Abstract
As a novelty, this article proposes the empirical operationalization of an indicator sensitive to nursing care called patient satisfaction based on functional capacity and quality of life assessments. This was a descriptive cross-sectional study with a sample of 351 individuals aged 65 and older residing in the community. Data acquisition was performed using the structured interview method, employing a core set of 25 codes taken from the International Classification of Functioning, Disability, and Health and the WHOQOL-BREF instrument of the World Health Organization. Confirmatory factor analysis was used to infer the reliability and construct validity of the proposed model, involving three latent factors: functional capacity, quality of life, and patient satisfaction with nursing care received. The proposed model showed good reliability and construct validity, although it failed regarding discriminant validity between latent factors. The greatest statistically significant predictor of the patient satisfaction latent factor was the quality of life latent factor (\(\beta =0.89;p<0.001\)), followed by the functional capacity latent factor (\(\beta =-0.77;p<0.001\)). The findings seem to suggest that patient satisfaction is an indicator that may be quantitatively measurable, with functional capacity and quality of life considered very significant predictors of patient satisfaction with the nursing care experience.
Similar content being viewed by others
Introduction
Various international organizations/institutions, such as the World Health Organization (WHO), the United Nations (UN), the World Bank (WB), the Organization for Economic Cooperation and Development (OECD), and the European Commission (EC), among others, have turned the world’s attention to the population aging. The pace of aging has accelerated in the past decade and is expected to accelerate even faster in the next two decades. Similarly, Portugal is expected to be among the OECD countries where population aging will occur “very quickly”1.
Individuals are living longer, as observed by the increase in the demographic indicator life expectancy at birth. However, even though people live longer, these extra years of life are often unhealthy. This finding emerges by comparing the demographic indicators life expectancy at birth and healthy life years at birth (the number of years an individual is expected to live without diseases or disabilities). For example, in the European Union (EU), the number of healthy life years at birth was estimated at 65.1 for women and 64.2 for men, which represents approximately 77.5% (for women) and 81.8% (for men) of the total life expectancy at birth, according to data from EUROSTAT in 20192.
Determining the healthy life years for the population aged 65 and older, whose prevalence of chronic diseases and disabilities is higher, the number of years of healthy life at age 65 (represented by the demographic indicator healthy life years at 65) in the EU, was estimated at 10.4 for women (6.9 for Portugal) and 10.2 for men (7.9 for Portugal), representing approximately 47.7% (for women) and 55.7% (for men) of the total life expectancy at 65 years of age (corresponding to the demographic indicator life expectancy at 65), according to data from EUROSTAT in 20192. Portugal has a much lower position in the ranking of EU countries concerning this demographic indicator, with an estimated total life expectancy at age 65 of 30.9% and 42.7% for women and men, respectively3,4,5,6.
The reduction in the number of healthy life years, which significantly impacts individuals aged 65 and older, is related to the high prevalence of multiple and complex chronic diseases (multimorbidity) that cause disabilities and dependencies. A systematic analysis regarding the “Global Burden of Disease Study 2019” reported that chronic diseases accounted for nine of the top ten causes of death worldwide7.
A National Health Service (NHS) report showed that in 2016, 41% of the Portuguese population had multimorbidity (11% had two chronic diseases, 8% had three, and 22% had four or more chronic diseases), and 18% already reported one chronic disease. The same report found that multimorbidity increases with age and is more prevalent in women than men8. According to work developed by Rodrigues et al.9 in 2018, the authors reported an even higher prevalence of multimorbidity among individuals aged 65 and older, estimated at 78.3% for the Portuguese population sample used in their research (estimates reported by age groups of 65–69, 70–74, 75–79 and 80 years and older were: 72.8%, 78.2%, 81.9%, and 83.4%, respectively).
Individuals with multimorbidity need long-term care provided by multidisciplinary teams that provide integration and continuity of care. However, in most health systems in Europe, care is currently organized around specific diseases, and interventions are often accomplished to improve clinical outcomes10. Unfortunately, this care approach does not adequately respond to the needs of individuals suffering from multimorbidity since care focusing on managing a single disease may be impractical, irrelevant, or even harmful10,11,12. In this regard, the need for health systems to design and provide “person-centered” care aligned with the needs and preferences of the recipient has emerged10,11,12,13.
If “person-centered” care is a central objective of modern health systems, and health decisions are to be shared between caregivers and patients, then action is necessary to reach this goal. However, it still needs to be clarified what individuals aged 65 and older, and their caregivers value in the care they receive, and research on this topic is emerging12. Thus, in recent years, patient satisfaction has emerged as a reflection (outcome) of patients’ experience with the health care received14.
Patient satisfaction has increasingly been considered an essential indicator of the suitability and efficiency of health care delivery, making it possible to understand the extent to which such care produces effective positive changes in the individuals’ health status (suitability) and simultaneously to obtain a measure of the health care system’s performance (efficiency), i.e., an indicator that captures the suitability and efficiency of the delivery of patient-centered quality health care14,15.
Nursing care is one of the main components of health services14 because nurses represent the largest workforce in patient care16. Recent research has been published to assess nursing care’s effect on the recipient’s health, thus providing further visibility to nursing care. This research has added empirical evidence on nursing-sensitive indicators to measure the value of nursing care for patients17,18.
One of the most revealing studies on this topic was published by Dubois et al.16,19, corroborated by Rapin et al.20, and supported by Afaneh et al.18, in which the first authors developed the Nursing Care Performance Framework (NCPF) that included a matrix of indicators related to the main functions of a nursing system, sectioned into three subsystems: (1) acquiring, deploying and maintaining resources; (2) transforming resources into services; and, (3) producing changes in patients' conditions. The third subsystem of the NCPF comprises four indicators that have been summarized into the patient satisfaction indicator, aiming to capture the changes in a patient’s functional status, disease state, or evolving health condition according to the nursing care provided, thus covering the outcomes that reflect16,19: (1) patient comfort and quality of life related to care (patient comfort and quality of life); (2) changes in knowledge, skills, and behaviors at the patient self-care level (patient empowerment); (3) the patient’s functional status (patient functional status); (4) patient safety (risk outcomes and safety).
