Institutional Review Board of the Faculty of Medicine, Chulalongkorn University (No. 0422/65). All research was performed in accordance with the Declaration of Helsinki.
Results
Participant characteristics
The characteristics of all participants are summarized as weighted prevalence estimates in Table 2. A total of 1144 participants were included in the final dataset: 390 individuals from 1999 to 2000, 387 from 2002 to 2003, and 367 from the 2003–2004 NHANES cycles. Of these, 89 (6.26%) patients were diagnosed with DSP. The median age (Q1, Q3) was 63 (55–73) years, and 798 (77.26%) were aged 40–70 years. The vast majority of participants were non-Hispanics (851/1144, 89.79%). Among all participants, 951 (81.90%) experienced their first menstrual period after 11 years of age, 516 (36.87%) had 4 or more pregnancies, and 573 (45.74%) breastfed their children. The age at menopause of participants aged < 45 years, 46–55 years, and ≥ 56 years were 37.12, 53.1, and 9.11%, respectively. Approximately one-third of the participants had their final menstrual period 20 years previously, and half of the participants had a total reproductive lifespan of ≤ 35 years. The number of exogenous hormone users was as high as 783, accounting for 76.77% of all participants, which was more than three times the number of women who had never used exogenous hormones.
Distal sensory polyneuropathy and associated factors
The sociodemographic characteristics, health-related lifestyles, medical conditions, and reproductive factors of all participants were compared between the DSP and non-DSP groups (Table 3). Compared to the non-DSP group, women with DSP were more likely to be older (p = 0.049), have a lower education level (p = 0. 013), longer time since menopause (p = 0.049), and less likely to use exogenous hormones (p = 0.031).
Association of reproductive factors and exogenous hormone with distal sensory polyneuropathy
Using a logistic regression model with purposeful selection of covariates, age, ethnicity, education, income status, BMI, age at menarche, breastfeeding history, time since menopause, and history of exogenous hormone use were included in the preliminary main effects model (Model 1 in Table 3, n = 835). In the interaction assessment with the preliminary main effects model, the two-way interaction term of menarche with ethnicity made contributed significantly to the fit of the model (p for interaction = 0.027); therefore, we added this interaction term as a source for confounding into the final model (Model 2 in Table 3, n = 835). After adjusting for all confounding factors, postmenopausal women with age at menarche ≤ 11 years exhibited a 8.13-fold higher risk of DSP than those with age at menarche > 11 years (OR = 8.13, 95% CI 1.24, − 53.28; p = 0.030); postmenopausal women with breastfeeding history experienced a 55% reduction in the odds of having DSP compared to those who breastfed no children (OR = 0.45, 95% CI 0.21, − 0.99; p = 0.047); postmenopausal women with time since menopause > 20 years were 3.18 times more likely to have DSP than those with shorter durations since menopause (< 20 years) (OR = 3.18, 95% CI 1.32, − 7.68; p = 0.011); and exogenous hormone users exhibited a reduction of 59% in the odds of having DSP compared to non-users (OR = 0.41, 95% CI 0.19, − 0.87; p = 0.022). Gravidity (crude OR = 1.09, 95% CI 0.59, − 1.99; p = 0.270) and total reproductive lifespan (crude OR = 0.83, 95% CI 0.39, − 1.76; p = 0.626) were not associated with DSP and were therefore not included in the final model. The age at menopause was not included in the final model. Age at menopause ≥ 56 years was associated with DSP (crude OR = 2.49, 95% CI 1.10, − 5.64; p = 0.030), but age at menopause < 45 years was not associated with DSP (crude OR = 1.24, 95% CI 0.63, 2.45; p = 0.520).
Subgroup analysis by ethnicity
We conducted a subgroup analysis by ethnicity after finding the two-way interaction term of menarche with ethnicity in preliminary main effects model. According to the subgroup analysis, negative associations of older age at menarche (OR = 6.24, 95% CI 1.23, − 31.76; p = 0.028) and breastfeeding (OR = 0.22, 95% CI 0.06, − 0.84; p = 0.028) with DSP were observed among Hispanic women (n = 219). Among non-Hispanic women (n = 616), we found higher odds of DSP among women with time since menopause > 20 years (OR = 3.91, 95% CI 1.48, − 10.37; p = 0.007), and lower odds of DSP among exogenous hormone users (OR = 0.38, 95% CI 0.15, − 0.94; p = 0.036) (Table 4).
