Abstract
To evaluate the sensitivity and specificity for screening and diagnosis of medial meniscal root injury using the distance ratio of medial joint space width between affected and unaffected knees in patients with potential medial meniscal root injury (MMRI) using plain radiographs, the study enrolled 49 patients with suspected MMRI who were then evaluated for MMRI using plain radiographs of both knees in the anteroposterior view and magnetic resonance imaging (MRI) findings. The ratios of peripheral medial joint space width between the affected and unaffected sides were calculated. The cut point value, sensitivity and specificity were calculated according to a receiver operating characteristic (ROC) curve. In the study, 18 and 31 patients were diagnosed with and without MMRI, respectively. The mean peripheral medial joint space width ratios comparing the affected side to the unaffected side in the standing position of the anteroposterior view of both knees in the MMRI and non-MMRI groups were 0.83 ± 0.11 and 1.04 ± 0.16, respectively, which was a significant difference (p-value < 0.001). The cut point value of the peripheral medial joint space width ratio between the affected and unaffected sides for suspected MMRI was 0.985, with sensitivity and specificity of 0.83 and 0.81, respectively, and for diagnosis was 0.78, with sensitivity and specificity of 0.39 and 1.00, respectively. The area under the ROC curve was 0.881. Patients with a possible MMRI had peripheral medial joint space width ratios less than patients with non-MMRI. This test can be used for reliably screening for or diagnosing medial meniscal root injury in primary or secondary care settings.
Similar content being viewed by others
Introduction
The incidence of medial meniscal root tear has substantially increased in recent years1,2,3,4. A medial meniscal root injury is biomechanically equivalent to having no meniscal tissue post-traumatic injury or post-operative total meniscectomy5, a condition which can rapidly progress to osteoarthritis if the diagnosis and treatment are delayed6,7,8,9. Choi et al.6 reported that medial meniscal root injury was found in 78.17% of patients less than 60 years old who underwent total knee arthroplasty. In contrast, patients who had been diagnosed at an early stage and treated with meniscal root repair had significantly better Lysholm and International Knee Documentation Committee (IKDC) scores and lower incidences of osteoarthritis8.
The clinical symptoms of patients with medial meniscal root injury generally involve a history of minor trauma (i.e. from squatting, changing position from sitting in a hyperflexion knee position to standing position, a low velocity fall, etc.) and persistent medial side knee pain10,11, which is usually diagnosed as osteoarthritis even in patients less than 50 years old12. To confirm the diagnosis and reduce the incidence of delayed or missed diagnosis of medial meniscal root injury, magnetic resonance imaging (MRI) is the gold standard investigation13,14,15,16. However, most patients with medial side knee pain first visit a doctor at a primary or secondary care unit where MRI is not available, and it would be beneficial for these patients if this kind of injury could be screened for at a primary or secondary care unit where plain radiographs are a standard investigation and readily available. Two studies, Bloecker et al.17 and Gale et al.18, evaluated the relationship between plain radiographs and intraarticular pathology using MRI, and both found that the center and periphery of the medial joint space were related to cartilage and meniscus, respectively17,18.
There are currently no screening tools readily available at primary or secondary care settings for screening or diagnosing medial meniscal root injury, which can lead to under-diagnosis of this disease with serious consequences for the patients. We felt that a careful examination of certain features of plain radiographs, available in some primary and all secondary care settings, might be able to provide sufficient evidence to indicate a risk of this type of injury, at which time at-risk patients could be referred in a timely way to a higher institute for proper management. The purpose of this study was to evaluate the sensitivity and specificity for screening or diagnosing medial meniscal root injury using the distance ratio of peripheral medial joint space width between affected and unaffected knees using plain radiographs. The hypothesis was that a patient with a medial meniscal root injury would have a smaller peripheral medial joint space width ratio than a patient without a medial meniscal root injury.