According to Dubois et al.16,19, patient satisfaction with the nursing care received is a subjective result that reflects the interaction of their expectations of care and their perceptions of actual outcomes resulting from provider services16. Although all the work related to the development of NCPF is theoretical, it is crucial to develop some empirical research related to the operationalization of this indicator, as stated by Dubois et al.16,19.
Thus, this article proposes to empirically operationalize the patient satisfaction indicator of the NCPF, resorting to previous research that assessed the functional capacity (developed by Goes et al.21) and quality of life (developed by Goes et al.22) of individuals aged 65 and older residing in the community. This study’s innovative nature consists of how the patient satisfaction indicator was operationalized, namely by using core indicators sensitive to nursing care (functional capacity and quality of life), instead of employing a single instrument specifically designed to assess patient satisfaction with the nursing care experience.
Methods
Study area, inclusion criteria, and sample size
This cross-sectional and descriptive study involved individuals aged 65 and older residing in the community in the south-central region of mainland Portugal, receiving nursing home care. This area, the Baixo Alentejo Region (BAR), was chosen because it is considered one of the oldest in the country (it has a large proportion of residents aged 65 and older).
The following inclusion criteria were considered: (1) being 65 years of age or older; (2) residing in BAR in their own home or the home of family or friends; (3) being interested in participating in the research; (4) being able to make their own decisions, even if they are ill or hospitalized due to the worsening of their health status; (5) having signed the written informed consent form; and (6) having answered both instruments correctly and entirely (no missing data was allowed).
The Local Health Unit of the RBA (LHUBA) database, containing 32,893 individuals aged 65 and older, was used for the sample composition23. The initial (random) sample included 468 individuals. However, some older adults did not answer correctly and entirely to both instruments during the interviews, resulting in missing data (117 cases). In addition, 32 older adults did not want to participate in the research, so the LHUBA health professionals did not collect their written informed consent forms. For these reasons, only 351 surveys were considered valid, fully meeting all five inclusion criteria mentioned above, and considered for analysis.
Instruments
Two instruments were considered for data collection: (1) the Elderly Nursing Core Set (ENCS); and (2) the WHOQOL-BREF.
The ENCS was the instrument employed to assess older adults' functional capacity. It was developed initially by Fonseca et al. and administered to a sample of institutionalized older adults24. Later, it was administered to a sample of older adults residing in their homes or at family members’ or friends’ homes by Goes et al.21. It comprises 25 questions based on the International Classification of Functioning, Disability, and Health (ICF)25, all scored on a Likert scale ranging from 1 to 5, with higher scores indicating a higher disability level regarding his or her functional capacity. The resulting scores on a 0–100% scale yield the profile of the individual's functional capacity as follows: (1) No disability: 0–4%; (2) Mild disability: 5–24%; (3) Moderate disability: 25–49%; (4) Severe disability: 50–95%; and (5) Complete disability: 96–100%, a feature that was not used in this article25 (an implementation of the profiles of the individual's functional capacity was published by Goes et al.22). The list of all 25 items of the ENCS is available in Appendix A.
The WHOQOL-BREF instrument is a short version of the WHOQOL-100 quality of life assessment tool developed by the WHO26. It comprises 26 questions (two are of general nature and were excluded from this research since they are not linked to the quality of life domains) that measure an individual's quality of life across four domains: physical health (7 questions), psychological health (6 questions), social relationships (3 questions), and environment (8 questions), which incorporates the subjective perception of an individual’s physical and psychological health, social relationships and environment22. The questions ask about an individual's satisfaction with various aspects of their life, such as their physical abilities, emotional state, social support, and living conditions. The responses are rated on a Likert scale ranging from 1 to 5, with higher scores indicating better quality of life. The WHOQOL-BREF is a widely used instrument for assessing the quality of life and has already been translated into Portuguese according to the research work developed by Canavarro et al.27. The list of all 24 items of the WHOQOL-BREF can be found in Appendix B.
The ENCS and WHOQOL-BREF instruments included a header for gathering interviewees’ bio-sociodemographic data, such as age, sex, marital status, and education level.
Data collection took place from January 2016 to April 2017. Health professionals of the LHUBA23 conducted the interviews in the participants’ homes using both instruments simultaneously. The duration of the interviews was 45–60 min, depending on the difficulties presented by the interviewees. The interviewees were also informed that they could withdraw from the research anytime, and all data would be destroyed. The data collected by these two instruments resulted in parallel samples: functional capacity21 and quality of life22 assessments of individuals aged 65 and older.
Data analysis
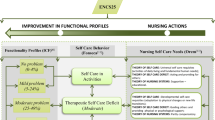
The conceptual model developed to operationalize the measurement of the patient satisfaction indicator (whose result was assigned to the output variable designated as Sat) is depicted in Fig. 1. The diagram shows the relationships that were established between the four dimensions that make up the “Nursing sensitive outcomes” block of the NCPF developed by Dubois et al.16,19 (highlighted by the yellow box on the left side of Fig. 1; see also Fig. 3 in Dubois et al.16, or Fig. 1 in Dubois et al.19), and the assessments of functional capacity (using the ENCS instrument21, whose result was assigned to the output variable designated as Func) and quality of life (using the WHOQOL-BREF instrument22, whose result was assigned to the output variable designated as QoL), with both constructs being represented by the two blue boxes in the central part of Fig. 1.
Subsequently, inferences were made about the association between Func and QoL output variables with the output variable Sat. For this purpose, the following research questions were specified: (1) does the variable Func manifests itself in the variable QoL? (2) Does the variable Sat manifests itself in the variable Func? (3) Does the variable Sat manifests itself in the variable QoL? (4) How far do the weighted scores of the three output variables vary as age increases?
The factorial validity of the models that allowed the previously mentioned research questions to be answered was confirmed by confirmatory factor analysis (CFA) using the lavaan package (version 0.6-11)28 for the R statistics software (version 4.2.0)29. In the lavaan package, the recommended method for estimating model parameters is the diagonally weighted least squares (DWLS) if ordinal data are used. This method was specifically designed when neither the assumption of normality nor the continuity property of the sampling data are considered plausible, in which the diagonal matrix of the final weights is used instead of the full weights matrix30.