Discussion
In this cross-sectional study of US postmenopausal women aged ≥ 40 years (NHANES 1999–2004), we observed negative associations of age at menarche, breastfeeding, and exogenous hormone use with DSP, and a positive association of time since menopause with DSP, after adjusting for important confounding variables. However, our study did not identify an association between gravidity, age at menopause, and total reproductive lifespan and DSP. We observed ethnicity differences in the associations between DSP and age at menarche, breastfeeding, time since menopause, and history of exogenous hormone use.
Context in the literature
Age at menarche
Early menarche usually correlates with greater cumulative estrogen exposure among women and has been demonstrated to be a significant neuroprotective factor12,29. In contrast, we observed a higher risk of DSP among women with age at menarche ≤ 11 years. The negative effect of early menarche has been demonstrated in several health conditions, such as diabetes, metabolic syndrome, cardiovascular disease, and even mortality in previous studies30,31. The higher frequency of peripheral neuropathy in postmenopausal women with early menarche (≤ 11 years) may be explained by metabolic mechanisms. Women aged ≤ 11 years at menarche are more likely to have higher BMI or subcutaneous fat levels in childhood (5–9 years)32. Weight gain and increased fat may persist throughout adulthood among women with early menarche, which correlates with impaired insulin response, increased insulin resistance, and dyslipidemia, eventually resulting in a range of metabolic issues33,34,35. All these metabolic disorders resulting from early menarche might potentially increase the risk of DSP later in women’s lives36,37. The risk of metabolic syndrome decreases by 8% when age at menarche increases by one additional year38. Compared to women with late menarche (> 15 years), those with early menarche had a 1.62-fold higher risk of being affected by metabolic disorders38. In this study, we defined early menarche as age < 11 years and categorized all study participants into two groups. The effects of late menarche on DSP should be investigated in future studies. Future longitudinal studies should be conducted to observe menarche history, subcutaneous fat accumulation, BMI, insulin sensitivity, and the occurrence of DSP.
Gravidity
Estrogen levels increase suddenly and dramatically (up to 300-fold) during early pregnancy and peak in late pregnancy, and higher gravidity might reflect a longer duration of exposure to high levels of estrogen39. However, we did not observe an association between gravidity and DSP among postmenopausal women in the US aged ≥ 40 years. Previous studies demonstrated a higher risk of peripheral nerve disorders during pregnancy and the postpartum period. These peripheral neuropathies are primarily caused by compression or weight gain, and their symptoms are usually temporary and reversible40. Pregnancy also has a complicated influence on metabolism, promoting increased insulin resistance, hyperlipidemia, adipogenesis and fat accumulation41. Frequent pregnancies have permanent adverse effects on lipid and glucose metabolism42. Our finding of the association between gravidity and DSP might be attenuated by aging and estrogen deficiency that occurs with menopause (natural ovarian failure or removal of ovaries)43. Besides the complex biological mechanisms, demographic and lifestyle factors might influence the association between gravidity and DSP. Women with greater pregnancies might have a better health condition because of a healthier lifestyle, better nutrition, and more social or family support from the multiparous family size44,45,46. Current evidence regarding the effect of gravidity on peripheral nerve conditions in postmenopausal women is limited. In our study, the number of gravidities was counted according to all types of pregnancies, including current pregnancy, live births, miscarriages, stillbirths, tubal pregnancies, or abortions. Future studies should examine whether pregnancy outcomes (such as live births) or pregnancy complications are associated with peripheral nerve changes.
Breastfeeding
In our study, a lower risk of DSP was observed among postmenopausal women who breastfed their children. During breastfeeding, prolactin and oxytocin increase and become major driving hormones; however, estrogen and progesterone decrease rapidly47. Both prolactin and oxytocin are well-known neuroprotective factors that provide strong neuronal protection as neuropeptides by exerting anti-apoptotic, anti-inflammatory, and antioxidant properties48,49. Moreover, breastfeeding could help reverse the metabolic changes that occur during pregnancy, such as visceral fat and insulin resistance43,50. Several benefits of breastfeeding have been confirmed for maternal health, even in the absence of early, exclusive or continued breastfeeding51. Additionally, exclusive breastfeeding slows the return of ovulation after delivery and may slow depletion of the ovarian pool, which might consequently slow down reproductive aging52. Reproductive aging can influence the cellular, tissue, organ, and system aging of organisms53. Hence, reproductive and metabolism-related mechanisms may work together in providing the protective effect of breastfeeding on DSP. Future studies should examine the effects of breastfeeding duration on the peripheral nervous system.
