Abstract
The factors affecting the outcomes of segmental femoral shaft fractures are currently unknown. We evaluated the outcomes of intramedullary (IM) nail fixation and investigated factors affecting nonunion of femoral shaft segmental fractures. A total of 38 patients who underwent IM nail fixation for femoral shaft segmental fractures (AO/OTA 32C2) at three university hospitals with a minimum 1-year follow-up period were retrospectively reviewed. The patients were divided into union (n = 32) and nonunion (n = 6) groups. We analyzed smoking status, diabetes mellitus, location of the segmental fragment, segment comminution, filling of the IM nail in the medullary canal, residual gap at the fracture site, use of a cerclage wire or blocking screws as factors that may affect the surgical outcome. In the union group, the average union time was 5.4 months (4–9 months). In the nonunion group, five patients required additional surgery within an average of 7.2 months (5–10 months) postoperatively, whereas one patient remained asymptomatic and did not require further intervention. On comparing the two groups, insufficient canal filling of the IM nail (union, 25.0%; nonunion, 83.3%; p = 0.012) and the presence of a residual gap at the fracture site after reduction (union, 31.3%; nonunion, 83.3%; p = 0.027) were significantly different. In the multivariate analysis, only insufficient canal filling of the IM nail was found to be a factor affecting nonunion, with an odds ratio of 13.3 (p = 0.036). In this study, a relatively high nonunion rate (15.8%) was observed after IM nail fixation. Insufficient IM nail canal filling and a residual gap at the fracture site post reduction were factors affecting segmental femoral shaft fracture nonunion after IM nail fixation.
Similar content being viewed by others
Introduction
Femoral shaft fractures have a reported incidence of 9.9–21 per 100,000 person-year, and segmental fractures account for approximately 13% of femoral shaft fractures1,2. Intramedullary (IM) nail fixation is the gold standard surgical treatment of femoral shaft fractures. Previous studies have reported successful outcomes after IM nail fixation for femoral shaft fractures3, including highly comminuted fractures (AO/OTA classification 32C3)4,5,6. Segmental femoral shaft fractures (AO/OTA classification 32C2) have little or no comminution and are more technically difficult to reduce due to the concentration of strain at the proximal and distal ends of the segment, leading to increased operative time and delayed time to union7,8. Therefore, the factors affecting the outcome of segmental femoral shaft fractures (AO/OTA classification 32C2) likely differ from those affecting other types of femoral shaft fractures. Although some studies have reported delayed union times after IM nailing for segmental femoral shaft fractures7,8, no studies have thoroughly reported on radiographic outcomes or investigated factors affecting nonunion. Therefore, this study examined the radiographic results of IM nail fixation for segmental femoral shaft fractures and analyzed the factors associated with nonunion.
Materials and methods
Ethical approval
This retrospective study was performed according to the Declaration of Helsinki standards and was approved by the institutional review boards of Hanyang University Hospital, Hanyang University Guri Hospital, and Yeungnam University Hospital. This study received exemption from informed consent by the institutional review board of Hanyang University Hospital.
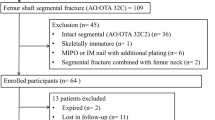
Patient selection
A retrospective multi-center review of the medical records of patients who underwent IM nail fixation for segmental femoral shaft fractures between July 2010 and October 2020 was conducted. Three orthopedic surgeons, all orthopedic trauma specialists with more than ten years of experience, performed all surgeries at three different university hospitals. Patients with segmental femoral shaft fractures who completed follow-up radiographs at least one year after IM nail fixation were included. Patients with open fractures, concomitant femoral fractures beyond the shaft (AO/OTA 31 or 33 fracture), major vascular injury, less than one year follow-up, or aged ≤ 18 years old were excluded.
Assessment of outcomes
Demographic data on age, sex, smoking, diabetes mellitus (DM), follow-up period, injury mechanism were collected. Injuries were divided into low- and high-energy according to the mechanism involved. Falls from less than 1 m in height were classified as low-energy injuries, while other injuries due to greater heights or traffic accidents were classified as high-energy injuries.
