Abstract
The burden of disease attributable to obesity is rapidly increasing and becoming a public health challenge globally. Using a nationally representative sample in Australia, this study aims to examine the association of obesity with healthcare service use and work productivity across outcome distributions. We used Household, Income and Labour Dynamics Australia (HILDA) Wave 17 (2017–2018), including 11,211 participants aged between 20 and 65 years. Two-part models using multivariable logistic regressions and quantile regressions were employed to understand variations in the association between obesity levels and the outcomes. The prevalence of overweight and obesity was 35.0% and 27.6%, respectively. After adjusting for socio-demographic factors, low socioeconomic status was associated with a higher probability of overweight and obesity (Obese III: OR = 3.79; 95% CI 2.53–5.68) while high education group was associated with a lower likelihood of being high level of obesity (Obese III OR = 0.42, 95% CI 0.29–0.59). Higher levels of obesity were associated with higher probability of health service use (GP visit Obese, III: OR = 1.42 95% CI 1.04–1.93,) and work productivity loss (number of paid sick leave days, Obese III: OR = 2.40 95% CI 1.94–2.96), compared with normal weight. The impacts of obesity on health service use and work productivity were larger for those with higher percentiles compared to lower percentiles. Overweight and obesity are associated with greater healthcare utilisation, and loss in work productivity in Australia. Australia’s healthcare system should prioritise interventions to prevent overweight and obesity to reduce the cost on individuals and improve labour market outcomes.
Similar content being viewed by others
Introduction
The growing prevalence of obesity and overweight has become a global public health concern. Globally, the prevalence of obesity has doubled since 19801. The Global Burden of Disease group (2017) estimated that high body mass index (BMI) contributed to 4.0 million deaths, which represented 7.1% of the deaths from any cause; it also contributed to 120 million disability-adjusted life-years (DALYs), which represented 4.9% of DALYs from any cause among adults globally1. Excessive body weight (including overweight and obesity) was associated with 8.4% of the overall health burden in Australia (2020)2. It is currently estimated that 2 in 3 Australian adults are overweight or obese2. Furthermore, there has been a worrying shift in the proportion of those who are ‘overweight’ to ‘obese’3. For example, while the prevalence of overweight has somewhat stabilised over the past three decades, there has been a large increase in prevalence of obesity from 18.7% in 1995 to 31.3% in 20184. The prevalence of overweight and obesity also follows a socioeconomic gradient, being more common in lower socio-economic groups and among the Indigenous population2. National statistics found that female Indigenous Australians are 1.2 times more likely to be overweight and 1.5 times more likely to be obese in comparison to their non-Indigenous counterparts2.
The rising burden of overweight and obesity has an impact on health systems and national economies. There are few studies investigating the economic impact of excessive weight on health service use, direct medical cost and productivity loss but most of them are from US or Europe5,6,7,8. These studies have demonstrated that higher level of BMI is associated with increased number of outpatient visits, emergency room visits, higher probability of hospitalisation, higher level of health expenditures and work productivity loss9,10,11,12.
The literature on the economic impact of overweight and obesity is extremely small compared to the rapid increase in prevalence of obesity in Australia. Existing studies examined the association between high BMI and health costs13,14,15. For example, Colagiuri and colleagues (2010) analysed 5-year follow-up data from the Australian Diabetes, Obesity and Lifestyle study and found that the annual total direct cost per person increased from $1472 for those of normal weight to $2788 for the obese in 200513. Brown and colleagues (2008) examined relationships between physical activity and BMI with health care costs in women. They reported that higher BMI was associated with increased risk of making more than 15 claims per year with the national Medicare health insurance16. There are two studies that examined the impact of high BMI on productivity loss in Australia, including one focused on Australian defence force personnel17, and one estimated the societal benefit of reducing obese together with five other risk factors in Australia18. However, these studies are limited in selected geographical areas or a subgroup of the populations. Little is known on the impact of overweight and obesity on health service use and productivity loss among general population in Australia. In addition, previous studies in Australia have utilised traditional linear regression, with a focus on the mean effect of obesity on economic outcomes. However, the association between overweight and obese and economic outcomes (such as service use, health cost and productivity loss) may vary across the distribution of outcomes. Quantile regression provides a more robust estimation on the effect between chronic conditions, risk factors and economic outcome across population19. To fill this important evidence gap, using a nationally presentative data, we present the first study in Australia that applied quantile regression methods to examine the effect of overweight and obesity on health service utilisation and labour force participation.