Menopause
Menopause marks the end of the reproductive phase of a woman's life, following a reduction in estrogen levels54. Postmenopausal status increases the risk of peripheral nerve disorders in non-diabetic obese women16. The age at menopause, total reproductive lifespan, and time since menopause were considered in this study. Early menopause is associated with shorter reproductive lifespan and lower cumulative estrogen exposure in women. Natural menopause usually occurs between the ages of 45–55 years worldwide55. The most prevalent type of premature or early menopause is surgical menopause, which causes abrupt loss of estrogen and progesterone in women56. In women with early menopause, shorter estrogen exposure can negatively affect the function of pancreatic β-cells and induce insulin resistance, which has demonstrated a harmful effect on peripheral nerves57,58. Additionally, early and premature menopause are more prevalent in women with chronic inflammatory diseases. Persistent chronic inflammation can induce peripheral neuropathy by impairing the efficiency of nerve regeneration and influencing the microenvironment in the peripheral nervous system, which is characterized by chronic macrophage infiltration, increased cytokine expression, and pro-inflammatory gene expression59. The term "total reproductive lifespan" refers to the time between menarche and menopause, which has been a superior variable for indicating the duration of exposure to endogenous estrogen, by comparing the age at menarche and age at menopause13. However, no associations between age at menopause and total reproductive lifespan with DSP were observed in our study.
Several factors may contribute to the absence of associations between distal sensory neuropathy and age at menopause and total reproductive lifespan. First, exogenous hormone use may influence these associations60. Second, surgical and natural menopause have inconsistent effects on women's health outcomes56. Premature or early natural menopause is usually a gradual process. In contrast, surgical removal of both ovaries causes an abrupt loss of ovarian hormones, including estrogen, progesterone, and testosterone, as well as damage to the hypothalamus–pituitary–gonadal axis56. However, our study did not differentiate between natural and surgical menopause in this regard. The characteristics of the study population should be considered in detail in future studies when exploring the associations between age at menopause and total reproductive lifespan with DSP.
Time since menopause > 20 years was found to be an independent risk factor for DSP among postmenopausal women aged ≥ 40 years in our study. In contrast to age at menopause and total reproductive lifespan (correlates to exposure to endogenous estrogen during the premenopausal phase), time since menopause could be used as a marker of endogenous estrogen deficiency during the postmenopausal phase. A longer time since menopause impairs glucose tolerance among women, which could induce neuropathies, mostly on the small nerve fibers61,62. Previous studies have demonstrated that women at > 20 years since menopause are at a greater risk of metabolic syndrome, cardiovascular disease, and elevated blood pressure than those at < 10 years since menopause63. In addition, the longer time since menopause could accelerate biological aging compared to a shorter duration after menopause, which might also accelerate peripheral nerve impairment64.
Exogenous hormone use
In our study, exogenous hormones are referred to as menopausal hormone therapy or contraceptive use, including exogenous estrogen and progesterone, both of which are neuroprotective factors19,65. Although both estrogen and progesterone are well-known neuroprotective factors, there is currently limited research on whether a history of exogenous hormone use affects peripheral nerves. We found that exogenous hormone users experienced a lower risk of DSP among postmenopausal women aged ≥ 40 years. In previous animal studies, aging nerves remained sensitive to estrogen and progesterone19. Estrogen and progesterone can regulate the expression of nerve growth factors in the peripheral organs of ovariectomized female mice. Nerve growth factor is a neurotrophic factor known to play a key protective role in the development and survival of sympathetic, sensory, and forebrain cholinergic neurons19. The influence of exogenous hormones on postmenopausal female neurological systems is currently under investigation. These contradictory results might be related to differences in hormone formulation and use, characteristics of hormone users, and variety of nerve types66. The regimen, timing, and dose of the exogenous hormones should be considered in future studies.
Ethnicity differences
It is important to conduct the racial/ethnic difference studies for identifying and addressing health disparities, understanding the related root causes67. However, it also necessary to be cautious for the distinctions between race and ethnicity because they are complex and multifaceted constructs67. In our study, we collapsed Mexican American and other Hispanic as Hispanic, while Non-Hispanic White, Black and Others as Non-Hispanic, because the small sample size from each race group prevented us from analyzing this issue via subgroup analysis. Hispanics are the largest minority group in the United States, who are exposed to higher health risks68. Female Hispanics are a growing population group and are exposed to poor social and health circumstances68. In the subgroup analysis, the associations of age at menarche and breastfeeding with DSP were only observed in the Hispanic group. In the US, the average age at menarche was > 14 years before 1900, but decreased to 12.43 years in 1988–1994 and 11.9 years in 2013–201769,70,71. Mexican Americans, the majority of the US Hispanic population, had the fastest rate of decline in the age of menarche72. Obesity is a major health problem in Hispanics68. Overweight or obese women usually have more metabolic disorders and inflammation2,73. Therefore, the results of the subgroup analysis suggest that the effect of age at menarche and breastfeeding on peripheral nerves might be closely associated with metabolic and inflammatory issues.