Results
Study population
Of the 75 patients enrolled, 26 patients were excluded, leaving 49 patients in the study, 18 patients with medial meniscal root injury and 31 patients with non-medial meniscal root injury. The demographic data are shown in Table 1; there were no significant differences between the groups. In the non-medial meniscal root injury group, the pathologies were meniscal tear of the anterior horn, body, or posterior horn in 1, 9, and 9 of 31 patients, respectively. The specific tear types were a degenerative tear in the 1 anterior horn patient, 5 horizontal tears and 4 degenerative tears in the 9 meniscus body tears, and 2 longitudinal tears, 4 horizontal tears and 3 degenerative tears in the 9 posterior horn tears.
The mean medial joint space widths of the affected and unaffected sides of the medial meniscal root injury group were 4.33 ± 1.57 and 5.25 ± 1.60 mm, respectively (p-value = 0.001), and of the non-medial meniscal root injury group were 5.37 ± 1.18 and 5.21 ± 1.16, respectively (p-value = 0.220). The differences in widths between the affected and unaffected sides in the medial meniscal root injury and the non-medial meniscal root injury groups were −0.93 ± 0.99 and 0.16 ± 0.72, respectively (p-value < 0.001).
The mean peripheral medial joint space width ratios comparing the affected side to the unaffected side in the standing position of the anteroposterior view of both knees in the medial meniscal root injury and non-medial meniscal root injury groups were 0.83 ± 0.11 and 1.04 ± 0.16, respectively, which was a significant difference (p-value < 0.001). The agreements between the peripheral medial joint space width ratio of the affected and unaffected sides and MRI findings, with sensitivity and specificity values, are shown in Table 2.
The cut point value of the peripheral medial joint space width ratio between the affected and unaffected sides for screening for medial meniscal root injury
We used the peripheral medial joint space width ratio between the affected and unaffected sides to discriminate between possible medial meniscal root injury and non-medial meniscal root injury. The cut point value of the peripheral medial joint space width ratio between the affected and unaffected sides for screening for medial meniscal root injury was 0.985; the overall parameters are shown in Table 2. The area under the receiver operating characteristic (ROC) curve was 0.839 (Fig. 1). The power analysis using the cut point value of 0.985 was 0.998.
The cut point value of the peripheral medial joint space width ratio between the affected and unaffected sides for diagnosing medial meniscal root injury
We used the peripheral medial joint space width ratio between the affected and unaffected sides to discriminate between medial meniscal root injury and non-medial meniscal root injury. The cut point value of the peripheral medial joint space width ratio between the affected and unaffected sides for diagnosing medial meniscal root injury was 0.78; the overall parameters are shown in Table 3. The area under the ROC curve was 0.839 (Fig. 1). The power analysis using the cut point value of 0.78 was 1.
There was high interobserver correlation between the experienced orthopaedist and the fourth-year orthopaedic resident in all measurements. The correlation coefficients of all assessments ranged between 0.80 and 0.87.
Discussion
We found that medial meniscal root injuries could be successfully screened for and/or diagnosed using plain radiographs. We found that all patients with a medial meniscal root injury had a smaller peripheral medial joint space width ratio than patients without medial meniscal root injury. The cut point value of the peripheral medial joint space width ratio between the affected and unaffected sides for screening for medial meniscal root injury was 0.985, with sensitivity and specificity of 0.83 (0.58, 0.96) and 0.81 (0.63, 0.93), respectively, and for diagnosing medial meniscal root injury was 0.78, with sensitivity and specificity of 0.39 (0.17, 0.64) and 1.00 (0.89, 1.00), respectively.
Osteoarthritis is an age-related disease which usually occurs in adults over 60 years of age19, although it can occur in patients aged less than 60 years following various traumas such as an intraarticular fracture, meniscal injury or osteochondral injury. Choi et al. reported that 78.17% of patients aged less than 60 years who had symptomatic osteoarthritis of the knees and underwent a TKA were found to have a medial meniscal root injury intraoperatively6. When this disease occurs in non-elderly patients, it often results from a missed medial meniscal root injury diagnosis, which is of concern since when a medial meniscal root injury is missed, the patient can rapidly develop symptomatic osteoarthritis which is much more difficult to treat and usually has lifelong consequences. The diagnostic gold standard investigation for medial meniscal root injury is MRI13,14,15,16,20, but this investigation is very expensive and available only in higher level hospitals. It is hard to identify patients at risk for this injury in primary or secondary care units which provide the first level of health care to individuals and families in most communities. It would be very useful if there was a simple investigation that could be used to screen for medial meniscal root injury in these clinics, which could decrease the incidence of delayed or missed diagnosis of this disease.
