Abstract
Many health authorities differentiate hospitalizations in patients infected with SARS-CoV-2 as being “for COVID-19” (due to direct manifestations of SARS-CoV-2 infection) versus being an “incidental” finding in someone admitted for an unrelated condition. We conducted a retrospective cohort study of all SARS-CoV-2 infected patients hospitalized via 47 Canadian emergency departments, March 2020-July 2022 to determine whether hospitalizations with “incidental” SARS-CoV-2 infection are less of a burden to patients and the healthcare system. Using a priori standardized definitions applied to hospital discharge diagnoses in 14,290 patients, we characterized COVID-19 as (i) the “Direct” cause for the hospitalization (70%), (ii) a potential “Contributing” factor for the hospitalization (4%), or (iii) an “Incidental” finding that did not influence the need for admission (26%). The proportion of incidental SARS-CoV-2 infections rose from 10% in Wave 1 to 41% during the Omicron wave. Patients with COVID-19 as the direct cause of hospitalization exhibited significantly longer LOS (mean 13.8 versus 12.1 days), were more likely to require critical care (22% versus 11%), receive COVID-19-specific therapies (55% versus 19%), and die (17% versus 9%) compared to patients with Incidental SARS-CoV-2 infections. However, patients hospitalized with incidental SARS-CoV-2 infection still exhibited substantial morbidity/mortality and hospital resource use.
Similar content being viewed by others
Introduction
The number of patients hospitalized with SARS-CoV-2 infection remains high in this third year of the pandemic. Our understanding of the impact of these hospitalizations on the healthcare system has been clouded by debate about whether we should include only those hospitalizations that are “for COVID-19” (i.e., direct manifestations of SARS-CoV-2 infection) or also those admitted for an unrelated condition and incidentally found to have SARS-CoV-2 infection1,2,3,4.
There is no standardized definition, however, to determine which hospitalized patients infected with SARS-CoV-2 were admitted “for COVID-19” and which have an incidental infection. In Canada and the United Kingdom, hospitals use ad hoc categorizations created by local infection prevention and control teams to classify admissions, with variability between institutions on whether provision of COVID-specific therapies such as remdesivir or tocilizumab are included in these definitions5,6. In the United States, the Centers for Disease Control defines a hospitalization as being “for COVID-19” if ICD-10 code U07.1 was (i) the primary discharge diagnosis or (ii) a secondary diagnosis and the patient was treated with remdesivir or had a primary diagnosis of sepsis, pulmonary embolism, acute respiratory failure, or pneumonia7. On the other hand, some US States only define hospitalizations as being “for COVID-19” if COVID-19 was the primary or secondary diagnosis and dexamethasone was prescribed8. However, a recent study of electronic health records (EHR) from 4 US health care systems found that EHR phenotypes that include discharge diagnosis codes were the best means to classify the cause of admissions, as laboratory tests or treatments for patients with COVID-19 were not standardized across systems or even across hospitals within the same system9. Without a standard definition that accurately differentiates the truly “incidental” infection (an asymptomatic patient not requiring treatment) from all other SARS-CoV-2 positive patients, the healthcare needs of some hospitalized patients will be misjudged, leading to poor future resource allocation and contributing to system-wide capacity breakdowns.
In this study, we describe the proportion of patients with SARS-CoV-2 infection hospitalized during the various pandemic waves in Canada in whom COVID-19 was adjudged (using a priori standardized definitions derived by consensus of clinicians in emergency medicine, infectious diseases, and general internal medicine and based on hospital discharge diagnoses) to be (i) the Direct cause for the admission, versus (ii) a potential Contributing factor for the admission, versus (iii) an Incidental finding, as well as their resource use and outcomes.
Methods
Study design, setting, participants, and data sources
As described in full elsewhere10 and on our website (www.ccedrrn.com) data for the Canadian COVID-19 Emergency Department Rapid Response Network (CCEDRRN) population-based registry were retrospectively collected via manual chart review from 47 emergency departments (EDs), encompassing a mix of academic and community-based EDs, located in 6 provinces across Canada. We included all patients hospitalized between March 1/20 and July 24/22 who had confirmed SARS-CoV-2 infection using a nucleic acid amplification test or rapid antigen test in the 14 days prior to or during their index ED visit, or in the first 5 days after hospitalization, confirmed positive at a healthcare facility. Thus, our focus was on patients admitted with SARS-CoV-2 infection rather than nosocomially acquired infections. Trained research assistants at each site collected information on baseline characteristics, hospital course, treatments, and outcomes within 30 days. For patients with multiple hospitalizations and/or positive tests during the study period, we included only their first hospitalization related to a positive test within 14 days. As described below, we used a priori standardized definitions to classify the cause of hospitalization on the basis of the hospital (not ED) discharge diagnoses.
