Abstract
The prevalence of cesarean sections is rising rapidly and is becoming a global issue. Vaginal birth after a cesarean section is one of the safest strategies that can be used to decrease the cesarean section rate. Different fragmented primary studies were done on the success rate of vaginal birth after cesarean section and its associated factors in Ethiopia. However, the findings were controversial and inconclusive. Therefore, this meta-analysis was intended to estimate the pooled success rate of vaginal birth after cesarean section and its associated factors in Ethiopia. Pertinent studies were searched in PubMed, Google Scholar, ScienceDirect, direct open-access journals, and Ethiopian universities' institutional repositories. The data were analyzed using Stata 17. The Newcastle–Ottawa quality assessment tool was used to assess the quality of the studies. I squared statistics and Egger’s regression tests were used to assess heterogeneity and publication bias, respectively. A random effects model was selected to estimate the pooled success rate of vaginal birth after cesarean section and its associated factors. The PROSPERO registration number for this review is CRD42023413715. A total of 10 studies were included. The pooled success rate of vaginal birth after a cesarean section was found to be 48.42%. Age less than 30 years (pooled odds ratio (OR) 3.75, 95% CI 1.92, 7.33), previous history of vaginal birth (OR 3.65, 95% CI 2.64, 504), ruptured amniotic membrane at admission (OR 2.87, 95% CI 1.94, 4.26), 4 cm or more cervical dilatation at admission (OR 4, 95% CI 2.33, 6.8), a low station at admission (OR 5.07, 95% CI 2.08, 12.34), and no history of stillbirth (OR 4.93, 95% CI 1.82, 13.36) were significantly associated with successful vaginal birth after cesarean section. In conclusion, the pooled success rate of vaginal birth after a cesarean section was low in Ethiopia. Therefore, the Ministry of Health should consider those identified factors and revise the management guidelines and eligibility criteria for a trial of labor after a cesarean section.
Similar content being viewed by others
Introduction
Worldwide, the cesarean section (CS) rate has increased dramatically and has become an international concern1,2,3,4. In 2018, the overall CS rate was 21.1% in the world, 25.7% in Europe, 23.1% in Asia, 42.8% in Latin America and the Caribbean, and 9.2% in Africa3.
The CS rate was 29.5% in Ethiopia5. According to a meta-analysis study conducted in Ethiopia, CS has been associated with a high rate of maternal and neonatal morbidity and mortality, such as postpartum hemorrhage, severe anemia, surgical site infection, maternal mortality, perinatal asphyxia, neonatal sepsis, and early neonatal death5.
Various factors are contributing to the increasing cesarean section rates. Women's and families' preferences, health professionals' views and beliefs, and healthcare organizations and financial structures are some of the factors contributing to the rising CS rate3,4. In addition, the shifts in the obstetrics field, such as the decreased use of operative vaginal delivery, the decline in vaginal breech delivery, and the decreased use of vaginal birth after cesarean (VBAC), have increased the global CS rates1,5,6.
Several attempts have been made to reduce the CS rate1,7. VBAC is one of the best strategies that can be used to decrease the CS rate and is associated with a lower incidence of maternal and neonatal morbidity and mortality as compared to repeat CS2,8,9,10,11,12. A successful trial of labor after cesarean (TOLAC) reduces the risk of blood loss, hysterectomy, and associated puerperal infections13. However, unsuccessful TOLAC increases the above-mentioned maternal morbidity, uterine rupture, and adverse perinatal outcomes14,15,16.
The success rates of VBAC vary widely in different countries, with a global success rate ranging from 60 to 80%17,18. It was around 80.7% in Taiwan19, 63.4% in the UK20, 73% in Iraq1, 72.1% in Pakistan13, 57.6% in the DRC21, and 61.7% in Nigeria6.
The success rate of VBAC is influenced by several factors. Some of the factors were the service provider's choice, cervical dilatation, prior vaginal delivery, younger maternal age, indication for previous CS, fetal weight, obesity, diabetes, gestational age, and hypertensive disorders complicating pregnancy14,16,17,21,22,23.
