Abstract
To conduct a systematic review of the comparative efficacy of various psychotropic medications for the treatment of disruptive behavior (DBs) in youths. To this aim, we systematically reviewed randomized clinical trials (RCTs) of various psychotropic medications targeting symptoms of DBs and applied network meta-analysis to investigate their relative efficacy. Fifty-five RCTs meeting the inclusion criteria were selected. To predict and interpret relative treatment efficacy, we compared the efficacy of various psychotropic medications prescribed for DB symptoms based on their mechanism of action. Network meta-analysis revealed that for reducing DBs, second-generation antipsychotics, stimulants, and non-stimulant ADHD medications were more efficacious than placebo, and second-generation antipsychotics were the most efficacious. The dopaminergic modulation of top-down inhibitory process by these medications is discussed in this review. This study offers information on the relative efficacy of various psychotropic medications for the treatment of DB, and insight into a potential neurobiological underpinning for those symptoms. It also illustrates the potential utility of these neurobiological mechanisms as a target for future treatment studies.
Similar content being viewed by others
Introduction
Disruptive behavior problems (DBs) in children and adolescents are one of the most common reasons for referral to mental health care facilities1. They are a primary component of serious child and adolescent psychopathologies2, and are characterized by behavioral manifestations that typically share difficulties in modulation of aggression, self-control, and impulsivity, and also result in threats to the safety of others and disrupt social norms3,4. Oppositional, aggressive, and hyperactive behaviors present in early childhood often predict negative mental health outcomes later in life, ranging from school failure to substance abuse and criminality5,6.
For complex disorders with limited existing treatment options and interventions with relatively lower efficacy/effectiveness, clinicians and researchers have attempted to identify subgroups of individuals based on clusters of specific symptoms or other clinical and/or socio-environmental factors7. The utility of identifying subgroups is unfortunately limited by the methods used, such as using a categorical diagnostic approach8. Because individuals with the same categorical diagnosis display a wide range of symptoms, groups characterized in this manner are very heterogeneous9. Furthermore, youth with multiple comorbid disorders are more common in child and adolescent psychiatry10.
Recent clinical research has shifted interest to shared transdiagnostic psychopathologies, in accordance with the dimensional model for common psychiatric disorders11. Prior studies have demonstrated that DBs are associated with almost all forms of psychopathology in children and adolescents and are broadly present alongside both internalizing and externalizing symptoms12,13,14. Therefore, DBs may be excellent candidates as trans-diagnostic markers for studying the effectiveness of interventions, as well as guide ongoing and future child and adolescent psychiatric research and clinical practice15.
Use of a transdiagnostic method is further supported by the fact that there may be a common underlying pathophysiological mechanism of DBs in youths across various psychiatric diagnoses. Impairments in emotion regulation and inhibitory control16,17,18,19 may be key predictors of DBs20,21. According to the dysregulation hypothesis, DBs can be induced by the failure of top-down modulation of neural areas implicated in emotional responding16. This model possibly implicates the mesolimbic dopamine system, including projections from the ventral tegmental area to the nucleus accumbens and ventral striatum, and eventually to the prefrontal cortex22,23,24. Additionally, previous research has suggested that DBs in various psychiatric diagnoses result from dysfunction in the serotonergic and dopaminergic systems in the prefrontal cortex25,26,27.
Regarding psychopharmacological interventions, a number of agents have been studied for treatment of DBs in children and adolescents. Prior clinical trials investigated the efficacy of stimulants28,29,30,31, atomoxetine28,32,33,34, atypical antipsychotics30,35,36,37,38,39,40, mood stabilizers39,41, and anticonvulsants42,43 for treatment of DBs in youths with various psychiatric diagnoses (i.e., Attention Deficit Hyperactivity Disorder (ADHD), Conduct Disorder (CD), Oppositional Defiant Disorder (ODD), Disruptive Mood Dysregulation Disorder (DMDD), Major Depressive Disorders (MDD), Anxiety Disorders, Autism Spectrum Disorder (ASD), and tic disorder). Most of the previous studies, however, focused on the primary symptoms of each categorical diagnoses, for example, inattention in ADHD, or global improvement, and reported on DBs as co-occurring symptoms. Additionally, several systematic reviews reported an overview of the efficacy and safety of common medications for DBs44,45,46.
The previous studies leave a general gap in knowledge on the relative efficacy of each agent in the treatment of DBs, especially in regard to the different mechanisms of action of medications and their potential impact on the neurobiology of DBs. These studies did not use an objective appraisal of the evidence with a thorough methodological approach47, and many of them compared only two interventions (i.e., placebo vs pharmacological intervention), in which a conventional pair-wise meta-analysis may be conducted48.
We have instead applied network meta-analysis (NMA)49. Unlike traditional meta-analyses, which only allow for direct comparisons of interventions using the pooled data from clinical trials with similar treatment arms, NMA enables the estimation of relative effects of interventions without direct comparison50. Specifically, NMA is a method for comparison among multiple treatments simultaneously in a single analysis by integrating direct and indirect data from randomized controlled trials in a network. NMA has become a focus of clinical research since it may help examine the comparative efficacy of several treatments often utilized in clinical practice simultaneously49.
To this end, we systematically reviewed randomized trials (55 in total) of various psychopharmacological agents targeting the symptoms that represent DBs (i.e., aggression, hostility, impulsivity, conduct problems, and oppositional defiant problems) and applied NMA to determine their relative efficacy. We included the previous studies of psychotropic agents across medication classes (stimulants, anticonvulsants, second-generation antipsychotics, selective serotonin reuptake inhibitors (SSRIs), aripiprazole, tricyclic antidepressants, non-stimulant ADHD medication, lithium, and dasotraline), which contain valid measures for DBs even though the treatment of DBs may not have been a primary outcome.
Methods
Study protocol registration
This study was written in compliance with the recommendation of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement51. The study protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) in February 2022 (CRD42021256959). Supplementary Table 1 reported our results based on the updated PRISMA checklist for NMA.
Search strategy and study selection
We applied a comprehensive search strategy in literature databases. Six electronic databases (PubMed, Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE, Web of Science, PsycINFO, and ProQuest Dissertations) were used for literature search and review for articles published up to February 2022 with the following search terms: (disruptive behavior OR conduct problem OR oppositional problem OR defiant problem OR aggression OR hostility OR impulsivity) AND (children OR adolescent OR youth) AND (randomized OR random OR randomly OR randomization OR randomization OR RCT OR RCTS) AND (pharmacological treatment OR pharmacological therapy OR pharmacological intervention OR drug OR medication OR medication treatment OR norepinephrine-dopamine reuptake inhibitors (methylphenidate stimulants, amphetamine stimulants, OR bupropion) OR dopamine receptor antagonists (aripiprazole, haloperidol, ziprasidone, OR ecopipam) OR GABA receptor agonists (divalproex sodium, valproate sodium, divalproex, diazepam, zolpidem, OR carbamazepine) OR selective norepinephrine reuptake inhibitors (atomoxetine) OR serotonin-norepinephrine inhibitors (duloxetine, desvenlafaxine, nortriptyline, clomipramine, imipramine, OR venlafaxine) OR serotonin-dopamine antagonists (risperidone, lurasidone, clozapine, OR quetiapine) OR selective serotonin reuptake inhibitors (sertraline, paroxetine, escitalopram, fluvoxamine, trazodone, OR fluoxetine) OR Serotonin-norepinephrine-dopamine reuptake inhibitor (dasotraline) OR lithium. After the initial search and review, a manual search was performed by reviewing the reference lists of all identified publications and reviewing similar articles suggested by the meta-analysis and systematic review articles relevant to this topic52. To supplement incomplete reports in the original papers, relevant authors were contacted.