Two studies have evaluated the relationship between the medial joint space and the intraarticular structure by comparing MRI images and plain radiographs17,18. Both studies found that the center of the medial joint space was related to the cartilage and the periphery of the medial joint space was related to the meniscus. We applied the information from these studies to evaluate medial meniscal root injury by measuring the peripheral medial joint space width. Another factor is that if there is a load transfer to the knee joint in patients with medial meniscal root injury, there will be no hoop stress to decrease the peripheral medial joint space width. In this study, we measured the peripheral area of the medial joint space using radiographs taken with the knee in a standing, weight-bearing position to determine if such radiographs could be used for reliable screening or diagnosis of a medial meniscal root injury. We found that when the peripheral medial joint space width ratio between the affected and unaffected knees in patients with medial meniscal root injury was less than 0.985, the sensitivity and specificity were 0.83 and 0.81, respectively, and when the ratio was less than 0.78, the sensitivity and specificity were 0.39 and 1.00, respectively.
Based on the results of this study, we recommend that patients with symptoms indicating possible medial meniscal root injury should have anteroposterior radiographs of both knees with the patient in the standing, weight-bearing position, to perform our test described in this paper to avoid delayed or missed diagnosis of medial meniscal root injury, a disease which can quickly progress to osteoarthritis. These measurements involve quite small distances, so to ensure adequate accuracy when doing the measurements, we recommend first enlarging the image. If the peripheral medial joint space width ratio between the knees is less than 0.985, the doctor should be concerned about medial meniscal root injury (sensitivity = 0.83) and consider referring the patient for further investigation and treatment at a higher-level hospital. A peripheral medial joint space width ratio between the knees of less than 0.78 was strongly associated with medial meniscal root injury (specificity = 1.00).
The primary strength of this study is our confirmation that using a plain radiograph in an anteroposterior standing view of both knees, a simple investigation available in some primary care units and all secondary care units, can be used to screen for or diagnose medial meniscal root injury. This position is achievable in patients with any degree of knee pain, in contrast to the Rosenberg21 or one leg standing views22. The Rosenberg view is a posteroanterior view with weight-bearing in 45 degrees of knee flexion, while the one leg standing position is an anteroposterior view with full extension and weight-bearing. Either of these positions is hard to maintain for patients with moderate to severe knee pain. Additionally, the measurement method used in our study had high validity and was easy to perform based on clear anatomical landmarks.
There were some limitations to this study. First, it was hard to control the quality of the radiographic images due to the varying knee positions of the patients and the beam tilt, however, we compensated for this problem by using the distance ratio between the affected and unaffected sides. Second, pathology in a knee can lead to a patient not having full extension on an injured knee, leading to altered values even when comparing contralateral knees as each knee may not be at the same angle. Third, there were only small numbers of patients in both groups of this study. For further research, we plan to increase the number of patients through a multicenter trial. Fourth, patients with knee pathologies other than medial meniscal root injury such as modified Outerbridge grade 3 and 4 chondral lesions were excluded, as these pathologies can interfere with the joint space in one or both knees. Fifth, the results from this study would be difficult to apply to a patient with contralateral medial joint space narrowing (i.e. from osteoarthritis), and could thus result in falsely elevated values, and we suggest referring these patients to an orthopedist.
Conclusion
Patients with a medial meniscal root injury have a peripheral medial joint space width ratio less than patients without medial meniscal root injury. This test can be used for reliably screening for or diagnosing medial meniscal injury in a primary or secondary care settings.