Although different fragmented primary studies were done in different district areas of Ethiopia, the overall success rate of VBAC is unknown. In addition, the success rate of VBAC obtained from those primary studies was widely variable, ranging from 35.07 to 69.4%24,25. Furthermore, the associated factors for VBAC found in those studies were controversial and inconclusive. Therefore, this meta-analysis was conducted to estimate the pooled success rate of VBAC and its associated factors in Ethiopia. The findings of this study may enable policymakers to design strategies for improving the success rate of vaginal birth after a cesarean section. The results of this study may also help obstetric care providers by enabling them to deliver evidence-based counseling on VBAC, which has a major impact on averting repeated CS.
Methods
Sources of information and search strategies
This review was carried out following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guideline26 (Table S1). The protocol was registered in PROSPERO. The PROSPERO registration number for this review is CRD42023413715. We used PubMed, Google Scholar, ScienceDirect, and direct open-access journal (DOAJ) databases to find relevant studies. Initially, studies were exhaustively searched by using the full title ("Vaginal birth after cesarean section and its associated factors in Ethiopia") and keywords ("success rate," "successful," "vaginal birth after a cesarean section", "vaginal delivery after the cesarean section", "trial of labor after the cesarean section", "determinants", "associated factors", "predictors", "Ethiopia"). These keywords were connected using the Boolean operators ("OR" and/or "AND"). Besides this, reference lists of all included studies were assessed to find missed studies. Moreover, unpublished studies were searched in Ethiopian universities’ institutional repositories, mainly at the University of Gondar, Jimma, Addis Ababa, and Haramaya. The search details for PubMed were as follows: ("Successful" [All Fields] OR "Success rate" [All Fields]) AND ("vaginal birth after cesarean" [All Fields] OR "vaginal birth after cesarean" [MeSH Terms] OR ("vaginal"[All Fields] AND "birth"[All Fields] AND "after"[All Fields] AND "cesarean"[All Fields]) OR "vaginal birth after cesarean"[All Fields]) AND section[All Fields] AND ("determinants"[All Fields] OR "associated factors" [All fields] OR "Predictors" [All Fields]) AND ("Ethiopia"[MeSH Terms] OR "Ethiopia" [All Fields]). The search period was between 2005/01/01 and 2022/11/20 (Table S2).
Eligibility criteria
The authors followed CoCoPop approaches (condition, context, and population) to establish search strategies and identify eligible studies.
Inclusion criteria: This systematic review and meta-analysis included articles that fulfilled the following criteria:
-
Condition (Co): We included studies that examined at least one or more of the following key outcomes: (1) success rate of vaginal birth after cesarean section; (2) determinants or associated factors of successful VBAC
-
Context (Co): We included studies that were conducted in Ethiopia.
-
Population (Pop): Studies that were done among laboring mothers with previous cesarean sections
-
Study design: Cross-sectional and case–control studies
-
Publication condition: Both published and unpublished studies
-
Language: We included all studies written in the English language.
Exclusion criteria: We excluded studies that had a different outcome of interest.
Outcome measurement
This meta-analysis study has two outcomes, namely, the success rate of vaginal birth after cesarean section and its associated factors.
Station: It refers to the relationship of the fetal head's lowermost portion in the pelvic canal with the ischial spines or indicates the degree of engagement of the presenting part. The station above the ischial spine was categorized as high (0), and the station below the ischial spine was categorized as low (> 0) in the pelvic examination24.
Heterogeneity: We used the following cut points to define the level of heterogeneity: When I-squared (I2) is zero, there is no heterogeneity; if the value is 25%, there is mild heterogeneity; if the value is 50%, there is moderate heterogeneity; if the value is 75%, there is high heterogeneity; and if the value is 100%, there is substantial heterogeneity.
Study selection, quality assessment, and data extraction process
All retrieved studies were exported to Endnote Version 7 software for screening. After the removal of duplicate studies, the remaining studies were evaluated for their relevance, accessibility of full text, outcomes of interest, and quality score. Finally, those studies that fulfilled the inclusion criteria and had high-quality scores were included.
The Newcastle–Ottawa quality assessment tool adapted for cross-sectional and case–control studies was used to assess the quality of the studies28. Two authors (DA and YB) assessed the quality of the studies individually. Disparities at the time of quality assessment were resolved through discussion and consensus by involving the third reviewer (NG). Finally, articles that received a score of 7 points out of 10 possible points for cross-sectional and case–control studies were considered high-quality and included in this study (Table S3).
