Abstract
Population-based estimates of pathogenic variation burden in gynecologic cancer predisposition genes are a prerequisite for the development of effective precision public health strategies. This study aims to reveal the burden of pathogenic variants in a comprehensive set of clinically relevant breast, ovarian, and endometrial cancer genes in a large population-based study. We performed a rigorous manual classification procedure to identify pathogenic variants in a panel of 17 gynecologic cancer predisposition genes in a cohort of 7091 individuals, representing 0.35% of the general population. The population burden of pathogenic variants in hereditary gynecologic cancer-related genes in our study was 2.14%. Pathogenic variants in genes ATM, BRCA1, and CDH1 are significantly enriched and the burden of pathogenic variants in CHEK2 is decreased in our population compared to the control population. We have identified a high burden of pathogenic variants in several gynecologic cancer-related genes in the Slovenian population, most importantly in the BRCA1 gene.
Similar content being viewed by others
Introduction
Hereditary gynecologic cancers include breast, ovarian, and endometrial cancer, as well as some other rare cancers of the female reproductive system1, where a pathogenic variant, leading to a distinctly increased lifetime risk of cancer development, has been discovered in a cancer-related gene2. Altogether, pathogenic variants in gynecologic cancer predisposition genes account for 5–10% of breast, ovarian, and endometrial cancer3,4 with carriers of pathogenic variants in these genes having a significantly increased lifetime risk for developing cancer (up to 72%)5. However, the burden of hereditary gynecologic cancer has not been established in the general population6, since the disease is characterized by both late-onset and incomplete penetrance7.
Furthermore, genomic data varies between populations, even between different European populations17. For instance, it has been shown that genetic testing in Slovenian patients with breast and ovarian cancer consistently yields very high BRCA1 and BRCA2 detection rates compared to patients from other populations8. It is imperative that population-specific studies are conducted to gain insight into the genetic diversity of pathogenic findings in specific populations.
Public health genomics is a field, concerned with the assessment of the health characteristics of a particular population by evaluating the impact of genetic risk factors on the population’s health status as well as disease burden9,10,11. By determining the genetic risk factors burden, such as pathogenic variation in genes in a population-based study, we are able to evaluate the likelihood of pathogenic findings in the general population12, which can be used to develop precision medicine-based population health strategies, such as population-specific disease prevention, screening, and surveillance10. Hereditary cancers, specifically hereditary gynecologic cancers, have been noted as a priority in public health genomics11.
A few studies focused on the burden of pathogenic and likely pathogenic variants in genes associated with different cancer syndromes in unaffected individuals in population-based cohorts, namely analyzing large international control databases13,14, population-based biobanks15, or individuals who underwent exome sequencing for other conditions16,17. The burden of pathogenic variation in unaffected individuals has been determined in the control cancer-free population in case–control studies as well6,18,19,20. A wide prevalence range of pathogenic variants in unaffected individuals was reported in these studies (from 0.5 to 4.8%), depending on the methodology and the number of genes analyzed17,20. Yet, only a few previous studies have examined the population burden of gynecologic cancer predisposition genes beyond BRCA1/2 and Lynch syndrome genes in national cohorts18,19,21.
Several genes have previously been associated with gynecologic cancer development7 and even more are currently being evaluated as candidate gynecologic cancer predisposition genes22. Professional organizations have published screening and/or treatment guidelines for carriers of pathogenic variants in only a limited number of genes, with strong evidence for cancer predisposition7, making them clinically significant, as they present actionable information to patients. Discoveries in the dynamic field of cancer research are published daily and thus making a panel of clinically significant genes a moving target; however, leading professional organizations have published lists of genes that they deem clinically significant7,23,24. There is a lack of large-scale population-based studies providing assessments of pathogenic variants burden in a comprehensive panel of clinically significant breast, ovarian and endometrial cancer predisposition genes in the general population6.
To develop precision population health strategies, this study aims to assess the population burden of germline pathogenic variants in clinically actionable gynecologic cancer predisposition genes in the Slovenian general population, consequently estimating the burden of individuals with hereditary cancer syndromes on a population level.
Methods
Ethical approval
All experimental protocols were approved by the Medical Ethics Committee of the Republic of Slovenia (0120-170/2022/03).
Study population
We investigated cancer variants in exome datasets of 7091 individuals who were referred to the Clinical Institute of Genomic Medicine, University Medical Centre, Ljubljana, Slovenia from July 2014 to May 2022 for exome sequencing for various rare genetic conditions other than cancer. This data is stored in the Slovenian genomic database. All patients gave informed consent for participation and all methods were performed in accordance with the Declaration of Helsinki. The patient data were non-reciprocally de-identified identified and aggregated data on variant frequencies was assessed. GnomAD non-cancer population was chosen as a control for our study (N = 134,187).