Methods
Sample and data
We used the nationally representative cross-sectional data from the Household, Income and Labour Dynamics in Australia (HILDA) wave 17, which was conducted between 2017 and 2018. HILDA is a nationally representative longitudinal study of Australian residents aged 15 years and above. The baseline survey of HILDA commenced in 2001, collecting information annually on various aspects of life in Australia, including demographics, socio-economic status, healthcare utilisation, work productivity, and the Health-Related Quality of Life (HRQoL). Multi-stage sampling approach was used to select sample households. First, a stratified random sample of 488 Census Collection District containing 200 to 250 households in each district was selected20. A sample of 22 to 34 dwellings were then randomly selected, and within each dwelling, up to three random households were selected20. Interviews and self-completed questionnaire following the University of Melbourne’s ethical guidelines were used for data collection. Further detailed description of the survey objectives and data collection method can be found elsewhere20. HILDA Wave 17 includes a total of sample including 17,570 respondents with a response rate of 96.4%. In this analysis, we included working-age respondents between 20 and 65 years old with Body Mass Index (BMI) ≥ 18.5 kg/m2 and excluded those who had a missing value on outcomes and any of the covariates. The final sample consists of 11,211 respondents.
Measures obesity levels
The survey provided respondents’ BMI, which was derived from self-reported weight in kilograms and height in meters (kg/m2). We classified BMI into five obesity levels according to the World Health Organisation (WHO) definition; normal weight (BMI: 18.5–24.9 kg/m2), overweight (BMI: 25–29.9 kg/m2), obesity class I (BMI: 30–34.9 kg/m2), obesity class II (BMI: 35–39.9 kg/m2), and obesity class III (BMI: ≥ 40 kg/m2)21.
Outcomes
In this study, health service use was measured using the number of General Practitioner (GP) visits and nights spent at hospital, as well as the number of prescribed medications for regular use in the previous 12 months. Work productivity was measured through the number of paid sick leave days taken in the last 12 months for the respondents who were employed at the time of the survey.
Covariates
Covariates included sex, age group (20–29, 30–39, 40–49, 50–59, 60–65), education level (low, middle, high), household income (1–4 quantiles of sample), Indigenous status (Non-Indigenous Australian, Indigenous Australian), country of birth (Australia, main English-speaking countries, other), marital status (married/de facto, others), Australian state (New South Wales, Victoria, South Australia, Queensland, Western Australia, Tasmania, Northern Territory, Australian Capital Territory), residential area (urban, rural), alcohol intake (no alcohol intake, drink alcohol less than 3 days per week, drink alcohol 3 and more days per week), smoking (non-smoker, ex-smoker, current smoker).
Statistical analysis
We examined the determinants of overweight and obesity using multivariable logistic regression models. Two-part models were used to investigate the association of overweight and obesity with health service use and work productivity loss. First, we applied a multivariable logistic regression model to examine the probability of observing positive binary outcomes for any health service use (yes/no) and any sick leave taken (yes/no) against obesity levels. Second, for those with positive binary outcomes for these variables, we performed multivariable quantile regression to estimate the different impacts of overweight and obesity on health service use and loss of work productivity across their distributions (10th, 25th, 50th, 75th, and 90th percentiles). The quantile regression is estimating the quantiles for the outcome variable associated with a set of independent variables and covariates without assuming normality or homoscedasticity of the underlying distribution22,23. Advantage of the quantile regression is the robustness to outliers as it allows for assessing the full distribution of the outcome variable and is suitable for modelling outcomes that are not normally distributed or are highly skewed22,23.