The overall quality of fit of the CFA models was based on the following indices, as recommended by Marôco31: (1) \({\chi }^{2}\) statistic with correction for degrees of freedom: \({\chi }^{2}/\left(df\right)\); (2) Comparative Fit Index (CFI); (3) Tucker–Lewis Index (TLI); (4) Standardized Root Mean Square Residual (SRMR); (5) Root Mean Square Error of Approximation (RMSEA); (6) 90% confidence interval for the RMSEA population (RMSEACI(90%)).
Reliability and construct validity of the CFA models were carried out based on the following procedures, as recommended by Marôco31: (1) individual reliability of the reflective items, by verifying whether the standardized factorial loadings \({\lambda }_{ij}\) (referred to as the ith reflective item of jth latent factor) were greater than 0.5 (that is, if \({\lambda }_{ij}\ge 0.5\)); (2) construct reliability (a measure of internal consistency in scale items), by verifying if composite reliability (CR) of each latent factor (\({CR}_{j}\) of the jth latent factor) is greater than 0.7 (that is, if \({CR}_{j}\ge 0.7\)); (3) construct validity, according to the following steps: (3-a) factorial validity, by verifying whether the items were the reflection of the latent factors that were intended to be measured; (3-b) convergent validity, by verifying whether the average variance extracted (AVE) for each latent factor (\({AVE}_{j}\) of the jth latent factor) was greater than 0.5 (that is, if \({AVE}_{j}\ge 0.5\)); (3-c) discriminant validity, by verifying whether the expression \(\left({AVE}_{l} \bigwedge { AVE}_{k}\right)\ge {\phi }_{lk}^{2}\) returns a logical value of TRUE, where \({\phi }_{lk}^{2}\) is the square of the correlation between the latent factors l and k. The factor score weights (fsw), inferred from the respective SEM model, were used as weights to calculate the weighted scores of the output variables Func, QoL, and Sat.
Finally, Spearman’s rank-order correlation (ρ) was the measure of association used to infer how the weighted scores of the three output variables (latent factors) Func, QoL, and Sat vary with the variable Age.
Ethical considerations
The study protocol, design, interview procedures, research methods, and the written informed consent form were approved on July 6, 2014, by the Health Ethics Committee of the Local Health Unit of Baixo Alentejo (HECLHUBA32), with reference number 2/2014. The interviews only began after the respondents expressed their full agreement to participate in the research and freely signed the informed consent form. All the research methods were carried out in full accordance with the guidelines of the Helsinki Declaration33, aiming to protect the dignity, privacy, and freedom of the participants, as stated in the operating regulations of HECLHUBA34.
Ethical approval
Institutional review board This research was conducted in accordance with the Helsinki Declaration and approved by the Institutional Review Board (or Ethics Committee) of HECLHUBA (protocol code 2/2014, approved in February 2014).
Results
The sociodemographic characteristics of the interviewees are listed in Table 1. The age of the respondents ranged from 65 to 101 years, with an average of 78.1 and a standard deviation of 7.86. The sample data collected showed a higher proportion of women than men. Most interviewees were married, and 32.5% were widowed, of whom 76.3% were women and 23.7% were men. Regarding education level, approximately half of the interviewees (\(46.4\%=29.6\%+16.8\%\)) had no formal education, and 29.6% (57.8% women and 42.2% men) were illiterate.
Figure 2 shows the results of the CFAFunc-QoL model, which tests whether the Func latent factor manifests itself in the QoL latent factor, looking to answer the first research question posted in the “Data analysis” section. The 25 instruments items comprising the ENCS25, shown in Fig. 1 (left side), were grouped into five latent factors based on an exploratory factor analysis previously developed according to the research published by Goes et al.21: (1) first group of Selfcare-Activities of daily living (SC-ADL(1)); (2) a second group of Selfcare-Activities of daily living (SC-ADL(2)); (3) Mental functions (MF); (4) Communication (COM); (v) Social Relationships (SR(a)). Regarding the 24 items of the WHOQOL-BREF instrument, they were grouped into four latent factors, namely (see Goes et al.22 for details): (1) Physical Health (Phys); (2) Psychological (Psych); (3) Social Relationships (SR(b)); and (4) Environment (Env).
The CFAFunc-QoL model was developed without any correlation between the errors of the observed variables. The global indices revealed a very acceptable fit: (1) \({\chi }^{2}/\left(df\right)=2.488\) (\(p<0.001\)); (2) CFI = 0.988; (3) TLI = 0.988; (4) SRMS = 0.082; (5) RMSEA = 0.065; and (6) RMSEACI(90%) = [0.062;0.068]. The standardized factor loadings (\({\lambda }_{ij}\)) between the latent factors (represented by ellipses) and the observed variables (represented by small rectangles and identified by the respective code, as specified in Appendices A and B) are presented together with the observed variables for better visualization (all statistically very significant for \(p<0.001\)). A summary analysis of its values shows that the model presented adequate individual reliability of the reflective items (\({\lambda }_{ij}\ge 0.5\) for almost all items and \({\lambda }_{ij}<0.5\) only in three cases, respectively: e355 = 0.44; F3.3 = 0.44; F19.3 = 0.40).
The CFAFunc-QoL model (see Fig. 2) was favorable regarding construct reliability because the latent factors mostly presented CR values greater than 0.7 (SC-ADL(1) = 0.97; SC-ADL(2) = 0.95; MF = 0.94; COM = 0.97; SR(a) = 0.75; Phys = 0.91; Psych = 0.90; Env = 0.82; Func = 0.92; QoL = 0.94), except for SR(b), whose value was 0.66 (according to Hair et al.35, values between 0.5 and 0.7 may be considered “acceptable” in the case of experimental studies). All the observed variables reflect the measured latent factor, so the model presented adequate factorial validity. Regarding convergent validity, only the SC-ADL(1), SC-ADL(2), and Env latent factors reported AVE values lower than 0.50, namely 0.39, 0.39, and 0.30, respectively, as shown in Table 2 (according to Hair et al.35, AVE values between 0.5 and 0.3 may be considered “acceptable” in experimental studies, as is the case of the present research). Finally, on checking the logical value of TRUE for the expression \(\left({AVE}_{i} \bigwedge { AVE}_{j}\right)\ge {\phi }_{ij}^{2}\), where \({\phi }_{ij}^{2}\) is the square of the correlation between the latent factors i and j, the model failed regarding discriminant validity (see Table 2).