Variable definitions
Prior work from our group demonstrated that it is challenging to accurately dichotomize hospitalizations into only 2 groups (those that are “for COVID-19” versus “with incidental infection”) using discharge diagnoses data11. As the data collected in the study case report forms included the most responsible diagnosis at the time of discharge and up to 10 secondary diagnoses but not the background rationale, symptom timelines, or supporting notes, we chose to instead classify hospitalizations into one of 3 categories (adapted from the Centres for Disease Control classification system and based on definitions established by expert consensus of the ED physicians and hospital internists in the CCEDRRN)7. We used the most responsible diagnosis assigned at hospital discharge to classify each hospitalization in a patient with SARS-CoV-2 infection at the time of admission as:
-
1.
COVID-19 is the direct cause of admission (herewith referred to as the “Direct” group) if the Most Responsible Diagnosis at discharge was any of the following: COVID-19, upper respiratory tract infection, pneumonia, viral pneumonia, sinusitis, pharyngitis, bronchitis, flu-like illness, Adult Respiratory Distress Syndrome, respiratory failure, or sepsis.
-
2.
COVID-19 is a potential contributing factor for the hospitalization (herewith referred to as the “Contributing” group) if the Most Responsible Diagnosis at discharge was:
-
thromboembolic phenomena (including acute coronary syndrome, ischemic stroke, transient ischemic attack, other arterial clot, pulmonary embolism, or deep venous thrombosis),
-
acute kidney injury,
-
electrolyte abnormalities (hypo- or hypernatremia, hypo- or hyperkalemia, hypo- or hypercalcemia, hypo- or hypermagnesemia)
-
exacerbations of heart failure, asthma, COPD, or Multiple Sclerosis
-
Delirium, Confusion, Altered level of consciousness
-
Diabetic ketoacidosis
-
Syncope or falls,
-
Acute functional decline,
-
Rhabdomyolysis,
-
Mental health issues (anxiety, depression)
-
Overdose/suicide attempt
-
Chest pain or angina (stable or unstable), or ischemic heart disease
-
-
3.
SARS-CoV-2 infection is an incidental finding if the Most Responsible Diagnosis at discharge was anything other than those listed under 1 or 2 above (herewith referred to as the “Incidental” group). Note that this is not synonymous with the patient being asymptomatic.
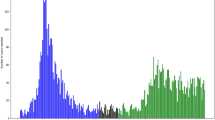
We defined the Canadian pandemic waves as: Mar 1/20–June 30/20 (wave 1), July 1/20–Feb 14/21 (wave 2), Feb 15/21–Jul 14/21 (wave 3, driven largely by the spread of the alpha variant across Canada), July 15/21–Nov 27/21 (wave 4, driven largely by the spread of the delta variant across Canada), and Nov 28/21 onwards (wave 5, beginning when the first case of omicron was reported in Canada).
Statistical analyses
Summary statistics (e.g., mean, standard deviation [SD], median, interquartile range, count, percent) describe the patient characteristics, acute care utilization, and outcomes. Differences among hospitalization groups were assessed by chi-square tests and analysis of variance. To ensure patient privacy, a cell size restriction policy prohibited us from reporting counts of less than six. A p-value < 0.05 was considered statistically significant. All analyses were performed in Stata (Version 16.1, StataCorp, College Station, Texas).
Ethics approval
The University of British Columbia (UBC) Clinical Research Ethics Board reviewed and approved the full study protocol with a waiver for individual patient informed consent given its observational nature, allowing us to capture consecutive patient samples in participating EDs. Each participating ED obtained consent for registry data collection from their local Institutional Ethics Review Boards as well. Our work was performed in accordance with the Declaration of Helsinki.
Results
Of the 82,965 patients presenting to the 47 participating EDs during the study, 14,290 (17%) had confirmed SARS-CoV-2 infection based on PCR testing, and were admitted to hospital (Fig. 1): 9942 (70%), 630 (4%) and 3718 (26%) were adjudged to have COVID-19 as the Direct cause, a potential Contributing factor, or an Incidental finding for their hospitalization, respectively.