In this study, the coefficients at the lower percentiles of the health service use distribution (e.g. the 10th, 20th, and 30th percentiles) indicate the association between obesity and low level of health service use, while the coefficient at the higher percentiles of the health service use distributions (e.g. 70th, 80th, and 90th percentiles) reflect the association between overweight and obesity and high level of health service use. In addition, we performed Ordinary Least Square models (OLS) and presented estimated mean change of the outcomes by overweight and obesity levels to compare with the estimated change at different points of outcome distributions obtained from multivariable quantile regression models. All multivariable regression models were adjusted for covariates listed above and p-values < 0.05 were considered statistically significant. All analyses were performed using Stata 15 (Stata Corp., College Station, Texas).
Results
Sample characteristics
The study sample consisted of 11,211 respondents. The median age of respondents was 42 (IQR 30–53) and BMI was 26.4 (IQR 23.4–30.5). The majority of respondents were married/de facto (70.6%), living in an urban area (87.4%), with a middle or high education level (84.1%). The prevalence of each obesity level was 37.5% (normal weight), 35.0% (overweight), 16.8% (obese I), 6.69% (obese II), and 4.08% (obese III). (Table 1).
Sociodemographic correlates of overweight and obesity
Table 2 presents the determinants of each obesity level. The odds of being obese were higher for those in lower socioeconomic group (SEIFA 5: Obese II OR = 2.46, 95% CI 1.85–3.28, Obese III OR = 3.79, 95% CI 2.53–5.68) compared to higher socioeconomic group. Respondents who are not in the labour force have 65% higher likelihood of being highest level of obese (95% CI 1.29–2.11). Middle age group (40–49 years old and 50–59 years old) showed higher likelihood of being overweight and obese compared to other age groups. On the other hand, higher education level and higher alcohol intake showed adverse relationship with obesity level. High education group had 53% (95% CI 0.36–0.61) and 58% (95% CI 0.29–0.59) lower likelihood of being obese II and obese III, respectively. The odds of being severe obese were significantly lower for those who were born in non-English speaking countries (Obese II OR = 0.29, 95% CI 0.21–0.41, Obese III: OR = 0.26, 95% CI = 0.17–0.41). Drinking alcohol more than 3 days per week had 70% lower likelihood of being obese III (95% CI = 0.22–0.41). In addition, we found that Indigenous status has a positive association with lower obesity level (Obese II OR = 1.68, 95% CI 1.09–2.60) but the association was not significant for Obese III (OR = 0.9, 95% CI 0.50–1.60).
Association between obesity, health service use, and work productivity
Health service use across percentiles of outcome variables
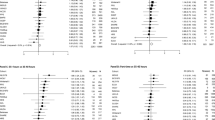
Table 3 describes the association between obesity levels and health service use. A higher level of obesity was associated with higher probability of using any GP (Obese III: OR = 1.42 95% CI 1.04–1.93), hospitalisation (Obese III: OR = 1.60 95% CI 1.22–2.09), as well as use of prescribed medication (Obese III: OR = 2.40, 95% CI 1.94–2.96).
Amongst those with normal weight and had any health service use, the estimated mean number of GP visit, nights at hospital, and prescribed medications were higher than their median (GP visit: 5.32 vs. 3, nights in hospital: 5.68 vs. 3, prescribed medication: 1.90 vs. 1), illustrating the positively skewed nature of the distributions.
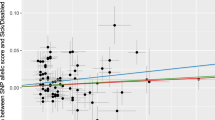
Table 3a shows the relationships between obesity level and GP visits by health service use quantile. An increase in BMI (from normal weight to overweight, obese I, obese II, and obese III) was associated with a higher likelihood of GP visits and a higher number of GP visits in every quantile group. The effect of obesity on GP visits was found to be greater in the upper tail of health service use distributions than in the lower tail. For example, the coefficient for obese II was 0 (95% CI − 0.15–0.15) for the 10th percentile, and 3.58 (95% CI 2.21–4.95) for the 90th percentile). The coefficient for obese III was 1.0 (95% CI 0.81–1.19) for the 10th percentile and 6.54 (95% CI 4.83, 8.25) for the 90th percentile.
Table 3b presents the relationship between obesity level and number of nights at a hospital. Number of nights in hospital was positively associated with obesity II and III at the 75th and 90th percentiles of the distribution while it was negatively associated with a lower level of obesity. However, these associations were not statistically significant.
