Abstract
There are prevalent financial relationships between dermatologists and pharmaceutical companies in Japan. However, little was known about the extent of whole picture of the personal payments made to dermatologists by pharmaceutical companies. This study aimed to examine the personal payments to the board-certified dermatologists by the Japanese Dermatological Association from the pharmaceutical companies between 2016 and 2019. Using the publicly disclosed payments data by the pharmaceutical companies between 2016 and 2019, we evaluated the magnitude, prevalence, and trends in the personal payments made to all board-certified dermatologists for the lecturing, writing, and consulting compensations. The payments were descriptively analyzed overall and by dermatologist demographics. Additionally, the payment trends were assessed by generalized estimating equation models. Of 6883 active board-certified dermatologists, 3121 (45.3%) received a total of $33,223,806 personal payments between 2016 and 2019. The median per-physician payments and number of payments (interquartile range) were $1737 ($613–$5287) and 4.0 (2.0–10.0) over the 4 years, respectively. Only top 1%, 5%, 10% of dermatologists received 41.7% (95% confidence interval [CI] 38.2–45.1%), 76.9% (95% CI 74.7–79.1%), and 87.6% (95% CI 86.2–88.9%) of overall payments. The number of dermatologists receiving payments and per-dermatologist payments increased by 4.3% (95% CI 3.1‒5.5%, p < 0.001) and 16.4% (95% CI 13.5‒19.4%, p < 0.001) each year. The board-certification in dermatology-oncology, in cosmetic dermatology, and male sex were significantly associated with higher personal payments with relative monetary values of 2.29 (95% CI 1.65–3.19, p < 0.001), 3.16 (95% CI 1.89–5.26, p < 0.001), and 5.38 (95% CI 4.12–7.04, p < 0.001). Less than half of Japanese board-certified dermatologists received lower personal payments from the pharmaceutical companies than those to other specialists. However, these personal payments were increasingly more prevalent and greater over the 4 years.
Similar content being viewed by others
Introduction
Financial collaboration between physicians and pharmaceutical companies can benefit patients by deepening understanding of illnesses and developing their new diagnostic methods and treatments, but also harm patient care by expensive and inappropriate prescriptions, biasing guideline recommendations favorable for pharmaceutical industry, and jeopardizing results and interpretations of clinical trial. In response to public call for greater transparency in the physician-industry financial relationships, transparency acts and guidelines were developed and the financial transfers made by pharmaceutical companies to physicians were publicly disclosed in many developed countries, such as the Physician Payment Sunshine Act and the Open Payments Database in the United States1,2. In Japan, instead of legislative regulation, Japan Pharmaceutical Manufacturers Association (JPMA), the largest trade organizations of major pharmaceutical companies in Japan, published a transparency guidance and the payments for lecturing, consulting, and writing compensations to physicians have been voluntarily disclosed by each pharmaceutical company affiliated to the JPMA since 20133.
Due to this payment disclosure, we previously reported there were substantial and prevalent financial relationships between pharmaceutical companies and physicians in several specialties including oncology, hematology, pediatrics, infectious diseases, and pulmonology in Japan4,5,6,7,8. These personal payments were often made to physicians in authoritative and influential positions such as clinical practice guideline authors6,9,10,11,12, society board members6,13, university professors6,7,14, and television expert commentators15. We also found that there was a pattern in recipient of personal payments by factors such as gender and regions.
Among several specialties, dermatologists have had strong financial ties to the pharmaceutical companies in Japan. Indeed, executive board members of the Japanese Dermatological Association (JDA) received the second highest payments in the median amounts among those representing 18 major clinical medicine specialties in Japan13. Additionally, 90.6% of the JDA clinical practice guideline authors received $10,281 in median personal payments between 2016 and 201716. In 13 out of 32 (40.6%) JDA guidelines, all authors accepted personal payments from the pharmaceutical companies16. These payments were disproportionately distributed to physicians by the demographic differences including gender16.
Additionally, a previous study assessing patients’ awareness and perception of financial relationships between physicians and pharmaceutical companies demonstrated that the majority of patients expect physicians to be transparent about their financial conflicts of interest with pharmaceutical companies and to minimize the non-research financial relationships such as speaking fees, gifts and meals from pharmaceutical companies in Japan17. Growing body of evidence mostly from the United States and other developed countries show that the non-research payments to physicians significantly influence physicians’ prescribing patterns leading to increased prescriptions and healthcare costs18,19,20,21,22,23,24,25. Reducing these non-research payments to physicians might lead to more proper and balanced care, as well as greater transparency and independence of physicians. Thus, as a first step towards the above goal, the investigation of financial relationships between physicians and pharmaceutical companies is of particular importance for all patients, healthcare professionals, and policymakers.