Selection criteria and full-text screening
The review process identified randomized clinical trials (RCTs) assessing the efficacy of psychotropic medications on disruptive behavior. All RCTs of pharmacological treatment reporting measures of symptoms that may represent underlying disruptive behavior were considered for inclusion. Based on our literature review3,53, the following symptoms were selected because they may represent underlying DB: (1) aggression/hostility, (2) oppositional/defiant problem, (3) conduct problem and (4) impulsivity. For the measurements that were used for each symptom, see Table 2.
The following exclusion criteria were applied: (1) abstract-only articles, case reports and case series (2) overlapping data set (3) animal studies (4) studies which did not report the mean or standard deviation in the post-treatment measurements (5) studies investigating comparison of efficacy between psychotropic medications with similar enough mechanism of drug action (i.e., risperidone vs. quetiapine vs. clozapine or dextroamphetamine vs. methylphenidate vs. bupropion) (6) studies of combination of more than one psychotropic medication, as it is difficult to distinguish the efficacy of psychotropic medication from that of combined effect (7) studies using unreliable measurement and studies with unclear data which included non-peer-reviewed publication. There were no limitations on the language, year of publication, country, gender, or ethnicity of the patients. Through the predefined eligibility criteria, two independent reviewers first screened and chose the title and abstract, then conducted full-text screening of included articles. Any disagreement between the reviewers was decided by an independent experienced literature reviewer.
Data extraction
A standardized template file was created based on a pilot extraction with the two most relevant references. Two researchers separately extracted the data using this template file. Extracted data included: title, authors, publication year, and participants’ characteristics including age, gender, sample size and diagnosis. The data for the dosages of each psychotropic medication, methods of administration, trial duration, measurements for symptoms representing underlying DB, and pre- and post-treatment scores for symptoms were also extracted. The data extracted was reviewed by the two independent researchers and disagreements were resolved through discussion to reach a consensus.
Risk of bias assessment
Two reviewers independently evaluated the validity of each RCT through “The Cochrane Risk of Bias Tool for randomized controlled trials”54. The tool evaluates RCT using a set of domains of bias including random sequence generation, allocation concealment, selective reporting, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and other sources of bias. Each study domain was assigned a rating of low, high, or unclear risk. Any discrepancies were resolved by a discussion among reviewers or guidance from an independent experienced literature reviewer.
Summary measure
Statistical analysis
As pre-specified in the study protocol, we analyzed psychotropic medications according to their primary mechanisms of action. This led to categorization of the listed psychotropic medications as follows: (1) Norepinephrine and dopamine reuptake inhibitors (stimulants), (2) GABA receptor agonists (anticonvulsants), (3) serotonin-dopamine antagonists (second-generation antipsychotics), (4) selective serotonin reuptake inhibitors (SSRIs), (5) dopamine receptor modulator (aripiprazole), (6) Serotonin-Norepinephrine Reuptake inhibitors (Tricyclic antidepressants, TCA), (7) selective norepinephrine reuptake inhibitors (non-stimulant ADHD medication such as guanfacine and clonidine), (8) serotonin-norepinephrine-dopamine reuptake inhibitor (dasotraline) and (9) lithium. The list of medications in each category is provided in Table 1. After the categorization, NMA was performed to compare the efficacy of different psychotropic medications with a frequent random-effects model, which preserves randomized treatment comparisons within trials using the net-meta R package version 8.0 (available at: http://CRAN.R-project.org/package=netmeta)55. International Society for Pharmacoeconomics and Outcome Research (ISPOR) recommend the NMA for comparing efficacy between different treatment modalities56. NMA enables simultaneous comparisons between all treatment arms across the studies in a single analysis by combining both direct and indirect comparisons57.
Heterogeneity is estimated by the I2 and Q statistics, which measure the percentage of total variation in point estimates among studies that is attributable to heterogeneity55,58. The I2 statistic describes the percentage of variation that is not attributable to chance. A value of I2 from 0 to 50% was considered unlikely to be important, 50–75% as moderate heterogeneity, and 75–90% as considerable heterogeneity59. Also, the Q statistics, which are a statistic for inconsistency, are calculated using the weighted sum of squared differences across studies, which represents the variation of treatment effect between direct and indirect comparisons at the meta-analytic level60. Significant heterogeneity was examined to be present when the p for heterogeneity was < 0.05 in the result of Q statistics.
To assess inconsistency in the network, a net-heat plot was used61. The net-heat plot is helpful to examine direct comparisons that might be likely sources of important inconsistency in the network. In that graph, the larger the gray box, the more important that treatment comparison is relative to another treatment comparison and the colored backgrounds indicate the degree of inconsistency in the network61. Additionally, the node-splitting method was used for assessment of inconsistency in the forest plots of NMA62. Publication bias was assessed by adjusted funnel plots. If data were sufficient, an Egger’s test of the intercept with centralized effect size and SE was further conducted63.
Since we assumed that the included studies differed with respect to clinical and other factors, we applied random-effects models instead of fixed-effect models. To rank the treatments based on their efficacy for each outcome, P-scores, a statistical parameter in frequentist NMA and ranging from 0 to 1, were calculated using the surface under the cumulative ranking curve (SUCRA)64. A higher P-score expresses the probability that the treatment would be better than the competing treatments65.
To interpret frequentist NMA, we checked the confidence interval to find any significant difference between the treatment arm and placebo. Then, we ordered the treatment using P-score.
Results
Search results
Our initial search yielded 1678 papers relative to our research terms. Title/abstract screening excluded 1552 irrelevant papers while a further 78 papers were excluded following full-text screening due to unavailability of data extraction, presence of adjunctive treatment, etc. Seven additional papers were included from the manual search. In total, 55 RCTs (comprising 5684 patients) were included for the NMA (Fig. 1). In addition, there were four studies comparing individual agent arms against each other (stimulant vs. non-stimulant ADHD medication, second-generation antipsychotic vs. dopamine receptor modulator, and second-generation antipsychotic vs. anticonvulsant) (Table 2, Fig. 2A). For the list of the articles included, see Table 2.
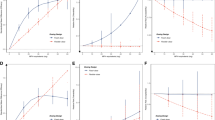
The result of NMA for disruptive symptoms. (A) The network graph representing treatment arms included in the network for disruptive symptoms, the thickness of the lines shows the number of studies. (B) Random effect model forest plot for comparison of each treatment arm vs. placebo. (C) Ranking of medications for disruptive symptoms using SUCRA values. (D) Comparison of the included agent groups: standardized mean differences (95% CI). Each cell represents the effect of the column-defining agent group compared to the row-defining agent group. DRA Dopamine receptor antagonist/aripiprazole, NDRI Norepinephrine–dopamine reuptake inhibitor/stimulant, SDA Serotonin dopamine antagonist/second-generation antipsychotics, sNRI Selective norepinephrine reuptake inhibitors/non-stimulant ADHD medication, SNDRI Serotonin-norepinephrine-dopamine reuptake inhibitor, SNRI Serotonin-norepinephrine reuptake inhibitors/tricyclic antidepressants, SSRI selective serotonin reuptake inhibitor.
Study characteristics
The characteristics of included studies are summarized in Table 1. Studies were performed and published between 1990 and 2021. Across studies, a total of 15 distinct psychotropic medications were represented. (1) one stimulant (Norepinephrine–dopamine reuptake inhibitor, NDRI): methylphenidate; (2) one non-stimulant ADHD medication (Selective norepinephrine reuptake inhibitors, SNRI): atomoxetine; (3) three second-generation antipsychotics (Serotonin dopamine antagonist, SDA): risperidone olanzapine and quetiapine (4) one dopamine receptor modulator (Dopamine receptor antagonist, DRA): aripiprazole (5) two SSRIs selective serotonin reuptake inhibitor): sertraline and fluoxetine; (6) three anticonvulsants (GABA receptor agonists, GRA): valproate sodium, divalproex, and carbamazepine (7) two TCAs (Serotonin-Norepinephrine Reuptake inhibitors, SNRI): desipramine and imipramine (8) one Serotonin-norepinephrine-dopamine reuptake inhibitor (Serotonin-norepinephrine-dopamine reuptake inhibitor, SNDRI): dasotraline (9) lithium.