The association between obesity level and number of prescribed medications is presented in Table 3c. Higher obesity level was associated with higher likelihood of an increasing number of prescribed medications compared to normal weight at the upper tail of the distribution. The effect of obesity was greater at the 75th and 90th percentiles of the distribution compared to the lower tail. For example, the coefficient for obese II was 0.76 (95% CI 0.43–1.09) for the 75th percentile and 1.34 (95% CI 0.74–1.94) for the 90th percentile. The coefficient for obese III was 1.23 (95% CI 0.84–1.62) for the 75th percentile and 2.20 (95% CI 1.49–2.91) for the 90th percentile.
Work productivity by percentiles
As shown in Table 4, a higher level of obesity was associated with higher probability of taking any sick leave compared to normal weight (Obese II: OR = 1.45, 95% CI 1.19–1.76, Obese III: OR = 1.62 95% CI 1.25–2.09). Of respondents who took any sick leave, the impact of obesity levels on number of sick leave was larger at the higher quantiles compared to lower quantiles. The coefficients for obese II was 0.52 (95% CI − 0.11–1.14) for the 10th percentile and 1.91 (95% CI 0.96–2.86) for the 75th percentile. The coefficient for obese III was 0.61 (95% CI − 0.19–1.41) for the 10th percentile and 2.83 (95% CI 1.62–4.03) for the 75th percentile. The association between high level of obesity and number of sick leave was not statistically significant at the 90th percentile of the distribution.
Discussion
Principal findings
Overall, the prevalence of overweight and obesity was 35.0% and 27.6%, respectively, among Australian residents aged 15 years and above during the period of 2017–2018. After adjusting for socio-demographic factors, low socioeconomic status was associated with overweight and high level of obesity while high education group was associated with a lower likelihood of being obese. Generally, a higher level of obesity was associated with higher probability of health service use, and work productivity loss. Regarding quantile analyses, using quintile regression methods, this study showed that the high level of obesity had significantly increased number of GP visits and prescribed medications across the outcome distributions, In terms of work productivity loss, the impact of obesity levels on number of sick leave was larger at upper tiles of distributions. These findings suggested that the impacts of overweight and obesity on health service use could be higher for obese individuals mainly because these individuals may have more healthcare needs.
Comparison with existing literature
We found that the prevalence of overweight and obesity was 35.0% and 27.6%, which is consistent with population data from Australia1,24. Our findings that lower income and educational attainment were associated with higher probability and levels of obesity is also in line with literature in Australia and other high-income countries25,26.
Higher levels of obesity were associated with increased number of GP visits and number of prescribed medications, which has been found in studies from other high-income countries9,11,12,27,28. The quantile regression analysis show that such association was more profound among those at upper tiles of distribution (i.e. among those use more GP service and prescribe more medications). This is in line with a study used quantile regression to examine association between BMI categories with health costs29. The finding of increased health service use is indicative of the direct costs of overweight and obesity in Australia, with annual estimates of between $2 Billion and $3.8 Billion24,30,31.
Overweight and obesity were associated with increased likelihood and number of sick leave days taken, and the effect was larger at upper tiles of distributions. Though focused on a sample from defence force in Australia, the author also found that productivity losses from full days off work were higher in the obese subgroup compared with the normal cohort17. Our finding is also in line with a border literature on the indirect costs of obesity on productivity loss32,33,34, with obesity believed to incur productivity costs of almost $5 Billion annually in Australia31,35,36.
Strengths and limitations
This is the first study to explore healthcare use and productivity loss associated with obesity using nationally representative data in Australia. Besides, this is a novel study to estimate the effect of obesity applying quantile regression which reflects the variations in the impact of obesity across the outcome distributions.
