Abstract
Survival following out-of-hospital cardiac arrest (OHCA) remains low, typically less than 10%. Bystander cardiopulmonary resuscitation (CPR) and bystander-AED use have been shown to improve survival by up to fourfold in individual studies. Numerous community-based interventions have been implemented worldwide in an effort to enhance rates of bystander-CPR, bystander-AED use, and improve OHCA survival. This systematic review and meta-analysis aims to evaluate the effect of such interventions on OHCA outcomes. Medline and Embase were systematically searched from inception through July 2021 for studies describing the implementation and effect of one or more community-based interventions targeting OHCA outcomes. Two reviewers screened articles, extracted data, and evaluated study quality using the Newcastle–Ottawa Scale. For each outcome, data were pooled using random-effects meta-analysis. Of the 2481 studies identified, 16 met inclusion criteria. All included studies were observational. They reported a total of 1,081,040 OHCAs across 11 countries. The most common interventions included community-based CPR training (n = 12), community-based AED training (n = 9), and dispatcher-assisted CPR (n = 8). Health system interventions (hospital or paramedical services) were also described in 11 of the included studies. Evidence certainty among all outcomes was low or very low according to GRADE criteria. On meta-analysis, community-based interventions with and without health system interventions were consistently associated with improved OCHA outcomes: rates of bystander-CPR, bystander-AED use, survival, and survival with a favorable neurological outcome. Bystander CPR—14 studies showed a significant increase in post-intervention bystander-CPR rates (n = 285 752; OR 2.26 [1.74, 2.94]; I2 = 99%, and bystander AED use (n = 37 882; OR 2.08 [1.44, 3.01]; I2 = 54%) and durvival—10 studies, pooling survival to hospital discharge and survival to 30 days (n = 79 206; OR 1.59 [1.20, 2.10]; I2 = 95%. The results provide foundational support for the efficacy of community-based interventions in enhancing OHCA outcomes. These findings inform our recommendation that communities, regions, and countries should implement community-based interventions in their pre-hospital strategy for OHCA. Further research is needed to identify which specific intervention types are most effective.
Similar content being viewed by others
Introduction
Out-of-hospital cardiac arrest (OHCA) is a leading cause of morbidity and mortality worldwide1,2. The incidence of OHCA varies significantly in the literature, affecting 30 to 97 individuals per 100,000 person-years3. Survival rates remain low, typically less than 10%4. However, these survival rates can vary by up to five-fold in different areas suggesting that there may be opportunities for improvement2,5,6. The American Heart Association’s “chain of survival”, was developed in the early 2000s as a systematic and organized community-based approach to help improve the survival rates of OHCA by combining scientific literature and community-based initiatives7. Over two decades since the original publication, early bystander cardiopulmonary resuscitation (bystander-CPR) and early defibrillation remain key links in improving OHCA survival8. Despite this, the provision of bystander-CPR remains poor. Bystander-CPR is estimated to occur in approximately 40% of OHCAs with some areas reporting rates as low as 19%1,3. The rates of bystander automatic external defibrillator (bystander-AED) use are quite variable, ranging from 2 to 37%3.
In effort to strengthen the various links in the chain of survival and improve survival following OHCA, communities, regions, and countries across the world have implemented a range of educational interventions. Many studies have reported the efficacy of such interventions in improving rates of bystander-CPR and bystander-AED use as well as important clinical outcomes: overall survival and survival with a favorable neurological outcome following an OHCA9,10.
There have been excellent reviews addressing broad community interventions including emergency medical services, fire and police, however there have been few evaluating the efficacy of community-based interventions targeting laypersons11. Specifically analysis of initiatives’ characteristics associated with greater impact. This systematic review and meta-analysis explores these factors and the effects of community-based and health system interventions on rates of bystander-CPR, bystander-AED use, survival, and survival with a favorable neurological outcome among individuals experiencing OHCA. These findings will be critical to inform future systemic policy and provide guidance for the implementation of interventions focused on community and national pre-hospital OHCA care to ultimately reduce morbidity and mortality from OHCA.