A total of 9 diagnoses were included in the RCTs on disruptive behavior ADHD (n = 3988, 70.16%), disruptive behavior disorders (DBD) (n = 714, 12.56%), pervasive developmental disorder (n = 274, 4.82%), bipolar disorder (BD) (n = 217, 3.82%), ASD (n = 215, 3.78%), CD (n = 147, 2.59%), obsessive–compulsive disorder (n = 92, 1.62%), MDD (n = 31, 0.54%), and ODD (n = 6, 0.11%).
In total, 3490 and 2194 children and adolescents with psychiatric disorders were randomly assigned to active psychotropic medications and placebo, respectively. The age range of subjects in the RCT’s was 2–20 years (RCT’s mean = 7.03). Sixteen studies did not provide specific information on age. Subjects in both sets of RCT’s were predominantly male (83.75%) with 23 studies not reporting sex.
The mean duration of trials was 57.44 days (SD = 46.29) for medication treatment. There was one study that did not provide the duration.
Network meta-analysis results for disruptive behavior
The relative efficacy of each agent group compared with placebo was conducted for disruptive behavior symptoms (Fig. 2b). The network consisted of 55 studies comparing nine agent groups versus placebo, which were stimulant (NDRI), non-stimulant ADHD medication (sNRI), second-generation antipsychotic (SDA), lithium, dopamine receptor modulator (DRA), SSRI, anticonvulsant (GRA), TCA (SNRI) and SNDRI.
Four agent groups were significantly more efficacious than placebo when data was combined in the NMA: second-generation antipsychotic with a Standardized Mean Differences (SMD) of 0.668 (95% CI 0.537–0.800), stimulant with 0.633 (95% CI 0.513–0.752), dopamine receptor modulator with 0.402 (95% CI 0.046–0.757) and non-stimulant ADHD medication with 0.386 (95% CI 0.280–0.492) (Fig. 2b). The effect sizes from traditional meta-analysis are presented in the supplementary data (Fig. S6).
Second-generation antipsychotics (SDA) had the highest probability for being the most efficacious agents for disruptive behavior symptoms (P score = 0.9356) followed by stimulants (P score = 0.8906), then dopamine receptor modulators (P score = 0.5932), while placebo ranked as the least efficacious in reducing the symptoms of disruptive behavior (P score = 0.0811) (Fig. 2c).
The Fig. 2d shows detailed results of pairwise meta-analyses. Even though the second-generation antipsychotics and stimulants showed the highest efficacies for disruptive behavior symptoms when compared to placebo, the direct and indirect pairwise comparisons among medications revealed they weren’t significantly more efficacious than various agent groups including TCA, lithium, SSRI and dopamine receptor modulator. There were significant differences between second-generation antipsychotic and anticonvulsant with an SMD of 0.574 (95% CI 0.216–0.933), between the second-generation antipsychotic and SNDRI with 0.460 (0.114–0.806), and between the second-generation antipsychotic and non-stimulant ADHD medication with 0.282 (0.114–0.451). Stimulant also showed significant differences in its efficacy when compared with anticonvulsant (SMD 0.539 95% CI 0.164–0.914), SNDRI (SMD 0.425, 95% CI 0.083–0.766) and non-stimulant ADHD medication (SMD 0.247, 95% CI 0.095–0.399).
Quality assessment
We applied rigorous methods of quality assessment to provide evidence of the integrity of the NMA results. Supplementary Figs. S1 and S2 presented the methodological features examined for each trial and a summary result of the judged risk of bias across studies based on the Cochrane risk of bias tool. 22(40%) trials were assessed as a high risk of bias, 34 (61.81%) trials as unclear risk, and 12 (21.81%) as low risk of bias in disruptive symptoms.
Figure 2a show the network of eligible comparisons for efficacy in disruptive symptoms. All agent groups had at least one placebo-controlled trial. In network quality analysis for disruptive symptoms, we did not find evidence for heterogeneity (Q = 54.74, p = 0.1768, tau2 = 0.0086, I2 = 16). Also, there was no evidence of significant inconsistency between the direct and indirect estimates (i.e., all p-values were above 0.05) of disruptive symptoms (Tables S1, S2). The node-splitting method was also used to evaluate consistency between direct and indirect estimates (Fig. S3). For illustrating the consistency pattern that existed in each comparison, net heat plots were also formed to detect hot spots (red squares) indicating greater inconsistency among comparisons (Fig. S4). There was no significant inconsistency between direct and indirect evidence for most comparisons, as demonstrated by both the node splitting approach (P-value > 0.05) and net heat plots. Therefore, we concluded that the consistency model is valid in our NMA.
Potential publication bias in NMA was assessed through the funnel plots produced (Fig. S5). The result of the funnel plots showed no significant asymmetry pattern, and most studies were normally distributed in the funnel plot. Therefore, we determined that there was no significant publication bias in our research.
Discussion
To our knowledge, this is the first NMA of Randomized Clinical Trials (RCTs) to date exploring the individual efficacy of pharmacological treatments on disruptive behavior problems (DBs) in youths with various psychiatric disorders. The efficacy of 9 psychotropic medications on treatment of symptoms representing underlying DBs varied widely. NMA revealed that, for reducing disruptive symptoms, second-generation antipsychotics, stimulant, and non-stimulant ADHD medications were significantly more efficacious than placebo, and second-generation antipsychotics were the most efficacious. For disruptive symptoms, there is a consistent finding that psychotropic medications with higher dopaminergic receptor affinity, including methylphenidate and risperidone, showed significant efficacy in reducing these symptoms compared to the other psychotropic agents30,46,66.
For reducing disruptive symptoms, the effect size of only second-generation antipsychotics (SMD = 0.668) was large enough to be compatible with treatment of other primary/secondary symptoms of, for example, schizophrenia67 or autistic spectrum disorder68,69 in youths. Stimulants (SMD = 0.633) also showed the efficacy for reducing disruptive symptoms, but the effect size was relatively small or similar compared to the impact on main symptoms of ADHD (SMD over 0.8 and 0.6 for hyperactivity and inattention)70,71,72. The effect sizes of the other agent groups were small to medium (SMD values of 0.3–0.5) for disruptive symptoms, and generally lower than the effect size found in previous meta-analyses for these agents in reducing primary symptoms of ADHD (non-stimulant ADHD medication: SMD over 0.7 and 0.5 for hyperactivity and inattention)70,71,72, Tourette’s disorder (dopamine receptor modulator: SMD over 0.5 for tic)25,73, and depression (SSRI: SMD over 0.5 for depression)48,74. Therefore, while our results show that stimulants, dopamine receptor modulators, SSRIs, and non-stimulant ADHD medications may all decrease disruptive symptoms and may have neural level impacts on the pathophysiology of disruptive behavior in youths with various psychiatric disorders, the magnitude of their effect might be lower than that found in treatment of primary symptoms of specific disorders.
The fact that psychotropic medications with dopaminergic affinity (i.e., second-generation antipsychotics, stimulants, and dopamine receptor modulators) were significantly efficacious for reducing disruptive behavior problems indicates that while the exact nature of dopamine’s relationship to disruptive behavior is not completely understood, dysfunction in the dopaminergic system itself may play a significant role in youths’ response to these medications (e.g. reducing affective aggression)30,75,76. Consideration should be given to the fact that although stimulants and second-generation antipsychotics both impact the dopaminergic system, their specific mechanisms of action are quite different (i.e., methylphenidate is a dopamine agonist, but risperidone and olanzapine are D2 receptor and 5-HT2a antagonists).