However, there are some limitations. First, we use self-reported data for BMI which may be biased due to measurement error. An existing study indicates that obese people are likely to underestimate weight37. In addition, self-reporting of health service use and productivity is likely to cause recall error as the respondents are required to remember and report information from the last 12 months. Second, the outcomes of the impact of obesity on health service use and productivity in this study might be underestimated, as the survey data was not collected from patients with severe illness or those admitted to hospital. Third, healthcare utilisation and productivity loss were not specifically due to illness or disability associated with obesity, and could have included other unrelated reasons and conditions such as acute illnesses and physical injury. Fourth, we used alcohol consumption based on weekly frequency but not on intensity, thus, it may not reflect the actual amount of alcohol consumption. Further, our analysis on work productivity only looked at number of sick leave days as an indicator due to the availability of question. Thus, the results might not capture the full picture of the burden of obesity. Other indicators of work productivity such as wage loss or presenteeism should be taken into account for future studies. Another limitation of our study is that our estimation may be biased as a result of omitting confounding factors that may be associated with outcomes, such as individuals' local environment and genetic factors, which are not captured in the HILDA survey. Lastly, the interpretation of causal effect might be limited because of the use of cross-sectional study design. Future studies need to consider using longitudinal data to observe a long-term effect of obesity on outcomes.
Policy implications
These findings highlight the significant variance in the demands that differing severities of overweight and obesity can place on health care systems, as well as its implication for employment productivity on both a personal and population level. This raises the question as to the appropriateness of direct and indirect cost estimates for obesity based on linear regression models. While this may capture mean estimated costs, they do not reflect the implications at the different quantiles of the distribution of outcomes.
Our results of the quantile regression analyses demonstrate the associations between obesity or overweight largely varied at different quantiles. The impact of obesity is larger for those with a higher degree of obesity and with greater use of health service and lower work productivity. A likely account for this result was that obese individuals suffer double economic burdens of increasing use of health services and reduced work productivity.
It is evident from our findings that policy approaches to address obesity and its impacts must be two-fold; firstly, addressing the prevalence of overweight and obesity in Australia, and secondly in reducing its association with adverse health service and productivity outcomes. A range of policy approaches are needed in order to confer both benefits, targeting obesity on both an individual and a population or workforce level. There are a number of broad measures to reduce the prevalence of excess weight which are supported by the literature; taxes on low nutrition foods and sugar sweetened beverages, while politically difficult have been modelled to reduce obesity and improve productivity35,38,39, as have investments in urban design to facilitate greater physical activity40,41. On an individual level, there is evidence for utilisation of bariatric surgery to both reduce excess weight and its impact on employees wellbeing, as well as reducing barriers to employment42,43.
It is also necessary that interventions and programs target those who already suffer from overweight and obesity, in order to improve their wellbeing and occupational performance. There is encouraging evidence that workplace-based health interventions can see improvements in health and productivity before a noticeable decline in overweight and obesity44,45,46. Evidence supports targeted interventions by Primary care practitioners35,47, however a lack of implementation of established guidelines for obesity management in Australia has hampered the effectiveness of this48,49. Failure to focus on both the management and prevention of obesity will see poor returns in the form of ongoing costs for both individuals and wider societal costs (Supplementary Table 1).
Data availability
Data is publicly available from Household, Income and Labour Dynamics in Australia Survey website: https://melbourneinstitute.unimelb.edu.au/hilda.
Change history
31 May 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41598-023-35911-0
Abbreviations
- BMI:
-
Body mass index
- HILDA:
-
Household, income, and labour dynamics Australia
- HRQoL:
-
Health-related quality of life
- SEIFA:
-
Socio-economic indexes for areas
- OLS:
-
Ordinary least squares
References
Health Effects of Overweight and Obesity in 195 Countries over 25 Years. New England Journal of Medicine. 2017;377(1):13–27.
Health AIo, Welfare. Overweight and obesity: an interactive insight. Canberra: AIHW; 2020.
Health AIo, Welfare. Australia's health 2018. Canberra: AIHW; 2018.
National Health Survey: First results: Australian Bureau of Statistics; 2018. https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-first-results/latest-release#data-download (2018).
Kent, S. et al. Body mass index and healthcare costs: A systematic literature review of individual participant data studies. Obes. Rev. 18(8), 869–879 (2017).
Goettler, A., Grosse, A. & Sonntag, D. Productivity loss due to overweight and obesity: A systematic review of indirect costs. BMJ Open 7(10), e014632 (2017).
Tsai, A. G., Williamson, D. F. & Glick, H. A. Direct medical cost of overweight and obesity in the USA: A quantitative systematic review. Obes. Rev. 12(1), 50–61 (2011).