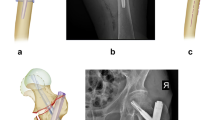
Radiographic data on the location of the fractured segment, segment comminution, surgical reduction technique, implant type, and time to union were analyzed. The fractured segment was classified by the involved anatomic area: subtrochanteric, subtrochanteric-isthmus, isthmus, isthmus-distal 1/3, and distal 1/3-supracondylar. All patients underwent surgery in a closed reduction manner. Depending on the surgeon’s decision, some cases involved minimal invasive percutaneous reduction techniques such as applying downward pressure on the lesser trochanter with long forceps or a Hohmann retractor, manipulating the segment using a Schanz pin (joy stick technique) (Fig. 1), applying a cerclage wire using cerclage wire passer, or using a blocking screw9. Although reamed IM nails with interlocking screws were used in all patients, the type of IM nail implant was determined by fracture location or surgeon preference. Antegrade IM nails were used in most cases with retrograde IM nails only used in four cases. Since our aim in this study was to analyze overall radiographic union after IM nail fixation, both antegrade and retrograde IM nail cases were included since both would lead to similar indirect bone healing at the fracture site.
A 43-year-old male patient with a left femur segmental fracture caused by a motorcycle accident. (a) Plain radiograph at the initial visit. Segmental fracture was observed around the isthmus of the femur. (b) To aid reduction, a minimal skin incision was made in the lesser trochanter area, and the Hohmann retractor was placed on the lesser trochanter and pressed down to negate the flexion deforming force. (c) It was difficult to achieve reduction by a closed mean due to the absence of bony contact at the fracture site. (d) A percutaneous incision was made and a Schanz pin was inserted to manipulate the fracture site using the joy stick technique. (e) Intraoperative clinical photograph of the joystick technique. (f, g) Plain radiographs after surgery show good quality of reduction, restoring alignment, and the length of femur.
Patients were followed up at one, two, three, six, nine months, and one year postoperatively, followed by every 6 months thereafter. Plain radiographs were taken at each follow-up visit. If delayed union or nonunion was suspected at any visit, monthly follow-up was done. Evidence of radiographic union included the presence of adequate callus bridging at the fracture site, the disappearance of the fracture line in a minimum of three cortices on anteroposterior and lateral plain femur radiographs, and union of both the proximal and distal ends of the fractured segment. The absence of an adequate bridging callus on either end of the fractured segment was not considered as union. Nonunion was defined as failure to achieve union on plain radiographs by nine months postoperatively or no visible progression of bone healing on serial plain radiographs for more than three consecutive months10,11.
Patients diagnosed with nonunion underwent computed tomography (CT) to confirm the location and extent of the nonunion prior to a second operation (Fig. 2). Nonunion was classified as hypertrophic, oligotrophic, or atrophic according to the Weber and Cech classification system12. A second operation was performed only when there was no progression of union on serial radiographs, or when it was deemed that union could not be achieved without additional surgery. The specific surgical approach used was based on the type of nonunion and the surgeon’s preferred method.
A 24-year-old male patient with a right femur segmental fracture caused by a motorcycle accident. (a) Plain radiograph at the initial visit. Segmental fracture was observed between the subtrochanteric area and the isthmus of the femur. (b) Fracture was treated with intramedullary nailing. Traction force was applied and cerclage wires were used for reduction. (c, d) Plain radiographs 9 months after surgery. Oligotrophic nonunion with little callus formation at distal isthmic area was observed. Second operation with plate augmentation was planned for nonunion. (e, f) Before the second operation, computed tomography (CT) was performed to confirm the location and extent of the nonunion. On CT coronal and sagittal planes, it is noted that there is no callus formation in the distal isthmic area. (g, h) Plain radiographs 46 months after second operation. Complete union was achieved.
In order to determine the factors associated with non-union, we analyzed smoking status, DM, fractured segment location, segment comminution, filling of the IM nail in the medullary canal, residual gap at the fracture site, and use of a cerclage wire or blocking screws. For the filling of the IM nail, the distance between the inner cortex and the IM nail was measured if a gap between the IM nail and the inner cortex was visible in the isthmic portion on the immediate postoperative anteroposterior plain radiograph. In case the inner cortex and IM nail were in contact on one side, the distance was measured on the opposite side, and if both sides were out of contact, each distance was measured and summated. It was defined as insufficient filling if the measured distance was ≥ 2 mm13. A residual gap at the fracture site was defined as a gap of ≥ 2 mm at each end of segment on the immediate postoperative anteroposterior or lateral plain radiograph14. Two orthopedic surgeons who did not participate in the operations evaluated each radiograph twice, one month apart. If there was initial disagreement, the surgeons reached a consensus through discussion.