Sequencing and variant calling
The samples for exome sequencing were enriched using TruSight One, TruSight Exome, and Nextera Coding Exome capture kits by Illumina or Agilent SureSelect Human All Exon v2 and Agilent SureSelect Human All Exon v5 capture kits by Agilent Technologies. Sequencing was performed on Illumina MiSeq or Illumina HiSeq 2500 platforms. A minimum median exome coverage was 60x, with over 95% of targets covered with at least 10 × sequencing depth. Raw sequence files were processed using a custom exome analysis pipeline and aligned to UCSC hg19 human reference genome as previously described by our group25.
Gene panel
We constructed an innovative gene panel containing genes associated with gynecologic cancer. Several professional resources were examined for gynecologic cancer-related genes: NCCN guidelines for hereditary breast and ovarian cancer7, Genomics England PanelApp panels for gynecologic cancers23, and ClinGen’s expert panel recommendations24. Only genes with definite associations and available clinical recommendations were included in our gene panel: PanelApp’s green list (15 genes), NCCN’s strong evidence level (16 genes), and definite association by ClinGen’s expert panels (17 genes). Genes defined as having a strong connection by multiple of those sources were included in our panel. We were able to construct an innovative gene panel encompassing 17 genes causative of breast, ovarian, and/or endometrial cancer (Table 1). The presence of pathogenic variants in this panel of 17 gynecologic cancer-related genes has not been analyzed in an unaffected population before.
Variant filtering
The variant filtering process was based on both effect (functional effect, clinical impact) and frequency of the variants in control populations, where found variants had to satisfy both types of criteria to be included.
Firstly, the functional effect was assessed. The criterion for inclusion was either for the variant to have a moderate or high impact on protein function (inframe insertion/deletion, frameshift, missense, canonical splice site variant, stop/start loss, stop gain, UTR region deletion) or to have a high effect on protein splicing (> 0.5 SNV rf or ada score)26. Secondly, the variant’s frequency in control populations (gnomAD and our whole dataset) was evaluated. Variants were excluded from further evaluation for appearing in > 10 heterozygotes in the gnomAD population or > 20 individuals in our dataset and for being present in more than three individuals in the homozygous state in gnomAD or our dataset.
The remaining variants were filtered based on their ClinVar classification. Variants classified as benign and likely benign or conflicting between benign/likely benign and a variant of uncertain significance in the ClinVar database were excluded from further analysis. Furthermore, variants in noncoding regions and synonymous variants not predicted to affect splicing that were not present in ClinVar or were classified as VUS in ClinVar were excluded as well.
The only exception was known pathogenic variants (as evaluated by multiple unanimous submissions in ClinVar database27), where the effect and frequency filtering criteria were not enforced.
All remaining variants were evaluated using the ACMG guidelines28 and classified as a pathogenic, likely pathogenic, variant of uncertain significance, likely benign, or benign.
Overview of variant classification
ACMG criteria28 were applied to the filtered variants for annotation and classification of genetic variants based on population frequency, functional effects of variants, published research, and more. We have considered population frequency, as it is recorded in GnomAD v.2.1.129 (for criteria PS4, PM2_SUP, BA1, BS1) (accessed 5th of May 2022). PM2 was used as a supporting criterion PM2_SUP30. The benign frequency cut-off was adopted from Varsome calculations31 (BS1) (accessed 14th of March 2022). The loss of function variants were classified according to ClinGen’s algorithm32. The PVS1 criterion was considered for loss of function variants, appearing in genes, fulfilling ClinGen’s criteria for haploinsufficiency. Null variants in coding exons before the last 50 nucleotides of the penultimate exon and variants where known pathogenic variants were appearing downstream of the said variant, were predicted to undergo nonsense-mediated decay. A variant was considered to affect a biologically relevant transcript if it was present in an exon with a pext score of > 0.5 (sourced from gnomAD). In variants, appearing in canonical splice sites, disruption of the reading frame was assessed. Z-scores were collected from gnomAD and missense variants in genes, for which z-score exceeded 3.0933 were assigned PP2 criteria. ClinVar27 was used for the identification of known pathogenic variants (for criteria PS1 and PM5). We have used an agreement of multiple predictive in silico tools as a measurement of the pathogenicity of the variants (PP3, BP4). Conservation was assessed using PhastCons34 and splice sites were identified based on Human Splicing Finder 3.135 (BP7). Prevalence of variants in cases vs controls and previous records in patients (PS4), functional studies (PS3, BS3), and previous accounts of variant segregation (PP1, BS4) were extracted from the literature. PS4 criterion was used according to ClinGen’s guidelines36. PS4_STR was assigned to variants, appearing in > 0.001% of the gnomAD population, for which case–control studies reported OR > 5. Extremely rare variants (< 0.001% of the gnomAD population) were divided into three categories: PS4_STR, PS4_MOD, and PS4_SUP, according to the number of patients with variant previously reported: > 4 STR, > 2 MOD, > 1SUP36. Data regarding repeat regions were extracted from RepeatMasker via UCSC Genome Browser37 (PM4, BP3). Data on functional domains were extracted from UniProt38 (PM1). Criteria PP5 and BP6 were not used because of recent recommendations against their use39. This work was performed on data without identifiers or phenotypes, so genotype–phenotype correlations were not possible and criteria PS2, PM3, PM6, PP4, BP2, and BP5 were not applied. Specific classification criteria by ClinGen were used to classify variants in the ATM gene40. For the PMS2 gene, only variants, appearing in the non-homologous regions of the PMS2 gene, as assessed by Alignability of 100mers by GEM (via UCSC Browser) were considered. Rules for combining criteria for the classification of variants were adopted from ACMG guidelines28 with amendments by classification modeling guidelines by Tavtigian et al.41. Most importantly, variants with a very strong and a moderate criterion were classified as pathogenic and variants with two strong criteria were classified as likely pathogenic. Variants with PVS1 and PM2_SUP criteria only were classified as likely pathogenic according to ClinGen’s recommendation30.