Results of the CFAFunc-QoL model also seem to suggest that the functional capacity was significantly manifested in the interviewees’ quality of life, with strong explanatory power because the value of the standardized regression coefficient (β) was − 0.791 (\(p<0.001\)). It should be noted that the negative value of the coefficient is because the items of ENCS and WHOQOL-BREF instruments have their response scales inverted. Given that \(\beta =-0.791\) (a value qualitatively classified as “strong”) and that \({\left(-0.791\right)}^{2}=0.626\), then the Func latent factor explained 62.6% of the variance that occurs in the QoL latent factor.
Figure 3 shows the CFAFunc-QoL-Sat model that tests whether the Sat latent factor manifests itself in the Func and QoL latent factors, looking to answer the second and third research questions posted in the “Data analysis” section. It was also developed without any correlation between the errors of the observed variables. The model presented an acceptable global fit since \({\chi }^{2}/\left(df\right)=2.456\) (\(p<0.001\)). It also showed adequate individual reliability of the items because the factor loadings \({\lambda }_{ij}\) were mostly greater than 0.5 (only 18.4% were less than 0.5), and none were less than 0.3. The latter threshold of 0.3 is considered acceptable for exploratory studies35.
The CFAFunc-QoL-Sat model (see Fig. 3) showed composite reliability, with CR values consistently higher than 0.7, except for the SR(a) and SR(b) latent factors, which had values of 0.57 and 0.59, respectively. Concerning construct validity, the model presented adequate factorial validity because, like the previous model (see Fig. 2), the items seem to reflect the latent factors to be measured. Regarding convergent validity, the AVE values were higher than 0.5, except again for the SR(a), SR(b), and Env latent factors, with values of 0.21 (low value even for experimental studies35), 0.33, and 0.31, respectively (acceptable values in case of experimental studies35). On checking the logical value of TRUE for the expression \(\left({AVE}_{i} \bigwedge { AVE}_{j}\right)\ge {\phi }_{ij}^{2}\), the model failed concerning discriminant validity (see Table 3).
As shown in Fig. 3, the Sat latent factor manifests itself very significantly in the Func latent factor, with strong explanatory power because the standardized value of the regression coefficient was \(\beta =-0.77\) (\(p<0.001\)). Moreover, the Sat latent factor manifests itself very significantly in the latent factor QoL, with strong explanatory power, because the standardized value of the regression coefficient was \(\beta =0.89\) (\(p<0.001\)). Given that the values of the standardized beta coefficients are − 0.77 and 0.89 and that \({\left(-0.77\right)}^{2}=0.593\) and \({0.89}^{2}=0.792\), the Sat latent factor explained 59.3% and 79.2%, respectively, of the variance that occurs in the Func and QoL latent factors.
In short, results of the CFAFunc-QoL-Sat model seem to suggest that the most significant predictor of the Sat latent factor was the QoL latent factor (\(\beta =0.89;p<0.001\)), followed by the Func latent factor (\(\beta =-0.77;p<0.001\)).
From the CFAFunc-QoL-Sat model, it was possible to infer the values of the factor score weights (fsw), which enabled the calculation of the weighted scores of each of the three latent factors considered in this research, Func, QoL, and Sat. To do this, the formulation presented in Table 4 was used, which was based on the individuals’ responses to the instruments’ items and the fsw values (used as weights, with all being normalized to 1).
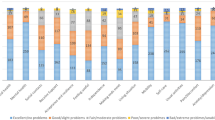
The graph in Fig. 4 shows the average sample scores for the Func, QoL, and Sat latent factors: (1) unweighted averages (AVG—black bars), calculated using the formulation proposed by Goes et al.21,22; (2) weighted averages (AVG(fsw)—light gray bars), calculated employing the formulation presented in Table 4, whose weights are the fsw values inferred from the CFA model depicted in Fig. 3 normalized to 1. The remaining values are MaxDiff (+) and MaxDiff (−), that is, the maximum positive difference and the maximum negative difference found throughout the 351 elements of the sample, using the expression AVG − AVG(fsw) (dark gray bars). For the latent factor Sat, the score was calculated only using the formulation shown in Table 4, as there is no reference for its calculation in the research developed by Dubois et al.16,19.
Average Func, QoL, and Sat latent factors scores, on a scale of 0–100%, using unit weights (black bars) versus employing the formulation listed in Table 4 (light gray bars). The values indicated by the dark gray bars correspond to the maximum individual differences (either positive or negative) found throughout all 351 elements of the sample.
Finally, it was also tested how the scores of the three latent factors, weighted by the fsw values, varied with age, using the measure of association Spearman’s rank order correlation (ρ), looking to answer the fourth research question posted in the “Data analysis” section. The results showed the following: (1) \({\rho }_{{\varvec{F}}{\varvec{u}}{\varvec{n}}{\varvec{c}}}=0.434\) (moderate association); (2) \({\rho }_{{\varvec{Q}}{\varvec{o}}{\varvec{L}}}=-0.289\) (weak association); (3) \({\rho }_{{\varvec{S}}{\varvec{a}}{\varvec{t}}}=-0.320\) (weak association), all statistically highly significant (\(p<0.001\)). A brief analysis of the ρ values showed that the Func latent factor presented the highest association with variable age, whose result (\({\rho }_{{\varvec{F}}{\varvec{u}}{\varvec{n}}{\varvec{c}}}=0.434\)) suggests that as age increases, the likelihood of obtaining a more severe functional profile seems to increase (a finding that is consistent with the previous research conducted by Goes et al.21, when this latent factor was considered individually). Secondly, in decreasing order, a lower association occurred for the Sat latent factor (\({\rho }_{{\varvec{S}}{\varvec{a}}{\varvec{t}}}=-0.320\)), which suggests that as age increases, satisfaction with nursing care received by the interviewees seems to decrease. Finally, the third and lowest association occurred for the QoL latent factor (\({\rho }_{{\varvec{Q}}{\varvec{o}}{\varvec{L}}}=-0.289\)), which suggests that as age increases, individuals aged 65 and older seem to realize their quality of life more negatively (a finding that is also consistent with the previous research conducted by Goes et al.36, when this latent factor was considered individually).