Nevertheless, there was no document describing the whole magnitude and prevalence of dermatologists accepting personal payments from the pharmaceutical companies in Japan. Considering that 8333, equal to 73.7% of all dermatologists, received more than $34 million in the United States in 201426, we hypothesized that there were substantial and prevalent financial relationships between dermatologists and pharmaceutical companies in Japan. This study purposed to evaluate magnitude, prevalence, and trends in personal payments from pharmaceutical companies to dermatologists in Japan for the recent years.
Methods
Study design and participants
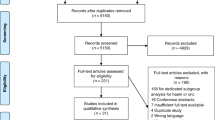
This cross-sectional analysis examined the personal payments for the lecturing, consulting, and writing proposes made to board-certified dermatologists by the JDA from the JPMA member companies between 2016 and 2019. The board certification in dermatology was one of the nineteen basic specialties in Japan.
This study included all dermatologists board-certified by the JDA as of September 30, 2021. The JDA was established in 1900 and the largest and sole professional medical association certifying dermatologists in Japan. Names, affiliations, JDA-certified specialist certification in dermatology-oncology or cosmetic dermatology, and gender of all board-certified dermatologists were publicly available from the JDA webpage (https://www.dermatol.or.jp/modules/spMap/doctors?pref=&sp=1&words =).
Data collection
The payment data considering lecturing, consulting, and writing compensations were disclosed at individual level by the pharmaceutical companies. Definitions of payment categories were described previously5,6. We collected payment data from all 92 pharmaceutical companies belonging to the JPMA to the board-certified dermatologists between 2016 and 2019, sorting by dermatologists’ names, as described previously7,12,16. The payments in 2019 were the latest analyzable payment data as of August 2022. The payment recipients’ affiliations were matched to the JDA-reported dermatologists’ affiliation, in order to delete payment data to different person with duplicate name27. As for a payment which we could not verify, we excluded the payment from the analysis. The detailed procedure was noted previously5,11,28. Information on whether dermatologists work in facilities accredited by the JDA for the use of biologics was collected from the JDA webpage.
Analysis
We performed descriptive analysis on the payment data including average (standard deviation [SD]) and median (interquartile range [IQR]) payments and number of payments. Per-physician payments were calculated based on dermatologists receiving payments, as in other studies2,26,29. Payment concentration were evaluated by the Gini index and the shares of the value of payments held by the top 1%, 5%, 10%, and 25% of dermatologists. The Gini index ranges from 0 to 1, and the greater the Gini index, the greater the disparity in the distribution of payments on the specialist basis11. Additionally, the trends in annual personal payments to dermatologists were examined by population-averaged generalized estimating equation (GEE) models with panel-data of payments clustering each dermatologist between 2016 and 20195,6. The log-linked linear GEE model with Poisson distribution for the number of dermatologists receiving payments and negative binomial regression GEE model for the per-dermatologist payments were applied, as the payments were highly skewed. As several pharmaceutical companies disaffiliated from or newly affiliated to the JPMA between 2016 and 2019, the payment trends in industry payments were calculated based on the payments from the companies continuously affiliated with JPMA throughout the 4 years. Separately, we examined the associations between (1) the 4-year total payment amounts and (2) the likelihood of dermatologists to receive payments and the dermatologist demographic characteristics using (1) a multivariable negative binomial model and (2) a modified log-linked Poisson regression model, respectively. Gender, whether a dermatologist had board-certification in dermatology-oncology or cosmetic dermatology, practicing regions, and whether a dermatologist works in facilities accredited by the JDA for the use of biologics were set as independent variables, and the number of dermatologists receiving payments and per-dermatologist payment values were set as dependent variables, respectively29,30,31. Japanese yen (¥) was converted into dollars ($) using 2019 average monthly exchange rate of ¥109.0 per $1, respectively. All analyses were conducted using Microsoft Excel, version 16.0 (Microsoft Corp) and Stata version 17.0 (StataCorp).