Regarding data extraction, all the necessary data were extracted by two reviewers (DA and SB) using Microsoft Excel. The Excel contains the following components: The first author’s name, publication year, study region, study setting, study period, sample size, the success rate of VBA, and an adjusted odds ratio (AOR) with a 95% confidence interval for significant risk factors of successful VBAC.
Statistical analysis
The data were analyzed using Stata version 17. A random effects model was selected to determine the pooled success rate of vaginal birth after a cesarean section and its associated factors27,28,29. Subgroup analysis and sensitivity analysis were conducted to identify the source of heterogeneity. Finally, publication bias was assessed by using Egger’s regression test30.
Results
Search results
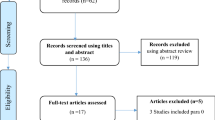
A total of 360 studies were searched from different international databases and Ethiopian universities' institutional repositories. All the retrieved studies were transferred to Endnote 7 reference manager for screening. Then a total of 325 studies were removed due to irrelevant articles, duplication, and different outcomes of interest. Lastly, 10 studies that fulfilled the inclusion criteria were included (Fig. 1).
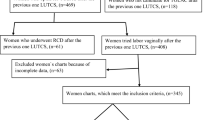
Characteristics of included studies
This meta-analysis included a total of 10 studies with 2588 study participants24,25,31,32,33,34,35,36,37. Among these, five were cross-sectional studies24,25,34,36 and the remaining were case–control studies31,32,33,35,37. Concerning geographical distribution, four regions and one administrative City, namely, the Oromia region, the South Nation Nationalities and Peoples Region (SNNPR), the Amhara region, the Harar region, and Addis Ababa administrative City, were represented (Table 1).
The pooled success rate of vaginal birth after cesarean section in Ethiopia
Five primary studies were included to determine the pooled success rate of vaginal birth after a cesarean section24,25,34,36,38. The pooled success rate of vaginal birth after a cesarean section was 48.42 with a 95% CI of 35.72 to 61.1. A marked type of heterogeneity was detected across the studies (I2 = 95.7%). The highest rate of successful vaginal birth after a cesarean section was reported by Misgan et al.25, while the lowest success rate of VBAC was reported by Derebe et al.24 (Fig. 2).
Subgroup analysis
Subgroup analysis was done to identify the source of heterogeneity and minimize the random variations between the point estimates of primary studies and pooled success rate of VBAC by using sample size, publication status, and study period. However, heterogeneity was still observed between the studies. The overall success rate of VBAC was found to be 54.22% in published studies, 55.57% in studies with a sample size of less than 300, and 48.45% in studies conducted after 2018 (Table 2).
Sensitivity analysis
Sensitivity analysis was done to check the influences of individual studies on the overall success rate of VBAC. There was no significant influence of individual studies on the pooled success rate of VBAC. When Derebe et al. and Misgan et al. were excluded from the analysis, the pooled success rate of VBAC was found to be high and low, with success rates of 51.82% and 42.67%, respectively (Table 3).
Publication bias
Publication biases were assessed objectively by using Egger’s regression test, and the results indicated that there was no publication bias or small study effect between the studies (p-value = 0.683).
Factors associated with successful vaginal delivery after cesarean section
A total of nine studies reported one or more associated factors for successful VBAC. The most common factors reported by the majority of studies were a history of vaginal birth, a ruptured amniotic membrane at admission, and a cervical dilatation of four or more centimeters at admission (Table 4).
The relationship between cervical dilation at admission and vaginal birth after cesarean section: The effect of cervical dilation at admission on successful vaginal birth after a cesarean section was evaluated using six studies24,25,31,34,35,36. In this study, cervical dilation of more than or equal to 4 cm at admission was found to be significantly associated with a successful vaginal birth after a cesarean section. Those mothers with cervical dilation ≥ 4 cm at admission were four times more likely to have a successful VBAC (pooled odds ratio 4, 95% CI 2.33, 6.8) (Fig. 3).