We identified a significant positive association between the time since menopause and exogenous hormone use with DSP only in the non-Hispanic group. The association between the time since menopause and DSP might be explained by estrogen levels74. Estrogen levels in postmenopausal women reach their lowest point in the first 2 years after the final menstrual period54. Estrogen levels during the postmenopausal phase in non-Hispanic women are lower than those in Hispanics. Moreover, Hispanic women usually have the highest rates of obesity68. Adipocytes produce estrogens through aromatase activity, and obese women have higher levels of circulating estrogens than other women during the postmenopausal phase75. Hence, ethnicity differences in estrogen levels during the postmenopausal phase and obesity status might potentially lead to ethnicity heterogeneity in the association between time since menopause and DSP. In addition, Hispanics in the US are covered by fewer preventive health services than other ethnic groups68. This could be a potential explanation for the absence of an association between exogenous hormone use and DSP.
Strengths and limitations
This study has several strengths. First, we investigated the association between reproductive factors and DSP in postmenopausal women using nationally representative data. Second, we used logistic regression with a purposeful selection strategy to assess the association between exposure and outcome. This strategy allowed us to correctly identify and retain confounders at a higher rate than other selection algorithms. Our findings might provide a rationale for the occurrence and development of DSP in women. Finally, we identified that the effects of reproductive factors and exogenous hormone use on DSP were not constant by ethnicity.
Despite its strengths, this study has several limitations. First, the assessment of peripheral neuropathy was limited to the monofilament test which was the only available test in NHANES 1999–2004. Therefore, we cannot conclude whether our findings from a small number of events could be generalized among current postmenopausal women in the because NHANES 1999–2004 was conducted almost 20 years ago. Additonally, other objective examinations, such as nerve conduction studies or skin biopsies, were not available from the NHANES. Second, bias should be considered. Recall bias in assessing exposure may have existed among postmenopausal women in this study, especially among those of advanced age. A selection bias from excluding those with medical diseases may have led to an apparent association. Third, additional study participants’ characteristics based on blood tests were not provided in our study, because the sample size in the fasting subsample was small. Our study did not include blood cholesterol or other inflammatory biochemical markers as potential confounders, which may explain the underlying mechanisms of DSP. Diabetes was defined as a self-reported medical history through interviews. Therefore, non-diabetic status may be misclassified. Fourth, premature or early natural menopause is usually a gradual process, while surgical removal of both ovaries causes an abrupt loss of ovarian hormones. The natural menopause or surgical menopause should be distinguished in the future study. Fifth, this was a cross-sectional study, and only the prevalence of DSP was reported; therefore, a causal relationship could not be confirmed. Lastly, the study population included only postmenopausal women in the United States. Future studies should be conducted among participants in different countries and ethnic groups and ethnicity differences should be considered.
Conclusion
Age at menarche, time since menopause, breastfeeding, and exogenous hormone use were associated with DSP among postmenopausal US women aged ≥ 40 years. Ethnicity-based heterogeneity was also observed in these associations. Our findings may provide a rationale for the etiology of peripheral neuropathy among postmenopausal women in the United States. Reproductive factors may influence peripheral nerve health via both hormone- and metabolism-related pathways. Greater exposure to estrogen before menopause might not prevent peripheral neuropathy. In contrast, estrogen deficiency might be associated with biological aging to cause peripheral nerve damage in postmenopausal women. Therefore, promoting breastfeeding may reduce the burden of peripheral neuropathy in middle-aged postmenopausal women. Exogenous hormone use may help slow nerve damage or recover damaged nerves, and could potentially be used in the management of peripheral neuropathy. Further research is required to investigate the underlying mechanisms.
Data availability
Data from NHANES could be downloaded online. The datasets generated and analyzed during the current study are available from the first author.
References
Gorson, K. C. & Ropper, A. H. Additional causes for distal sensory polyneuropathy in diabetic patients. J. Neurol. Neurosurg. Psychiatry 77, 354–358. https://doi.org/10.1136/jnnp.2005.075119 (2006).
Stino, A. M. & Smith, A. G. Peripheral neuropathy in prediabetes and the metabolic syndrome. J. Diabetes Investig. 8, 646–655. https://doi.org/10.1111/jdi.12650 (2017).