Ethical approval
The Ethics Committee of the Medical Governance Research Institute approved this study. This study is a retrospective cross-sectional analysis of publicly available information so informed consent from participants were waived by the Ethics Committee of the Medical Governance Research Institute. This study was performed in accordance with relevant guidelines/regulations.
Results
There were 6883 board-certified dermatologists by JDA including 3556 (51.7%) male, 92 (1.3%) dermatology-oncology specialists, and 49 (0.7%) cosmetic dermatology specialists. Of 6883 board-certified dermatologists by JDA, 3121 (45.3%) received 43,475 personal payments totaling $33,223,806 between 2016 and 2019. The median per-physician payments, number of payments, and number of companies making payments were $1737 (IQR $613–$5287), 4.0 (IQR 2.0–10.0), and 3.0 (IQR 1.0–6.0) over the 4 years, respectively (Table 1) The number of dermatologists receiving more than $10,000, $50,000, and $100,000 in the 4-year combined total were 511 (7.4%), 159 (2.3%), and 72 (1.1%), respectively. Only top 1%, 5%, 10% of dermatologists received 41.7%, 76.9%, and 87.6% of overall payments. Gini index for per-physician 4-year total payments was 0.917, indicating that only a small number of dermatologists received substantial amounts of personal payments from the pharmaceutical companies. Of 3121 dermatologists with payments, 68.3% (2133 dermatologists) received payments from more than one company.
As for payment categories, lecturing payments occupied 81.2% in monetary amounts and 84.5% of all payments in the number of payments. (Table 2) Consulting payments were the highest per-payment value with an average of $1009, while the lecturing payment was the lowest per-payment value with $735. Among 6883 dermatologists, 2954 (42.9%), 1210 (17.6%), and 533 (8.0%) received one or more payments for lecturing, consulting, and writing compensations from the pharmaceutical companies over the 4 years.
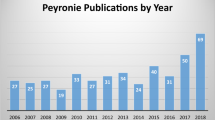
Table 3 shows the annual trends in personal payments to the dermatologists between 2016 and 2019. The total personal payments increased from $6,507,920 in 2016 to $9,536,625 in 2018, and $9,422,603 in 2019. The number of dermatologists receiving payments also increased by 4.3% (95% CI 3.1‒5.5%, p < 0.001) annually, from 1800 (26.2%) in 2016 to 2042 (29.7%) in 2018. Median annual personal payments per dermatologist were the highest in 2018, with $1046 (IQR $511‒$3024). Per-dermatologist payments significantly increased by 14.1% (95% CI 11.2‒16.9%, p < 0.001) each year.
Additionally, among 3556 male dermatologists, 2087 (58.7%) accepted more than one personal payments from the pharmaceutical companies over 4 years (Table 4). Meanwhile, 1034, equal to 31.1% of female dermatologists, received personal payments. Male dermatologists were more likely to accept personal payments from the pharmaceutical companies over the 4 years (p < 0.001 in Chi-square test). Median per-dermatologist payments were $2414 (IQR $817–$7480) in male and $984 (IQR $473–$2554) in female. The male dermatologists were 1.88 (95% CI 1.78–1.99, p < 0.001) times more likely to accept personal payments and received 4.63 (95% CI 3.57–6.02, p < 0.001) times larger personal payments per dermatologist than female.
Of 92 dermatology-oncology specialists and 49 cosmetic dermatology specialists, 89 (96.7%) and 42 (85.7%) received personal payments, while 44.3% (2990 out of 6742) of JDA board-certified dermatologists did. (Table 4) Median per-dermatologists payments were $1643 (IQR: $590–$4985) in board-certified dermatologists, $6464 (IQR: $2059–$17,793) in board-certified dermatology-oncology specialists, and $3365 (IQR: $1505–$12,475) in board-certified cosmetic dermatology specialists. The board-certified dermatology-oncology specialists and board-certified cosmetic dermatology specialists were 1.37 (95% CI 1.28–1.47, p < 0.001) times and 1.74 (95% CI 1.53–1.97, p < 0.001) times more likely to receive payments than the board-certified dermatologists. The per-dermatologist payments were 2.73 (95% CI 1.63–4.60, p < 0.001) times in board-certified dermatology-oncology specialists and 3.91 (95% CI 1.92–7.97, p < 0.001) times in board-certified cosmetic dermatology specialists larger than those in the board-certified dermatologists. Not surprisingly, the dermatologists working in a facility accredited by the JDA for the use of biologics were 1.65 times (95% CI 1.57–1.73, p < 0.001) more likely to receive personal payments and per-dermatologist payment values were 6.99 times (95% CI 5.47–8.93, p < 0.001) higher in dermatologists working in JDA-accredited facilities than those without.