The association between ruptured amniotic membrane at admission and VBAC: Three primary studies were used to determine the relationship between ruptured membranes and successful VBAC24,25,33. The result revealed that ruptured amniotic membranes at admission were significantly associated with successful VBAC. Those mothers who had a rupture of the amniotic membrane at admission were 2.87 times more likely to have a successful VBAC (pooled odds ratio 2.87, 95% CI 1.94, 4.26) (Fig. 4).
The association between having a low station at admission and successful VBAC: The association between having a low station at admission (station ≥ 0) and successful VBAC was examined using three studies24,31,37. The result indicated that having a low station at admission was significantly associated with a successful VBAC. Mothers who had a low station at admission were 5.11 times more likely to have a successful VBAC than mothers with a high station (pooled odds ratio 5.07, 95% CI 2.08, 12.34) (Fig. 5).
The association between previous history of vaginal delivery and successful VBAC: Five studies were used to investigate the relationship between previous vaginal delivery history and successful VBAC24,32,33,34,35. This study discovered that a previous history of vaginal birth was significantly associated with a successful VBAC. Those mothers with a previous history of vaginal delivery were 3.65 times more likely to have a successful vaginal birth after a cesarean section (pooled odds ratio 3.65, 95% CI 2.64, 504) (Fig. 6).
The association between no history of stillbirth and successful VBAC: Three primary studies were used to examine the relationship between no history of stillbirth and successful VBAC31,32,37. The result showed that mothers with no history of stillbirth were 4.93 times more likely to have a successful VBAC than mothers with a history of stillbirth (pooled odds ratio 4.93, 95% CI 1.82, 13.36) (Fig. 7).
The association between maternal age and successful VBAC: Finally, we used two studies to examine the relationship between maternal age below 30 years and successful VBAC24,35. This study found that maternal age under 30 years was significantly associated with successful VBAC. Those mothers whose age was less than 30 years were 3.75 times more likely to have a successful VBAC as compared to those with older age (pooled odds ratio 3.75, 95% CI 1.92, 7.33) (Fig. 8).
Discussion
This meta-analysis assessed the pooled success rate of VBAC and its associated factors in Ethiopia. To the best of our knowledge, this research is the first of its type in Ethiopia to examine the overall success rate of VBAC and the contributing factors.
The pooled success rate of VBAC was found to be 48.42% with a 95% CI of 35.72 to 61.1. This finding was lower than a study finding in Australia (64.4%)39, the UK (63.4%)20, and China (84%)22. This finding was also lower than a finding of a meta-analysis study in developed countries40. The variation in the success rate of VBAC across countries could be due to differences in hospital settings or eligibility criteria for a trial of labor after a cesarean section. Furthermore, the higher success rate of VBAC in the previous studies might be due to the availability of advanced labor monitoring machines, which might decrease the unnecessary repeated CS. In addition, the discrepancies might be due to the variations in the management modalities for labor abnormalities among those mothers who had TOLAC. In our country, CS is the only treatment option for prolonged labor secondary to poor uterine contractions among those mothers who had a TOLAC.
The finding of this study was also lower than the finding of a meta-analysis study in Sub-Saharan African countries, which has a 69% success rate of VBAC41. The variation in the success rate of VBAC might be due to disparities in sample size, where the previous study used several primary studies and a large sample size as compared to our study. In addition, discrepancies in the threshold level for TOLAC, intrapartum fetal monitoring, and quality of health services between the countries might contribute to this difference.
The finding of this study revealed that having a ruptured amniotic membrane at admission was significantly associated with successful VBAC. This finding was supported by a study finding in China22. This could be explained by the release of natural prostaglandins during the rupture of the amniotic membrane. Prostaglandin facilitates the progress of labor and decreases the chance of labor abnormalities, mainly poor uterine contractions42.
This study also found a strong association between previous history of vaginal delivery and successful VBAC. This finding is in agreement with a study finding in China22, Turkey23, and Thailand14. This finding is also in agreement with a meta-analysis study, which revealed that the history of previous vaginal deliveries is one of the most important factors for the success of VBAC40. The possible reason could be due to good psychological readiness and awareness of the advantage of vaginal delivery in those mothers with a history of vaginal delivery.