Statistical analysis
The differences between the burden of pathogenic variants in the study and control populations were calculated by Chi-squared test (χ2 test), with two-tailed analysis. We considered p < 0.05 as statistically significant. Odds ratios (OR) at the 95% confidence interval for each gene were calculated as well.
Ethics declaration
All patients gave informed consent for participation and all methods were performed in accordance with the Declaration of Helsinki. All data was de-identified.
Results
Variant filtering and classification
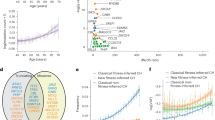
Altogether, 649 rare and functional variants in 17 genes were found in our study population of 7091 exomes. After the variant filtering process resulted in 603 variants, manual classification was employed and 74 unique pathogenic and likely pathogenic variants in 13 cancer genes were found, appearing one or more times in the Slovenian genomic database (Fig. 1). No pathogenic/likely pathogenic variants were found in four of the investigated genes.
Variant filtering and classification process. Amidst 694 rare and functional or known pathogenic variants found in our population, 107 variants were classified as benign (B), likely benign (LB), or a variant of uncertain significance (VUS) during the filtering process (filtered variants). Firstly, 82 variants were classified as B, LB, or conflicting between B, BL, and VUS based on their ClinVar classification. Next, variants in noncoding regions and synonymous variants that were not present in ClinVar or were classified as VUS in ClinVar were assigned VUS status (21 variants). We added 12 variants to the classification group since they are known pathogenic variants, frequent in control populations and cancer patients. The resulting 603 variants were classified manually according to the American College of Medical Genetics and Genomics and the Association for Molecular Pathology (ACMG) standards and guidelines for the interpretation of sequence variants (ACMG guidelines). We classified 603 variants into five categories: pathogenic (P), likely pathogenic (LP), variant of uncertain significance, and likely benign or benign. Six variants were classified as benign, 127 were likely benign, 396 were VUS, of which ten were conflicting between B/LB and P/LP and there was not enough data to classify the remaining 381 variants into either B/LB or P/LP categories. Lastly, 14 variants were likely pathogenic and 60 were classified as pathogenic.
The burden of (likely) pathogenic variants in our study population and control population
The burden of likely pathogenic and pathogenic variants in our cohort was 2.14%, 152 heterozygotes were found to carry a pathogenic or likely pathogenic variant in a gene linked to gynecologic cancer. The most frequently found variants were in BRCA1 and BRCA2 genes, present in 0.40% and 0.25% of the studied population, respectively. Heterozygous (likely) pathogenic variants in ATM were present in 0.51% of our population. CHEK2 had a variant prevalence of 0.31%. Variants in mismatch repair (MMR) genes, associated with Lynch syndrome (MLH1, MSH2, MSH6, and PMS2 genes) were present in 20 heterozygotes (10 in PMS2) and altogether appeared in 0.28% of the studied population. Pathogenic variants in RAD51C and PALB2 were present in 0.13% of our cohort, pathogenic variants in BARD1 were present in 0.06% of heterozygotes and pathogenic variants in BRIP1 and CDH1 had a prevalence of 0.04% (Table 2).
Chi-squared test with two-tailed analysis was used and odds ratios were calculated to enable a comparison of Slovenian population frequencies of pathogenic variants to control the population of the gnomAD database (Table 2). The Slovenian population was statistically significantly (p < 0.05) enriched for pathogenic variants in ATM, BRCA1, and CDH1 genes when compared to the gnomAD non-cancer control population. Pathogenic variants in CHEK2 had a lower prevalence in the Slovenian population when compared to the control population, mainly due to the low prevalence of the c.1100del variant in the Slovenian population; its prevalence is five times higher in the control population (0.04% vs 0.21%). A statistically significant difference could not be established for the other genes from our study.