A simplistic view of dopamine in mental disorders and their treatment has been that Dopamine levels are either too high or too low in specific brain regions. This may not, however, be sufficient to provide an explanation of the nature of dopaminergic dysfunction in various clinical presentations77,78,79,80,81. One potential explanation is that while stimulants and second-generation antipsychotics seem to have different mechanisms of action, they both result in augmenting tonic dopamine levels and reducing exaggerated phasic responses79,81. Secondly, it is also possible that not only the stimulants, but also the second-generation antipsychotics may directly affect top-down modulation by facilitating dopaminergic neurotransmission in the prefrontal cortex, even if they primarily affect the limbic system. It has been shown that acute treatment with second-generation antipsychotics, especially risperidone and olanzapine, increases the extracellular levels of dopamine in the prefrontal cortex (one of the main areas implicated in top-down modulation) as well as the nucleus accumbens82,83. The increased dopamine level in the nucleus accumbens induced by second-generation antipsychotics may mainly be due to the blockade of presynaptic D2 receptors84, since D2/3 receptor affinities of antipsychotics is associated with their preferential effects on dopamine levels there82. Since most prefrontal dopaminergic neurons do not possess D2 auto receptors, the increase dopamine release in the prefrontal cortex induced by second-generation antipsychotics appears to involve additional receptors85. Serotonergic pathways might also influence the regulation of extracellular dopamine in the prefrontal cortex86. Local activation of 5-HT2A receptors in the prefrontal cortex influences dopamine neuron activity in the ventral tegmental area and dopamine release in the mesocortical pathway87. The combined effects on D2 and 5-HT2A antagonism induced by second-generation antipsychotics (not just by reducing dopaminergic action) may have a more complex mechanism of reducing disruptive behavior in youths.
Clinically there has been concern that the effect of second-generation antipsychotics on disruptive symptoms is merely a product of their sedating effect88, due to their anti-histaminergic and anti-cholinergic actions89, however, it is also possible that these systems may play a critical role in disruptive behavior symptoms90,91. The fact that both stimulants and second-generation antipsychotics can exercise their impact on the neural areas of bottom-up emotional processing in addition to top-down cognitive control92, indicates that the symptoms of disruptive behavior may be driven by more complex mechanisms, which requires further future study.
In sum, the present NMA demonstrated that stimulants (i.e., methylphenidate) and second-generation antipsychotics, specifically risperidone, have large effect sizes in the treatment of DBs in children and youths, while mood stabilizers, SNRIs, α-2 agonists and antidepressants showed low to medium effect sizes. These results suggest that those agents with a higher affinity for dopamine receptors may be useful in the management of DBs, a result consistent with the hypothesis that DBs are due to deficits in the top-down inhibitory processes in the mesolimbic dopamine system.
There are a few caveats to offer. While this review examined various psychotropic medications for the treatment of symptoms of disruptive behavior, it did not take into account administration method, dosage or duration of treatment, safety or tolerability issues, or the age, gender and race/ethnicity of participants. These were not explored due to lack of reported information.
Secondly, we excluded studies that combined two or more psychotropic medications or psychotropic medication with other modalities of treatment (behavioral intervention/therapy) due to limitations of statistical analysis. We also did not examine studies that implemented neurobiological assessment methods to evaluate the neural level changes in the underlying pathophysiology of disruptive behavior (such as neuroimaging or genetics) to reduce measurement heterogeneity. Future study is warranted on these as well.
Third, some agent groups had small sample sizes, such as lithium (n = 27) and TCAs (SNRI) (n = 48). Previous work suggests that treatment efficacy would be overestimated in studies with small sample sizes93, therefore, it might be difficult to accurately assess the treatment efficacy of lithium and TCAs for DBs.
Fourth, because the symptom indicators for DBs applied in this study included symptoms in the context of externalizing disorders (i.e., ADHD, CD, ODD, DBD), there is a disparity in sample size between externalizing and internalizing disorders. The generalization of our findings to the full spectrum of pediatric psychiatric symptoms is therefore limited by the inability to interpret findings in symptoms manifested in internalizing disorders (i.e., depressive disorders, anxiety disorders, obsessive–compulsive and related disorders, trauma and stress-related disorders, and dissociative disorders). DBs in Autism Spectrum Disorder are a significant clinical issue, but these may or may not share the mechanisms of DBs in the externalizing disorders94,95. Thus, although in many cases stimulants and antipsychotic medications are being used for DBs in Autism Spectrum Disorders94, our current finding may not apply to those cases, and future study is necessary. In addition, disruptive behavior problems in other psychiatric diagnoses (such as BD and psychotic disorder) in children and adolescents may benefit from a separate and comprehensive study with similar design as this, since the underlying neurobiological mechanism of disruptive behavior problem in those diagnoses may significantly differ from the ones included in the current study96,97.
Lastly, including studies with various scales to measure DB symptoms may potentially limit interpretability. The analysis methodology we used (NMA), however, allows us to pool data from different trials with similar treatment arms, to measure relative effects of interventions98. In addition, all of the studies that were included in the NMA implemented the scales to measure similar if not identical disruptive behavior elements, such as oppositional/defiance, overt aggression, and hyperactivity/impulsivity (see Table 2)99. Previous studies demonstrated high levels of overlap and strong correlations of these symptoms with each other100.
Despite these limitations, our study was able to identify the efficacy of various psychotropic medications for treating the various symptoms of disruptive behavior, and speculates that this efficacy may be related to the mechanism of action of medications at the neural level. In particular, psychotropic medications with dopaminergic affinity, especially the second-generation antipsychotics, were particularly efficacious in treating the symptoms of disruptive behavior.
Clinical implication and conclusion
Based on this review, several pharmacotherapies such as second-generation antipsychotics and stimulants may have potential efficacy for the treatment of disruptive behavior symptoms in the psychiatric diagnoses included in our study. This may be a first step toward refining and individualizing treatment options for youth with externalizing disorders, as well as eventually improving our understanding of the underlying neurobiological mechanisms of disruptive behavior in these diagnoses. Future study may consider incorporating a trans-diagnostic concept into designing RCTs targeting DBs.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Change history
09 January 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41598-023-51047-7
Abbreviations
- ADHD:
-
Attention deficit hyperactivity disorder
- ANX:
-
Anxiety disorder
- ASD:
-
Autism spectrum disorder
- BD:
-
Bipolar disorder
- CD:
-
Conduct disorder
- DBD:
-
Disruptive behavior disorder
- DB:
-
Disruptive behavior
- DRA:
-
Dopamine receptor antagonist/dopamine receptor modulator
- GRA:
-
GABA receptor agonists
- MDD:
-
Major depressive disorder
- NDRI:
-
Norepinephrine–dopamine reuptake inhibitor/stimulant
- NMA:
-
Network meta-analysis
- OCD:
-
Obsessive–compulsive disorder
- ODD:
-
Oppositional defiant disorder
- PDD:
-
Pervasive developmental disorder
- RCT:
-
Random control trial
- SDA:
-
Serotonin dopamine antagonist/second-generation antipsychotics
- SMD:
-
Standardized mean differences
- SNDRI:
-
Serotonin-norepinephrine-dopamine reuptake inhibitor
- sNRI:
-
Selective norepinephrine reuptake inhibitors/non-stimulant ADHD medication
- SNRI:
-
Serotonin-norepinephrine reuptake inhibitors/tricyclic antidepressants
- SSRI:
-
Selective serotonin reuptake inhibitor
References
Breitenstein, S. M., Hill, C. & Gross, D. Understanding disruptive behavior problems in preschool children. J. Pediatr. Nurs. 24(1), 3–12 (2009).
Shaw, D. S., Owens, E. B., Vondra, J. I., Keenan, K. & Winslow, E. B. Early risk factors and pathways in the development of early disruptive behavior problems. Dev. Psychopathol. 8(4), 679–699 (1996).