Doughty, C. T. & Seyedsadjadi, R. Approach to peripheral neuropathy for the primary care clinician. Am. J. Med. 131, 1010–1016. https://doi.org/10.1016/j.amjmed.2017.12.042 (2018).
Pop-Busui, R. et al. Diabetic neuropathy: A position statement by the American diabetes association. Diabetes Care 40, 136–154. https://doi.org/10.2337/dc16-2042 (2017).
Gregg, E. W. et al. Prevalence of lower extremity diseases associated with normal glucose levels, impaired fasting glucose, and diabetes among U.S. adults aged 40 or older. Diabetes Res. Clin. Pract. 77, 485–488. https://doi.org/10.1016/j.diabres.2007.01.005 (2007).
Gordois, A., Scuffham, P., Shearer, A., Oglesby, A. & Tobian, J. A. The health care costs of diabetic peripheral neuropathy in the US. Diabetes Care 26, 1790–1795. https://doi.org/10.2337/diacare.26.6.1790 (2003).
Staff, N. P. & Windebank, A. J. Peripheral neuropathy due to vitamin deficiency, toxins, and medications. Continuum (Minneap Minn) 20, 1293–1306. https://doi.org/10.1212/01.CON.0000455880.06675.5a (2014).
England, J. D. et al. Practice parameter: Evaluation of distal symmetric polyneuropathy: Role of laboratory and genetic testing (an evidence-based review). Report of the American academy of neurology, American association of neuromuscular and electrodiagnostic medicine, and American academy of physical medicine and rehabilitation. Neurology 72, 185–192. https://doi.org/10.1212/01.wnl.0000336370.51010.a1 (2009).
Hanewinckel, R., van Oijen, M., Ikram, M. A. & van Doorn, P. A. The epidemiology and risk factors of chronic polyneuropathy. Eur. J. Epidemiol. 31, 5–20. https://doi.org/10.1007/s10654-015-0094-6 (2016).
Singer, M. A., Vernino, S. A. & Wolfe, G. I. Idiopathic neuropathy: New paradigms, new promise. J. Peripher. Nerv. Syst. 17(Suppl 2), 43–49. https://doi.org/10.1111/j.1529-8027.2012.00395.x (2012).
Ginter, E. & Simko, V. Women live longer than men. Bratisl Lek Listy 114, 45–49. https://doi.org/10.4149/bll_2013_011 (2013).
Dubal, D. B. & Wise, P. M. Estrogen and neuroprotection: From clinical observations to molecular mechanisms. Dialogues Clin. Neurosci. 4, 149–161 (2002).
Jett, S. et al. Endogenous and exogenous estrogen exposures: How women’s reproductive health can drive brain aging and inform alzheimer’s prevention. Front. Aging Neurosci. 14, 831807. https://doi.org/10.3389/fnagi.2022.831807 (2022).
Kandil, M. R., Darwish, E. S., Khedr, E. M., Sabry, M. M. & Abdulah, M. A. A community-based epidemiological study of peripheral neuropathies in Assiut, Egypt. Neurol. Res. 34, 960–966. https://doi.org/10.1179/1743132812Y.0000000099 (2012).
Su, H. et al. Natural menopausal age and cardiovascular disease risk factors in older Chinese women: Guangzhou Biobank cohort study. Menopause 28, 1410–1417. https://doi.org/10.1097/GME.0000000000001856 (2021).
Dias, L. S. et al. Polyneuropathy in severely obese women without diabetes: Prevalence and associated factors. Obes. Surg. 29, 953–957. https://doi.org/10.1007/s11695-018-03627-0 (2019).
Qian, X. et al. Reduced peripheral nerve conduction velocity is associated with Alzheimer’s disease: A cross-sectional study from China. Neuropsychiatr. Dis. Treat. 18, 231–242. https://doi.org/10.2147/NDT.S349005 (2022).
Corra, M. F. et al. Peripheral neuropathy in Parkinson’s disease: Prevalence and functional impact on gait and balance. Brain https://doi.org/10.1093/brain/awac026 (2022).
Schumacher, M. et al. Novel perspectives for progesterone in hormone replacement therapy, with special reference to the nervous system. Endocr Rev. 28, 387–439. https://doi.org/10.1210/er.2006-0050 (2007).
Frick, K. M. Estrogens and age-related memory decline in rodents: What have we learned and where do we go from here?. Horm Behav. 55, 2–23. https://doi.org/10.1016/j.yhbeh.2008.08.015 (2009).
Dusendang, J. R. et al. The association between perceived discrimination in midlife and peripheral neuropathy in a population-based cohort of women: The study of women’s health across the nation. Ann. Epidemiol. 37, 10–16. https://doi.org/10.1016/j.annepidem.2019.07.012 (2019).
Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. Hyattsville, M. U. S. D. o. H. https://www.cdc.gov/nchs/nhanes/index.htm. (1999–2004).
Benchimol, E. I. et al. The reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med. 12, e1001885. https://doi.org/10.1371/journal.pmed.1001885 (2015).
Hicks, C. W., Wang, D., Windham, B. G., Matsushita, K. & Selvin, E. Prevalence of peripheral neuropathy defined by monofilament insensitivity in middle-aged and older adults in two US cohorts. Sci. Rep. 11, 19159. https://doi.org/10.1038/s41598-021-98565-w (2021).
Gregg, E. W. et al. Prevalence of lower-extremity disease in the US adult population >=40 years of age with and without diabetes: 1999–2000 national health and nutrition examination survey. Diabetes Care 27, 1591–1597. https://doi.org/10.2337/diacare.27.7.1591 (2004).
Clinical Guidelines on the Identification. Evaluation, and treatment of overweight and obesity in adults-the evidence report National Institutes of Health. Obes. Res. 6(Suppl 2), 51S-209S (1998).
Heeringa, S., West, B. T. & Berglund, P. A. in Applied Survey Data Analysis. 2nd edn, (CRC Press, Taylor & Francis Group, New York, 2017).
Hosmer, D. W., Lemeshow, S. & Sturdivant, R. X. Wiley Series in Probability and Statistics 398 1 Online Resource (Wiley, 2013).
Mishra, S. R., Waller, M., Chung, H. F. & Mishra, G. D. Epidemiological studies of the association between reproductive lifespan characteristics and risk of Type 2 diabetes and hypertension: A systematic review. Maturitas 155, 14–23. https://doi.org/10.1016/j.maturitas.2021.09.009 (2022).
Cohen, R. Z., Seeman, M. V., Gotowiec, A. & Kopala, L. Earlier puberty as a predictor of later onset of schizophrenia in women. Am. J. Psychiatry 156, 1059–1065. https://doi.org/10.1176/ajp.156.7.1059 (1999).
Stöckl, D. et al. Reproductive factors and its association with peripheral arterial disease in women aged 52–81 years: The KORA F4 study. Atherosclerosis 228, 224–229. https://doi.org/10.1016/j.atherosclerosis.2013.01.035 (2013).
Freedman, D. S. et al. Relation of age at menarche to race, time period, and anthropometric dimensions: The bogalusa heart study. Pediatrics 110, e43. https://doi.org/10.1542/peds.110.4.e43 (2002).
Gill, D. et al. Age at menarche and adult body mass index: A mendelian randomization study. Int. J. Obes. (Lond) 42, 1574–1581. https://doi.org/10.1038/s41366-018-0048-7 (2018).
Wilson, D. A., Derraik, J. G., Rowe, D. L., Hofman, P. L. & Cutfield, W. S. Earlier menarche is associated with lower insulin sensitivity and increased adiposity in young adult women. PLoS ONE 10, e0128427. https://doi.org/10.1371/journal.pone.0128427 (2015).
Feng, Y. et al. Effects of age at menarche, reproductive years, and menopause on metabolic risk factors for cardiovascular diseases. Atherosclerosis 196, 590–597. https://doi.org/10.1016/j.atherosclerosis.2007.06.016 (2008).
Rumora, A. E. et al. Chain length of saturated fatty acids regulates mitochondrial trafficking and function in sensory neurons. J. Lipid Res. 60, 58–70. https://doi.org/10.1194/jlr.M086843 (2019).
Schlesinger, S. et al. General and abdominal obesity and incident distal sensorimotor polyneuropathy: Insights into inflammatory biomarkers as potential mediators in the KORA F4/FF4 cohort. Diabetes Care 42, 240–247. https://doi.org/10.2337/dc18-1842 (2019).
Kim, Y. & Je, Y. Early menarche and risk of metabolic syndrome: A systematic review and meta-analysis. J. Womens Health (Larchmt) 28, 77–86. https://doi.org/10.1089/jwh.2018.6998 (2019).
Schock, H. et al. Hormone concentrations throughout uncomplicated pregnancies: A longitudinal study. BMC Pregnancy Childbirth 16, 146. https://doi.org/10.1186/s12884-016-0937-5 (2016).
Wong, C. A. et al. Incidence of postpartum lumbosacral spine and lower extremity nerve injuries. Obstet Gynecol 101, 279–288. https://doi.org/10.1016/s0029-7844(02)02727-8 (2003).