This study also found a strong association between a cervical dilatation of four centimeters or more at admission and a successful VBAC. Evidence from Pakistan13 and Nigeria6 supports the current finding. This might be because obstetric care providers usually encourage TOLAC when cervical dilatation is more than or equal to 4 cm. Furthermore, those mothers who are in the active phase of labor might have better progress of labor that results in successful VBAC as compared to the latent first stage of labor.
Maternal age below 30 years was also significantly associated with successful VBAC. Evidence from the meta-analysis study supports the present finding and revealed that younger women, especially those 35 years old, are more likely to have a successful and safe VBAC40. Another study also reported that maternal age of above 30 years was independently associated with Failed TOLAC43. This may be because older mothers are less likely to attempt TOLAC due to a fear of urine rupture.
Furthermore, we found a strong association between a low station at admission and a successful VBAC. This finding was supported by a previous study that reported that women who had a station lower than − 1 were significantly associated with successful VBAC44,45.
Lastly, no history of stillbirth was significantly associated with a successful VBAC. Evidence revealed that a history of fetal complications or adverse birth outcomes in the previous pregnancy increased the cesarean delivery rate46. Previous history of stillbirth during labor could influence women's preferences on the mode of delivery and the obstetric care provider's decision to halt or continue a vaginal birth in women with a history of cesarean section1.
This study has some limitations. The lack of studies from some regions might affect the generalizability of this study. Furthermore, the presence of heterogeneity across the studies might affect the pooled success rate of VBAC.
Conclusion
The overall success rate of VBAC was low in Ethiopia. A successful VBAC was significantly associated with a history of vaginal birth, a ruptured amniotic membrane at admission, a low station at admission, age less than 30 years, cervical dilatation of four or more centimeters at admission, and no history of stillbirth. Therefore, the Ministry of Health should consider those identified factors and revise the management guidelines and eligibility criteria for TOLAC. Moreover, obstetric care providers should prevent repeated CS by providing appropriate antenatal counseling regarding influencing factors for VBAC and the chance of achieving a successful VBAC.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials. Furthermore, the corresponding author (DA) will be contacted if someone wants to request the data from this study.
Abbreviations
- CS:
-
Cesarean section
- ES:
-
Effect size
- OR:
-
Odds ratio
- SNNPR:
-
Southern Nations, Nationalities, and Peoples Region
- TOLAC:
-
Trial of Labor after Cesarean section
- VBAC:
-
Vaginal Birth after Cesarean section
References
Razzak, M. A. A., Hamdan, M. N. A. & Abutiheen, A. A. K. The success rate of vaginal birth after cesarean section in Kerbala maternity hospital. Iraq Med. J. 2(1), 32–35 (2018).
Dalal, M. et al. Maternal and neonatal outcome in pregnancy with previous lower segment cesarean section undergoing a trial of scar. Int. J. Reprod. Contracept. Obstet. Gynecol. 10(9), 3435 (2021).
Betran, A. P., Ye, J., Moller, A.-B., Souza, J. P. & Zhang, J. Trends and projections of cesarean section rates: Global and regional estimates. BMJ Glob. Health 6(6), e005671 (2021).
Betran, A. P. et al. Interventions to reduce unnecessary cesarean sections in healthy women and babies. The Lancet. 392(10155), 1358–1368 (2018).
Gedefaw, G. et al. Prevalence, indications, and outcomes of cesarean section deliveries in Ethiopia: A systematic review and meta-analysis. Patient Saf. Surg. 14(1), 1–10 (2020).
Adewole, A. et al. Delivery outcome and predictors of successful vaginal birth after primary cesarean delivery: A comparative study: Vaginal birth after cesarean section. Babcock Univ. Med. J. 5(1), 1–10 (2022).
Ugwu, G. O., Iyoke, C. A., Onah, H. E., Egwuatu, V. E. & Ezugwu, F. O. Maternal and perinatal outcomes of delivery after a previous Cesarean section in Enugu, Southeast Nigeria: A prospective observational study. Int. J. Womens Health. 6, 301–305 (2014).
Ansari, N. et al. Factors associated with vaginal birth after previous C-section in pregnant women. Pak. J. Med. Health Sci. 16(04), 564 (2022).
Tahseen, S. & Griffiths, M. Vaginal birth after two cesarean sections (VBAC-2)—A systematic review with meta-analysis of success rate and adverse outcomes of VBAC-2 versus VBAC-1 and repeat (third) cesarean sections. BJOG Int. J. Obstet. Gynaecol. 117(1), 5–19 (2010).