Methods
Search strategy
Electronic searches were conducted in Medline and Embase databases from their earliest record (1946 and 1966 respectively) to December 8, 2021. The search strategy was constructed by one investigator and peer-reviewed using PRESS (Peer Review of Electronic Search Strategies) guidelines by a librarian12. We performed citation and conference abstract searches. The full search strategy is presented in eAppendix C in the Online-only Data Supplement.
Inclusion and exclusion criteria
Included studies needed to report one or more community-based intervention. Community-based interventions were defined as initiatives with a goal of increasing rates of bystander-CPR or bystander-AED use among the lay population. Community included members of a defined geographical community experiencing OHCA. Cities, counties, provinces, states, and countries were all eligible for inclusion as a defined “community”.
To meet inclusion criteria, studies must have reported pre- and post-intervention rates of at least one of the primary outcomes of interest: bystander-CPR and bystander-AED rates. Secondary outcomes of interest for this systematic review were survival to hospital discharge, survival to 30 days, and survival with favourable neurological outcomes (Cerebral Performance Category score of 1 (good cerebral performance) or 2 (moderate cerebral disability))13. We excluded studies that only targeted non-lay persons, i.e. dispatcher-assisted CPR, fire fighters, police. Studies exclusively reporting dispatch-assisted CPR or interventions exclusively targeting a population sub group (i.e. first responders, healthcare personnel or school students) did not meet the inclusion criteria for community-based interventions.
Study selection
Title and abstract screening were completed using a web-based platform Rayyan14. Screening was completed independently by two reviewers and blinding was maintained throughout. Conflicts were resolved by discussion until a consensus was reached between investigators.
Data extraction
Data extraction was completed by two reviewers using a standardized data extraction form. The full data extraction form can be found in eAppendix D. In cases where there were multiple publications describing a single study, the most complete report, in terms of population size and study duration, was used as the primary source.
Assessment of risk of bias and certainty of evidence
Two reviewers completed risk of bias assessments without blinding for each study using the Newcastle–Ottawa scale, a validated tool for quality assessment of non-randomized studies in meta-analyses15. (eAppendix E). Evidence certainty and strength of recommendations for each outcome was evaluated through the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach by one reviewer and verified by a second reviewer16.
Statistical analysis and data synthesis
Data was synthesized using Review Manager 5.4. Individual and pooled odds ratios (ORs) with 95% confidence intervals (CIs) were calculated for the 4 outcomes of interest using all studies with sufficient data. A random effects meta-analysis was used due to the significant heterogeneity between studies. Heterogeneity was assessed through the I2 statistic using criteria from the GRADE handbook: low, ≤ 40%; moderate, 30–60%; substantial, 50–90%; or considerable inconsistency, ≥ 7517. Studies were stratified post-hoc into sub-groups by the duration of the study intervention. Publication bias was evaluated by inspection of the funnel plot for each outcome.
This review meets the criteria for the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) and MOOSE (Meta-analysis of Observational Studies in Epidemiology) reporting guidelines (eAppendices A & B in the Online-only Data Supplement). The protocol was registered in the PROSPERO database (CRD42021246438). All data are within the manuscript and additional files.
Results
Included studies and characteristics
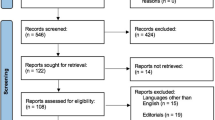
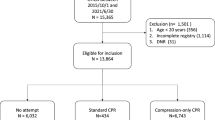
A total of 2481 records were retrieved. After the removal of 632 duplicates, 1849 articles were screened by title and abstract. Of the 137 articles that underwent full text review(Kappa 0.9), 16 met the pre-determined inclusion criteria(Kappa 0.97) (Fig. 1).
All 16 included studies were observational studies (retrospective n = 9; prospective n = 7). Of these, 6 were conducted in Europe, 6 in the Asia–Pacific region, and 4 in North America. The number of analyzed OHCAs per study ranged from 216 to 816,385 (median = 6103; IQR 3325–38,061) with the total number of included OHCAs reaching 1,091,103. Study and intervention duration ranged from 1.2 to 15 years and 1 day to 15 years, respectively. Full study characteristics are outlined in Table 1.