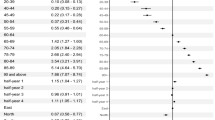
While COVID-associated symptoms were more common in those with hospitalizations deemed to be Directly due to COVID-19 (96%), 82% of the Contributing group and 75% of the Incidental group exhibited at least one COVID-related symptom on presentation to the ED (Table 1). The most common were shortness of breath (50%), cough (45%), generalized weakness (37%), or fever/chills (32%). Patients with Incidental SARS-CoV-2 infection were younger and had less hypertension, diabetes, underlying lung disease, or moderate or severe liver disease, but were more likely to have active cancer, and to smoke or misuse alcohol or illicit substances, compared to those patients hospitalized for COVID-19 (Table 1). Patients hospitalized for COVID-19 were more likely to present with Canadian Triage and Acuity Scale (CTAS) status 1 or 2 (emergent or needing acute resuscitation) at presentation. Among those with known vaccine status, hospitalizations in unvaccinated patients were more likely to be Direct COVID-19 admissions (75%) than hospitalizations in fully vaccinated patients (53%, p < 0.001).
While any of the COVID therapies (dexamethasone, remdesivir, tocilizumab, sotrovimab, or nirmatrelvir/ritonavir) were more likely to have been dispensed to the Direct Hospitalization group (55%), they were also prescribed in 21% of the Contributing group and in 19% of patients in the Incidental group (Table 2).
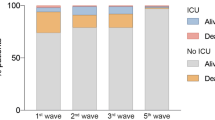
While COVID-19 was deemed the Direct cause of the admission in 88% of patients hospitalized during the first pandemic wave, this decreased markedly (Fig. 2) to 53% of hospitalizations during wave 5 (corresponding to the Omicron surge in Canada). Of note, 99% of hospitalizations where COVID-19 was deemed to be the Direct cause had a most responsible diagnosis of COVID-19 with respiratory manifestations. The proportion of SARS-CoV-2 positive hospitalizations that were deemed to be directly due to COVID-19 using our criteria was similar across provinces in each wave (eFigure 1) and was consistently larger than the proportion of hospitalizations meeting the CDC definition for a hospitalization “caused by COVID-19” (Fig. 2). Of the 8246 hospitalizations in known unvaccinated patients, 6190 (75.1%) were for COVID-19 directly and of the 381 hospitalizations in partially vaccinated patients, 275 (72.1%); in comparison, in fully vaccinated patients 557 (53.4%) of 1043 hospitalizations were for COVID-19 (Table 1).
SARS-CoV-2 was a potential contributing factor in 630 hospitalizations (4% overall, ranging from 2% in Wave 1 to 7% in the Omicron wave). The most common primary diagnoses (e Appendix Table e1) in the Contributing group were diseases of the nervous system (such as stroke or delirium), poisonings or injuries (including adverse drug reactions, alcohol misuse, and falls), endocrine or metabolic abnormalities (hyponatremia, diabetic ketoacidosis, or other electrolyte disturbances), or circulatory system conditions (principally heart failure, arrhythmias, or acute coronary syndrome). SARS-CoV-2 was deemed Incidental in 3718 admissions (26% overall, ranging from 10% in Wave 1–41% in the Omicron wave). The most common primary diagnoses in the Incidental group were diseases of the digestive system (abdominal surgeries, liver disorders, diverticulitis or cholecystitis, and bowel obstructions), non-cardiac circulatory system conditions (principally hypertension), or non-stroke non-delirium diseases of the nervous system (principally seizures, dementia, or lower motor neuron conditions).
Patients in the Direct group exhibited significantly longer LOS and a higher rate of critical care admission (with longer critical care stays), and were more likely to die in hospital, compared to the other groups (Table 2). However, those in the Incidental group exhibited substantial morbidity: mean hospital LOS 12 days, 11% were admitted to a critical care unit (for a mean of 9.5 days), and 9% died within 30 days (Table 2). Those in the Contributing group had comparatively better outcomes, although their CTAS distribution suggests they were less sick at baseline and their mix of diagnoses was substantially different from the other categories (Table 1).