Active range of motion exercises were started immediately after surgery. Partial weight bearing was gradually increased as tolerated by the patient. The degree and timing of partial weight bearing were determined according to the patient's condition15. Walking aids were removed and full weight bearing was allowed when a patient was deemed to be able to walk independently. There were no significant differences in postoperative rehabilitation protocols between the involved institutions.
Statistical analysis
An independent t-test was performed for continuous variables as a comparative analysis between the union and nonunion groups. The Mann–Whitney U test was used as a non-parametric test for continuous variables. For categorical variables, Fisher's exact test and chi-square test were used. To identify risk factors for nonunion, univariate and multivariate logistic regression analyses were performed using factors identified as significant among the related factors. Cohen’s kappa coefficient of agreement was used to assess the intra-observer reliability and inter-observer agreement of radiographic measurements. Statistical significance was set at a p-value of 0.05. Statistical analyses were performed using SPSS Statistics (version 20.0; SPSS Inc., Chicago, IL, USA).
Results
Of the 55 patients initially identified, 17 were excluded (four due to open fractures, five due to concomitant femoral fractures, two due to vascular injury, and six due to insufficient follow-up). The final included study population consisted of 38 femurs from 38 patients. The mean patient age was 45.4 (18–74) years, and 33 patients (86.8%) were male whereas five (13.2%) were female. There were six smokers (15.8%) and four diabetic patients (10.5%). The mean follow-up period was 28.6 (12–68) months. Low-energy injuries occurred in three cases and high-energy injuries occurred in the remaining 35. All three low-energy injuries were ground-level falls whereas high-energy injuries included motorcycle accidents (16 cases), automobile accidents (11 cases), falls from height above 1 m (six cases), ski injury (one case), and crushing injury by heavy objects (one case). By segmental fracture location, one case involved the subtrochanteric area, 16 involved the subtrochanteric-isthmus area, 14 involved the isthmic area, three involved the isthmus-distal 1/3 area, and four involved the distal 1/3-supracondylar area (Table 1). Segment comminution was observed in 22 cases (57.9%). Among the patients undergoing minimally invasive percutaneous reduction techniques, 12 (31.6%) underwent cerclage wiring and two (5.3%) involved use of blocking screws. Expert Asian Femoral Nail (A2FN; Synthes, Solothurn, Switzerland) was used in 17 cases, Proximal Femoral Nail Antirotation (PFNA; Synthes, Solothurn, Switzerland) in 10 cases, Zimmer Natural Nail (ZNN; Zimmer, Warsaw, IN, USA) in seven cases and Distal Femoral Nail (DFN; Synthes, Solothurn, Switzerland) in four cases. Each IM nail was used without any version changes throughout the study. Union was obtained without additional surgery in 32 cases (84.2%), and the average time to union was 5.4 months (3–9 months). Insufficient filling of the IM nail was observed in 13 cases (34.2%), and a residual gap was found in 15 cases (39.5%) (Table 1).
Nonunion was confirmed in 6/38 cases (15.8%), all resulting from high-energy injuries (Table 2). Regarding the type of nonunion, hypertrophic nonunion was observed in one case and oligotrophic nonunion in five cases. In four nonunion cases, the segmental fragment was located at the isthmus, and nonunion occurred at the proximal segment end. In the other two nonunion cases, the segmental fracture was located at subtrochanteric-isthmic region and the nonunion occurred in the distal segment end (Fig. 2). There was no significant difference in the nonunion rate according to surgeon (p = 0.760). Among the six nonunion cases, a cerclage wire was used initially in one case. Five of the six non-union cases required a second surgery, with the time to second surgery averaging 7.2 months from the initial operation. Four patients underwent plate augmentation and one underwent exchange nailing (Table 2). One nonunion patient was asymptomatic, and was followed up without additional surgery.