Interventions reported in each study were categorized as either community-based interventions only (n = 5) or community-based intervention plus health system interventions (n = 11). Health system interventions refer to those that target hospital or paramedicine specific care. Community-based intervention categories included CPR (n = 12) or AED (n = 9) training initiatives, dispatcher-assisted CPR programs (n = 8), school-based training (n = 6), mass media or awareness campaigns (n = 6), public access defibrillation programs (n = 6), brief mass training events (n = 5), legislative changes mandating CPR training for certain sub-populations (n = 3), and notification systems to alert participating bystanders of a nearby OHCA (n = 2). Detailed descriptions of the interventions reported in each study can be found in Table 2.
Outcomes
Table 1 outlines the outcomes reported in each study and Table 2 shows the corresponding pre- and post-intervention rates. Results of meta-analyses are presented in forest plots (Figs. 2, 3, 4) and summarized in Table 3.
Bystander-CPR (critical outcome)
Bystander-CPR rates were reported in all 16 studies of which 14 of these studies showed significant improvement in bystander-CPR (p < 0.05). Meta-analysis of 14 studies showed a significant difference in post-intervention bystander-CPR rates (n = 285 752; OR 2.26 [1.74, 2.94]; I2 = 99%; Fig. 2). All three intervention duration subgroups were significantly improved following interventions with increasing effect size noted with greater intervention duration: 0–4.9 years (OR 1.50 [1.16, 1.95]), 5–9.9 years (OR 2.12 [1.34, 3.36]), and 10–15 years (OR 4.25 [1.83, 9.86]).
Bystander AED Rates (important outcome)
Five of the included studies reported data on bystander-AED rates. All 5 reported increases; 4 were statistically significant while the last was not. Meta-analysis of the pooled results showed a significant change in the post-intervention period (n = 37 882; OR 2.08 [1.44, 3.01]; I2 = 54%).
Survival (critical outcome)
Survival was reported in 12 studies. Two studies reported survival to 30 days; both showed significant increases (p < 0.05). The remaining 10 studies described survival to hospital discharge. Among these, 5 reported significant increases and 4 reported non-significant increases. The final study had a significant decrease in survival to discharge (13.7% to 10.5%; p < 0.01) though the findings did not remain significant following multivariable adjustment (p = 0.08)17. Meta-analysis included 10 studies, pooling survival to hospital discharge and survival to 30 days (n = 79 206; OR 1.59 [1.20, 2.10]; I2 = 95%; Fig. 4). Among the sub-groups, 0–4.9 years (1.62 [1.03, 2.55]) and 10–15 years (OR 1.75 [1.48, 2.08]) were significantly improved as compared to 5–9.9 years (1.35 [0.85, 2.14]).
Survival with favorable neurological outcome (critical outcome)
Survival with favorable neurological outcome, CPC 1 or 2, was reported in 9 studies. Of these, 7 had significant improvement (p < 0.05). One study noted a negligible increase (8.3% to 8.7%; p = 0.87)5. The last study noted a significant decrease (10.4% to 8.9%; p < 0.01) though the decrease was not statistically significant after their multivariable adjustment (p = 0.07)17. On meta-analysis of 8 studies, the pooled results were significant (n = 272,882; OR 1.42 [1.06, 1.90]; I2 = 96%). Among the sub-groups only 10–15 years was significant (OR 1.79 [1.31, 2.43]); the effect size increased with intervention duration.
Risk of bias and certainty of evidence
The Newcastle–Ottawa tool was used to assess the quality of included studies on a scale of 0 to 8. Nine studies received scores of 7 or 8; three a score of 5 or 6, and the remaining four a score of 3 or 4 (Table 4).
The certainty of effect size for each outcome was evaluated according to GRADE criteria and was found to be low or very low certainty in all outcomes of interest (Table S1 in the Online-only Data Supplement). The main shortcomings across outcomes were the risk of bias and inconsistency due to significant heterogeneity among studies. A dose–response gradient was noted for rates of bystander-CPR, survival, and survival with favorable neurological outcome.