Discussion
This research proposes operationalizing the patient satisfaction indicator with nursing care provided to people aged 65 and older residing in the community, following the theoretical framework developed by Dubois et al. concerning the third subsystem of their NCPF, aimed at “the production of outcomes that lead to positive changes in a patient’s functional status, disease state, or evolving condition as the desired end result of the interactions between patients, nursing staff, and nursing processes”16,19. Rather than capturing the interviewees' perceptions of the nursing care they received and their overall satisfaction with the health care experience through an assessment based on a single instrument explicitly developed for this purpose, the proposed model was based on the assessments of their functional capacity21 and quality of life22, considered by several researchers to be priority outcome indicators sensitive to nursing care14,17,18,19. Nevertheless, the innovative nature of this research makes the comparison of the findings with those developed by other researchers somehow challenging due to the limited number of published research on the topic.
The two CFA models developed in this research performed well concerning the quality of fit, reliability, and construct validity (factorial and convergent validity). However, both failed in discriminant validity between latent factors, suggesting that functional capacity, quality of life, and patient satisfaction were latent factors that were found to be somewhat correlated, which is expected to some extent considering the type of constructs evaluated21,22,37.
The CFAFunc-QoL model developed within this research allowed simultaneously relating the interviewees’ functional capacity with their quality of life, using the ENCS21 and the WHOQOL-BREF22 instruments. With this model, it was possible to map the objective assessment of functional capacity into the subjective assessment of the interviewees’ quality of life. The findings seem to suggest a statistically significant empirical relationship between functional capacity and quality of life outcome indicators. They also suggest that when defining the nursing care needs according to the different levels of functional capacity based on a self-care model following the work developed by Goes et al.21, the respective nursing care provided seems to manifest markedly in the interviewees’ quality of life because the Func latent factor explains a significant portion of the variance that occurs in the QoL latent factor. In other words, by attempting to reduce the functional problems of the interviewees with nursing interventions, thus decreasing the score resulting from their functional capacity assessment, the nursing care provided also seems to lead to an increase in their quality of life scores. These findings make sense in theoretical terms and are aligned with those published by some researchers. As individuals age, they may experience declines in physical and cognitive abilities that can limit their ability to perform daily activities and participate in social events38,39. Some scientific evidence has shown that nursing care can help older adults maintain or regain their independence by assisting them with daily living activities, managing chronic health conditions (especially in individuals suffering from multimorbidity), and promoting overall health and well-being40,41,42. There is robust scientific evidence showing that nursing care contributes to improving functional capacity, helping older adults to remain active and engaged, and allowing them to live more autonomously with fewer dependencies, resulting in better physical and mental health and quality of life outcomes40,41,42,43,44,45.
The CFAFunc-QoL-Sat model developed within this research allowed relating functional capacity, quality of life, and satisfaction with nursing care provided to older adults residing in the community. The findings seem to suggest that both the functional capacity and the quality of life of the interviewees are determinants of satisfaction with the nursing care experience since the correlations obtained between the Func and QoL latent factors with the Sat latent factor were found to be statistically very significant. However, patient satisfaction with such care seems to have a more significant impact on the assessment of quality of life than the assessment of functional capacity due to a more significant proportion of the variance explained by the CFAFunc-QoL-Sat model regarding the former latent factor. Given that the CFAFunc-QoL-Sat model captured what was most similar among the three latent factors, the results suggest that patient satisfaction with the nursing care provided to them seems to be more related to their needs, standards, and expectations (obtained during their quality of life assessment) and not so much with the objective evaluation performed by health professionals (obtained during their functional capacity assessment). Several research studies proclaim that patient satisfaction is crucial in assessing the quality of nursing care, providing valuable insights into how patients perceive their care experiences12,16,17,18,19,20. Moreover, older adults who are satisfied with their nursing care, whose assessment is considered subjective by researchers15,16,19,20, seem to experience an increased quality of life22,36,44,46, which also results in a subjective assessment aiming at capturing older adults’ perception of their health, hopes, expectations, and feelings after the delivery of nursing care22,44,46, suggesting that one subjective assessment (patient satisfaction) seems to be more related to another subjective assessment (quality of life), compared to a non-subjective one (functional capacity). Finally, some researchers also report that when older adults feel that their nursing care needs are being met, they appear to feel more comfortable and secure, improving both physical and psychological well-being14,15,20,22,46, which seems to be aligned with the findings reported here, through the analyses of the standardized regression coefficients, namely: a decrease in the functional capacity assessment score (empowerment of interviewees' functional capacity), simultaneously seems to increase the quality of life assessment score, yielding a positive effect on patient satisfaction with nursing care provided to them.
Concerning the measures of association found between the scores of Func, QoL, and Sat latent factors with the variable Age, the results seem to suggest the following interpretations. With regard to the effect that the scores of these factors exhibit, the strongest was assigned to the Func latent factor when compared to QoL and Sat latent factors, suggesting that as age increases, the likelihood of older adults presenting functional problems of greater complexity seems to increase, leading to a greater need for nursing care, a finding that was already reported by Goes et al.21. As people get older, they may experience a range of physical and cognitive changes that can affect their ability to perform daily living activities, such as dressing, cooking, cleaning, and driving21,38,39. This decline in functional capacity can be due to various factors, including natural age-related changes in the body, the development of chronic health conditions, and environmental factors, such as living conditions and access to health care38,39. Thus, the association type between functional capacity and age reported in this research is aligned with that was found by other researchers, as they also reported significant evidence of functional decline or loss of independence as people age12,38,39,47. Regarding the measure of association between the score of QoL latent factor and the variable Age, the result suggests that as age increases, the quality of life of the interviewees seems to decrease, which is also expected and stated by some researchers, mainly due to due to health problems, financial difficulties, or social isolation12,13,14,22,36,44. However, it is important to mention that some older adults may experience an improved quality of life as they age, mainly if they can maintain their physical health through regular exercise, a healthy diet, and managing chronic health conditions properly, which is also reported in some scientific literature on the topic47,48. Finally, concerning the association between the score of Sat latent factor and the variable Age, the result suggests that as age increases, the satisfaction with the nursing care delivered to the interviewees seems to decrease. However, this relationship is expected because older adults will tend to be less satisfied with the impact that the worsening of functional problems may have on their quality of life, a finding that is also corroborated by other researchers12,14,22,38,44.