Description of likely pathogenic and pathogenic variants in our study
We have identified 74 distinct pathogenic and likely pathogenic variants in our study population in the following 13 cancer-related genes: ATM, BARD1, BRCA1, BRCA2, BRIP1, CDH1, CHEK2, MLH1, MSH2, MSH6, PALB2, PMS2, in RAD51C (Supplementary Table S1).
Pathogenic and likely pathogenic variants in BRCA1 and BRCA2 genes were present in 0.65% of our population. The most common pathogenic variants in BRCA genes in our cohort were c.5266dupC, c.181T>G, and c. 1687C>T in the BRCA1 gene and c.3975_3978dupTGCT and c.7806-2A>G in the BRCA2 gene, which have been previously reported to be the five most common pathogenic variants in BRCA1/2 genes in Slovenian HBOC families, representing 67% of pathogenic variants in Slovenian cancer patients42; together, they represent 71% of the pathogenic variation in BRCA genes in our study. The most frequent variant in our population is c.5266dupC in BRCA1, which is the one most common pathogenic BRCA1 variants worldwide43. The most common variant in BRCA2 is c.7806-2A>G, a Slovenian founder variant44. Two BRCA1 variants, previously not described in the Slovenian population, are c.3331_3334delCAAG and c.4065_4068delTCAA, which have been identified in other populations in breast and ovarian cancer patients45,46. Two BRCA2 variants, 1813delA, and c.8755-1G>A have not been described in the Slovenian population yet, but have been previously described in other populations47,48.
ATM represents the most frequently mutated gene in our population (likely pathogenic/ pathogenic variants were present in 0.51% of the cohort). Most of the variants are known pathogenic variants, however, three of the found variants (c.2007T>A, c.7452_7453delAT, and c.8708delC) were previously unreported in scientific literature and were classified as likely pathogenic based on their loss of function effect (frameshift and stop gained) and absence in the control population of gnomAD project. Variants in MMR genes (MLH1, MSH2, MSH6, and PMS2) were found in 20 heterozygotes and together appeared in 0.28% of the studied population. These variants are known pathogenic variants, described in many populations worldwide in patients with Lynch-related cancers49,50,51. Eight different pathogenic and likely pathogenic variants were found in the CHEK2 gene in our study, representing 0.31% of our cohort. This is statistically significantly lower than the prevalence in the control database (p < 0.05). Three of the found variants, c.444+1G>A, c.1100del, and c.349A>G, were previously described in the Slovenian population amongst the most frequent CHEK2 pathogenic variants in Slovenian CHEK2 positive breast cancer patients52. Pathogenic variants in RAD51C and PALB2 were present in 0.13% of our cohort. Pathogenic variants in CDH1 had a prevalence of 0.04% in our cohort, a substantial enrichment in comparison to the gnomAD population (p < 0.05). The cumulative prevalence of pathogenic variants in BARD1 was 0.06% and in the BRIP1 gene it was 0.04%; among those, BARD1 variants c.1381G>T and c.1538T>G, and BRIP1 variants c.318delT and c.368C>A, had never been described in scientific literature or databases; yet their loss of function effect and absence from control populations led to the classification as (likely) pathogenic. No pathogenic and likely pathogenic variants were detected in our study population for RAD51D, STK11, PTEN, or TP53.
Discussion
The population burden of pathogenic variants in hereditary gynecologic cancer-related genes in Slovenia is 2.14%, according to our study. The estimation is based on an analysis of pathogenic variants in 17 clinically significant gynecologic cancer predisposition genes, in a population-based cohort of 7091 unaffected individuals, representing 0.35% of the Slovenian population. Further analysis revealed that our population is enriched for pathogenic variants in ATM, BRCA1, and CDH1 genes and that prevalence of pathogenic variants in the CHEK2 gene is lower in the Slovenian population, when compared to GnomAD non-cancer control population. This estimate presents the first report of the burden of population burden of pathogenic variants associated with any disease in Slovenia one of the first to show the burden of gynecologic cancer-related pathogenic variants on a population level and as such warrants both scientific and clinical attention.