Heterogeneity and sensitivity analysis
Heterogeneity for pooled bystander-AED analysis was moderate (I2 = 54%). Pooled I2 values for the other 3 outcomes were considerable: bystander-CPR (I2 = 99%), survival (I2 = 95%), and survival with favorable neurological outcome (I2 = 96%). Stratification by intervention duration accounted for some heterogeneity. Among the 9 sub-groups heterogeneity decreased to low in 3 groups (survival 10–15 years; survival with favorable neurological outcome 0–4.9 and 10–15 years) and to substantial in 2 groups (bystander-CPR 0–4.9 years; survival 0–4.9 years). Despite the heterogeneity, the authors chose to present the results of the meta-analyses according to the following rationale. First, there is a clear positive trend among all outcomes. Second, there is a pattern among the stratified outcomes (larger effect size with greater intervention duration) suggesting the outcomes are not random; further, this dose–response gradient may be critical to informing the duration of future initiatives. Third, the observed heterogeneity is accounted for when judging the certainty of evidence through the GRADE approach and contributes to our low certainty in the effect size of outcomes. As such, the meta-analyses are presented in this paper, but the pooled estimates must be interpreted with caution18.
Discussion
Principle findings
This systematic review and meta-analysis included 16 studies reporting on 1,091,103 OHCAs in 11 countries. The findings suggest that community-based interventions and community-based interventions plus health system interventions are associated with significant improvement in all 4 outcomes of interest. The data suggest a relationship between intervention duration and effect size as noted in meta-analyses and examining commonalities among the least effective studies5,19. Further, community-based interventions plus health system interventions were noted to have a slightly larger effect suggesting the importance of bundling interventions.
Findings in the context of previous work
Our review is the first to evaluate the efficacy of community-based interventions, defined as those explicitly targeting laypersons. There have been two systematic reviews (one with meta-analysis) assessing the effects of broader system-based interventions including those targeting first-responders, EMS, and hospital systems; many of the included studies in both reviews lacked interventions targeting laypersons. However, these reviews reported similar improvements in system-level and clinical outcomes as those described in our review: improved bystander-CPR, survival, and survival with favorable neurological outcome20,21. Thus, our findings provide further support for the efficacy of health system interventions and foundational evidence for the efficacy of community-based interventions.
We observed a pattern of greater improvement among studies which bundled the 3 most common community-based interventions: CPR training, AED training, and dispatcher-assisted CPR (included in 12, 9, and 8 studies respectively). A recent systematic review compared outcomes between EMS systems with dispatch-assisted CPR to EMS systems where it is not offered22. They found that dispatcher-assisted CPR is associated with significantly higher bystander-CPR rates (n = 9 studies; OR 3.10 [2.25, 4.25]) but not increased rates of high-quality bystander-CPR; nor was there any significant improvement in survival following OHCA22. It is possible that this bundle of 3 interventions has a synergistic effect; prior resuscitation training provides competency and higher quality CPR while dispatcher-assisted CPR can prompt action resulting in a greater overall intervention effect.
We found a temporal trend between intervention duration and enhanced outcomes. There are several possible explanations for this trend. A lack of training is a significant barrier to providing bystander-CPR and bystander-AED23,24. Cultural relevance of curriculum, costs, and language concerns have been shown to impact CPR/AED training attainment. With long-term training initiatives, a greater proportion of the population could be trained, increasing the likelihood that a qualified bystander will be present at an OHCA event. It is also possible that with prolonged exposure to mass media and awareness campaigns, there is a change in the culture regarding resuscitation that increases the comfort of bystanders to perform CPR23,24.
Implications
The GRADE Evidence to Decision framework was utilized to inform recommendations given our findings in the context of broader considerations (full description in eAppendix F of the Online-only Data Supplement). The observational design and the high heterogeneity between included studies were the primary contributors that reduced the evidence certainty of outcomes to low or very low.
We strongly recommend based on low quality evidence that communities, regions, and countries assess their current pre-hospital strategy for OHCA care and consider implementing community-based interventions, especially when combined with health system interventions, to improve OHCA outcomes.
Strengths and limitations
The strengths of this review include robust methods to select, appraise, and analyze study findings. Included studies provide generalizable results as they span 24 years, 11 countries, include over one million OHCAs, and describe a range of community-based interventions and health system interventions. As with all research, the findings of this review should be considered in the context of study limitations. The observational design of studies resulted in a high risk of bias and the potential for confounding variables. Temporal trends in CPR and OHCA outcomes may limit the certainty of the effects of the interventions in the included studies. Significant heterogeneity between studies also reduces the certainty of evidence among outcomes of interest. There is substantial heterogeneity in the patient populations (non-EMS witnessed arrests, arrests that received resuscitation, all OHCA, OHCA transported to hospital) which may bias the results of this meta-analysis. There exists potential for misclassification of “laypersons”—international EMS personnel and reporting systems may have differing definitions.