Regarding the mean scores obtained for the sample, those based on the fsw values inferred from the CFAFunc-QoL-Sat model, results seem to suggest that the interviewees are somewhat satisfied with the nursing care provided to them (average score greater than 50%), which seems to be revealing of the positive effect that such care had on their health condition. This finding reinforces the importance of providing the best possible nursing care to a patient and/or caregiver (family or friends) that effectively improves their level of rehabilitation, readaptation, and reintegration49,50, preferably in their homes, as the sample comprised individuals aged 65 and older residing in the community12,13,21,38,40. Nursing care planning based on functional capacity, quality of life, and patient satisfaction indicators seems to become more coherent with the real nursing care needs of individuals, as it makes it possible to encode a wide range of information about the patient, from which it will be possible to decide on the most appropriate nursing interventions and nursing resources to be made available11,16,18,19,20.
In summary, taking into account the strong associations found in this research between the Func, QoL, and Sat latent factors, the extreme relevance of the provision of nursing care to the studied population group emerges, as such care is a promoter of positive changes in their functional condition21,38,42,45 and their quality of life22,44,51, especially as age advances. In this context, the need for a person-centered nursing care setting is highlighted, as has been discussed by several researchers, ensuring the integrity and continuity of that care, making it more comprehensive and capable of effectively responding to the real needs of older adults, whose multimorbidity is more prevalent throughout their life cycle10,11,12,46,49. Measuring patient satisfaction, involving standardized assessments of functional capacity and quality of life, as a nursing-sensitive outcome indicator, provides a person-reported assessment that allows a deep understanding of that person's life, values, priorities, and preferences, all important for better management of their health condition18,19,20,52.
Conclusions
Patient satisfaction seems to be a significant indicator for health care quality assessment. It is sensitive to nursing care, according to the theoretical model developed by the authors that conceived the NCPF. It is also considered in several models to be both an outcome of nursing services and a primary determinant of the overall satisfaction with the care experience. The models developed in this research and the resulting findings suggest that patient satisfaction indicator should be used to evaluate the contribution of the nursing profession as a reference and surplus value for the sustainability of health systems since the care provided can effectively produce changes in patients’ conditions with multimorbidity. Finally, both the functional capacity and quality of life assessments seem to be very significant predictors of patient satisfaction with nursing care.
The major limitation of this research is related to the fact that this was not a longitudinal study, so it was not possible to perform a long-term follow-up assessment, which might identify some cause-effect relationship between the delivery of nursing care and their effects on interviewees’ health condition.
Data availability
All data and materials in this research can be obtained by contacting the corresponding author: Henrique Oliveira (hjmo@lx.it.pt).
References
OECD. Pensions at a Glance 2021: OECD and G20 Indicators (OECD Publishing, 2021). https://doi.org/10.1787/ca401ebd-en.
EUROSTAT. Healthy life years statistics. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Healthy_life_years_statistics (2019). Accessed 7 Apr 2023.
PORDATA. Life expectancy at birth by sex. https://www.pordata.pt/en/DB/Europe/Search+Environment/Chart/5827551 (2022). Accessed 7 Apr 2023.
PORDATA. Healthy life years at birth by sex. https://www.pordata.pt/en/DB/Europe/Search+Environment/Chart/5827552 (2022). Accessed 7 Apr 2023.
PORDATA. Life expectancy at 65 by sex. https://www.pordata.pt/en/DB/Europe/Search+Environment/Chart/5827553 (2022). Accessed 7 Apr 2023.
PORDATA. Healthy life years at 65 by sex. https://www.pordata.pt/en/DB/Europe/Search+Environment/Chart/5827554 (2022). Accessed 7 Apr 2023.
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9 (2020).
World Health Organization. Regional Office for Europe and European Observatory on Health Systems Policies. Health system review: Portugal: phase 1 final report (World Health Organization. Regional Office for Europe, Copenhagen), https://apps.who.int/iris/handle/10665/345635 (2018). Accessed 7 Apr 2023.
Rodrigues, A. M. et al. Challenges of ageing in Portugal: Data from the EpiDoC Cohort. Acta Med. Port. https://doi.org/10.20344/amp.9817 (2016).
van der Heide, I. et al. Patient-centeredness of integrated care programs for people with multimorbidity. Results from the European ICARE4EU project. Health Policy 122, 36–43. https://doi.org/10.1016/j.healthpol.2017.10.005 (2018).
American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. Patient-centered care for older adults with multiple chronic conditions: A Stepwise Approach from the American Geriatrics Society. J. Am. Geriatr. Society. 60, 1957–1968. https://doi.org/10.1111/j.1532-5415.2012.04187.x (2012).
Kuluski, K. et al. What is important to older people with multimorbidity and their caregivers? Identifying attributes of person centered care from the user perspective. Int. J. Integr. Care. https://doi.org/10.5334/ijic.4655 (2019).
Lopes, M. Desafios de Inovação em Saúde: Repensar os Modelos de Cuidados (Imprensa da Universidade de Évora, 2021). https://imprensa.uevora.pt/uevora/catalog/book/24. Accessed 3 Mar 2023.
Karaca, A. & Durna, Z. Patient satisfaction with the quality of nursing care. Nurs. Open 6, 535–545. https://doi.org/10.1002/nop2.237 (2019).
Larson, E., Sharma, J., Bohren, M. A. & Tunçalp, Ö. When the patient is the expert: Measuring patient experience and satisfaction with care. Bull. World Health Organ. 97, 563–569. https://doi.org/10.2471/blt.18.225201 (2019).