Material and methods
This prospective review was approved by our institutional review board, and was performed in accordance with the relevant guidelines and regulations (REC 62-276-11-1). 75 patients with medial side knee pain were included in the study, aged between 23 and 69 years, enrolled from December 2019 to November 2021. Informed consent was obtained from all patients. The inclusion criteria were a history of minor trauma within the previous 3 months (i.e. from squatting, changing position from sitting in a hyperflexion knee position to standing position, a low velocity fall, etc.), pain on deep flexion, and tenderness at the medial joint line. The exclusion criteria were cartilage injury grade 3 or greater as shown on MRI (using the modified Outerbridge classification23), or a history of knee surgery, rheumatoid disease, soft tissue or bone tumors, or contralateral knee pain.
All patients had MRIs of the affected knee and anteroposterior view plain radiographs of both knees taken in the standing position.
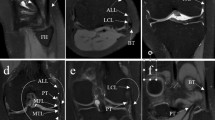
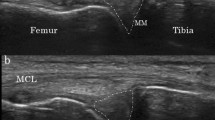
Joint space width measurements
Medial joint space width refers to the cartilage and meniscal structure of the knee. Two previous studies have reported that the center of the medial joint space was related to the cartilage and the periphery of the medial joint space was related to the meniscus17,18. To measure the joint space width, the distance from the most medial point to the most lateral point (yellow line in Fig. 2) was measured, and 11.25% of this distance measured inward from the most medial point of the tibial plateau was taken as the landmark (Fig. 2, red dot). The peripheral medial joint space width was measured perpendicularly from the red dot on Fig. 2 to the medial femoral condyle (white and blue lines). The ratio was then calculated by dividing the peripheral medial joint space width of the affected knee by the same measurement on the unaffected side. Each peripheral medial joint space width was measured three times by one experienced orthopaedist and one fourth-year orthopaedic resident, both of whom were blinded to the clinical data and MRI results. MRI results were reported by an experienced musculoskeletal radiologist.
An anteroposterior radiographic image of both knees showing the peripheral medial joint space distance between the medial femoral condyle and the medial tibial plateau of the affected (blue line) and unaffected (white line) knees. The study analysis was based on the ratio of the peripheral medial joint space distance in the affected knee (A, blue line) relative to the peripheral medial joint space distance in the unaffected knee (B, white line) (A, B).
Statistical analysis
The statistical analysis was performed with the R program and epicalc package (version 3.4.3, R Foundation for Statistical Computing, Vienna, Austria). The differences between the medial joint space width ratio of the affected and unaffected sides were analyzed using unpaired t-test. Statistical significance was set at P ≤ 0.05. The results are presented as mean ± SD. The parameters for diagnosing medial meniscal root injury of the medial joint space width ratio of the affected and unaffected sides were calculated in relation to the MRI findings, with sensitivity and specificity calculated for a 95% CI, and positive and negative predictive values. Inter-observer and intra-observer reliabilities were assessed by calculating intraclass correlation coefficient values (Supplementary file).
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Change history
22 November 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41598-023-47677-6
References
Bin, S., Kim, J. M. & Shin, S. J. Radial tears of the posterior horn of the medial meniscus. Arthroscopy J. Arthrosc. Relat. Surg. 20, 373–378 (2004).
Hwang, B. Y. et al. Risk factors for medial meniscus posterior root tear. Am. J. Sports Med. 40, 1606–1610 (2012).
Ozkoc, G. et al. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg. Sports Traumatol. Arthrosc. 16, 849–854 (2008).
Bhatia, S., Laprade, C. M., Ellman, M. B. & Laprade, R. F. Meniscal root tears: Significance, diagnosis, and treatment. Am. J. Sports Med. 42, 3016–3030 (2014).
Allaire, R., Muriuki, M., Gilbertson, L. & Harner, C. D. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J. Bone Joint Surg. Am. 90, 1922–1931 (2008).
Choi, E.-S. & Park, S.-J. Clinical evaluation of the root tear of the posterior horn of the medial meniscus in total knee arthroplasty for osteoarthritis. Knee Surg. Relat. Res. 27, 90–94 (2015).
Sung, K. et al. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg. Sports Traumatol. Arthrosc. 24, 1455–1468 (2016).
Chung, K. S. et al. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: A minimum 5-year follow-up. Arthroscopy J. Arthrosc. Relat. Surg. 31, 1941–1950 (2015).