In the Slovenian general population, the highest burden of (likely) pathogenic variants was found in the BRCA1 and BRCA2 genes, 0.65%, with 0.40% in BRCA1 and 0.25% in BRCA2. Until recently, the prevalence of pathogenic variants in BRCA genes in the general population has been estimated to be between 1:300 and 1:500 (0.2–0.3%)53. However, based on population studies, this fact has recently been challenged. An early study on exomes of 60.706 individuals from the ExAC project has shown that the burden of pathogenic variants BRCA genes is closer to 1:161 (0.62%)14, and several recent studies have reported higher than before thought burden of pathogenic variants in the different cancer-free cohorts15,54,55. Our results support the claim that the burden of BRCA pathogenic variants in the unaffected population might be higher than traditionally estimated. Furthermore, we report two unique features of the Slovenian population: a high prevalence of pathogenic variants in the BRCA1 gene compared to the control population, which is reflected in high detection rates of pathogenic variants in BRCA genes in Slovenian HBOC patients as well8 and a higher burden of pathogenic BRCA1 variants compared to BRCA2 pathogenic variants in the Slovenian population. In most populations, the BRCA2 pathogenic variants prevail6, however, a higher burden of BRCA1 pathogenic variants has been previously described in cancer patient populations from a few eastern and central European countries56.
A high burden of several other cancer-predisposing genes was reported in our study. Pathogenic or likely pathogenic variants in the ATM gene are the most frequent (0.51%) and compared to that of gnomAD, the prevalence of ATM (likely) pathogenic variants in the Slovenian population is significantly increased (p = 0.00143). Pathogenic variants in MMR genes (MLH1, MSH2, MSH6, and PMS2), that are involved in the development of Lynch syndrome are present in 0.28% of our study population. Compared to other populations (0.18% in a recent large study in the Chinese population57), the percentage is high and is close to that of BRCA1/2, and ATM pathogenic variants. The distribution of pathogenic variants among MMR genes in our study seems remarkable: 50% of variants were found in PMS2, 25% in MSH6, and 15% in MLH1 and 10% in MSH2, as it is not reflective of the distribution of pathogenic variants in MMR genes in cancer populations, where up to 90% of variants are found in MLH1 and MSH2 genes58. The high burden of PMS2 variants may be explained by some recent findings and general facts: firstly, PMS2 pathogenic variants have low penetrance as discovered in a recent study59; secondly, a significant part of the pathogenic variation in MMR genes is due to large-scale deletions60, and this variation, not included in our analysis, might contribute to the redistribution of pathogenicity among the MMR genes; and finally, Lynch syndrome is grossly underdiagnosed61, leaving MSH2 and PMS2 pathogenic variant carriers frequently unidentified62, therefore, current studies of pathogenic variants distribution in recognized Lynch syndrome patients may not reflect the true distribution either in the patient group or in the general population. The burden of pathogenic variants in the CHEK2 gene is statistically significantly decreased in the Slovenian population compared to the gnomAD population (p = 0.0043), mostly due to the low prevalence of the c.1100del variant in our population. This variant is very common in Northern and Western European populations63 and these populations are the main component of the gnomAD cohort29, explaining the high prevalence in the gnomAD population. Moreover, this variant has been rarely found in Southern European and non-European populations64,65. Our study supports the claim, that the prevalence of this variant is less frequent outside of the Northern European populations. Seven previously unreported likely pathogenic variants in four gynecologic cancer genes (ATM, BARD1, and BRIP1) were found in the Slovenian genomic database40. In light of the fact that these variants were discovered in our apparently non-cancer-affected population, additional functional studies will be required to demonstrate their pathogenic effect. We have not discovered any pathogenic variants in RAD51D, STK11, PTEN, and TP53 genes in our non-cancer affected study population of 7091 participants; this is not surprising since most of these genes had none to a very low pathogenic variant prevalence in control populations in previous studies66.
While several studies were undertaken to reveal the carrier rate of cancer pathogenic variants in unaffected populations6,15,16, ours is the first study to evaluate this particular panel of clinically significant gynecologic cancer-related genes in a general population, therefore, making the comparability of the burden in our population (2.14%) challenging. A recent study in a Swiss population has analyzed the prevalence of pathogenic variants in a panel of breast and ovarian cancer genes in a non-cancer cohort16. The study enrolled only 400 non-cancer cases undergoing exome sequencing and included 19 genes, having 16 genes coinciding with our study. The prevalence of pathogenic variants in this unaffected population (2.2%) is similar to our study. Another study included a large sample of 32.544 unaffected women as controls and reported the prevalence of pathogenic variants in 12 breast-cancer-related genes (11 the same as in our study) to be 1.63%6, which is a reasonably similar result considering the lower number of genes included. The differences between studies may be partially explained by differences in the methodological approach, most importantly in gene selection and classification methodology, different sample sizes of the previous studies, as well as unique population characteristics such as the presence of Slovenian founder BRCA2 variant in our study44 and high burden of BRCA1 pathogenic variants in the Slovenian population8.