Dubois, C.-A., D’Amour, D., Pomey, M.-P., Girard, F. & Brault, I. Conceptualizing performance of nursing care as a prerequisite for better measurement: A systematic and interpretive review. BMC Nurs. 12, 7. https://doi.org/10.1186/1472-6955-12-7 (2013).
Oner, B. et al. Nursing-sensitive indicators for nursing care: A systematic review (1997–2017). Nurs. Open 8, 1005–1022. https://doi.org/10.1002/nop2.654 (2020).
Afaneh, T., Abu-Moghli, F. & Ahmad, M. Nursing-sensitive indicators: A concept analysis. Nurs. Manage. 28, 28–33. https://doi.org/10.7748/nm.2021.e1982 (2021).
Dubois, C.-A. et al. Which priority indicators to use to evaluate nursing care performance? A discussion paper. J. Adv. Nurs. 73, 3154–3167. https://doi.org/10.1111/jan.13373 (2017).
Rapin, J., D’Amour, D. & Dubois, C.-A. Indicators for evaluating the performance and quality of care of ambulatory care nurses. Nutr. Res. Pract. https://doi.org/10.1155/2015/861239 (2015).
Goes, M., Lopes, M. J., Oliveira, H., Fonseca, C. & Marôco, J. A nursing care intervention model for elderly people to ascertain general profiles of functionality and self care needs. Sci. Rep. 10, 1770. https://doi.org/10.1038/s41598-020-58596-1 (2020).
Goes, M., Lopes, M., Marôco, J., Oliveira, H. & Fonseca, C. Psychometric properties of the WHOQOL-BREF(PT) in a sample of elderly citizens. Health Qual. Life Outcomes 19, 146. https://doi.org/10.1186/s12955-021-01783-z (2021).
LHUBA. Local Health Unit of Baixo Alentejo (Unidade Local de Saúde do Baixo Alentejo). http://www.ulsba.min-saude.pt/2019/02/28/comissao-de-etica-para-a-saude/ (2022). Accessed 17 Apr 2023.
Fonseca, C. Modelo de autocuidado para pessoas com 65 e mais anos de idade, necessidades de cuidados de enfermagem Ph.D. thesis, Universidade de Lisboa. https://repositorio.ul.pt/handle/10451/12196 (2014). Accessed 16 Mar 2023.
World Health Organization. International Classification of Functioning, Disability and Health (ICF). https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health (2022). Accessed 14 Mar 2023.
World Health Organization. WHOQOL: Measuring Quality of Life. https://www.who.int/tools/whoqol/whoqol-bref (2022). Accessed 14 Mar 2023.
Canavarro, M. et al. WHOQOL-Bref (Versão em Português de Portugal do Instrumento Abreviado de Avaliação da Qualidade de Vida da Organização Mundial de Saúde). http://www.fpce.uc.pt/saude/WHOQOL_Bref.html (2010). Accessed 14 Mar 2023.
Rosseel, Y. lavaan: An R package for structural equation modeling. J. Stat. Softw. 48(2), 1–36. https://doi.org/10.18637/jss.v048.i02 (2012).
R Core Team. The R Project for Statistical Computing. https://www.r-project.org/ (2022). Accessed 3 Mar 2023.
Rosseel, Y. The Lavaan tutorial: Categorical data. https://lavaan.ugent.be/tutorial/cat.html (2022). Accessed 3 Mar 2023.
Marôco, J. Análise de Equações Estruturais: Fundamentos teóricos, Software e Aplicações (Report Number 2021).
HECLHUBA. The LHUBA’s health ethics committee. http://www.ulsba.min-saude.pt/2019/02/28/comissao-de-etica-para-a-saude/ (2022). Accessed 17 Apr 2023.
HECLHUBA. Helsinki declaration (Portuguese version). http://www.ulsba.min-saude.pt/wp-content/uploads/sites/15/2019/02/declaracaohelsinquia.pdf (2022). Accessed 17 Apr 2023.
HECLHUBA. The health ethics committee of LHUBA. http://www.ulsba.min-saude.pt/wp-content/uploads/sites/15/2019/02/Documento-Guia.pdf (2022). Accessed 17 Apr 2023.
Hair, J.; Anderson, R.; Tatham, R.; Black, W. Multivariate Data Analysis; Pearson Education Limited: 2009; p. 739. https://www.amazon.com/Multivariate-Data-Analysis-Joseph-Hair/dp/0138132631. Accessed 7 Apr 2023.
Goes, M., Lopes, M. J., Oliveira, H., Fonseca, C. & Mendes, D. Biological and socio-demographic predictors of elderly quality of life living in the community in Baixo-Alentejo, Portugal. in Gerontechnology Communications in Computer and Information Science (eds García-Alonso, J., Fonseca, C.) Chapter 28, 319–326. https://doi.org/10.1007/978-3-030-16028-9_28 (Springer Cham 2019).
Osborne, J. Best Practices in Exploratory Factor Analysis (CreateSpace Independent Publishing Platform, 2014).
Martín Lesende, I. et al. Functional decline and associated factors in patients with multimorbidity at 8 months of follow-up in primary care: The functionality in pluripathological patients (FUNCIPLUR) longitudinal descriptive study. BMJ Open https://doi.org/10.1136/bmjopen-2018-022377 (2018).
Franceschi, C. et al. The continuum of aging and age-related diseases: Common mechanisms but different rates. Front. Med. https://doi.org/10.3389/fmed.2018.00061 (2018).
Pho, A. T. et al. Nursing strategies for promoting and maintaining function among community-living older adults: The CAPABLE intervention. Geriatr. Nurs. 33, 439–445. https://doi.org/10.1016/j.gerinurse.2012.04.002 (2012).
Pfeifer, L. O., Helal, L., Oliveira, N. L. & Umpierre, D. Correlates of functional physical capacity in physically active older adults: A conceptual-framework-based cross-sectional analysis of social determinants of health and clinical parameters. Aging Clin. Exp. Res. 35, 127–136. https://doi.org/10.1007/s40520-022-02274-x (2022).