Eyberg, S. M., Nelson, M. M. & Boggs, S. R. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. J. Clin. Child Adolesc. Psychol. 37(1), 215–237 (2008).
Milone, A., Sesso, G. Disruptive Behavior Disorders: Symptoms, Evaluation and Treatment. 225 (Multidisciplinary Digital Publishing Institute, 2022).
Campbell, S. B. Behavior Problems in Preschool Children: Clinical and Developmental Issues. (Guilford Press, 2006).
Loeber, R. & Dishion, T. Early predictors of male delinquency: A review. Psychol. Bull. 94(1), 68 (1983).
Bonadio, F. T., Dynes, M., Lackey, J., Tompsett, C. & Amrhein, K. Grouping youth with similar symptoms: A person-centered approach to transdiagnostic subgroups. J. Clin. Psychol. 72(7), 676–688 (2016).
Lanza, S. T. & Rhoades, B. L. Latent class analysis: An alternative perspective on subgroup analysis in prevention and treatment. Prev. Sci. 14(2), 157–168 (2013).
Brodbeck, J. et al. The structure of psychopathological symptoms and the associations with DSM-diagnoses in treatment seeking individuals. Compr. Psychiatry 55(3), 714–726 (2014).
Kessler, R. C., Chiu, W. T., Demler, O. & Walters, E. E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62(6), 617–627 (2005).
Cook, S. C., Schwartz, A. C. & Kaslow, N. J. Evidence-based psychotherapy: Advantages and challenges. Neurotherapeutics 14(3), 537–545 (2017).
Thomas, J. M. & Guskin, K. A. Disruptive behavior in young children: What does it mean?. J. Am. Acad. Child Adolesc. Psychiatry 40(1), 44–51 (2001).
Vander Stoep, A. et al. Identifying comorbid depression and disruptive behavior disorders: Comparison of two approaches used in adolescent studies. J. Psychiatr. Res. 46(7), 873–881 (2012).
August, G. J., Realmuto, G. M., MacDonald, A. W., Nugent, S. M. & Crosby, R. Prevalence of ADHD and comorbid disorders among elementary school children screened for disruptive behavior. J. Abnorm. Child Psychol. 24(5), 571–595 (1996).
Hawks, J. L., Kennedy, S. M., Holzman, J. B. & Ehrenreich-May, J. Development and application of an innovative transdiagnostic treatment approach for pediatric irritability. Behav. Ther. 51(2), 334–349 (2020).
Hsieh, I.-J. & Chen, Y. Y. Determinants of aggressive behavior: Interactive effects of emotional regulation and inhibitory control. PLoS One 12(4), e0175651 (2017).
Blair, R. J. R. The neurobiology of psychopathic traits in youths. Nat. Rev. Neurosci. 14(11), 786–799 (2013).
Buhle, J. T. et al. Cognitive reappraisal of emotion: A meta-analysis of human neuroimaging studies. Cereb. Cortex 24(11), 2981–2990 (2014).
Hwang, S. et al. Dual neurocircuitry dysfunctions in disruptive behavior disorders: Emotional responding and response inhibition. Psychol. Med. 46(7), 1485–1496 (2016).
Ridderinkhof, K. R., Van Den Wildenberg, W. P., Segalowitz, S. J. & Carter, C. S. Neurocognitive mechanisms of cognitive control: The role of prefrontal cortex in action selection, response inhibition, performance monitoring, and reward-based learning. Brain Cogn. 56(2), 129–140 (2004).
Goghari, V. M. & MacDonald, A. W. III. The neural basis of cognitive control: Response selection and inhibition. Brain Cogn. 71(2), 72–83 (2009).
Potegal, M. Temporal and frontal lobe initiation and regulation of the top-down escalation of anger and aggression. Behav. Brain Res. 231(2), 386–395 (2012).
Lischinsky, J. E. & Lin, D. Neural mechanisms of aggression across species. Nat. Neurosci. 23(11), 1317–1328 (2020).
Beauchaine, T. P. Future directions in emotion dysregulation and youth psychopathology. J. Clin. Child Adolesc. Psychol. 44(5), 875–896 (2015).
Seo, D., Patrick, C. J. & Kennealy, P. J. Role of serotonin and dopamine system interactions in the neurobiology of impulsive aggression and its comorbidity with other clinical disorders. Aggress. Violent. Behav. 13(5), 383–395 (2008).
Daw, N. D., Kakade, S. & Dayan, P. Opponent interactions between serotonin and dopamine. Neural Netw. 15(4–6), 603–616 (2002).
Jalain, C. I. The impact of serotonin and dopamine on human aggression: A systematic review of the literature. (2014).
Shih, H.-H., Shang, C.-Y. & Gau, S. S. F. Comparative efficacy of methylphenidate and atomoxetine on emotional and behavioral problems in youths with attention-deficit/hyperactivity disorder. J. Child Adolesc. Psychopharmacol. 29(1), 9–19 (2019).
Coghill, D. R., Rhodes, S. M. & Matthews, K. The neuropsychological effects of chronic methylphenidate on drug-naive boys with attention-deficit/hyperactivity disorder. Biol. Psychiat. 62(9), 954–962 (2007).
Gadow, K. D. et al. Severely aggressive children receiving stimulant medication versus stimulant and risperidone: 12-month follow-up of the TOSCA trial. J. Am. Acad. Child Adolesc. Psychiatry 55(6), 469–478 (2016).
Hinshaw, S. P. Stimulant medication and the treatment of aggression in children with attentional deficits. J. Clin. Child Adolesc. Psychol. 20(3), 301–312 (1991).
Bangs, M. E. et al. Atomoxetine for the treatment of attention-deficit/hyperactivity disorder and oppositional defiant disorder. Pediatrics 121(2), e314–e320 (2008).
Dell’Agnello, G. et al. Atomoxetine hydrochloride in the treatment of children and adolescents with attention-deficit/hyperactivity disorder and comorbid oppositional defiant disorder: A placebo-controlled Italian study. Eur. Neuropsychopharmacol. 19(11), 822–834 (2009).
Kelsey, D. K. et al. Once-daily atomoxetine treatment for children with attention-deficit/hyperactivity disorder, including an assessment of evening and morning behavior: A double-blind, placebo-controlled trial. Pediatrics 114(1), e1–e8 (2004).
Findling, R. L. et al. A double-blind pilot study of risperidone in the treatment of conduct disorder. J. Am. Acad. Child Adolesc. Psychiatry 39(4), 509–516 (2000).
Aman, M. G. et al. Double-blind, placebo-controlled study of risperidone for the treatment of disruptive behaviors in children with subaverage intelligence. Am. J. Psychiatry. 159(8), 1337–1346 (2002).
Snyder, R. et al. Effects of risperidone on conduct and disruptive behavior disorders in children with subaverage IQs. J. Am. Acad. Child Adolesc. Psychiatry 41(9), 1026–1036 (2002).
Connor, D. F., McLaughlin, T. J. & Jeffers-Terry, M. Randomized controlled pilot study of quetiapine in the treatment of adolescent conduct disorder. J. Child Adolesc. Psychopharmacol. 18(2), 140–156 (2008).
Malone, R. P., Delaney, M. A., Luebbert, J. F., Cater, J. & Campbell, M. A double-blind placebo-controlled study of lithium in hospitalized aggressive children and adolescents with conduct disorder. Arch. Gen. Psychiatry 57(7), 649–654 (2000).
Buitelaar, J. K., Van der Gaag, R. J. & Melman, C. T. A randomized controlled trial of risperidone in the treatment of aggression in hospitalized adolescents with subaverage cognitive abilities. J. Clin. Psychiatry 62(4), 239–248 (2001).