Our work is notable for the large cohort size, a manual review of variants using the ACMG standards for interpretation28, and an exclusive focus on the gynecologic cancer genes. There are, however, some limitations to our study design. The anonymization of our study disabled the use of patient phenotypes and family history in the classification of the variants. As a result, it is possible that some of the patients who underwent exome sequencing at our institution for non-cancer Mendelian disorders may harbor a personal or family history of cancer, in addition to the primary reason for their genetic analysis. Family history of cancer in carriers and potential additional segregation analysis might allow some variants to be upgraded. Secondly, our analysis does not include copy number variation analysis or methylation analysis, as some of this variation may be significant in cancer predisposition risk, therefore, prevalence calculations might be slightly underestimated. Nevertheless, even without considering this additional variation, an important number of unaffected individuals in our study have been found to be carriers of a pathogenic variant in a gynecologic cancer predisposition gene.
This study provides an assessment of the burden of pathogenic variation in a panel of clinically significant hereditary gynecologic cancer genes in a general population. Understanding the population burden of hereditary gynecologic cancer will ultimately lead to the development and implementation of precision public health strategies in a sector of hereditary gynecologic cancer and is expected to help bridge the gap between an individual and the population’s health in public health genomics. Our dataset of unaffected individuals has a high number of carriers of pathogenic variants of several clinically actionable genes, especially BRCA1, and this presents an opportunity to discuss population or opportunistic genomic screening67, a strategy that has been often suggested as a cost-effective tool to discover pre-symptomatic carriers68.
In conclusion, we report a population burden of 2.14% of the pathogenic variation in clinically actionable gynecologic cancer-related genes in a large non-cancer population in a Slovenian population-based study.
Data availability
The datasets generated and/or analyzed during the current study are available in the ClinVar repository (accession numbers SCV002762771 to SCV002762841).
References
Neto, N. & Cunha, T. M. Do hereditary syndrome-related gynecologic cancers have any specific features?. Insights Imaging 6, 545–552 (2015).
Pruthi, S., Gostout, B. S. & Lindor, N. M. Identification and management of women with BRCA mutations or hereditary predisposition for breast and ovarian cancer. Mayo Clin. Proc. 85, 1111–1120 (2010).
Angeli, D., Salvi, S. & Tedaldi, G. Genetic predisposition to breast and ovarian cancers: How many and which genes to test?. Int. J. Mol. Sci. 21, 1128 (2020).
Lu, K. H. Hereditary gynecologic cancers: Differential diagnosis, surveillance, management and surgical prophylaxis. Fam. Cancer 7, 53–58 (2008).
Kuchenbaecker, K. B. et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA 317, 2402–2416 (2017).
Hu, C. et al. A population-based study of genes previously implicated in breast cancer. N. Engl. J. Med. 384, 440–451 (2021).
Daly, M. B. et al. NCCN guidelines version 2.2021 genetic/familial high-risk assessment: Breast, ovarian, and pancreatic. J. Natl. Comprehensive Cancer Netw. 6, 77–102 (2021).
Blatnik, A. et al. Prevalence of BRCA1/2 pathogenic variants in triple negative breast cancer patients stratified according to age at diagnosis. J. Clin. Oncol. 38, e13677–e13677 (2020).
Green, R. F. et al. Evaluating the role of public health in implementation of genomics-related recommendations: A case study of hereditary cancers using the CDC Science Impact Framework. Genet. Med. 21, 28–37 (2019).
Molster, C. M. et al. The evolution of public health genomics: Exploring its past, present, and future. Front Public Health 6, (2018).
Khoury, M. J. et al. From public health genomics to precision public health: A 20-year journey. Genet. Med. 20, 574–582 (2018).
Yamaguchi-Kabata, Y. et al. Evaluation of reported pathogenic variants and their frequencies in a Japanese population based on a whole-genome reference panel of 2049 individuals article. J. Hum. Genet. 63, 213–230 (2018).
de Andrade, K. C. et al. Variable population prevalence estimates of germline TP53 variants: A gnomAD-based analysis. Hum. Mutat. 40, 97–105 (2019).
Maxwell, K. N., Domchek, S. M., Nathanson, K. L. & Robson, M. E. Population frequency of germline BRCA1/2 mutations. J. Clin. Oncol. 34, 4183–4185 (2016).
Abul-Husn, N. S. et al. Exome sequencing reveals a high prevalence of BRCA1 and BRCA2 founder variants in a diverse population-based biobank. Genome Med. 12, (2019).
Kraemer, D. et al. Prevalence of genetic susceptibility for breast and ovarian cancer in a non-cancer related study population: Secondary germline findings from a Swiss single centre cohort. Swiss Med .Wkly 149, (2019).
Chirita-Emandi, A. et al. Challenges in reporting pathogenic/potentially pathogenic variants in 94 cancer predisposing genes—in pediatric patients screened with NGS panels. Sci. Rep. 10, 223 (2020).
Fujita, M. et al. Population-based Screening for Hereditary Colorectal Cancer Variants in Japan. Clin. Gastroenterol. Hepatol. 20, 2132–2141 (2020).