Verstraten, C. C. J. M. M., Metzelthin, S. F., Schoonhoven, L., Schuurmans, M. J. & Man-van Ginkel, J. M. Optimizing patients’ functional status during daily nursing care interventions: A systematic review. Res. Nursing Health. 43, 478–488. https://doi.org/10.1002/nur.22063 (2020).
Miller, J. M., Sabol, V. K. & Pastva, A. M. Promoting older adult physical activity throughout care transitions using an interprofessional approach. J. Nurse Practitioners. 13, 64-71.e62. https://doi.org/10.1016/j.nurpra.2016.08.006 (2017).
Khodadad Kashi, S., Mirzazadeh, Z. S. & Saatchian, V. A systematic review and meta-analysis of resistance training on quality of life, depression, muscle strength, and functional exercise capacity in older adults aged 60 years or more. Biol. Res. Nursing. 25, 88–106. https://doi.org/10.1177/10998004221120945 (2022).
Forman, D. E. et al. Prioritizing functional capacity as a principal end point for therapies oriented to older adults with cardiovascular disease: A scientific statement for healthcare professionals from the American Heart Association. Circulation https://doi.org/10.1161/cir.0000000000000483 (2017).
Kuipers, S. J., Cramm, J. M. & Nieboer, A. P. The importance of patient-centered care and co-creation of care for satisfaction with care and physical and social well-being of patients with multi-morbidity in the primary care setting. BMC Health Services Res. https://doi.org/10.1186/s12913-018-3818-y (2019).
Jeste, D. V. et al. Association between older age and more successful aging: Critical role of resilience and depression. Am. J. Psychiatry. 170, 188–196. https://doi.org/10.1176/appi.ajp.2012.12030386 (2013).
Masi, C. M., Chen, H.-Y., Hawkley, L. C. & Cacioppo, J. T. A meta-analysis of interventions to reduce loneliness. Personality Social Psychol. Rev. 15, 219–266. https://doi.org/10.1177/1088868310377394 (2010).
Edvardsson, D., Watt, E. & Pearce, F. Patient experiences of caring and person-centredness are associated with perceived nursing care quality. J. Adv. Nursing. 73, 217–227. https://doi.org/10.1111/jan.13105 (2017).
Lukewich, J. A., Tranmer, J. E., Kirkland, M. C. & Walsh, A. J. Exploring the utility of the Nursing Role Effectiveness Model in evaluating nursing contributions in primary health care: A scoping review. Nurs. Open 6, 685–697. https://doi.org/10.1002/nop2.281 (2019).
Pequeno, N. P. F., Cabral, N. L. A., Marchioni, D. M., Lima, S. C. V. C. & Lyra, C. O. Quality of life assessment instruments for adults: A systematic review of population-based studies. Health Qual. Life Outcomes. https://doi.org/10.1186/s12955-020-01347-7 (2020).
Porter, M. E., Larsson, S. & Lee, T. H. Standardizing patient outcomes measurement. N. Engl. J. Med. 374, 504–506. https://doi.org/10.1056/NEJMp1511701 (2016).
Acknowledgements
The authors acknowledge the support received from all the health professionals who contributed to data acquisition, especially those who conducted the interviews with the individuals in the sample, as well as the professional support received from the primary health care teams of ULSBA (http://www.ulsba.min-saude.pt/). This research was funded by FEDER. Programa Interreg VA España-Portugal (POCTEP), Instituto Internacional de Investigação e Inovação em Envelhecimento–Capitaliza. “0786_CAP4ie_4_P”.
Author information
Authors and Affiliations
Contributions
M.G. and H.O. conceived the research under the supervision of M.L. C.F. contributed to the conception of the ENCS under the supervision of M.L. H.O. conceived the statistical analyses for all data. L.P. and M.M. contributed to the systematic review. All authors drafted and revised the manuscript for important intellectual content. M.G. and H.O. had full access to the data and assumed responsibility for its integrity. H.O. is the guarantor of all data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A
List of ENCS items21.
Selfcare-Activities of daily living—1 (8)
-
d230 Carrying out daily routine
-
d410 Changing basic body position
-
d415 Maintaining body position
-
d450 Walking
-
d465 Moving around using equipment
-
d510 Washing oneself
-
d520 Caring for body parts
-
d540 Dressing
Selfcare-Activities of daily living—2 (3)
-
d530 Toileting
-
d550 Eating
-
d560 Drinking
Mental functions (6)
-
b110 Consciousness functions
-
b114 Orientation functions
-
b140 Attention functions
-
b144 Memory functions
-
b152 Emotional functions
-
b164 Higher-level cognitive functions
Communication (3)
-
d310 Communicating with—receiving—spoken messages
-
d330 Speaking
-
d350 Conversation
Environment factors (4)
-
d760 Family relationships
-
e310 Immediate family
-
e320 Friends
-
e340 Personal care providers and personal assistants
-
e355 Health professionals
Appendix B
List of WHOQOL‑BREF items/facets22.
Physical Health domain
-
F1.4 Pain and discomfort
-
F2.1 Energy and fatigue
-
F3.3 Sleep and rest
-
F9.1 Mobility
-
F10.3 Activities of daily living
-
F11.3 Dependence on medication or health care
-
F12.4 Work capacity
Psychological domain
-
F4.1 Positive feelings
-
F5.3 Thinking, learning, memory and concentration
-
F6.3 Self-esteem
-
F7.1 Body image and appearance
-
F8.1 Negative feelings
-
F24.2 Spirituality/religion and personal beliefs
Social relationships domain
-
F13.3 Personal relations
-
F14.4 Practical social support
-
F15.3 Sex
Environment domain
-
F16.1 Physical safety and security
-
F17.3 Home environment
-
F18.1 Financial resources
-
F19.3 Health and social care: availability and quality
-
F20.1 Opportunities to acquire new information and skills
-
F21.1 Recreation and leisure
-
F22.1 Physical environment (pollution/noise/traffic/climate)
-
F23.3 Transport
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goes, M., Oliveira, H., Lopes, M. et al. A nursing care-sensitive patient satisfaction measure in older patients. Sci Rep 13, 7607 (2023). https://doi.org/10.1038/s41598-023-33805-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-33805-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.