Abstract
Chemoradiotherapy (CRT) and radiotherapy (RT) are treatment options for esophageal squamous cell carcinoma (ESCC), but local residual/recurrent cancer after CRT/RT is a major problem. Endoscopic resection (ER) is an effective treatment option for local residual/recurrent cancer. To ensure the efficacy of ER, complete removal of endoscopically visible lesions with cancer-free vertical margins is desired. This study aimed to identify the endoscopic parameters associated with the complete endoscopic removal of local residual/recurrent cancer. In this single-center, retrospective study, we used a prospectively maintained database to identify esophageal lesions that were diagnosed as local residual/recurrent cancer after CRT/RT and treated by ER between January 2012 and December 2019. We evaluated the associations of endoscopic R0 resection with findings on conventional endoscopy and endoscopic ultrasonography (EUS). In total, 98 lesions (83 cases) were identified from our database. The rate of endoscopic R0 resection was higher for flat lesions (100% versus 77%, P = 0.00014). EUS was performed for 24 non-flat lesions, and endoscopic R0 resection was achieved for 94% of lesions with an uninterrupted fifth layer. Flat lesions on conventional endoscopy and lesions with an uninterrupted fifth layer on EUS are good candidates for ER.
Similar content being viewed by others
Introduction
Esophageal cancer is the seventh most common cancer and sixth most common cause of cancer-related mortality worldwide1, and squamous cell carcinoma is the predominant type of esophageal cancer in Asia2. Chemoradiotherapy (CRT) is a treatment option for esophageal squamous cell carcinoma (ESCC), and radiotherapy (RT) is applied for patients who are not suitable for CRT, such as elderly patients and patients with complications. Although CRT/RT can preserve the esophagus and is expected to achieve a complete response, local residual/recurrent cancer after CRT/RT remains a major problem3. Although esophagectomy is a promising treatment for local residual/recurrent cancer, it is associated with high mortality and morbidity rates4,5. Endoscopic resection (ER) is an alternative to esophagectomy that is minimally invasive and effective if complete resection of local residual/recurrent cancer is achieved6,7.
The major limitation of ER is difficulty in achieving en bloc R0 resection. Low R0 resection rates have been reported for ER of local residual/recurrent cancer because of its technical difficulty7,8. Even if pathological examination of the resected specimen reveals a positive horizontal margin, the outcome after ER is usually favorable if the endoscopically visible lesion is removed9. However, the outcome after ER with pathological evidence of a positive vertical margin has not been thoroughly evaluated. To ensure the efficacy of ER, complete removal of the endoscopically visible lesion with a cancer-free vertical margin is desired.
To completely remove the lesion with a cancer-free vertical margin, accurate preoperative assessment of the cancer invasion depth is essential. However, this is sometimes difficult for local residual/recurrent cancer, mainly because of fibrosis and vascular change caused by CRT/RT. To the best of our knowledge, few studies have investigated the accuracy of the preoperative diagnosis for ER of local residual/recurrent cancer after CRT/RT. Therefore, this study aimed to identify the preoperative diagnostic factors associated with the complete endoscopic removal of local residual/recurrent cancer.
Methods
Study design and patients
This was a single-center, retrospective study. Using a prospectively maintained database, we identified esophageal cancerous lesions that were diagnosed as local residual/recurrent cancer after CRT/RT and treated by ER between January 2012 and December 2019. The inclusion criteria were as follows: (1) local residual/recurrent cancer after definitive CRT/RT clinically diagnosed as T1 by endoscopy and/or endoscopic ultrasonography (EUS) and (2) pathologically confirmed esophageal cancer using the resected specimen. Locally recurrent tumors were defined as lesions that recurred after the confirmation of complete response to CRT/RT at least once, whereas residual tumors were defined as lesions that did not disappear after CRT/RT. Lesions diagnosed as local recurrence after ER or photodynamic therapy (PDT) were excluded.
Pretreatment evaluation and treatment strategy
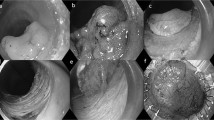
Before treatment, endoscopy was performed with white light imaging, narrow-band imaging, or blue laser imaging, as well as iodine staining. The location, macroscopic type (protrusion, excavation, unevenness, submucosal tumor-like appearance, and erosion), lesion size, and circumference of the lesion were evaluated. Protrusion was defined as the presence of an elevation of > 1 mm, whereas excavation was defined as the presence of a depression of > 1 mm. Lesions with protrusion, excavation, unevenness, submucosal tumor-like appearance, and erosion were defined as non-flat lesions. Representative images of these findings are presented in Fig. 1.