Yang, Y.-Z., Ye, X.-P. & Sun, X.-X. Maternal and neonatal morbidity: Repeat Cesarean versus a trial of labor after previous Cesarean delivery. Clin. Investig. Med. E135–E45 (2017).
Gupta, P., Jahan, I. & Jograjiya, G. R. Is vaginal delivery safe after previous lower-segment cesarean section in a developing country?. Niger. Med. J. J. Nigeria Med. Assoc. 55(3), 260 (2014).
Lundgren, I. et al. Clinicians’ views of factors of importance for improving the rate of VBAC (vaginal birth after cesarean section): A study from countries with low VBAC rates. BMC Pregnancy Childbirth 16(1), 1–10 (2016).
Siddiqui, S. A. Obstetric factors for unsuccessful trial of labor in second-order birth following previous cesarean. Ann. Saudi Med. 33(4), 356–362 (2013).
Thapsamuthdechakorn, A., Sekararithi, R. & Tongsong, T. Factors associated with successful trial of labor after cesarean section: A retrospective cohort study. J. Pregnancy. 2018 (2018).
Frass, K. & AlHarazi, A. Outcome of vaginal birth after cesarean section in women with one previous section and spontaneous onset of labor. EMHJ East. Mediterr. Health J. 17(8), 646–650 (2011).
Tsai, H.-T. & Wu, C.-H. Vaginal birth after cesarean section—The world trend and local experience in Taiwan. Taiwan. J. Obstet. Gynecol. 56(1), 41–45 (2017).
Minh, T. & Phuoc, H. The success rate and associated factors of vaginal birth after cesarean section at Tu Du Hospital in Vietnam. Int. J. Pregnancy Child Birth 4(3), 129–133 (2018).
Landon, M. B., Grobman, W. A., Health EKSNIoC, editors. What we have learned about the trial of labor after cesarean delivery from the maternal-fetal medicine units cesarean registry. Seminars in perinatology. Elsevier (2016).
Li, W.-H. et al. Vaginal birth after cesarean section: 10 years of experience in a tertiary medical center in Taiwan. Taiwan. J. Obstet. Gynecol. 55(3), 394–398 (2016).
Knight, H. et al. Vaginal birth after cesarean section: A cohort study investigating factors associated with its uptake and success. BJOG Int. J. Obstet. Gynaecol. 121(2), 183–192 (2014).
Maroyi, R. et al. Factors associated with successful vaginal birth after a primary cesarean section in women with an optimal inter-delivery interval. Int. J. Womens Health 13, 903–909 (2021).
Li, Y.-X. et al. Predicting the success of vaginal birth after cesarean delivery: A retrospective cohort study in China. BMJ Open 9(5), e027807 (2019).
Senturk, M. B., Cakmak, Y., Atac, H. & Budak, M. S. Factors associated with successful vaginal birth after cesarean section and outcomes in the rural area of Anatolia. Int. J. Womens Health 7, 693–697 (2015).
Derebe, T., Mulat, A., Mihiret, M., Feyisa, W., Tebabal, A., Wubet, T., et al. Factors associated with successful vaginal birth after lower uterine transverse cesarean section delivery in public hospitals of Bahir Dar City, Northwest, Ethiopia (2022).
Misgan, E., Gedefaw, A., Negash, S. & Asefa, A. Validation of a vaginal birth after cesarean delivery prediction model in teaching hospitals of Addis Ababa University: A cross-sectional study. BioMed Res. Int. 2020, 1540460 (2020).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 8(5), 336–341 (2010).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ (Clin. Res. Ed.) 327(7414), 557–560 (2003).
Borenstein, M., Hedges, L. V., Higgins, J. P. & Rothstein, H. R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synthesis Methods 1(2), 97–111 (2010).
DerSimonian, R. & Kacker, R. Random-effects model for meta-analysis of clinical trials: An update. Contemp. Clin. Trials 28(2), 105–114 (2007).
Peters, J. L., Sutton, A. J., Jones, D. R., Abrams, K. R. & Rushton, L. Comparison of two methods to detect publication bias in meta-analysis. JAMA 295(6), 676–680 (2006).