Dickstein, D. P. et al. Randomized double-blind placebo-controlled trial of lithium in youths with severe mood dysregulation. J. Child Adolesc. Psychopharmacol. 19(1), 61–73 (2009).
Hollander, E. et al. Divalproex sodium vs placebo for the treatment of irritability in children and adolescents with autism spectrum disorders. Neuropsychopharmacology 35(4), 990–998 (2010).
Pavuluri, M. N. et al. Double-blind randomized trial of risperidone versus divalproex in pediatric bipolar disorder. Bipolar Disord. 12(6), 593–605 (2010).
O’Connor, N. & Corish, J. Pharmacological management of acute severe behavioural disturbance: A survey of current protocols. Australas. Psychiatry 25(4), 395–398 (2017).
Gurnani, T., Ivanov, I. & Newcorn, J. H. Pharmacotherapy of aggression in child and adolescent psychiatric disorders. J. Child Adolesc. Psychopharmacol. 26(1), 65–73 (2016).
Pringsheim, T., Hirsch, L., Gardner, D. & Gorman, D. A. The pharmacological management of oppositional behaviour, conduct problems, and aggression in children and adolescents with attention-deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder: A systematic review and meta-analysis. Part 1: psychostimulants, alpha-2 agonists, and atomoxetine. Can. J. Psychiatry. 60(2), 42–51 (2015).
Finckh, A. & Tramèr, M. R. Primer: Strengths and weaknesses of meta-analysis. Nat. Clin. Pract. Rheumatol. 4(3), 146–152 (2008).
Cipriani, A. et al. Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: A network meta-analysis. Lancet 388(10047), 881–890 (2016).
Rouse, B., Chaimani, A. & Li, T. Network meta-analysis: An introduction for clinicians. Intern. Emerg. Med. 12(1), 103–111 (2017).
White, I. R. Network meta-analysis. Stand. Genom. Sci. 15(4), 951–985 (2015).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 8(5), 336–341 (2010).
Vassar, M., Atakpo, P. & Kash, M. J. Manual search approaches used by systematic reviewers in dermatology. J. Med. Libr. Assoc. JMLA. 104(4), 302 (2016).
Brestan, E. V. & Eyberg, S. M. Effective psychosocial treatments of conduct-disordered children and adolescents: 29 years, 82 studies, and 5,272 kids. J. Clin. Child Psychol. 27(2), 180–189 (1998).
Higgins, J. P. et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343, 5928 (2011).
Rücker, G. & Schwarzer, G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med. Res. Methodol. 15(1), 1–9 (2015).
Jansen, J. P. et al. Interpreting indirect treatment comparisons and network meta-analysis for health-care decision making: Report of the ISPOR Task Force on Indirect Treatment Comparisons Good Research Practices: Part 1. Value Health. 14(4), 417–428 (2011).
Dias, S., Sutton, A. J., Ades, A. & Welton, N. J. Evidence synthesis for decision making 2: A generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med. Decis. Making 33(5), 607–617 (2013).
You, R. et al. The changing therapeutic role of chemo-radiotherapy for loco-regionally advanced nasopharyngeal carcinoma from two/three-dimensional radiotherapy to intensity-modulated radiotherapy: A network meta-analysis. Theranostics. 7(19), 4825 (2017).
Collaboration, C. Cochrane handbook: General methods for Cochrane reviews. Heterogeneity. (2014).
Ribassin-Majed, L. et al. What is the best treatment of locally advanced nasopharyngeal carcinoma? An individual patient data network meta-analysis. J. Clin. Oncol. 35(5), 498 (2017).
Krahn, U., Binder, H. & König, J. Visualizing inconsistency in network meta-analysis by independent path decomposition. BMC Med. Res. Methodol. 14(1), 1–12 (2014).
Neupane, B., Richer, D., Bonner, A. J., Kibret, T. & Beyene, J. Network meta-analysis using R: A review of currently available automated packages. PLoS ONE 9(12), e115065 (2014).
Sterne, J. A. & Egger, M. Funnel plots for detecting bias in meta-analysis: Guidelines on choice of axis. J. Clin. Epidemiol. 54(10), 1046–1055 (2001).
Salanti, G., Ades, A. & Ioannidis, J. P. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: An overview and tutorial. J. Clin. Epidemiol. 64(2), 163–171 (2011).
Najafi, Z., Taghadosi, M., Sharifi, K., Farrokhian, A., Tagharrobi, Z. The effects of inhalation aromatherapy on anxiety in patients with myocardial infarction: A randomized clinical trial. Iran. Red Crescent Med. J. 16(8) (2014).
Pappadopulos, E., Woolston, S., Chait, A., Perkins, M., Connor, D. F., Jensen, P. S. Pharmacotherapy of aggression in children and adolescents: Efficacy and effect size. J. Can. Acad. Child Adolesc. Psychiatry/Journal de l'Académie canadienne de psychiatrie de l'enfant et de l'adolescent. (2006).
Sarkar, S. & Grover, S. Antipsychotics in children and adolescents with schizophrenia: A systematic review and meta-analysis. Indian J. Pharmacol. 45(5), 439 (2013).
Sharma, A. & Shaw, S. R. Efficacy of risperidone in managing maladaptive behaviors for children with autistic spectrum disorder: A meta-analysis. J. Pediatr. Health Care 26(4), 291–299 (2012).
D’Alò, G. L. et al. Impact of antipsychotics in children and adolescents with autism spectrum disorder: A systematic review and meta-analysis. Health Qual. Life Outcomes 19(1), 1–19 (2021).
Faraone, S. V. & Buitelaar, J. Comparing the efficacy of stimulants for ADHD in children and adolescents using meta-analysis. Eur. Child Adolesc. Psychiatry 19(4), 353–364 (2010).
Rodrigues, R. et al. Practitioner review: Pharmacological treatment of attention-deficit/hyperactivity disorder symptoms in children and youth with autism spectrum disorder: A systematic review and meta-analysis. J. Child Psychol. Psychiatry 62(6), 680–700 (2021).
Patra, S., Nebhinani, N., Viswanathan, A. & Kirubakaran, R. Atomoxetine for attention deficit hyperactivity disorder in children and adolescents with autism: A systematic review and meta-analysis. Autism Res. 12(4), 542–552 (2019).
Liu, Y. et al. Effectiveness and tolerability of aripiprazole in children and adolescents with Tourette’s disorder: A meta-analysis. J. Child Adolesc. Psychopharmacol. 26(5), 436–441 (2016).
Qin, B. et al. Selective serotonin reuptake inhibitors versus tricyclic antidepressants in young patients: A meta-analysis of efficacy and acceptability. Clin. Ther. 36(7), 1087–954.e4 (2014).
Comai, S., Tau, M. & Gobbi, G. The psychopharmacology of aggressive behavior: A translational approach. Part 1 neurobiology. J. Clin. Psychopharmacol. 32(1), 83–94 (2012).
Narvaes, R. & Martins de Almeida, R. M. Aggressive behavior and three neurotransmitters: Dopamine, GABA, and serotonin—A review of the last 10 years. Psychol. Neurosci. 7(4), 601 (2014).
Yanofski, J. The dopamine dilemma: Using stimulants and antipsychotics concurrently. Psychiatry (Edgmont) 7(6), 18 (2010).
Grace, A. A. Phasic versus tonic dopamine release and the modulation of dopamine system responsivity: A hypothesis for the etiology of schizophrenia. Neuroscience 41(1), 1–24 (1991).
Braun, A., Laruelle, M. & Mouradian, M. Interactions between D1 and D2 dopamine receptor family agonists and antagonists: The effects of chronic exposure on behavior and receptor binding in rats and their clinical implications. J. Neural Transm. 104(4), 341–362 (1997).