EUS was additionally performed for lesions with endoscopic findings suspicious for submucosal invasion by board-certified fellows of the Japan Gastroenterological Endoscopy Society with extensive experience in EUS of gastrointestinal tract tumors. EUS was mainly performed using a jelly-filled method with a 20-MHz miniature probe, and it typically demonstrated the esophageal wall as a nine-layered structure10. The cancer invasion depth and continuity of the fifth layer were evaluated using EUS (Fig. 2).
Computed tomography was usually performed for ESCC staging. ER was principally selected when ESCC was diagnosed as clinical N0M0.
ER was mainly performed for local residual/recurrent T1 cancer (mucosal or submucosal cancer). PDT was mainly performed for cancers diagnosed as suspicious for T2.
ER
ER was performed via endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD). EMR was performed using the transparent distal translucent cap method11. ESD was mainly performed using a HookKnife (Olympus, Tokyo, Japan) or FlushKnife BT (Fujifilm Medical, Tokyo, Japan). In most ESD procedures, the clip with line method was applied to gain good counter traction12.
Histological assessments
Resected specimens were fixed in 10% formalin and cut into 2-mm slices. After the specimens were embedded in paraffin, they were sliced into 3-μm-thick sections and stained with hematoxylin and eosin. Histological assessments were performed according to the Japanese Classification of Esophageal Cancer guidelines13. The invasion depth, horizontal depth, and vertical margin were evaluated histologically. R0 resection was defined as en bloc resection with negative margins. Endoscopic R0 resection was defined as endoscopic total removal of the lesion with a negative vertical margin. Endoscopic R1 resection was defined as resection that did not meet the criteria for endoscopic R0 resection.
Statistical analysis
All continuous variables are reported as the median (range), and all categorical variables are summarized as frequencies (percentages). Fisher’s exact test and the Mann–Whitney U test were used to compare clinical variables. P < 0.05 indicated statistical significance. All analyses were performed on a personal computer using the EZR software package, version 1.55 (Saitama Medical Center, Jichi Medical University, Tochigi, Japan)14.
Ethics approval
Waived informed consent was obtained from the ethics committee of Osaka International Cancer Institute. Instead of obtaining informed consent, all participants were provided opportunities to decline study participation prior to the present investigation using the opt-out method on the website of Osaka International Cancer Institute. The study protocol including opt-out consent was approved by the ethics committee of Osaka International Cancer Institute on March 4, 2022 (No. 21216). This retrospective study was performed in accordance with relevant guidelines and regulations.
Results
Patients and lesions
In total, 98 lesions (83 patients) were identified from our database. The characteristics of the patients and lesions are summarized in Table 1. For cancer before CRT/RT, the proportion of clinical T1 lesions was 67%. The radiation dose was unknown in one patient, but he was treated with a radiation dose exceeding 50 Gy as the primary therapy. Of the remaining 82 patients, 100%, 59% and 7% received chemotherapy with radiation doses of at least 50, 60, and 70 Gy, respectively. The chemotherapy regimen was unknown in 4 of 69 patients treated with CRT. Of the remaining 65 patients, 91%, 89% and 94% received chemotherapy with 5-FU, CDDP, and platinum agents including CDDP, respectively. For residual /recurrent cancer, the median tumor size was 12 mm (2–50), and 80% of tumors were recurrent lesions.
ER and histopathological assessments
The proportion of lesions treated with ESD was 72% (71/98 lesions). The en bloc and endoscopic R0 resection rates were 94% and 91%, respectively. The endoscopic R0 resection rate was not significantly different between ESD and EMR (89% versus 96%, P = 0.437). The adverse events included two cases of perforation and four cases of esophageal stricture requiring dilatation for symptoms. The characteristics of ER and histopathological assessments are summarized in Table 2. The comparison between flat lesions and non-flat lesions are summarized in Table 3.
Endoscopic R0 resection and endoscopic and EUS findings
The associations between endoscopic R0 resection and conventional endoscopic findings (e.g., elevation, excavation, unevenness, submucosal tumor like appearance, protuberance within the depression, and erosion) are presented in Table 4. Endoscopic R0 resection was significantly associated with elevation, an excavation submucosal tumor like-appearance, and non-flat lesions. The endoscopic R0 resection rates were 100% (59/59 lesions) for flat lesions and 77% (30/39 lesions) for non-flat lesions (P = 0.00014).