Table 5 showed the lists of ten pharmaceutical companies making the largest personal payments between 2016 and 2019. Of 75 companies making payments, payments for ten companies with top-largest payments accounted for 73.4% of overall payment amounts. Maruho made the highest number of payments and largest total payments to the highest number of dermatologists, with 6888 (15.8% of overall number of payments) payments totaling $6,003,214 (18.1% of overall payment amounts) to 1515 equal to 22.0% of all dermatologists over the 4 years. Of the top ten companies, five including Taiho Pharmaceutical, Novartis, Sanofi, Eli Lilly, and Eisai made increasingly personal payments to the dermatologists between 2016 and 2019. The total payments from Sanofi increased from $40,872 in 2016 to $862,320 in 2019. Similarly, Eli Lilly increased their payment from $150,707 in 2016 to $568,142 in 2019.
Discussion
Contrary to our hypothesis, this study demonstrated that a large number but less than half (45.3%) of board-certified dermatologists received personal payments for reimbursement of lecturing, consulting, and writing from the pharmaceutical companies in Japan. The personal payments to dermatologists totaled $33,223,806 in monetary values and 43,475 in the number of payments between 2016 and 2019. Only the small number of dermatologists accepted substantial amounts of payments. Additionally, these personal payments have significantly increased during this 4-year period. There were gender differences in the patterns of payment receipt. Dermatologists with specialist certifications in dermatology-oncology and cosmetic oncology received larger personal payments from the pharmaceutical companies. To the best of our knowledge to date, this study is the first analysis assessing the financial relationships between pharmaceutical companies and all board-certified dermatologists in Japan. Although we previously reported the physician-industry financial relationships in several specialties, this study added several important insights into this issue in Japan.
Notably, we found that proportion of physicians receiving personal payments in dermatology was the lowest among previously documented specialties4,5,6,7,8,28. The proportions of physicians receiving payments ranged from 64.7% in hematology5 to 70.7% in oncology7 in Japan. Feng et al. reported 73.7% of all dermatologists received one or more payments from the healthcare industry in the United States in 201426. Additionally, per-physician payments to dermatologists were also one of the lowest in Japan, followed by pediatric oncologists4,5,6,7,8,28,32. The reason for this lower payments may be explained by our limitation in data collection. We included only payments for lecturing, consulting, and writing purposes, and could not collect payments for more prevalent categories such as meals, travel and accommodations, and educations, which were widely made to dermatologists in the United States. Compensation for lecturing, consulting and writing was generally targeted at physicians with extensive clinical or research experience, typically physicians working in universities or general hospitals6,16,33. According to a survey by the Japanese Ministry of Health, Labor, and Welfare in 2020, 60.3% of dermatologists worked in clinics and hospitals with less than 20 inpatient beds in Japan34. Considering this nature, we may have underestimated the whole dermatologist-industry financial relationships in Japan.
However, we illustrated that these personal payments were increasingly made to board-certified dermatologists from the pharmaceutical companies in Japan since 2016. Behind the increasing trends in personal payments, there were increasing introduction of novel biologic drugs for atopic dermatitis and psoriasis in Japan. Our findings that the dermatologists working in the JDA-accredited facilities for use of biologics received significantly larger payments support this assumption. Remarkable progress in novel drugs for atopic dermatitis and psoriasis have been recorded worldwide. Many novel biologic drugs based on different pathways such as risankizumab (Skyrizi® marketed by AbbVie was approved in March 2019)35, secukinumab (Cosentyx® manufactured by Novartis Pharma and marketed by Maruho was approved in December 2014)36, brodalumab (Lumicef marketed by Kyowa Kirin was approved in July 2016)37, and adalimumab (Humira manufactured by AbbVie and marketed by Eisai was approved in June 2016)38 were introduced into psoriasis treatment. Also, dupilumab (Dupixent® marketed by Sanofi) was introduced for atopic dermatitis treatment in January 2018. In Japan, most of these novel biologics for psoriasis and atopic dermatitis are available only to dermatologists working at JDA-certified facilities. It is reasonable for the pharmaceutical companies to market their products to them and ask them to give lectures other dermatologists. Due to the introduction of novel biologic drugs for atopic dermatitis, increasing trends in personal payments from healthcare industry was also observed among allergists and clinical immunologists in the United States39. Considering that five biologic drugs including baricitinib, delgocitinib, upadacitinib, nemolizumab, and abrocitinib additionally gained approval for atopic dermatitis after 2020, the personal payments from the pharmaceutical companies to the dermatologists will continue to increase in Japan.