Future direction
Implementation of community-based interventions for OHCA is needed for high-risk communities, particularly those with suboptimal EMS services. However, additional data on cost-effectiveness (costs per life saved) is needed. Moreover, with advancements in technology, novel interventions to engage the community in resuscitation need to be investigated, including crowdsourcing technologies, drone-delivered AEDs, AED registries and pocket AEDs.
Conclusion
Community-based interventions are associated with significant improvement in all 4 outcomes of interest: rates of bystander-CPR, bystander-AED use, survival, and survival with a favorable neurological outcome following OHCA. We recommend that communities and policymakers assess their current pre-hospital strategy for OHCA care and consider implementing a bundle of community-based interventions. For greatest impact, initiatives should be sustainable and continued long term.
Data availability
All data are within the manuscript and additional files.
References
Virani, S. S. et al. Heart disease and stroke statistics—2020 update: A report from the American Heart Association. Circulation 141(9), e139–e596 (2020).
Graham, R. M. A. M. & Andrea, M. S. Strategies to Improve Cardiac Arrest Survival (National Academies Press, 2015).
Kiguchi, T. et al. Out-of-hospital cardiac arrest across the World: First report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation 152, 39–49 (2020).
Yan, S. et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: A systematic review and meta-analysis. Crit. Care 24, 1–13 (2020).
Uber, A., Sadler, R. C., Chassee, T. & Reynolds, J. C. Does non-targeted community CPR training increase bystander CPR frequency? Prehosp. Emerg. Care 22(6), 753–761 (2018).
Chan, P. S., McNally, B., Tang, F. & Kellermann, A. Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation 130(21), 1876–1882 (2014).
American Heart Association. Part I. Introduction to the international guidelines 2000 for CPR and ECG. Circulation 102, 1–3421 (2000).
Cummins, R. O., Ornato, J. P., Thies, W. H. & Pepe, P. E. Improving survival from sudden cardiac arrest: The" chain of survival" concept A statement for health professionals from the Advanced Cardiac Life Support Subcommittee and the Emergency Cardiac Care Committee, American Heart Association. Circulation 83(5), 1832–47 (1991).
Ho, A. F. W. et al. Implementation of a National 5-Year Plan for Prehospital Emergency Care in Singapore and impact on out-of-hospital cardiac arrest outcomes from 2011 to 2016. J. Am. Heart Assoc. 9(21), e015368 (2020).
Hollenberg, J. et al. Improved survival after out-of-hospital cardiac arrest is associated with an increase in proportion of emergency crew–witnessed cases and bystander cardiopulmonary resuscitation. Circulation 118(4), 389–396 (2008).
Scapigliati, A. et al. Community initiatives to promote basic life support implementation—A scoping review. J. Clin. Med. 10(24), 5719 (2021).
McGowan, J. et al. PRESS peer review of electronic search strategies: 2015 guideline statement. J. Clin. Epidemiol. 75, 40–46 (2016).
Jennett, B. & Bond, M. Assessment of outcome after severe brain damage: A practical scale. The Lancet 305(7905), 480–484 (1975).
Ouzzani, M., Hammady, H., Fedorowicz, Z. & Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 5, 1–10 (2016).
Peterson, J., Welch, V., Losos, M. & Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-analyses 1–12 (Ottawa Hospital Research Institute, 2011).
Schünemann, H. J. GRADE: From grading the evidence to developing recommendations. A description of the system and a proposal regarding the transferability of the results of clinical research to clinical practice. Z. Evid. Fortbildung Qual. im Gesundheitswesen. 103(6), 391–400 (2009).
van Diepen, S. et al. Multistate 5-year initiative to improve care for out-of-hospital cardiac arrest: Primary results from the HeartRescue Project. J. Am. Heart Assoc. 6(9), 5716 (2017).
Guyatt, G. H. et al. GRADE guidelines: 7. Rating the quality of evidence—Inconsistency. J. Clin. Epidemiol. 64(12), 1294–302 (2011).