EUS was performed for 24 non-flat lesions, and the EUS findings of fifth layer were categorized into the following: uninterrupted (18 lesions), slurred (5 lesions), or ruptured (1 lesion). For lesions treated by CRT, the fifth layer was uninterrupted in 12 lesions, slurred in 3 lesions, and ruptured in 1 lesion. For lesions treated by RT, the fifth layer was uninterrupted in six lesions and slurred in two lesions. There was no significant association between the treatment regimen (CRT or RT) and continuity of fifth layer (P > 0.99). The associations between endoscopic R0 resection and EUS finding are presented in Table 4. There was a significant association between endoscopic R0 resection and the presence of an uninterrupted fifth layer (P = 0.0065). For tumors with an uninterrupted fifth layer, the endoscopic R0 resection rate was 94% (17/18 lesions).
Surveillance endoscopy and the local control status after ER
Of 83 patients, 25 were excluded from surveillance at our hospital, including 2 patients who underwent esophagectomy (one for a positive vertical margin on resected specimen and the other for residual disease confirmed immediately after ER) and 23 patients who underwent surveillance at a referral source hospital. In total, 71 lesions in 58 patients were subjected to surveillance endoscopy at our hospital. The median time from ER to the last endoscopy and median number of surveillance endoscopies were 51 months (6–126 months) and 11 (2–26), respectively. Local recurrence was observed in 12 patients (12 lesions). Six patients underwent additional ER, and five patients underwent ablation. One patient with a poor general condition did not receive additional treatment. One patient with re-recurrence after additional ER underwent esophagectomy.
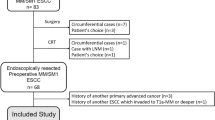
Proposed strategy of preoperative evaluation
Based on the results of this study, we have proposed a strategy for preoperative evaluation (Fig. 3). Flat lesions on conventional endoscopy, which had a 100% endoscopic R0 resection rate, are good candidates for ER. Lesions with an uninterrupted fifth layer on EUS are also good candidates for ER, as indicated by an endoscopic R0 resection rate of 94%.
Discussion
In this study, the endoscopic R0 resection rate for flat lesions on conventional endoscopy was 100% (59/59 lesions), and that for lesions with an uninterrupted fifth layer on EUS was 94% (17/18 lesions).
EUS is widely used to diagnose T stage ESCC15,16,17. Conversely, a recent multicenter prospective study revealed that additional EUS after conventional endoscopy did not improve the diagnostic accuracy regarding the invasion depth of T1 ESCC18. In the diagnosis of local recurrent cancer after CRT/RT, radiation-induced fibrosis can make an accurate diagnosis more difficult compared with that of ordinal esophageal cancer. However, the diagnostic accuracy concerning the cancer invasion depth is not important for the preoperative diagnosis of local recurrent cancer because additional esophagectomy is indicated mainly based on the completeness of the resection. Therefore, the preoperative assessment of resectability is more important than the assessment of the cancer invasion depth in cases of local recurrent cancer after CRT/RT. In this study, we evaluated interruption, slurring, or rupture of the fifth layer by EUS and found that endoscopic R0 resection was achieved in 94% (17/18) of lesions without interruption of the fifth layer, versus 33% (2/6) in lesions with a slurred or ruptured fifth layer. Therefore, EUS might be a useful modality for the preoperative assessment of local residual/recurrent cancer after CRT/RT.
Although the endoscopic R0 resection rate was 91% for all 98 lesions, the R0 resection rate was only 73%. Several possible causes can be considered. Prior CRT/RT can induce scaring and submucosal fibrosis, which makes ER difficult. Furthermore, in cases complicated by stricture induced by prior CRT/RT, a sufficient horizontal margin had to be sacrificed to avoid worsening of the stricture. However, the en bloc and R0 resection rates were comparable to those in previous reports7,8,19. Furthermore, the horizontal margin was not a risk factor for failure after ER in a previous study20. Therefore, ER can be curative as long as the endoscopically visible lesion is removed with a negative vertical margin.