Additionally, our study has added novel insights in the context of previous studies. Only a small number of dermatologists including dermatologists with specialist certifications received substantial amounts of personal payments from the pharmaceutical companies. We previously reported that the JDA clinical practice guidelines authors received from $4127 to $7043 in median annual payments. The JDA executive board members received $24,213 in median per-member payments from the pharmaceutical companies in 2016. Considering median annual personal payments were $882‒$1,046 among the board-certified dermatologists, this study provided evidence that the personal payments to influential dermatologists such as clinical practice guideline authors and society board members were considerably higher than those to general dermatologists. Unlike the physicians conducting clinical trials or developing novel therapies, considering leading physicians who are in highly ethical and authoritative positions such as professional medical society board members and clinical practice guideline authors have considerable impact on other physicians’ clinical practice and patient care, these physicians must be independent and minimize their financial relationships with the pharmaceutical companies40,41,42. Otherwise, these leading physicians at least must be transparent about their financial relationships with the pharmaceutical companies, though most of the financial relationships between the leading dermatologists and the pharmaceutical companies were undisclosed and underdeclared by the dermatologists in Japan16.
There were large gaps in personal payments between male and female dermatologists in Japan, which was consistent with our previous study assessing the financial conflicts of interest among the JDA clinical practice guidelines authors16. The gender differences in industry payments are well-described in the United States as well, as fewer female physicians received lower personal payments from the pharmaceutical and medical devices manufacturers than male physicians in the United States43,44,45,46,47,48,49. Many factors would have contributed to the lower personal payments from the pharmaceutical companies to female physicians in Japan. First, Female physicians tended to have lower motivation for negotiating their payments and accepted lower earnings for non-monetary benefits such as flexibility of work time and location. Therefore, female dermatologists might not have negotiated the lower personal payments and might have declined the lecturing events sponsored by the pharmaceutical companies in Japan. Other possible reason is the lower representation of female physicians in Japanese medical society. Harada et al. reported that only 5.7% (20 out of 351) of all Japanese editors-in-chiefs of medical academic journals were female50. Of 296 dermatology clinical practice guideline authors, only 49 equal to 16.6% were female in Japan16. Thus, the lower personal payments to the dermatologists might be due to the lower presentations in academic and research positions in Japan. Future study should examine the lower personal payments to the female dermatologists from the pharmaceutical companies adjusting other covariables.
This study included several limitations. First, as the transparency guidance was a voluntary self-disclosure of the payments by the pharmaceutical companies, although unethical, the pharmaceutical companies may not have accurately disclosed and hidden the payment data. Additionally, though physicians can correct the payment data by personal contacts with the companies, there was no official dispute and correction process in the current self-disclosure in Japan. Thus, there were possibilities in inaccuracies of payment data disclosed by the companies. Second, despite we repeatedly cross-checking the collected data for any errors by two or more persons, the inclusion of errors in the collected data by our study team could not be ruled out. Third, as the payment data concerning various categories including meals, educational activities, transportation and accommodations were not disclosed with individual name of recipients by the pharmaceutical companies in Japan3, this study would have underreported the prevalence and magnitude of financial relationships between the dermatologists and pharmaceutical companies in Japan. Fourth, there were possible confounding factors influencing the personal payments to the dermatologists other than dermatologists’ gender and specialist certification which were not included in the database of the JDA board-certified dermatologists.
In conclusion, this study found that 45.3% of Japanese board-certified dermatologists received lower personal payments for the reimbursement of lecturing, consulting, and writing than those to other specialists between 2016 and 2019. Only a small portion of dermatologists, such as those with specialist certification and male sex, received vast majority of payments from the pharmaceutical companies. Furthermore, these personal payments were increasingly more prevalent and greater over the 4 years during the study period.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Marshall, D. C., Jackson, M. E. & Hattangadi-Gluth, J. A. Disclosure of industry payments to physicians: An epidemiologic analysis of early data from the open payments program. Mayo Clin. Proc. 91(1), 84–96 (2016).