Momozawa, Y. et al. Germline pathogenic variants of 11 breast cancer genes in 7,051 Japanese patients and 11,241 controls. Nat. Commun. 9, 4–6 (2018).
Petridis, C. et al. Frequency of pathogenic germline variants in BRCA1, BRCA2, PALB2, CHEK2 and TP53 in ductal carcinoma in situ diagnosed in women under the age of 50 years. Breast Cancer Res. 21, 53 (2019).
Southey, M. C. et al. Population-based estimates of breast cancer risk for carriers of pathogenic variants identified by gene-panel testing. NPJ Breast Cancer 7, 153 (2021).
Milne, R. L. et al. Identification of ten variants associated with risk of estrogen-receptor-negative breast cancer. Nat. Genet. 49, 1767–1778 (2017).
Martin, A. R. et al. PanelApp crowdsources expert knowledge to establish consensus diagnostic gene panels. Nat. Genet. 51, 1560–1565 (2019).
Rehm, H. L. et al. ClinGen-the clinical genome resource. N. Engl. J. Med. 372, 2235–2242 (2015).
Maver, A. et al. Phenotype-driven gene target definition in clinical genome-wide sequencing data interpretation. Genet. Med. 18, 1102–1110 (2016).
Jian, X., Boerwinkle, E. & Liu, X. In silico prediction of splice-altering single nucleotide variants in the human genome. Nucleic Acids Res. 42, 13534–13544 (2014).
Landrum, M. J. et al. ClinVar: Public archive of relationships among sequence variation and human phenotype. Nucleic Acids Res. 42, 980–985 (2014).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 17, 405–424 (2015).
Karczewski, K. J. et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 581, 434–443 (2020).
Clinical Genome Resource. SVI Recommendation for Absence/Rarity (PM2) - Version 1.0. https://clinicalgenome.org/site/assets/files/5182/pm2_-_svi_recommendation_-_approved_sept2020.pdf (2020).
Kopanos, C. et al. VarSome: The human genomic variant search engine. Bioinformatics 35, 1978–1980 (2019).
Abou Tayoun, A. N. et al. Recommendations for interpreting the loss of function PVS1 ACMG/AMP variant criterion. Hum. Mutat0 39, 1517–1524 (2018).
Samocha, K. E. et al. A framework for the interpretation of de novo mutation in human disease. Nat. Genet. 46, 944–950 (2014).
Siepel, A. et al. Evolutionarily conserved elements in vertebrate, insect, worm, and yeast genomes. Genome Res. 15, 1034–1050 (2005).
Desmet, F. O. et al. Human Splicing Finder: An online bioinformatics tool to predict splicing signals. Nucleic Acids Res. 37, (2009).
Clinical Genome Resource. ClinGen general sequence variant curation process standard operating procedure. https://www.clinicalgenome.org/working-groups/sequence-variant-interpretation/ (2019).
Kent, W. J. et al. The human genome browser at UCSC. Genome Res. 12, 996–1006 (2002).
Bateman, A. et al. UniProt: The universal protein knowledgebase in 2021. Nucleic Acids Res. 49, D480–D489 (2021).
Biesecker, L. G. & Harrison, S. M. The ACMG/AMP reputable source criteria for the interpretation of sequence variants. Genet. Med. 20, 1687–1688 (2018).
Clinical Genome Recource. ClinGen Hereditary Breast, Ovarian and Pancreatic Cancer Expert Panel Specifications to the ACMG/AMP Variant Interpretation Guidelines for ATM Version 1.1. https://www.clinicalgenome.org/site/assets/files/7451/clingen_hbop_acmg_specifications_atm_v1_1.pdf (2022).
Tavtigian, S. v. et al. Modeling the ACMG/AMP variant classification guidelines as a Bayesian classification framework. Genet. Med. 20, 1054–1060 (2018).
Stegel, V. et al. The occurrence of germline BRCA1 and BRCA2 sequence alterations in Slovenian population. BMC Med. Genet. 12, (2011).
Hamel, N. et al. On the origin and diffusion of BRCA1 c.5266dupC (5382insC) in European populations. Eur. J. Hum. Genet. 19, 300–306 (2011).
Krajc, M. et al. Five recurrent BRCA1/2 mutations are responsible for cancer predisposition in the majority of Slovenian breast cancer families. BMC Med. Genet. 9, (2008).
Fernandes, G. C. et al. Prevalence of BRCA1/BRCA2 mutations in a Brazilian population sample at-risk for hereditary breast cancer and characterization of its genetic ancestry. Oncotarget 7, 80465–80481 (2016).
Blay, P. et al. Mutational analysis of BRCA1 and BRCA2 in hereditary breast and ovarian cancer families from Asturias (Northern Spain). BMC Cancer 13, (2013).
Machackova, E. et al. Spectrum and characterisation of BRCA1 and BRCA2 deleterious mutations in high-risk Czech patients with breast and/or ovarian cancer. BMC Cancer 8, (2008).