Lehnert, T., Streltchenia, P., Konnopka, A., Riedel-Heller, S. G. & König, H. H. Health burden and costs of obesity and overweight in Germany: An update. Eur. J. Health Econ. 16(9), 957–967 (2015).
DiBonaventura, M., Lay, A. L., Kumar, M., Hammer, M. & Wolden, M. L. The association between body mass index and health and economic outcomes in the United States. J. Occup. Environ. Med. 57(10), 1047–1054 (2015).
Finkelstein, E., Fiebelkorn, I. C. & Wang, G. The costs of obesity among full-time employees. Am. J. Health Promot. 20(1), 45–51 (2005).
König, H.-H. et al. Health service use and costs associated with excess weight in older adults in Germany. Age Ageing 44(4), 616–623 (2015).
Espallardo, O. et al. The impact of severe obesity on healthcare resource utilisation in Spain. Obes. Surg. 27(8), 2058–2066 (2017).
Colagiuri, S. et al. The cost of overweight and obesity in Australia. Med. J. Aust. 192(5), 260–264 (2010).
Buchmueller TC, Johar M. Obesity and health expenditures: Evidence from Australia. 2015. p. 42–58.
Lee, C. M. Y. et al. The cost of diabetes and obesity in Australia. J. Med. Econ. 21(10), 1001–1005 (2018).
Brown, W. J., Hockey, R. & Dobson, A. J. Physical activity, body mass index and health care costs in mid-age Australian women. Aust. N. Z. J. Public Health 32(2), 150–155 (2008).
Peake, J. et al. The health and cost implications of high body mass index in Australian defence force personnel. BMC Public Health 12(1), 451 (2012).
Cadilhac, D. A. et al. The societal benefits of reducing six behavioural risk factors: An economic modelling study from Australia. BMC Public Health 11(1), 483 (2011).
Zhao, Y. et al. Medical costs and out-of-pocket expenditures associated with multimorbidity in China: Quantile regression analysis. BMJ Glob. Health 6(2), e004042 (2021).
The Household, Income and Labour Dynamics in Australia (HILDA) Survey. The University of Melbourne. [Internet]. Melbourne: Melbourne Institute; 2020. https://melbourneinstitute.unimelb.edu.au/hilda (2020).
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i-xii, 1–253.
Firpo, S., Fortin, N. M. & Lemieux, T. Unconditional quantile regressions. Econometrica 77(3), 953–973 (2009).
Koenker, R. & Hallock, K. F. Quantile regression. J. Econ. Perspect. 15(4), 143–156 (2001).
Australian Institute of Health and Welfare. A Picture of overweight and Obesity in Australia. Canberra: AIHW; 2017.
Ogden, C. L. et al. Prevalence of obesity among adults, by household income and education—United States, 2011–2014. MMWR Morb. Mortal. Wkly. Rep. 66(50), 1369 (2017).
Health AIo, Welfare. Overweight and obesity. Canberra: AIHW; 2020.
An, R. Health care expenses in relation to obesity and smoking among U.S. adults by gender, race/ethnicity, and age group: 1998–2011. Public Health 129(1), 29–36 (2015).
Lal, A., Moodie, M., Ashton, T., Siahpush, M. & Swinburn, B. Health care and lost productivity costs of overweight and obesity in New Zealand. Aust. N. Z. J. Public Health 36(6), 550–556 (2012).
Lee, S. M. et al. Incremental treatment costs attributable to overweight and obesity in patients with diabetes: Quantile regression approach. Obesity (Silver Spring) 26(1), 223–232 (2018).
Buchmueller, T. C. & Johar, M. Obesity and health expenditures: Evidence from Australia. Econ. Hum. Biol. 17, 42–58 (2015).
Crosland, P., Ananthapavan, J., Davison, J., Lambert, M. & Carter, R. The economic cost of preventable disease in Australia: A systematic review of estimates and methods. Aust. N. Z. J. Public Health 43(5), 484–495 (2019).
Hoque, M. E., Mannan, M., Long, K. Z. & Al, M. A. Economic burden of underweight and overweight among adults in the Asia-Pacific region: A systematic review. Trop. Med. Int. Health 21(4), 458–469 (2016).