PDT is a treatment option for local residual/recurrent cancer after CRT/RT, and it is indicated for T1–T2 lesions. Hatogai et al. reported 5-year local failure-free rates of 66.7% for EMR and 51.7% for PDT6. Because lesions treated by PDT included more advanced lesions (26.3% were T2 lesions), a strict comparison of efficacy between PDT and ER is difficult. In addition, ER and PDT have different characteristics. Specifically, PDT requires a special device for laser irradiation, and patients must avoid phototoxicity caused by the injection of a photosensitizer. Meanwhile, ER is a more common procedure, but it requires high skill for complete resection. Thus, further evaluation of ER is needed to clarify whether it has advantages over PDT in the treatment of local recurrent cancers after CRT/RT.
In this study, the 98 examined tumors consisted of 59 flat lesions, 39 non-flat lesions, and 18 lesions with an uninterrupted fifth layer. High endoscopic R0 resection rates were observed for flat lesions and lesions with an uninterrupted fifth later, whereas the endoscopic R0 resection rate was low for non-flat lesions. Although the number of each lesion type was not large, we considered that the numbers were acceptable to suggest an association between these findings and resectability. However, these results should be confirmed in a larger study. Moreover, salvage treatment following endoscopic R1 resection should be considered. Although esophagectomy is a highly curative treatment, it has high morbidity and mortality rates. The efficacy of other treatment options such as PDT should be evaluated along with no additional treatment.
Our study had several limitations. First, this was a single-center, retrospective study. Second, EUS was not performed before ER for all non-flat lesions. Third, lesions treated by PDT or esophagectomy were excluded. However, there are ethical concerns for performing ER when the lesion is difficult to completely resect by ESD or EMR or when patients refuse to undergo ER. Fourth, lymph node or organ metastases after ER and long-term outcomes were not evaluated in this study. However, the main aim of this study was to identify endoscopic and EUS findings associated with the complete endoscopic removal of local residual/recurrent cancer.
In conclusion, regarding the treatment for local residual/recurrent cancer after CRT/RT, flat lesions on conventional endoscopy and lesions with an uninterrupted fifth layer on EUS are good candidates for ER.
Data availability
The dataset analyzed during this study are not publicly available because of individual privacy. They are available from the corresponding author on reasonable request.
References
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424. https://doi.org/10.3322/caac.21492 (2018).
Rustgi, A. K. & El-Serag, H. B. Esophageal carcinoma. N. Engl. J. Med. 371, 2499–2509. https://doi.org/10.1056/NEJMra1314530 (2014).
Kato, H. et al. A phase II trial of chemoradiotherapy for stage I esophageal squamous cell carcinoma: Japan Clinical Oncology Group Study (JCOG9708). Jpn. J. Clin. Oncol. 39, 638–643. https://doi.org/10.1093/jjco/hyp069 (2009).
Taniyama, Y. et al. Different strategy of salvage esophagectomy between residual and recurrent esophageal cancer after definitive chemoradiotherapy. J. Thorac. Dis. 10, 1554–1562. https://doi.org/10.21037/jtd.2018.03.04 (2018).
Sugawara, K. et al. Association of preoperative inflammation-based prognostic score with survival in patients undergoing salvage esophagectomy. Dis. Esophagus 32, 258. https://doi.org/10.1093/dote/doy066 (2019).
Hatogai, K. et al. Local efficacy and survival outcome of salvage endoscopic therapy for local recurrent lesions after definitive chemoradiotherapy for esophageal cancer. Radiat. Oncol. 11, 31. https://doi.org/10.1186/s13014-016-0604-z (2016).
Ego, M. et al. Long-term outcomes of patients with recurrent squamous cell carcinoma of the esophagus undergoing salvage endoscopic resection after definitive chemoradiotherapy. Surg. Endosc. 35, 1766–1776. https://doi.org/10.1007/s00464-020-07571-y (2021).
Kondo, S. et al. Prognostic factors for salvage endoscopic resection for esophageal squamous cell carcinoma after chemoradiotherapy or radiotherapy alone. Endosc. Int. Open 4, E841-848. https://doi.org/10.1055/s-0042-109609 (2016).
Ishihara, R. et al. Local recurrence of large squamous-cell carcinoma of the esophagus after endoscopic resection. Gastrointest. Endosc. 67, 799–804. https://doi.org/10.1016/j.gie.2007.08.018 (2008).