There were no statistically significant differences between the two groups in terms of age, sex, smoking status, DM, injury mechanism, location of the segmental fragment, segment comminution, usage of cerclage wire or blocking screw, or the type of IM nail used (p > 0.05) (Table 1).
Insufficient IM canal filling occurred in five out of six nonunion cases, but in only eight out of 32 (25%) union cases (p = 0.012) (Table 1). Similarly, a residual gap of the fracture segment was observed in five of six nonunion cases (83.3%), but in only 10 of 32 (31.3%) in the union group (p = 0.027) (Table 1).
The odds ratio of insufficient filling of the medullary canal and residual gap at the fracture site was 14.9 (p = 0.021) and 11.0 (p = 0.039), respectively, in univariate analysis (Table 3). In multivariate analysis, insufficient filling of the medullary canal was found to be a factor associated with nonunion, with an odds ratio of 13.3 (p = 0.036) (Table 3). The Cohen's kappa (κ) coefficients for intra-observer reliability and inter-observer agreement by location of segmental fracture were 0.924 and 0.907, respectively. For insufficient filling, the intra-observer reliability and inter-observer agreement for both insufficient canal filling (0.917 and 0.842, respectively) and the presence of a residual gap (0.865 and 0.825, respectively) were graded as excellent.
Discussion
This study investigated the outcomes of IM nail fixation for segmental femoral shaft fractures (AO/OTA 32C2) and identified factors affecting nonunion. In our study, the overall union rate was 84.2%, lower than the previously reported 92–97.8% union after IM nailing for femoral shaft fractures16,17. One possibility for this discrepancy is that segmental fractures occur with higher energy injuries compared to simple or wedged femur shaft fractures and are often accompanied by more significant soft tissue damage18,19. Greater degrees of soft tissue damage correlate with reduced local blood flow to the injured area and poorer fracture healing, leading to a greater chance of nonunion or delayed union20.
In this study, six cases (15.8%) of nonunion were identified, and five (13.2%) of these nonunion cases were of the oligotrophic nonunion type. Insufficient canal filling of IM nail and the presence of a residual gap at the fracture site were identified as factors affecting nonunion. In previous reports of femoral shaft fractures, the most common nonunion type after IM nailing was hypertrophic21. However, we found oligotrophic non-union to be the most common non-union type in our femoral shaft segmental fracture populations. A possible reason for this difference is that segmental fractures occur in higher-energy injuries leading to a greater chance of both insufficient IM canal filling and persistence of a segmental fracture gap.
In femoral shaft segmental fractures, the segmental fragment can move or rotate relatively freely as there are no fixed parts at the fracture site and it is often out of anatomical alignment. As a result, it is difficult to achieve appropriate reduction because proper contact is required at both ends of the segmental fragment for optimal healing. Also, sufficient reaming may not be achieved since segmental fragments can move during reaming, and there is greater risk of surrounding soft tissue damage during reaming. For these reasons, it is difficult to obtain adequate reduction and perform sufficient reaming at the segmental fragment. Although open reduction would have been better for reduction quality, more stable rotational alignment, and reduced residual gap persistence, it would have exacerbated soft tissue and blood flow impairment to the fracture site already sustained by high-energy injury. This would be expected to adversely affect indirect bone healing after IM nailing and increase the complication rate. Previous studies have reported high infection rates and prolonged union times when open reduction is performed for IM nail fixation of femoral shaft fractures22,23. These limitations of open reduction caused our surgeons to perform minimal percutaneous reduction techniques even if there were difficulties associated with reduction and reaming.
In a retrospective case–control study of 211 patients, the authors recommended a minimum nail fit of 70% at the isthmus and ideally ≥ 90% to avoid reoperation24. In contrast, another retrospective study reported no correlation between nail diameter and nonunion. This lack of correlation may be due to the fact that there was only one case of insufficient IM canal filling greater than 2 mm in the study13. Our study included 13 cases of insufficient IM canal filling possibly due to the difficulty in reaming the segmental fragment sufficiently. Insufficient canal filling of IM nail was found to have a significant odds ratio of 14.9 and 13.4 (p = 0.021, 0.039) in univariate and multivariate analysis of factors affecting nonunion, respectively (Table 3). Therefore, although there is difficulty in reaming for femur shaft segmental fracture, we suggest that surgeons consider using an IM nail with the largest possible diameter.