Interpretation
Our study found that the proportion of hospitalized patients deemed to have Incidental SARS-CoV-2 infection increased proportionally across waves, but these patients still experienced substantial morbidity and mortality. We found that 75% of patients meeting our definition of “incidental infections” exhibited at least one symptom potentially attributable to COVID-19 when they presented for care, albeit that symptom may have been due to other reasons, and almost a fifth were treated with COVID-19 therapies by their attending physicians. Of note, the assignment of whether an infection was incidental rather than the cause or a contributor to the need for admission was made by our team based on the final diagnoses assigned by each patient’s attending physician at discharge, and it is thus not surprising that some patients received COVID-19 therapies during their hospital stay before the results of all tests were back and final diagnoses were apparent. In addition, it is likely that even in those who were asymptomatic and didn’t receive COVID-19 therapies, concomitant SARS-CoV-2 infection likely influenced treatment decisions and negatively impacted the length of stay for their most responsible diagnosis due to slower access to diagnostics, procedures, and allied health support due to infection control precautions. The mean hospital LOS for patients with “incidental” SARS-CoV-2 infection was 12 days, compared to an average hospital LOS in Canada of 6.9 days pre-pandemic16. If health authorities choose not to include “incidental” COVID-19 hospitalizations in planning, they may be substantially underestimating the current resource needs of hospitals, which could contribute to under-resourced and potentially overwhelmed hospitals. Incorporating the needs of these resource-intensive so-called ”Incidental” infections is necessary for accurate inpatient resource planning, and to direct public health measures aimed at protecting healthcare system capacity.
The diagnoses, demographics, and comorbidity profiles differed between the Direct, Contributing, and Incidental groups, therefore we cannot determine the excess mortality and morbidity that was directly attributable to SARS-CoV-2 infection in patients assigned other most responsible diagnoses. Future work would need to directly compare patients with “incidental SARS-CoV-2 infection” with a matched cohort with the same primary diagnoses but negative SARS-CoV-2 tests (this is not possible in our study as data was only systematically collected on patients with positive SARS-CoV-2 tests). However, others have shown that concomitant SARS-CoV-2 infection is associated with worse outcomes in patients with a wide variety of diagnoses17,18,19, supporting our assertion that healthcare capacity is influenced by all SARS-CoV-2 infected patients and not just those admitted specifically for COVID-19.
Our finding that the proportion of hospitalized patients with SARS-CoV-2 infection who were admitted for COVID-19 declined as the pandemic evolved is not surprising, and likely multifactorial. First, different variants of concern (with differences in transmissibility and virulence) drove each of the waves in Canada, and population prevalence rates increased with successive waves, increasing the chance that individuals hospitalized for other reasons would also have concomitant SARS-CoV-2 infection12,13. Second, the introduction of vaccinations and outpatient therapies also influenced clinical manifestations, severity of disease, and need for hospitalization in those with COVID-1913. However, although unvaccinated patients were more likely to be admitted for COVID-19 (75% of their hospitalizations with SARS-CoV-2 infection), even in fully vaccinated patients over half of hospitalizations were for COVID-19 and thus the upswing in “Incidental” SARS-CoV-2 infections over time was not just a manifestation of increasing vaccination rates. Third, as clinicians’ knowledge about the manifestations of COVID-19 expanded over time, it seems likely that their assignment of most responsible diagnoses in infected patients would have evolved commensurate with that knowledge. Our data is consistent with a recent CDC report on American hospitals that found that the proportion of admissions in SARS-CoV-2 infected patients that were attributed directly to COVID-19 declined from 84% in wave 1 to approximately half during the omicron wave7. Other reports have also confirmed that during the Omicron wave nearly half of hospitalizations in SARS-CoV-2 infected patients had incidental infections9,14. This aligns with data showing that patients infected with the Omicron variant experienced less involvement of the lower respiratory tract, less delirium, and less need for admission than those infected with earlier variants15.
Limitations
As with any retrospective observational study using chart reviews, there are limitations to our work, principally around the possibility of misclassification bias. As acknowledged earlier, our study design does not let us determine causation for the poor outcomes we observed in the Incidental infection group. It should be recognized that the Incidental group was heterogeneous and included a number of patients undergoing surgery or with active cancer or substance use disorders as well as patients with less severe illnesses. However, it remains a fact that these patients used substantial in-hospital resources, and had high in-hospital mortality, which should bear on resource planning.