Ristagno, G. et al. Increased rate of bystander-initiated CPR during the initial 3 months after completion of the week of cardiac arrest awareness “Viva!” in two Italian cities. Resuscitation 85, S2–S3 (2014).
Ko, Y.-C. et al. The effect of system performance improvement on patients with cardiac arrest: A systematic review. Resuscitation 157, 156–165 (2020).
Yu, Y. et al. Assessment of community interventions for bystander cardiopulmonary resuscitation in out-of-hospital cardiac arrest: A systematic review and meta-analysis. JAMA Netw. Open 3(7), e209256 (2020).
Nikolaou, N. et al. A systematic review and meta-analysis of the effect of dispatcher-assisted CPR on outcomes from sudden cardiac arrest in adults and children. Resuscitation 138, 82–105 (2019).
Riggs, M., Franklin, R. & Saylany, L. Associations between cardiopulmonary resuscitation (CPR) knowledge, self-efficacy, training history and willingness to perform CPR and CPR psychomotor skills: A systematic review. Resuscitation 138, 259–272 (2019).
Sasson, C. et al. Barriers and facilitators to learning and performing cardiopulmonary resuscitation in neighborhoods with low bystander cardiopulmonary resuscitation prevalence and high rates of cardiac arrest in Columbus, OH. Circ. Cardiovasc. Qual. Outcomes 6(5), 550–558 (2013).
Franek, O., Michaela, P. & Petra, S. Bystander resuscitation rate increased more than six times between 2003 and 2013 in the City of Prague. Resuscitation 96, 77–78 (2015).
Wissenberg, M. et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA 310(13), 1377–1384 (2013).
Dahan, B. et al. Impact of a public information campaign about the chain of survival on out of hospital cardiac arrest bystander cardiopulmonary resuscitation initiation. Eur. Heart J. 35, 14–5 (2014).
Iwami, T., Kitamura, T., Kiyohara, K. & Kawamura, T. Dissemination of chest compression—Only cardiopulmonary resuscitation and survival after out-of-hospital cardiac arrest. Circulation 132(5), 415–422 (2015).
Lai, H. et al. Interventional strategies associated with improvements in survival for out-of-hospital cardiac arrests in Singapore over 10 years. Resuscitation 89, 155–161 (2015).
Ro, Y. S. et al. Association between county-level cardiopulmonary resuscitation training and changes in survival outcomes after out-of-hospital cardiac arrest over 5 years: A multilevel analysis. Resuscitation 139, 291–298 (2019).
Mauri, R. et al. Fifty percent survival of cardiac arrest in Switzerland: An Utopian goal? Eur. Heart J. 31, 646 (2010).
Lin, H.-Y. et al. Assessing quality of bystander chest compression and shock delivery by electrocardiogram signals from public automated external defibrillators in Taiwan. Circulation 134, A15801 (2016).
Lick, C. J. et al. Take Heart America: A comprehensive, community-wide, systems-based approach to the treatment of cardiac arrest. Crit. Care Med. 39(1), 26–33 (2011).
Bergamo, C. et al. TAKE10: A community approach to teaching compression-only CPR to high-risk zip codes. Resuscitation 102, 75–79 (2016).
Del Rios, M. et al. Large urban center improves out-of-hospital cardiac arrest survival. Resuscitation 139, 234–240 (2019).
Funding
The funding was provided by MERLIN (2002-01).
Author information
Authors and Affiliations
Contributions
K.M.S. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: S.M.M., K.M.S. Acquisition of the data: K.M.S., R.O. Analysis and interpretation of data: K.M.S., R.O. Drafting of the manuscript: K.M.S., S.M.M. Critical revision of the manuscript for important intellectual content: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Simmons, K.M., McIsaac, S.M. & Ohle, R. Impact of community-based interventions on out-of-hospital cardiac arrest outcomes: a systematic review and meta-analysis. Sci Rep 13, 10231 (2023). https://doi.org/10.1038/s41598-023-35735-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-35735-y
This article is cited by
-
Trauma systems in high socioeconomic index countries in 2050
Critical Care (2024)
-
Family history, socioeconomic factors, comorbidities, health behaviors, and the risk of sudden cardiac arrest
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.