When the IM canal is insufficiently filled, it is necessary to increase the stability of the IM nail construct. Use of a blocking screw is one way to do this. Gao et al. and Ostrum et al. reported that inserting a blocking screw inhibits unstable fixation of the IM nail, thereby facilitating fracture healing25,26. In our study, there were only two cases in which a blocking screw was used since the segmental fragment was mainly located in the isthmus, and both cases resulted in uneventful union.
A residual gap, observed in 10 union cases (31.3%) in the union group but only five out of six nonunion cases (83.3%), was found to be another factor affecting with nonunion. This finding is consistent with the results of previous studies in which nonunion was more common with large interfragmentary gaps in comminuted femoral shaft fractures27,28,29, and in another study which reported a fracture site gap greater than 2 mm as a risk factor for nonunion21. Reducing the residual gap in femur shaft segmental fractures is suggested to be an important factor for obtaining favorable outcomes30,31. In all of nonunion patients in our study, only one side of the segment did not unite after operation. Therefore, we suggest that the strain on the proximal and distal portion of the segment might be different. However, the number of nonunion cases was insufficient to allow for evaluating the correlation between residual gap and strain. Further studies with larger numbers of segmental femoral fractures are necessary.
In some cases, using only a closed reduction method may not achieve satisfactory reduction of the segmental fragment. Therefore, in those cases we used minimally invasive percutaneous reduction techniques. For instance, cerclage wiring was performed in 12 cases (31.6%) and it improved the reduction quality and reduced the comminuted segment fracture gap. Although no difference in union rate or infection rate has been reported in open and closed IM nail fixations32, extra caution is needed when performing an open reduction to minimize soft tissue injury since segmental femoral shaft fracture is a high-energy injury. Other methods, such as various percutaneous reduction techniques and forward or backward striking techniques, are thought to be more advantageous than open reductions for reducing the residual gap30,31.
This study has some limitations. First, this was a retrospective study with a relatively small number of patients. Femoral segmental fractures are very rare, so it was difficult to recruit a large number of patients. Larger prospective studies are needed in the future. Second, although all surgeries were performed by trauma specialists using standard operative techniques, there was the potential for confounding since three surgeons were involved and different types of implants were used. We attempted to minimize bias by enrolling patients using strict inclusion criteria. Third, this study focused on radiographic outcomes rather than other clinical outcomes such as patient function or quality of life. Since this study was conducted on patients with non-articular fractures, we assumed that most of them would have no functional problems, and the retrospective nature of this study made it difficult to assess functional status. Also, clinical evaluation was difficult because there were many cases of insufficient follow-up after fracture union. The timing and degree of postoperative weight bearing may have influenced the nonunion rate. In our study, the effect of postoperative weight bearing on nonunion was minimized because we followed a staged rehabilitation protocol that included immediate postoperative range of motion exercises and progressive partial and full weight bearing based on the patient's pain tolerance.
Conclusions
In this study, femoral segment fractures showed a relatively high nonunion rate compared with non-segmental fractures. Factors affecting nonunion included insufficient canal filling of the IM nail and residual fracture gaps. Therefore, we suggest that use of larger diameter nails and taking steps to reduce the segment fracture gap are necessary in treatment of segmental femoral shaft fractures.
Data availability
The data presented in this study are available from the corresponding author on reasonable request.
References
Salminen, S. T., Pihlajamäki, H. K., Avikainen, V. J. & Böstman, O. M. Population based epidemiologic and morphologic study of femoral shaft fractures. Clin. Orthop. Relat. Res. 372, 241–249. https://doi.org/10.1097/00003086-200003000-00026 (2000).
Enninghorst, N., McDougall, D., Evans, J. A., Sisak, K. & Balogh, Z. J. Population-based epidemiology of femur shaft fractures. J. Trauma Acute Care Surg. 74, 1516–1520. https://doi.org/10.1097/TA.0b013e31828c3dc9 (2013).