Samaha, A.-N., Seeman, P., Stewart, J., Rajabi, H. & Kapur, S. “Breakthrough” dopamine supersensitivity during ongoing antipsychotic treatment leads to treatment failure over time. J. Neurosci. 27(11), 2979–2986 (2007).
Gianutsos, G., Hynes, M. D., Puri, S. K., Drawbaugh, R. B. & Lal, H. Effect of apomorphine and nigrostriatal lesions on aggression and striatal dopamine turnover during morphine withdrawal: Evidence for dopaminergic supersensitivity in protracted abstinence. Psychopharmacologia 34(1), 37–44 (1974).
Kuroki, T., Meltzer, H. Y. & Ichikawa, J. Effects of antipsychotic drugs on extracellular dopamine levels in rat medial prefrontal cortex and nucleus accumbens. J. Pharmacol. Exp. Ther. 288(2), 774–781 (1999).
Mørk, A., Witten, L. M. & Arnt, J. Effect of sertindole on extracellular dopamine, acetylcholine, and glutamate in the medial prefrontal cortex of conscious rats: A comparison with risperidone and exploration of mechanisms involved. Psychopharmacology 206(1), 39–49 (2009).
Westerink, B. & De Vries, J. On the mechanism of neuroleptic induced increase in striatal dopamine release: Brain dialysis provides direct evidence for mediation by autoreceptors localized on nerve terminals. Neurosci. Lett. 99(1–2), 197–202 (1989).
Lammel, S. et al. Unique properties of mesoprefrontal neurons within a dual mesocorticolimbic dopamine system. Neuron 57(5), 760–773 (2008).
Li, Z. et al. ACP-103, a 5-HT2A/2C inverse agonist, potentiates haloperidol-induced dopamine release in rat medial prefrontal cortex and nucleus accumbens. Psychopharmacology 183(2), 144–153 (2005).
Bortolozzi, A., Díaz-Mataix, L., Scorza, M. C., Celada, P. & Artigas, F. The activation of 5-HT2A receptors in prefrontal cortex enhances dopaminergic activity. J. Neurochem. 95(6), 1597–1607 (2005).
Volavka, J. & Citrome, L. Atypical antipsychotics in the treatment of the persistently aggressive psychotic patient: Methodological concerns. Schizophr. Res. 35, S23–S33 (1999).
Wetterling, T. Bodyweight gain with atypical antipsychotic. Drug Saf. 24(1), 59–73 (2001).
Reichmann, F. et al. The zebrafish histamine H3 receptor modulates aggression, neural activity and forebrain functional connectivity. Acta Physiol. 230(4), e13543 (2020).
Pavlou, H. J., Neville, M. C. & Goodwin, S. F. Aggression: Tachykinin is all the rage. Curr. Biol. 24(6), R243–R244 (2014).
Tarazi, F. I., Zhang, K. & Baldessarini, R. J. Long-term effects of olanzapine, risperidone, and quetiapine on dopamine receptor types in regions of rat brain: Implications for antipsychotic drug treatment. J. Pharmacol. Exp. Ther. 297(2), 711–717 (2001).
Nüesch, E. et al. Small study effects in meta-analyses of osteoarthritis trials: Meta-epidemiological study. BMJ 341, c3515 (2010).
Kaat, A. J. & Lecavalier, L. Disruptive behavior disorders in children and adolescents with autism spectrum disorders: A review of the prevalence, presentation, and treatment. Res. Autism Spectr. Disord. 7(12), 1579–1594 (2013).
Cai, R. Y., Richdale, A. L., Uljarević, M., Dissanayake, C. & Samson, A. C. Emotion regulation in autism spectrum disorder: Where we are and where we need to go. Autism Res. 11(7), 962–978 (2018).
Swann, A. C. Antisocial personality and bipolar disorder: Interactions in impulsivity and course of illness. Neuropsychiatry 1(6), 599 (2011).
Buchmann, A., Hohmann, S., Brandeis, D., Banaschewski, T., Poustka, L. Aggression in children and adolescents. Neurosci. Aggress. 421–442 (2014).
Salanti, G., Higgins, J. P., Ades, A. & Ioannidis, J. P. Evaluation of networks of randomized trials. Stat. Methods Med. Res. 17(3), 279–301 (2008).
Martel, M. M., Gremillion, M. L. & Roberts, B. Temperament and common disruptive behavior problems in preschool. Personal. Individ. Differ. 53(7), 874–879 (2012).
Olson, S. L. et al. Deconstructing the externalizing spectrum: Growth patterns of overt aggression, covert aggression, oppositional behavior, impulsivity/inattention, and emotion dysregulation between school entry and early adolescence. Dev. Psychopathol. 25(3), 817–842 (2013).
Bukstein, O. G. & Kolko, D. J. Effects of methylphenidate on aggressive urban children with attention deficit hyperactivity disorder. J. Clin. Child Psychol. 27(3), 340–351 (1998).
Evans, S. W. et al. Dose–response effects of methylphenidate on ecologically valid measures of academic performance and classroom behavior in adolescents with ADHD. Exp. Clin. Psychopharmacol. 9(2), 163 (2001).
Findling, R. L. et al. Methylphenidate in the treatment of children and adolescents with bipolar disorder and attention-deficit/hyperactivity disorder. J. Am. Acad. Child Adolesc. Psychiatry 46(11), 1445–1453 (2007).
Gorman, E. B., Klorman, R., Thatcher, J. E. & Borgstedt, A. D. Effects of methylphenidate on subtypes of attention-deficit/hyperactivity disorder. J. Am. Acad. Child Adolesc. Psychiatry 45(7), 808–816 (2006).
Handen, B. L., Johnson, C. R. & Lubetsky, M. Efficacy of methylphenidate among children with autism and symptoms of attention-deficit hyperactivity disorder. J. Autism Dev. Disord. 30(3), 245–255 (2000).
Huang, Y.-S., Yeh, C.-B., Chen, C.-H., Shang, C.-Y. & Gau, S.S.-F. A randomized, double-blind, placebo-controlled, two-way crossover clinical trial of ORADUR-methylphenidate for treating children and adolescents with attention-deficit/hyperactivity disorder. J. Child Adolesc. Psychopharmacol. 31(3), 164–178 (2021).
Kaplan, S. L., Busner, J., Kupietz, S., Wassermann, E. & Segal, B. Effects of methylphenidate on adolescents with aggressive conduct disorder and ADDH: A preliminary report. J. Am. Acad. Child Adolesc. Psychiatry 29(5), 719–723 (1990).
Klein, R. G. et al. Clinical efficacy of methylphenidate in conduct disorder with and without attention deficit hyperactivity disorder. Arch. Gen. Psychiatry 54(12), 1073–1080 (1997).
Kolko, D. J., Bukstein, O. G. & Barron, J. Methylphenidate and behavior modification in children with ADHD and comorbid ODD or CD: Main and incremental effects across settings. J. Am. Acad. Child Adolesc. Psychiatry 38(5), 578–586 (1999).
Pelham, W. E. et al. A comparison of morning-only and morning/late afternoon Adderall to morning-only, twice-daily, and three times-daily methylphenidate in children with attention-deficit/hyperactivity disorder. Pediatrics 104(6), 1300–1311 (1999).
Pelham, W. E. et al. Transdermal methylphenidate, behavioral, and combined treatment for children with ADHD. Exp. Clin. Psychopharmacol. 13(2), 111 (2005).
Pliszka, S. R. et al. The Texas Children’s Medication Algorithm Project: Report of the Texas Consensus Conference Panel on medication treatment of childhood attention-deficit/hyperactivity disorder. Part I. J. Am. Acad. Child Adolesc. Psychiatry. 39(7), 908–919 (2000).
Posey, D. J. et al. Positive effects of methylphenidate on inattention and hyperactivity in pervasive developmental disorders: An analysis of secondary measures. Biol. Psychiat. 61(4), 538–544 (2007).