Birara, M. & Gebrehiwot, Y. Factors associated with the success of vaginal birth after one cesarean section (VBAC) at three teaching hospitals in Addis Ababa, Ethiopia: A case–control study. BMC Pregnancy Childbirth 13(1), 1–6 (2013).
Dereje, L., Tilahun, T. & Markos, J. Determinants of successful trial of labor after a previous cesarean delivery in East Wollega, Western Ethiopia: A case–control study. SAGE Open Med. 10, 20503121221097596 (2022).
Girma, H. T., Mekonnen, H., Sendo, E. G. & Deressa, J. T. Factors associated with successful vaginal birth after cesarean section and its outcome in Asella Referral and Teaching Hospital, Ethiopia. Int. J. 7(1), 39 (2021).
Girma, Y., Menlkalew, Z. & Destaw, A. Vaginal delivery after cesarean section and its associated factors in Mizan Tepi University Teaching Hospital, Southwest Ethiopia. Heliyon 7(11), e08276 (2021).
Mekonnin, F. & Bulto, G. Determinants of successful vaginal birth after caesarean section at public hospitals in Ambo Town, Oromia Region, Central Ethiopia: A case–control study. Risk Manag. Healthc. Policy 14, 4083–4091 (2021).
Siraneh, Y., Assefa, F. & Tesfaye, M. Feto-maternal outcome of vaginal birth after cesarean and associated factors among mothers with previous cesarean scar at Attat Lord Merry Primary Hospital, Gurage Zone, South Ethiopia. J. Pregnancy Child Health 5(5), 390 (2018).
Tefera, M., Assefa, N., Teji Roba, K. & Gedefa, L. Predictors of success of trial of labor after cesarean section: A nested case–control study at public hospitals in Eastern Ethiopia. Womens Health 17, 17455065211061960 (2021).
Kumbi, A., Asefa, D. & Hiko, D. Incidence and outcomes of pregnancies among pregnant mothers with a previous cesarean scar in Jimma University specialized hospital southwest Ethiopia (2014).
Gardner, K., Henry, A., Thou, S., Davis, G. & Miller, T. Improving VBAC rates: The combined impact of two management strategies. Aust. N. Z. J. Obstet. Gynaecol. 54(4), 327–332 (2014).
Wu, Y., Kataria, Y., Wang, Z., Ming, W.-K. & Ellervik, C. Factors associated with successful vaginal birth after a cesarean section: A systematic review and meta-analysis. BMC Pregnancy Childbirth 19(1), 1–12 (2019).
Boulvain, M., Fraser, W. D., Brisson-Carroll, G., Faron, G. & Wallast, E. Trial of labor after cesarean section in sub-Saharan Africa: A meta-analysis. BJOG Int. J. Obstet. Gynaecol. 104(12), 1385–1390 (1997).
Fishel Bartal, M. et al. Trial of labor after cesarean (TOLAC) in women with premature rupture of membranes. J. Matern. Fetal Neonatal Med. 33(17), 2976–2982 (2020).
Parveen, S., Rengaraj, S. & Chaturvedula, L. Factors associated with the outcome of TOLAC after one previous cesarean section: a retrospective cohort study. J. Obstet. Gynaecol. 42(3), 430–436 (2022).
Rottenstreich, A. et al. Fetal head station at second-stage dystocia and subsequent trial of labor after cesarean delivery success rate. Obstet. Gynecol. 137(1), 147–155 (2021).
Durnwald, C. P. & Mercer, B. M. Vaginal birth after Cesarean delivery: Predicting success, risks of failure. J. Matern. Fetal Neonatal Med. 15(6), 388–393 (2004).
Gondwe, T. et al. Maternal factors associated with mode of delivery in a population with a high cesarean section rate. J. Epidemiol. Glob. Health 9(4), 252 (2019).
Acknowledgements
Not applicable.
Funding
Not applicable.
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Addisu, D., Gebeyehu, N.A., Biru, S. et al. Vaginal birth after cesarean section and its associated factors in Ethiopia: a systematic review and meta-analysis. Sci Rep 13, 7882 (2023). https://doi.org/10.1038/s41598-023-34856-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34856-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.