Unfortunately, there is no standard definition of hospitalization “for COVID-19” versus “with incidental SARS-CoV-2 infection”, with varying definitions used by regions and countries. We chose to use consensus-based definitions derived by clinicians experienced in COVID-19 care based on the most responsible diagnosis assigned at hospital discharge to classify hospitalizations, as we contend that the clinician actually caring for the patient during the course of their hospitalization is best situated to make this determination. This resulted in a higher proportion of admissions in each wave (approximately 10%) being classified as “Directly” due to COVID-19 using our definitions than would have been the case if we’d used the CDC definition (Fig. 2). In an earlier study conducted in British Columbia by our team, multiple reviewers assessed the medical charts of 1651 patients hospitalized during the omicron wave with a very high degree of consistency (kappa 0.89, 95% CI 0.83–0.96) in assignment of which hospitalizations were “for COVID-19” versus “with incidental infection” and that the CDC definition underestimated Direct COVID-19 hospitalizations by 9.8%11. Recognizing that some hospitalizations for non-COVID conditions (for example, thromboembolic events, heart failure or COPD exacerbations, diabetic ketoacidosis) may be attributable to the additional physiological burden of concomitant SARS-CoV-2 infection, we classified these hospitalizations as "Potential Contributing" rather than definitively assigning them to the “Direct” versus “Incidental” categories. We believe our 3 tier classification provides more granular information on prognosis and resource utilization in hospitalized patients with SARS-CoV-2 infection. While some may argue that patients admitted for anxiety, depression, or overdoses/suicide attempts within 14 days of a positive test for SARS-CoV-2 infection should not be included in the “Potential Contributing” category, we decided to do so as it was impossible to judge to what extent testing positive contributed to these patients’ mental health and we wanted to be as conservative as possible in declaring hospitalizations unrelated to COVID-19. It should be noted that this was a small number of patients (78) and if we classified these in the “Incidental” category instead it would have had minimal impact on our findings, increasing the prevalence of hospitalizations with incidental SARS-CoV-2 infections from 26.0 to 26.6%.
Conclusion
Patients admitted to hospital with a SARS-CoV-2 infection who met our definition of “Incidental” have increased proportionately over time but, contrary to assumptions, these patients still have substantial health resource needs. Thus, policy decision-making should not solely focus on the number of hospitalizations in which COVID-19 is implicated as the direct cause, but, using standardized definitions, should include all hospitalizations in patients with SARS-CoV-2 infection, which in turn may facilitate more accurate resource planning for hospitals. In addition, there is a need for standardized definitions to modify the existing ICD-10 code U07.1 to allow the distinction between those hospitalizations where COVID-19 is the Direct cause, a Potential Contributing Factor, or an Incidental finding to refine healthcare administrative data commonly used to inform hospital capacity planning and public health measures.
Data availability
To comply with Canada’s Healthcare Privacy Legislation, the dataset used for this study cannot be made publicly available. The dataset from this study is held securely in coded form within the University of British Columbia office of the Canadian COVID-19 Emergency Department Rapid Response Network (CCEDRRN, see www.ccedrrn.com). While legal data sharing agreements between the investigators, participating institutions, and CCEDRRN prohibit us from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, and requests should be forwarded to admin.ccedrrn@ubc.ca.
References
Zweig, D. Our most reliable pandemic number is losing meaning. The Atlantic, Sep 13, 2021. https://www.theatlantic.com/health/archive/2021/09/covid-hospitalization-numbers-can-be-misleading/620062/. (accessed 3 Apr 2023).
Fillmore, N. et al. The COVID-19 hospitalization metric in the pre- and postvaccination eras as a measure of pandemic severity: A retrospective, nationwide cohort study. Infect. Control Hosp. Epidemiol. 43, 1767–1772 (2022).
Picard, A. There’s nothing incidental about hospital patients with COVID-19. The Globe and Mail, January 17, 2022. https://www.theglobeandmail.com/opinion/article-theres-nothing-incidental-about-hospital-patients-with-covid-19/. (accessed 3 Apr 2023).
Khullar, D. Do the Omicron Numbers Mean What We Think They Mean? The New Yorker. 2022. Jan 16, 2022. https://www.newyorker.com/magazine/2022/01/24/do-the-omicron-numbers-mean-what-we-think-they-mean/ (accessed 3 Apr 2023).
Canadian Institute for Health Information. COVID-19 hospitalization and emergency department statistics [Product release]. (accessed 3 Apr 2023).
https://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-hospital-activity/ (accessed 18 Sep 2022).
Adjei, S. et al. Mortality risk among patients hospitalized primarily for COVID-19 during the omicron and delta variant pandemic periods—United States, April 2020–June 2022. MMWR Morb. Mortal Wkly. Rep. 71, 1182–1189 (2022).