Ricci, W. M., Gallagher, B. & Haidukewych, G. J. Intramedullary nailing of femoral shaft fractures: Current concepts. J. Am. Acad. Orthop. Surg. 17, 296–305. https://doi.org/10.5435/00124635-200905000-00004 (2009).
Meinberg, E. G., Agel, J., Roberts, C. S., Karam, M. D. & Kellam, J. F. Fracture and dislocation classification compendium-2018. J. Orthop. Trauma 32(Suppl 1), S1-s170. https://doi.org/10.1097/bot.0000000000001063 (2018).
Winquist, R. A., Hansen, S. T. Jr. & Clawson, D. K. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J. Bone Joint Surg. Am. 66, 529–539 (1984).
Johnson, K. D., Johnston, D. W. & Parker, B. Comminuted femoral-shaft fractures: Treatment by roller traction, cerclage wires and an intramedullary nail, or an interlocking intramedullary nail. J. Bone Joint Surg. Am. 66, 1222–1235 (1984).
Wiss, D. A., Brien, W. W. & Stetson, W. B. Interlocked nailing for treatment of segmental fractures of the femur. J. Bone Joint Surg. Am. 72, 724–728 (1990).
Wu, C. C., Shih, C. H., Ueng, W. N. & Chen, Y. J. Treatment of segmental femoral shaft fractures. Clin. Orthop. Relat. Res. 287, 224–230 (1993).
Avilucea, F. R., Yoon, R. S., Stinner, D. J., Langford, J. R. & Mir, H. R. Lower extremity fractures: Tips and tricks for nails and plates. Instr. Course Lect. 69, 433–448 (2020).
Wittauer, M. et al. Definition of long-bone nonunion: A scoping review of prospective clinical trials to evaluate current practice. Injury 52, 3200–3205. https://doi.org/10.1016/j.injury.2021.09.008 (2021).
Frölke, J. P. & Patka, P. Definition and classification of fracture non-unions. Injury 38(Suppl 2), S19-22. https://doi.org/10.1016/s0020-1383(07)80005-2 (2007).
Weber, B. & Cech, O. Pseudarthrosis, Pathology, Biomechanics, Therapy, Results (Hans Huber Medical Publisher, 1976).
Serrano, R. et al. Effect of nail size, insertion, and Δ canal-nail on the development of a nonunion after intramedullary nailing of femoral shaft fractures. J. Orthop. Trauma 33, 559–563. https://doi.org/10.1097/bot.0000000000001585 (2019).
Claes, L., Augat, P., Suger, G. & Wilke, H. J. Influence of size and stability of the osteotomy gap on the success of fracture healing. J. Orthop. Res. 15, 577–584. https://doi.org/10.1002/jor.1100150414 (1997).
Kubiak, E., Beebe, M., North, K., Hitchcock, R. & Potter, M. Early weight bearing after lower extremity fractures in adults. J. Am. Acad. Orthop. Surg 21, 727–738. https://doi.org/10.5435/JAAOS-21-12-727 (2013).
Basumallick, M. N. & Bandopadhyay, A. Effect of dynamization in open interlocking nailing of femoral fracture. A prospective randomized comparative study of 50 cases with a 2-year follow-up. Acta Orthop. Belg. 68, 42–48 (2002).
Karadimas, E. J., Papadimitriou, G., Theodoratos, G., Papanikolaou, A. & Maris, J. The effectiveness of the antegrade reamed technique: The experience and complications from 415 traumatic femoral shaft fractures. Strateg. Trauma Limb. Reconstr. 4, 113–121. https://doi.org/10.1007/s11751-009-0071-2 (2009).
Wu, C. C. & Chen, W. J. Healing of 56 segmental femoral shaft fractures after locked nailing. Poor results of dynamization. Acta Orthop. Scand. 68, 537–540. https://doi.org/10.3109/17453679708999022 (1997).
Ahn, J. C., Lee, D. D. & Cho, J. C. Treatment of the segmental fractures of the femoral shaft by intramedullary nailing. J. Korean Orthop. Assoc. 30, 686–693 (1995).