Tremmel, M., Gerdtham, U.-G., Nilsson, P. M. & Saha, S. Economic burden of obesity: A systematic literature review. Int. J. Environ. Res. Public Health 14(4), 435 (2017).
Goettler, A., Grosse, A. & Sonntag, D. Productivity loss due to overweight and obesity: A systematic review of indirect costs. BMJ open. 7(10), e014632 (2017).
PriceWaterhouseCooper. Weighing the cost of obesity: A case for action. 2015.
Cadilhac, D. A. et al. The societal benefits of reducing six behavioural risk factors: An economic modelling study from Australia. BMC Public Health 11, 483 (2011).
Skeie, G., Mode, N., Henningsen, M. & Borch, K. B. Validity of self-reported body mass index among middle-aged participants in the Norwegian Women and Cancer study. Clin. Epidemiol. https://doi.org/10.2147/CLEP.S83839 (2015).
Nomaguchi, T., Cunich, M., Zapata-Diomedi, B. & Veerman, J. L. The impact on productivity of a hypothetical tax on sugar-sweetened beverages. Health Policy 121(6), 715–725 (2017).
Carter, H. E., Schofield, D. J., Shrestha, R. & Veerman, L. The productivity gains associated with a junk food tax and their impact on cost-effectiveness. PLoS ONE 14(7), e0220209 (2019).
Brown, V. et al. Better transport accessibility, better health: A health economic impact assessment study for Melbourne, Australia. Int. J. Behav. Nutr. Phys. Act. 16(1), 89 (2019).
Sacks, G., Swinburn, B. & Lawrence, M. Obesity Policy Action framework and analysis grids for a comprehensive policy approach to reducing obesity. Obes. Rev. 10(1), 76–86 (2009).
Kantarovich, K., Wnuk, S., Cassin, S., Hawa, R. & Sockalingam, S. Employment outcomes 2 years after bariatric surgery: Relationship to quality of life and psychosocial predictors. Obes. Surg. 29(9), 2854–2861 (2019).
Mancini, A. et al. Bariatric surgery improves the employment rate in people with obesity: 2-year analysis. Surg. Obes. Relat. Dis. 14(11), 1700–1704 (2018).
Bhojani, F. A., Tsai, S. P., Wendt, J. K. & Koller, K. L. Simulating the impact of changing trends in smoking and obesity on productivity of an industrial population: An observational study. BMJ Open 4(4), e004788 (2014).
Anderson, L. M. et al. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: A systematic review. Am. J. Prev. Med. 37(4), 340–357 (2009).
Bilger, M., Finkelstein, E. A., Kruger, E., Tate, D. F. & Linnan, L. A. The effect of weight loss on health, productivity, and medical expenditures among overweight employees. Med. Care 51(6), 471–477 (2013).
Fitzpatrick, S. L. et al. An evidence-based guide for obesity treatment in primary care. Am. J. Med. 129(1), 115 (2016).
Forgione, N., Deed, G., Kilov, G. & Rigas, G. Managing obesity in primary care: Breaking down the barriers. Adv. Ther. 35(2), 191–198 (2018).
Turner, L. R., Harris, M. F. & Mazza, D. Obesity management in general practice: Does current practice match guideline recommendations?. Med. J. Aust. 202(7), 370–372 (2015).
Author information
Authors and Affiliations
Contributions
The concept for study was developed by J.L., M.I. and Y.Z. M.I. analyzed the data. M.I. D.M., Y.Z., P.T., C.W., H.T., and J.L. wrote the first draft, and all authors contributed and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: In the original version of this Article Tianxin Pan was incorrectly affiliated with ‘School of Population and Global Health, Nossal Institute for Global Health, University of Melbourne, Melbourne, Australia’. The correct affiliation is: ‘Health Economics Unit, Centre for Health Policy, Melbourne School of Population and Global Health, University of Melbourne, Melbourne, Australia’.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ishida, M., D’Souza, M., Zhao, Y. et al. The association between obesity, health service use, and work productivity in Australia: a cross-sectional quantile regression analysis. Sci Rep 13, 6696 (2023). https://doi.org/10.1038/s41598-023-33389-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-33389-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.