Stuebe, A. M. & Rich-Edwards, J. W. The reset hypothesis: Lactation and maternal metabolism. Am. J. Perinatol. 26, 81–88. https://doi.org/10.1055/s-0028-1103034 (2009).
Akter, S. et al. Higher gravidity and parity are associated with increased prevalence of metabolic syndrome among rural Bangladeshi women. PLoS ONE 8, e68319. https://doi.org/10.1371/journal.pone.0068319 (2013).
Baradaran, H. R. et al. Higher gravidity and parity are associated with increased prevalence of metabolic syndrome among rural bangladeshi women. PLoS ONE 8, e68319. https://doi.org/10.1371/journal.pone.0068319 (2013).
Anwar, M. Y., Marcus, M. & Taylor, K. C. The association between alcohol intake and fecundability during menstrual cycle phases. Hum. Reprod. 36, 2538–2548. https://doi.org/10.1093/humrep/deab121 (2021).
Jacobs, M. B., Kritz-Silverstein, D., Wingard, D. L. & Barrett-Connor, E. The association of reproductive history with all-cause and cardiovascular mortality in older women: The Rancho Bernardo study. Fertil. Steril. 97, 118–124. https://doi.org/10.1016/j.fertnstert.2011.10.028 (2012).
Farpour-Lambert, N. J., Ells, L. J., Martinez de Tejada, B. & Scott, C. Obesity and weight gain in pregnancy and postpartum: An evidence review of lifestyle interventions to inform maternal and child health policies. Front. Endocrinol. (Lausanne) 9, 546. https://doi.org/10.3389/fendo.2018.00546 (2018).
Kumar, P. & Magon, N. Hormones in pregnancy. Niger. Med. J. 53, 179–183. https://doi.org/10.4103/0300-1652.107549 (2012).
Saklani, P., Khan, H., Gupta, S., Kaur, A. & Singh, T. G. Neuropeptides: Potential neuroprotective agents in ischemic injury. Life Sci 288, 120186. https://doi.org/10.1016/j.lfs.2021.120186 (2022).
Ramos-Martinez, E., Ramos-Martinez, I., Molina-Salinas, G., Zepeda-Ruiz, W. A. & Cerbon, M. The role of prolactin in central nervous system inflammation. Rev. Neurosci. 32, 323–340. https://doi.org/10.1515/revneuro-2020-0082 (2021).
Grimes, S. B. & Wild, R. in Endotext (eds K. R. Feingold et al.) (2000).
North, K., Gao, M., Allen, G. & Lee, A. C. Breastfeeding in a global context: Epidemiology, impact, and future directions. Clin. Ther. 44, 228–244. https://doi.org/10.1016/j.clinthera.2021.11.017 (2022).
Langton, C. R. et al. Association of parity and breastfeeding with risk of early natural menopause. JAMA Netw. Open. 3, e1919615. https://doi.org/10.1001/jamanetworkopen.2019.19615 (2020).
Yureneva, S. et al. Searching for female reproductive aging and longevity biomarkers. Aging (Albany NY) 13, 16873–16894. https://doi.org/10.18632/aging.203206 (2021).
Randolph, J. F. et al. Change in follicle-stimulating hormone and estradiol across the menopausal transition: Effect of age at the final menstrual period. J. Clin. Endocrinol. Metab. 96, 746–754. https://doi.org/10.1210/jc.2010-1746 (2011).
Prasad, J. B., Tyagi, N. K. & Verma, P. Age at menopause in India: A systematic review. Diabetes Metab. Syndr. 15, 373–377. https://doi.org/10.1016/j.dsx.2021.01.013 (2021).
Faubion, S. S., Kuhle, C. L., Shuster, L. T. & Rocca, W. A. Long-term health consequences of premature or early menopause and considerations for management. Climacteric 18, 483–491. https://doi.org/10.3109/13697137.2015.1020484 (2015).
Anagnostis, P. et al. Early menopause and premature ovarian insufficiency are associated with increased risk of type 2 diabetes: A systematic review and meta-analysis. Eur. J. Endocrinol. 180, 41–50. https://doi.org/10.1530/EJE-18-0602 (2019).
Miscio, G. et al. Obesity and peripheral neuropathy risk: A dangerous liaison. J. Peripher. Nerv. Syst. 10, 354–358. https://doi.org/10.1111/j.1085-9489.2005.00047.x (2005).
Buttner, R. et al. Inflammaging impairs peripheral nerve maintenance and regeneration. Aging Cell 17, e12833. https://doi.org/10.1111/acel.12833 (2018).