Tringale, K. R. et al. Types and distribution of payments from industry to physicians in 2015. JAMA 317(17), 1774–1784 (2017).
Ozaki, A. et al. Overview and transparency of non-research payments to healthcare organizations and healthcare professionals from pharmaceutical companies in Japan: Analysis of payment data in 2016. Health Policy 124(7), 727–735 (2020).
Murayama, A. et al. Pharmaceutical payments to japanese board-certified infectious disease specialists: A four-year retrospective analysis of payments from 92 pharmaceutical companies between 2016 and 2019. Int. J. Environ. Res. Public Health 19(12), 7417 (2022).
Kusumi, E. et al. Pharmaceutical payments to Japanese certified hematologists: A retrospective analysis of personal payments from pharmaceutical companies between 2016 and 2019. Blood Cancer J. 12(4), 54 (2022).
Kamamoto, S. et al. Evaluation of financial relationships between Japanese certified pediatric hematologist/oncologists and pharmaceutical companies: A cross-sectional analysis of personal payments from pharmaceutical companies between 2016 and 2019. Pediatr. Blood Cancer. 69(10), e29891 (2022).
Ozaki, A. et al. Pharmaceutical payments to certified oncology specialists in Japan in 2016: A retrospective observational cross-sectional analysis. BMJ Open 9(9), e028805 (2019).
Murayama, A. et al. Nature and trends in personal payments made to the respiratory physicians by pharmaceutical companies in Japan between 2016 and 2019. Respiration 101(12), 1088–1098 (2022).
Hashimoto, T. et al. Evaluation of financial conflicts of interest and drug statements in the coronavirus disease 2019 clinical practice guideline in Japan. Clin. Microbiol. Infect. 28(3), 460–462 (2022).
Yamamoto, K. et al. Financial conflicts of interest between pharmaceutical companies and the authors of urology clinical practice guidelines in Japan. Int. Urogynecol. J. 32(2), 443–451 (2021).
Murayama, A. et al. Evaluation of conflicts of interest among participants of the Japanese nephrology clinical practice guideline. Clin. J. Am. Soc. Nephrol. 17(6), 819–826 (2022).
Saito, H., Ozaki, A., Sawano, T., Shimada, Y. & Tanimoto, T. Evaluation of pharmaceutical company payments and conflict of interest disclosures among oncology clinical practice guideline authors in Japan. JAMA Netw. Open. 2(4), e192834 (2019).
Saito, H., Ozaki, A., Kobayashi, Y., Sawano, T. & Tanimoto, T. Pharmaceutical company payments to executive board members of professional medical associations in Japan. JAMA Intern. Med. 179(4), 578–580 (2019).
Saito, H. et al. Pharmaceutical company payments to the professors of orthopaedic surgery departments in Japan. J. Bone Jt. Surg. Am. 102(9), e39 (2020).
Murayama, A. et al. Coronavirus disease 2019 experts appearing on Japanese television: Their characteristics and financial conflicts of interest with pharmaceutical companies. Clin. Microbiol. Infect. 27, 805–807 (2020).
Murayama, A. et al. Pharmaceutical company payments to dermatology Clinical Practice Guideline authors in Japan. PLoS ONE 15(10), e0239610 (2020).
Murayama, A. et al. Awareness and perceptions among members of a Japanese Cancer Patient Advocacy Group concerning the financial relationships between the pharmaceutical industry and physicians. Int. J. Environ. Res. Public Health. 19(6), 3478 (2022).
Duarte-García, A. et al. Association between payments by pharmaceutical manufacturers and prescribing behavior in rheumatology. Mayo Clin. Proc. 97(2), 250–260 (2022).
Mitchell, A. P. et al. Are financial payments from the pharmaceutical industry associated with physician prescribing? A systematic review. Ann. Intern. Med. 174(3), 353–361 (2021).
Inoue, K., Tsugawa, Y., Mangione, C. M. & Duru, O. K. Association between industry payments and prescriptions of long-acting insulin: An observational study with propensity score matching. PLoS Med. 18(6), e1003645 (2021).
Inoue, K. et al. Association between industry marketing payments and prescriptions for PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitors in the United States. Circ. Cardiovasc. Qual. Outcomes. 14(5), e007521 (2021).