Hill, M. Almost half of Mass. COVID hospitalizations are now classified as “incidental”. Here’s what that means. Boston.com Jan 21, 2022. https://www.boston.com/news/coronavirus/2022/01/21/almost-half-of-mass-covid-hospitalizations-are-now-classified-as-incidental-heres-what-that-means/ (accessed 28 Mar 2023).
Klann, J. G., Strasser, Z. H., Hutch, M. R., Kennedy, C. J., Marwaha, J. S., Morris, M., et al. for the Consortium for Clinical Characterization of COVID-19 by EHR (4CE). Distinguishing admissions specifically for COVID-19 from incidental SARS-CoV-2 admissions: National retrospective electronic health record study. J. Med. Internet. Res. 24, e37931 (2022).
Hohl, C. M., Rosychuk, R. J., McRae, A. D., et al. for the Canadian COVID-19 Emergency Department Rapid Response Network investigators and for the Network of Canadian Emergency Researchers and the Canadian Critical Care Trials Group. Development of the Canadian COVID-19 Emergency Department Rapid Response Network population-based registry: A methodology study. CMAJ Open. 9, e261–e270 (2021).
Hohl, C. M., Cragg, A., Pursell, E. et al. for the Canadian COVID-19 Emergency Department Rapid Response Network (CCEDRRN) investigators and for the Network of Canadian Emergency Researchers and the Canadian Critical Care Trials Group. Misclassifying SARS-CoV-2 admissions underestimates COVID-19 related hospital days and mortality. (under review).
Brown, P. E. et al. Omicron BA.1/1.1 SARS-CoV-2 infection among vaccinated Canadian adults. N. Engl. J. Med. 386, 2337–2339 (2022).
McAlister, F. A. et al. The impact of shifting demographics, variants of concern, and vaccination on outcomes during the first three COVID-19 waves in Alberta and Ontario: Retrospective cohort study. CMAJ Open 10, e400–e408 (2022).
Sah, P. et al. Asymptomatic SARSCoV-2 infection: A systematic review and meta-analysis. Proc. Natl. Acad. Sci. U. S. A. 118(34), e2109229118 (2021).
Menni, C. et al. Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: A prospective observational study from the ZOE COVID Study. Lancet 399, 1618–1624 (2022).
Canadian Institute for Health Information. Hospital Stays in Canada [product release]. https://www.cihi.ca.en/hospital-stays-in-canada(accessed 3 Apr 2023).
Thakker, R. A. et al. Comparison of coronary artery involvement and mortality in STEMI patients with and without SARS-CoV-2 during the COVID-19 Pandemic: A systematic review and meta-analysis. Curr. Probl. Cardiol. 47, 101032 (2022).
Greene, S. J., Lautsch, D., Yang, L., Tan, X. I. & Brady, J. E. Prognostic interplay between COVID-19 and heart failure with reduced ejection fraction. J. Card. Fail. 28, 1287–1297 (2022).
Bodilsen, J. et al. Hospital admission and mortality rates for non-covid diseases in Denmark during covid-19 pandemic: Nationwide population based cohort study. BMJ 373, n1135 (2021).
Acknowledgements
The Canadian COVID-19 Emergency Department Rapid Response Network is funded by the Canadian Institutes of Health Research (447679, 464947, and 466880), Ontario Ministry of Colleges and Universities (C-655-2129), Saskatchewan Health Research Foundation (5357), Genome BC (COV024 and VAC007) Fondation du CHU de Québec (Octroi No. 4007) Sero-Surveillance and Research (COVID-19 Immunity Task Force Initiative) provided peer-reviewed funding. The BC Academic Health Science Network and BioTalent Canada provided non-peer reviewed funding. These organizations are not-for-profit, and had no role in study conduct, analysis, or manuscript preparation.
Author information
Authors and Affiliations
Consortia
Contributions
Concept and design: F.A.M. and C.M.H. Data collection: all members of CCEDRRN. Data analysis and presentation: J.P.H. and R.J.R. First draft of manuscript: F.A.M. Criticial revisions of manuscript: F.A.M., J.P.H., C.A., A.D.M., L.J.M., L.G., I.C., R.J.R., C.M.H.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McAlister, F.A., Hau, J.P., Atzema, C. et al. The burden of incidental SARS-CoV-2 infections in hospitalized patients across pandemic waves in Canada. Sci Rep 13, 6635 (2023). https://doi.org/10.1038/s41598-023-33569-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-33569-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.