Shuster, L. T., Rhodes, D. J., Gostout, B. S., Grossardt, B. R. & Rocca, W. A. Premature menopause or early menopause: Long-term health consequences. Maturitas 65, 161–166. https://doi.org/10.1016/j.maturitas.2009.08.003 (2010).
Wu, S.-I., Chou, P. & Tsai, S.-T. The impact of years since menopause on the development of impaired glucose tolerance. J. Clin. Epidemiol. 54, 117–120. https://doi.org/10.1016/s0895-4356(00)00284-5 (2001).
Boulton, A. J. M. & Malik, R. A. Neuropathy of impaired glucose tolerance and its measurement. Diabetes Care 33, 207–209. https://doi.org/10.2337/dc09-1728 (2010).
Zhou, H., Zhang, C., Ni, J. & Han, X. Prevalence of cardiovascular risk factors in non-menopausal and postmenopausal inpatients with type 2 diabetes mellitus in China. BMC Endocr. Disord. 19, 98. https://doi.org/10.1186/s12902-019-0427-7 (2019).
Levine, M. E. et al. Menopause accelerates biological aging. Proc. Natl. Acad. Sci. USA 113, 9327–9332. https://doi.org/10.1073/pnas.1604558113 (2016).
Brann, D. W., Dhandapani, K., Wakade, C., Mahesh, V. B. & Khan, M. M. Neurotrophic and neuroprotective actions of estrogen: Basic mechanisms and clinical implications. Steroids 72, 381–405. https://doi.org/10.1016/j.steroids.2007.02.003 (2007).
Liu, R. et al. Female reproductive factors, menopausal hormone use, and Parkinson’s disease. Mov. Disord. 29, 889–896. https://doi.org/10.1002/mds.25771 (2014).
in Understanding Racial and Ethnic Differences in Health in Late Life: A Research Agenda The National Academies Collection: Reports funded by National Institutes of Health (eds R. A. Bulatao & N. B. Anderson) (2004).
Velasco-Mondragon, E., Jimenez, A., Palladino-Davis, A. G., Davis, D. & Escamilla-Cejudo, J. A. Hispanic health in the USA: A scoping review of the literature. Public Health Rev. 37, 31. https://doi.org/10.1186/s40985-016-0043-2 (2016).
Chumlea, W. C. et al. Age at menarche and racial comparisons in US girls. Pediatrics 111, 110–113. https://doi.org/10.1542/peds.111.1.110 (2003).
Martinez, G. M. Trends and patterns in menarche in the United States: 1995 through 2013–2017. Natl. Health Stat. Rep., 1–12 (2020).
Wyshak, G. & Frisch, R. E. Evidence for a secular trend in age of menarche. N. Engl. J. Med. 306, 1033–1035. https://doi.org/10.1056/NEJM198204293061707 (1982).
Jean, R. T. et al. Psychosocial risk and correlates of early menarche in Mexican-American girls. Am. J. Epidemiol. 173, 1203–1210. https://doi.org/10.1093/aje/kwq498 (2011).
Uranga, R. M. & Keller, J. N. The complex interactions between obesity, metabolism and the brain. Front. Neurosci. https://doi.org/10.3389/fnins.2019.00513 (2019).
Monteleone, P., Mascagni, G., Giannini, A., Genazzani, A. R. & Simoncini, T. Symptoms of menopause—Global prevalence, physiology and implications. Nat. Rev. Endocrinol. 14, 199–215. https://doi.org/10.1038/nrendo.2017.180 (2018).
Siiteri, P. K. Adipose tissue as a source of hormones. Am. J. Clin. Nutr. 45, 277–282. https://doi.org/10.1093/ajcn/45.1.277 (1987).
Acknowledgements
This work was financially supported by Graduate School Thesis Grant, Graduate School, Chulalongkorn University. I would like to express my deepest appreciation to all thesis committee.
Funding
This work was financially supported by the Graduate School Thesis Grant, Graduate School, Chulalongkorn University [Grant No.—059. batch 2/2021].
Author information
Authors and Affiliations
Contributions
All authors proposed and designed the study; J.L. generated and cleaned the dataset; J.L. and Y.C. analyzed the data and interpreted the results. J.L., S.S., J.A., and S.C. drafted the article. Every author reviewed the draft and approved the final version of the manuscript for publishing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, J., Chongpison, Y., Amornvit, J. et al. Association of reproductive factors and exogenous hormone use with distal sensory polyneuropathy among postmenopausal women in the United States: results from 1999 to 2004 NHANES. Sci Rep 13, 9274 (2023). https://doi.org/10.1038/s41598-023-35934-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-35934-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.