Hollander, M. A., Donohue, J. M., Stein, B. D., Krans, E. E. & Jarlenski, M. P. Association between opioid prescribing in Medicare and pharmaceutical company gifts by physician specialty. J. Gen. Intern. Med. 35(8), 2451–2458 (2020).
Mitchell, A. P., Winn, A. N., Lund, J. L. & Dusetzina, S. B. Evaluating the strength of the association between industry payments and prescribing practices in oncology. Oncologist. 24(5), 632–639 (2019).
Khan, R., Nugent, C. M., Scaffidi, M. A., Gimpaya, N. & Grover, S. C. Association of biologic prescribing for inflammatory bowel disease with industry payments to physicians. JAMA Intern. Med. 179(10), 1424–1425 (2019).
Goupil, B. et al. Association between gifts from pharmaceutical companies to French general practitioners and their drug prescribing patterns in 2016: Retrospective study using the French Transparency in Healthcare and National Health Data System databases. BMJ 5(367), l6015 (2019).
Feng, H., Wu, P. & Leger, M. Exploring the industry-dermatologist financial relationship: Insight from the open payment data. JAMA Dermatol. 152(12), 1307–1313 (2016).
Murayama, A. et al. Financial and intellectual conflicts of interest among Japanese Clinical Practice Guidelines authors for allergic rhinitis. Otolaryngol. Head Neck Surg. 166(5), 869–876 (2022).
Murayama, A. et al. Financial relationships between pharmaceutical companies and rheumatologists in Japan between 2016 and 2019. JCR J. Clin. Rheumatol. https://doi.org/10.1097/RHU.0000000000001922 (2023).
Tarras, E. S., Marshall, D. C., Rosenzweig, K., Korenstein, D. & Chimonas, S. Trends in industry payments to medical oncologists in the United States since the inception of the open payments program, 2014 to 2019. JAMA Oncol. 7(3), 440–444 (2021).
Marshall, D. C. et al. Trends in financial relationships between industry and radiation oncologists versus other physicians in the United States from 2014 to 2018. Int. J. Radiat. Oncol. Biol. Phys. 109(1), 15–25 (2021).
Marshall, D. C., Tarras, E. S., Rosenzweig, K., Korenstein, D. & Chimonas, S. Trends in industry payments to physicians in the United States From 2014 to 2018. JAMA 324(17), 1785–1788 (2020).
Murayama, A. et al. Pharmaceutical payments to Japanese board-certified head and neck surgeons between 2016 and 2019. OTO Open. 7(1), e31 (2023).
Wright, K. et al. Industry relationships with medical oncologists: Who are the high-payment physicians?. JCO Oncol. Pract. 18(7), e1164–e1169 (2022).
Ministry of Health Labour and Welfare's Committee for the Promotion of Health Technology Assessment Report of the Commitee for the Promotion of Health Technology Assessment. 1999 [cited 2021 June 1]. https://www.mhlw.go.jp/www1/houdou/1103/h0323-1_10.html.
Papp, K. A. et al. Risankizumab versus ustekinumab for moderate-to-severe plaque psoriasis. N. Engl. J. Med. 376(16), 1551–1560 (2017).
Langley, R. G. et al. Secukinumab in plaque psoriasis–results of two phase 3 trials. N. Engl. J. Med. 371(4), 326–338 (2014).
Mease, P. J., Helliwell, P. S., Hjuler, K. F., Raymond, K. & McInnes, I. Brodalumab in psoriatic arthritis: Results from the randomised phase III AMVISION-1 and AMVISION-2 trials. Ann. Rheum. Dis. 80(2), 185–193 (2021).
Revicki, D. et al. Impact of adalimumab treatment on health-related quality of life and other patient-reported outcomes: results from a 16-week randomized controlled trial in patients with moderate to severe plaque psoriasis. Br. J. Dermatol. 158(3), 549–557 (2008).
Murayama, A., Kamamoto, S., Saito, H., Tanimoto, T. & Ozaki, A. Industry payments to allergists and clinical immunologists in the United States during the coronavirus disease 2019 pandemic. Ann. Allergy Asthma Immunol. 129, 635–636 (2022).
Moynihan, R. Key opinion leaders: Independent experts or drug representatives in disguise?. BMJ 336(7658), 1402–1403 (2008).
Moynihan, R. et al. Pathways to independence: Towards producing and using trustworthy evidence. BMJ 3(367), l6576 (2019).