Goidescu, I. G., Caracostea, G., Eniu, D. T. & Stamatian, F. V. Prevalence of deleterious mutations among patients with breast cancer referred for multigene panel testing in a Romanian population. Clujul. Med. 91, 157–165 (2018).
Espenschied, C. R. et al. Multigene panel testing provides a new perspective on lynch syndrome. J. Clin. Oncol. 35, 2568–2575 (2017).
Haraldsdottir, S. et al. Comprehensive population-wide analysis of Lynch syndrome in Iceland reveals founder mutations in MSH6 and PMS2. Nat. Commun. 8, (2017).
Sjursen, W., McPhillips, M., Scott, R. J. & Talseth-Palmer, B. A. Lynch syndrome mutation spectrum in New South Wales, Australia, including 55 novel mutations. Mol. Genet. Genomic Med. 4, 223–231 (2016).
Besic, N., Blatnik, A., Nizic-Kos, T., Novakovic, S. & Krajc, M. Characteristics of breast cancer in Slovenian patients with germline CHEK2 c.444+1G>A mutation. J. Clin. Oncol. 38, e13536–e13536 (2020).
Culver, J., Lowstuter, K. & Bowling, L. Assessing breast cancer risk and BRCA1/2 carrier probability. Breast Dis. 27, 5–20 (2007).
Thompson, E. R. et al. Panel testing for familial breast cancer: Calibrating the tension between research and clinical care. J. Clin. Oncol. 34, 1455–1459 (2016).
Tang, C. S. man et al. Actionable secondary findings from whole-genome sequencing of 954 East Asians. Hum. Genet. 137, 31–37 (2017).
Janavičius, R. Founder BRCA1/2 mutations in the Europe: Implications for hereditary breast-ovarian cancer prevention and control. EPMA J. 1, 397–412 (2010).
Zhang, L. et al. Prevalence and spectrum of DNA mismatch repair gene variation in the general Chinese population. J. Med. Genet. 59, 652–661 (2022).
Rashid, M. U. et al. Prevalence and spectrum of MLH1, MSH2, and MSH6 pathogenic germline variants in Pakistani colorectal cancer patients. Hered Cancer Clin. Pract. 17, 1–16 (2019).
Dominguez-Valentin, M. et al. Cancer risks by gene, age, and gender in 6350 carriers of pathogenic mismatch repair variants: Findings from the Prospective Lynch Syndrome Database. Genet. Med. 22, 15–25 (2019).
Smith, M. J. et al. The contribution of whole gene deletions and large rearrangements to the mutation spectrum in inherited tumor predisposing syndromes. Hum. Mutat. 37, 250–256 (2016).
Hampel, H. & de la Chapelle, A. The search for unaffected individuals with Lynch syndrome: Do the ends justify the means?. Cancer Prev. Res. (Phila) 4, 1–5 (2011).
Sjursen, W. et al. Current clinical criteria for Lynch syndrome are not sensitive enough to identify MSH6 mutation carriers. J. Med. Genet. 47, 579–585 (2010).
Yang, Y., Zhang, F., Wang, Y. & Liu, S. C. CHEK2 1100delC variant and breast cancer risk in caucasians: A meta-analysis based on 25 studies with 29,154 cases and 37,064 controls. Asian Pac. J. Cancer Prev. 13, 3501–3505 (2012).
Mohamad, S. et al. Low prevalence of CHEK2 gene mutations in multiethnic cohorts of breast cancer patients in Malaysia. PLoS ONE 10, 1 (2015).
Bellosillo, B. et al. Absence of CHEK2 mutations in Spanish families with hereditary breast cancer [2]. Cancer Genet. Cytogenet. 161, 93–95 (2005).
Couch, F. J. et al. Associations between cancer predisposition testing panel genes and breast cancer. JAMA Oncol. 3, 1190–1196 (2017).
de Wert, G. et al. Opportunistic genomic screening. Recommendations of the European Society of Human Genetics. Eur. J. Hum. Genet. 29, 365–377 (2021).
Manchanda, R. et al. Cost-effectiveness of population-based BRCA1, BRCA2, RAD51C, RAD51D, BRIP1, PALB2 mutation testing in unselected general population women. J. Natl. Cancer Inst. 110, 714–725 (2018).
Author information
Authors and Affiliations
Contributions
U.K., L.L. and B.P. conceived and designed the study. A.M. prepared the sequencing data. U.K. analyzed the data. U.K. wrote the first draft of the manuscript. All authors contributed to the manuscript revision, read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kotnik, U., Maver, A., Peterlin, B. et al. Assessment of pathogenic variation in gynecologic cancer genes in a national cohort. Sci Rep 13, 5307 (2023). https://doi.org/10.1038/s41598-023-32397-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-32397-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.