Esaki, M. et al. Probe EUS for the diagnosis of invasion depth in superficial esophageal cancer: A comparison between a jelly-filled method and a water-filled balloon method. Gastrointest. Endosc. 63, 389–395. https://doi.org/10.1016/j.gie.2005.10.027 (2006).
Inoue, H. et al. Endoscopic mucosal resection with a cap-fitted panendoscope for esophagus, stomach, and colon mucosal lesions. Gastrointest. Endosc. 39, 58–62 (1993).
Oyama, T. Counter traction makes endoscopic submucosal dissection easier. Clin. Endosc. 45, 375–378. https://doi.org/10.5946/ce.2012.45.4.375 (2012).
Japan Esophageal, S. Japanese classification of esophageal cancer, 11th edition: Part I. Esophagus 14, 1–36. https://doi.org/10.1007/s10388-016-0551-7 (2017).
Kanda, Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48, 452–458. https://doi.org/10.1038/bmt.2012.244 (2013).
He, L. J. et al. Endoscopic ultrasonography for staging of T1a and T1b esophageal squamous cell carcinoma. World J. Gastroenterol. 20, 1340–1347. https://doi.org/10.3748/wjg.v20.i5.1340 (2014).
Kitagawa, Y. et al. Esophageal cancer practice guidelines 2017 edited by the Japan Esophageal Society: Part 1. Esophagus 16, 1–24. https://doi.org/10.1007/s10388-018-0641-9 (2019).
Park, C. H. et al. Clinical practice guideline for endoscopic resection of early gastrointestinal cancer. Clin. Endosc. 53, 142–166. https://doi.org/10.5946/ce.2020.032 (2020).
Ishihara, R. et al. Assessment of the diagnostic performance of endoscopic ultrasonography after conventional endoscopy for the evaluation of esophageal squamous cell carcinoma invasion depth. JAMA Netw. Open 4, 317. https://doi.org/10.1001/jamanetworkopen.2021.25317 (2021).
Hombu, T. et al. Salvage endoscopic resection (ER) after chemoradiotherapy for esophageal squamous cell carcinoma: What are the risk factors for recurrence after salvage ER?. Dig. Endosc. 30, 338–346. https://doi.org/10.1111/den.12984 (2018).
Fukuda, H. et al. Effect of horizontal margin status and risk of local recurrence after endoscopic submucosal dissection for superficial esophageal cancer. JGH Open 4, 160–165. https://doi.org/10.1002/jgh3.12233 (2020).
Acknowledgements
We thank Joe Barber Jr., PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
Y. T.: conception and design, drafting article, analysis of data, and final approval of the article. R. I.: conception and design, critical revision of the article for important intellectual content, and final approval of the article. N. M., Y. O., Y. K., H. S., T. N., K. M., M. M., S. S., A. M., T. K., S. Y., Y. T., K. H., N. U., T. M.: data collection and final approval of the article.
Corresponding author
Ethics declarations
Competing interests
Satoki Shichijo has received personal fees from Olympus Corporation, Boston Scientific Japan, Daiichi-Sankyo, EA Pharma, AstraZeneca, AI Medical Service Inc, Jannsen Pharmaceutical and Japanese Society of Gastroenterology. Takashi Kanesaka has received personal fees from Olympus Corporation. Yoji Takeuchi has received personal fees from Olympus Corporation, Boston Scientific Japan, FUJIFILM Medical Co., Ltd, Daiichi-Sankyo, Miyarisan Pharmaceutical, Asuka Pharmaceutical, AstraZeneca, EA Pharma, Zeria Pharmaceutical, Kaneka Medix and Kyorin Pharmaceutical. Noriya Uedo has received personal fees from Olympus Corporation, Boston Scientific Japan, FUJIFILM Medical Co., Ltd, Daiichi-Sankyo, Takeda Pharmaceutical, EA Pharma, Otsuka Pharmaceutical, AstraZeneca and Miyarisan Pharmaceutical. Ryu Ishihara has received personal fees from Olympus Corporation, FUJIFILM Medical Co., Ltd, Daiichi-Sankyo, Ono Pharmaceutical, EA Pharma and AstraZeneca. Other authors have no financial relationships to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tani, Y., Ishihara, R., Matsuura, N. et al. Endoscopic resection for local residual or recurrent cancer after definitive chemoradiotherapy or radiotherapy for esophageal squamous cell carcinoma. Sci Rep 13, 10451 (2023). https://doi.org/10.1038/s41598-023-32667-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-32667-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.