Harner, C. D., Mauro, C. S., Lesniak, B. P. & Romanowski, J. R. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Surgical technique. J. Bone Joint Surg. Am. 91(2), 257–270 (2009).
Kim, J. H. et al. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: A prospective comparison study. Arthroscopy J. Arthrosc. Relat. Surg. 27, 1644–1653 (2011).
Pache, S. et al. Meniscal roots: Current concepts review. Arch. Bone Joint Surg. 6, 250–259 (2018).
Nepple, J. J., Dunn, W. R. & Wright, R. W. Meniscal repair outcomes at greater than five years: A systematic literature review and meta-analysis. J. Bone Joint Surg. Ser. A 94, 2222–2227 (2012).
Lee, D. W., Ha, J. K. & Kim, J. G. Medial meniscus posterior root tear: A comprehensive review. Knee Surg. Relat. Res. 26, 125–134 (2014).
Krych, A. J. et al. High rate of missed lateral meniscus posterior root tears on preoperative magnetic resonance imaging. Orthop. J. Sports Med. 6, 1–6 (2018).
LaPrade, R. F. et al. Diagnostic accuracy of 3.0 T magnetic resonance imaging for the detection of meniscus posterior root pathology. Knee Surg. Sports Traumatol. Arthrosc. 23, 152–157 (2015).
Choi, S.-H., Bae, S., Ji, S. K. & Chang, M. J. The MRI findings of meniscal root tear of the medial meniscus: Emphasis on coronal, sagittal and axial images. Knee Surg. Sports Traumatol. Arthrosc. 20, 2098–2103 (2012).
Bloecker, K. et al. Contribution of regional 3D meniscus and cartilage morphometry byMRI to joint space width in fixed flexion knee radiography-Abetween-knee comparison in subjects with unilateral jointspace narrowing. Eur. J. Radiol. 82, e832–e839 (2013).
Gale, D. R. et al. Meniscal subluxation: Association with osteoarthritis and joint space narrowing. Osteoarthr. Cartil. 7, 526–532 (1999).
Zhang, Y. & Jordan, J. M. Epidemiology of osteoarthritis. Clin. Geriatr. Med. 26, 355–369 (2010).
Kim, C. & Tufescu, T. V. Infection in closed fractures. JBJS Case Connect. 2, e44 (2012).
Kodama, Y. et al. Preliminary diagnosis of medial meniscus posterior root tears using the Rosenberg radiographic view. Knee Surg. Relat. Res. 31, 1–8 (2019).
Pinsornsak, P., Naratrikun, K., Kanitnate, S. & Sangkomkamhang, T. The one-leg standing radiograph. Bone Joint Res. 5, 436–441 (2016).
Colak, C. et al. Comparison of clinical and semiquantitative cartilage grading systems in predicting outcomes after arthroscopic partial meniscectomy. In American Journal of Roentgenology vol. 215 441–447 (American Roentgen Ray Society, 2020).
Acknowledgements
The authors sincerely thank Jirawan Jayuphan of the Epidemiology Unit, Faculty of Medicine for providing statistical support, and Dave Patterson of the Office of International Relations, Faculty of Medicine for his assistance with the English language.
Author information
Authors and Affiliations
Contributions
C. C. carried out the idea of the study, performed the statistical analysis and drafted the manuscript, P. A. participated in the design of the study and performed the statistical analysis, T. B. carried out the idea and drafted the manuscript, W. P. conceived of the study and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained an error in the Material and methods section, where the patient inclusion period was incorrect. Full information regarding the corrections made can be found in the correction for this Article.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Asawatreratanakul, P., Boonriong, T., Parinyakhup, W. et al. Screening for or diagnosing medial meniscal root injury using peripheral medial joint space width ratio in plain radiographs. Sci Rep 13, 4982 (2023). https://doi.org/10.1038/s41598-023-31735-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-31735-0
This article is cited by
-
Meniscectomy is associated with a higher rate of osteoarthritis compared to meniscal repair following acute tears: a meta‐analysis
Knee Surgery, Sports Traumatology, Arthroscopy (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.