Rothman, D. J. et al. Professional medical associations and their relationships with industry: A proposal for controlling conflict of interest. JAMA 301(13), 1367–1372 (2009).
Pace, N. M. et al. Gender gap in industry relationships and scholarly impact among academic urologists in the United States. Urology 139, 90–96 (2020).
Raber, I. et al. Gender differences in industry payments among cardiologists. Am. Heart J. 223, 123–131 (2020).
Velez, D., Mehta, A., Rotker, K. & Thavaseelan, S. Gender disparities in industry payments to urologists. Urology 150, 59–64 (2021).
Eloy, J. A. et al. Association of gender with financial relationships between industry and academic otolaryngologists. JAMA Otolaryngol. Head Neck Surg. 143(8), 796–802 (2017).
Weng, J. K. et al. Evaluation of sex distribution of industry payments among radiation oncologists. JAMA Netw. Open. 2(1), e187377 (2019).
Tringale, K. R. & Hattangadi-Gluth, J. A. Types and distributions of biomedical industry payments to men and women physicians by specialty, 2015. JAMA Intern. Med. 178(3), 421–423 (2018).
Inoue, K., Blumenthal, D. M., Elashoff, D. & Tsugawa, Y. Association between physician characteristics and payments from industry in 2015–2017: Observational study. BMJ Open 9(9), e031010 (2019).
Harada, K. et al. Woman editors-in-chief of english-language medical journals published by the Japanese Professional Medical Associations. JMA J. 5(1), 114–117 (2022).
Acknowledgements
The authors thank the Tansa (formerly known as Waseda Chronicle) for providing payment data. Also, we appreciate Dr Tetsuya Tanimoto, Ms Hinari Kugo, Mr. Takuto Sakaemura, Mr. Kohki Yamada, Mr Haruki Shigeta, and Ms. Megumi Aizawa for their dedicated contribution on collecting and cross-checking the payment data. This study was funded in part by the Medical Governance Research Institute. This non-profit enterprise receives donations from pharmaceutical companies, including Ain Pharmacies, Inc., other organizations, and private individuals. This study also received support from the Tansa (formerly known as the Waseda Chronicle), an independent non-profit news organization dedicated to investigative journalism. None of the entities providing financial support for this study contributed to the design, execution, data analyses, or interpretation of study findings and the drafting of this manuscript. For the financial conflicts of interest, H.S. received personal fees from TAIHO Pharmaceutical Co. Ltd outside the scope of the submitted work. A.O. received personal fees from Medical Network Systems outside the scope of the submitted work. Regarding non-financial conflicts of interest among the study authors, all are engaged in ongoing research examining financial and non-financial conflicts of interest among healthcare professionals and pharmaceutical companies in Japan and the United States. Among their previous articles, the authors have self-cited several articles in this study to gain deeper insights and explain the context of financial conflicts of interest among healthcare professionals. The other authors have no example conflicts of interest to disclose.
Funding
This study was funded in part by the Medical Governance Research Institute. This non-profit enterprise receives donations from pharmaceutical companies, including Ain Pharmacies, Inc., other organizations, and private individuals. This study also received support from the Tansa (formerly known as the Waseda Chronicle), an independent non-profit news organization dedicated to investigative journalism. None of the entities providing financial support for this study contributed to the design, execution, data analyses, or interpretation of study findings and the drafting of this manuscript.
Author information
Authors and Affiliations
Contributions
A.M.: Study concept and design, data collection, investigation, resource, statistical analysis, visualization, supervision, drafting of the manuscript, reviewing of the manuscript, study administration. S.K.: Data collection, visualization, drafting of the manuscript, and critically reviewing of the manuscript. H.S.: Study concept and design, data collection, supervision, drafting of the manuscript, reviewing of the manuscript. A.O.: Study concept and design, drafting of the manuscript, reviewing of the manuscript, supervision.
Corresponding author
Ethics declarations
Competing interests
H.S. received personal fees from Taiho Pharmaceutical Co. Ltd outside the scope of the submitted work. A.O. received personal fees from Medical Network Systems outside the scope of the submitted work. Other remaining authors declared no financial conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Murayama, A., Kamamoto, S., Saito, H. et al. Pharmaceutical payments to Japanese board-certified dermatologists: a 4-year retrospective analysis of personal payments from pharmaceutical companies between 2016 and 2019. Sci Rep 13, 7425 (2023). https://doi.org/10.1038/s41598-023-34705-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34705-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.