Sinzig, J., Döpfner, M., Lehmkuhl, G. & Group, G. M. S. Long-acting methylphenidate has an effect on aggressive behavior in children with attention-deficit/hyperactivity disorder. J. Child Adolesc. Psychopharmacol. 17(4), 421–432 (2007).
Wolraich, M. L. et al. Randomized, controlled trial of OROS methylphenidate once a day in children with attention-deficit/hyperactivity disorder. Pediatrics 108(4), 883–892 (2001).
Arnold, L. E. et al. Atomoxetine for hyperactivity in autism spectrum disorders: Placebo-controlled crossover pilot trial. J. Am. Acad. Child Adolesc. Psychiatry 45(10), 1196–1205 (2006).
Dittmann, R. W. et al. Atomoxetine versus placebo in children and adolescents with attention-deficit/hyperactivity disorder and comorbid oppositional defiant disorder: A double-blind, randomized, multicenter trial in Germany. J. Child Adolesc. Psychopharmacol. 21(2), 97–110 (2011).
Gau, S. S. et al. A randomized, double-blind, placebo-controlled clinical trial on once-daily atomoxetine hydrochloride in Taiwanese children and adolescents with attention-deficit/hyperactivity disorder. J. Child Adolesc. Psychopharmacol. 17(4), 447–460 (2007).
Kaplan, S. et al. Efficacy and safety of atomoxetine in childhood attention-deficit/hyperactivity disorder with comorbid oppositional defiant disorder. J. Atten. Disord. 8(2), 45–52 (2004).
Michelson, D. et al. Atomoxetine in the treatment of children and adolescents with attention-deficit/hyperactivity disorder: A randomized, placebo-controlled, dose-response study. Pediatrics 108(5), e83-e (2001).
Michelson, D. et al. Once-daily atomoxetine treatment for children and adolescents with attention deficit hyperactivity disorder: A randomized, placebo-controlled study. Am. J. Psychiatry 159(11), 1896–1901 (2002).
Michelson, D. et al. Relapse prevention in pediatric patients with ADHD treated with atomoxetine: A randomized, double-blind, placebo-controlled study. J. Am. Acad. Child Adolesc. Psychiatry 43(7), 896–904 (2004).
Montoya, A. et al. Evaluation of atomoxetine for first-line treatment of newly diagnosed, treatment-naive children and adolescents with attention deficit/hyperactivity disorder. Curr. Med. Res. Opin. 25(11), 2745–2754 (2009).
Weiss, M. et al. A randomized, placebo-controlled study of once-daily atomoxetine in the school setting in children with ADHD. J. Am. Acad. Child Adolesc. Psychiatry 44(7), 647–655 (2005).
Aman, M. G., Binder, C. & Turgay, A. Risperidone effects in the presence/absence of psychostimulant medicine in children with ADHD, other disruptive behavior disorders, and subaverage IQ. J. Child Adolesc. Psychopharmacol. 14(2), 243–254 (2004).
Findling, R. L. et al. Long-term, open-label study of risperidone in children with severe disruptive behaviors and below-average IQ. Am. J. Psychiatry. 161(4), 677–684 (2004).
LeBlanc, J. C. et al. Risperidone reduces aggression in boys with a disruptive behaviour disorder and below average intelligence quotient: Analysis of two placebo-controlled randomized trials. Int. Clin. Psychopharmacol. 20(5), 275–283 (2005).
Pandina, G. J., Bossie, C. A., Youssef, E., Zhu, Y. & Dunbar, F. Risperidone improves behavioral symptoms in children with autism in a randomized, double-blind, placebo-controlled trial. J. Autism Dev. Disord. 37(2), 367–373 (2007).
Razjouyan, K., Danesh, A., Khademi, M., Davari-Ashtiani, R. & Noorbakhsh, S. A comparative study of risperidone and aripiprazole in attention deficit hyperactivity disorder in children under six years old: A randomized double-blind study. Iran. J. Pediatr. 28(1), 1–8 (2018).
Reyes, M., Buitelaar, J., Toren, P., Augustyns, I. & Eerdekens, M. A randomized, double-blind, placebo-controlled study of risperidone maintenance treatment in children and adolescents with disruptive behavior disorders. Am. J. Psychiatry 163(3), 402–410 (2006).
Shea, S. et al. Risperidone in the treatment of disruptive behavioral symptoms in children with autistic and other pervasive developmental disorders. Pediatrics 114(5), e634–e641 (2004).
Safavi, P., Hasanpour-Dehkordi, A. & AmirAhmadi, M. Comparison of risperidone and aripiprazole in the treatment of preschool children with disruptive behavior disorder and attention deficit-hyperactivity disorder: A randomized clinical trial. J. Adv. Pharm. Technol. Res. 7(2), 43 (2016).
Tohen, M. et al. Olanzapine versus placebo in the treatment of adolescents with bipolar mania. Am. J. Psychiatry 164(10), 1547–1556 (2007).
Carlson, G. A., Rapport, M. D., Pataki, C. S. & Kelly, K. L. Lithium in hospitalized children at 4 and 8 weeks: Mood, behavior and cognitive effects. J. Child Psychol. Psychiatry 33(2), 411–425 (1992).
Sallee, F. et al. Randomized, double-blind, placebo-controlled trial demonstrates the efficacy and safety of oral aripiprazole for the treatment of Tourette’s disorder in children and adolescents. J. Child Adolesc. Psychopharmacol. 27(9), 771–781 (2017).
Reddihough, D. S. et al. Effect of fluoxetine on obsessive-compulsive behaviors in children and adolescents with autism spectrum disorders: A randomized clinical trial. JAMA 322(16), 1561–1569 (2019).
Potter, L. A. et al. A randomized controlled trial of sertraline in young children with autism spectrum disorder. Front. Psychiatry. 10, 810 (2019).
Cueva, J. E. et al. Carbamazepine in aggressive children with conduct disorder: A double-blind and placebo-controlled study. J. Am. Acad. Child Adolesc. Psychiatry 35(4), 480–490 (1996).
Hellings, J. A. et al. A double-blind, placebo-controlled study of valproate for aggression in youth with pervasive developmental disorders. J. Child Adolesc. Psychopharmacol. 15(4), 682–692 (2005).
Klein, R. G., Koplewicz, H. S. & Kanner, A. Imipramine treatment of children with separation anxiety disorder. J. Am. Acad. Child Adolesc. Psychiatry 31(1), 21–28 (1992).
Klein, R. G. et al. Adolescent depression: Controlled desipramine treatment and atypical features. Depress. Anxiety 7(1), 15–31 (1998).
Spencer, T. et al. A double-blind comparison of desipramine and placebo in children and adolescents with chronic tic disorder and comorbid attention-deficit/hyperactivity disorder. Arch. Gen. Psychiatry 59(7), 649–656 (2002).
Findling, R. L. et al. Dasotraline in children with attention-deficit/hyperactivity disorder: A six-week, placebo-controlled, fixed-dose trial. J. Child Adolesc. Psychopharmacol. 29(2), 80–89 (2019).
Acknowledgements
This work was supported by the NIMH U01MH120155-01A1.
Author information
Authors and Affiliations
Contributions
J.S. and S.H. wrote the main manuscript text and B.J.L. and A.A. collected data. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article omitted an affiliation for Ji-Woo Seok. Full information regarding the correction made can be found in the correction for this Article.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seok, JW., Soltis-Vaughan, B., Lew, B.J. et al. Psychopharmacological treatment of disruptive behavior in youths: systematic review and network meta-analysis. Sci Rep 13, 6921 (2023). https://doi.org/10.1038/s41598-023-33979-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-33979-2
This article is cited by
-
Current Status of Psychopharmacological, Neuromodulation, and Oxytocin Treatments for Autism: Implications for Clinical Practice
Advances in Neurodevelopmental Disorders (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.