Lin, J. & Hou, S. M. Locked nailing of severely comminuted or segmental humeral fractures. Clin. Orthop. Relat. Res. 195–204, 2003. https://doi.org/10.1097/01.blo.0000038052.29678.ec (2003).
Ma, Y.-G., Hu, G.-L., Hu, W. & Liang, F. Surgical factors contributing to nonunion in femoral shaft fracture following intramedullary nailing. Chin. J. Traumatol. 19, 109–112. https://doi.org/10.1016/j.cjtee.2016.01.012 (2016).
Harper, M. C. Fractures of the femur treated by open and closed intramedullary nailing using the fluted rod. J. Bone Joint Surg. Am. 67, 699–708 (1985).
Tornetta, P. 3rd. & Tiburzi, D. Antegrade or retrograde reamed femoral nailing. A prospective, randomised trial. J. Bone Joint Surg. Br. 82, 652–654. https://doi.org/10.1302/0301-620x.82b5.10038 (2000).
Millar, M. J. et al. Nail fit: Does nail diameter to canal ratio predict the need for exchange nailing in the setting of aseptic, hypertrophic femoral nonunions?. J. Orthop. Trauma 32, 245–250. https://doi.org/10.1097/bot.0000000000001110 (2018).
Gao, K. D. et al. Treatment of aseptic diaphyseal nonunion of the lower extremities with exchange intramedullary nailing and blocking screws without open bone graft. Orthop. Surg. 1, 264–268. https://doi.org/10.1111/j.1757-7861.2009.00041.x (2009).
Ostrum, R. F. & Maurer, J. P. Distal third femur fractures treated with retrograde femoral nailing and blocking screws. J. Orthop. Trauma 23, 681–684. https://doi.org/10.1097/BOT.0b013e3181ad61f2 (2009).
Brinker, M. R. & O’Connor, D. P. The biological basis for nonunions. JBJS Rev. 4, 6. https://doi.org/10.2106/jbjs.Rvw.15.00078 (2016).
Calori, G. M., Albisetti, W., Agus, A., Iori, S. & Tagliabue, L. Risk factors contributing to fracture non-unions. Injury 38, S11–S18. https://doi.org/10.1016/S0020-1383(07)80004-0 (2007).
Rodriguez-Merchan, E. C. & Forriol, F. Nonunion: General principles and experimental data. Clin. Orthop. Relat. Res. 419, 4–12 (2004).
Lee, Q., Zeng, B. F., Luo, C. F., Wang, J. W. & Lu, N. J. Backstroke technique: An effective way to improve the healing of tibia fracture. Int. Orthop. 30, 329–332. https://doi.org/10.1007/s00264-006-0090-2 (2006).
Lim, S. J., So, S. Y., Yoon, Y. C., Cho, W. T. & Oh, J. K. A forward-striking technique for reducing fracture gaps during intramedullary nailing: A technical note with clinical results. Injury 46, 2507–2511. https://doi.org/10.1016/j.injury.2015.08.024 (2015).
Babalola, O. M. et al. Open Intramedullary nailing for segmental long bone fractures: An effective alternative in a resource-restricted environment. Niger. J. Surg. 22, 90–95. https://doi.org/10.4103/1117-6806.188983 (2016).
Author information
Authors and Affiliations
Contributions
I.K. organized the data, wrote the manuscript, and performed the statistical analysis. K.C.P. contributed to the study conception and design, organized the data, and wrote the manuscript. D.H.K. participated in writing this article in English. O.J.S. contributed in the revision process. K.T.H. conceptualized the study, participated in its design and helped to edit the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kook, I., Park, KC., Kim, DH. et al. A multicenter study of factors affecting nonunion by radiographic analysis after intramedullary nailing in segmental femoral shaft fractures. Sci Rep 13, 7802 (2023). https://doi.org/10.1038/s41598-023-34939-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34939-6
This article is cited by
-
Radiographic outcomes and non-union factor analysis in fragmentary segmental femoral shaft fractures (AO/OTA 32C3) treated with reamed antegrade nailing
Scientific Reports (2024)
-
Risk factors and healthcare costs associated with long bone fracture non-union: a retrospective US claims database analysis
Journal of Orthopaedic Surgery and Research (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.