Abstract
Antibiotic stewardship is viewed as having great public health benefit with limited direct benefit to the patient at the time of administration. The objective of our study was to determine if inappropriate administration of antibiotics could create conditions that would increase the rates of surgical infection. We hypothesized that sub-MIC levels of vancomycin would increase Staphylococcus aureus growth, biofilm formation, and rates of infection. S. aureus MRSA and MSSA strains were used for all experiments. Bacteria were grown planktonically and monitored using spectrophotometry. Quantitative agar culture was used to measure planktonic and biofilm bacterial burden. A mouse abscess model was used to confirm phenotypes in vivo. In the planktonic growth assay, increases in bacterial burden at ¼ MIC vancomycin were observed in USA300 JE2 by 72 h. Similar findings were observed with ½ MIC in Newman and SH1000. For biofilm formation, USA300 JE2 at ¼ and ½ MIC vancomycin increased biofilm formation by approximately 1.3- and 2.3-fold respectively at 72 h as compared to untreated controls. Similar findings were observed with Newman and SH1000 with a 2.4-fold increase in biofilm formation at ½ MIC vancomycin. In a mouse abscess model, there was a 1.2-fold increase with sub-MIC vancomycin at 3 days post infection. Our study showed that Sub-optimal vancomycin dosing promoted S. aureus planktonic growth and biofilm formation, phenotypic measures of bacterial virulence. This phenotype induced by sub-MIC levels of vancomycin was also observed to increase rates of infection and pathogenesis in our mouse model. Risks of exposure to sub-MIC concentrations with vancomycin in surgical procedures are greater as there is decreased bioavailability in tissue in comparison to other antibiotics. This highlights the importance of proper antibiotic selection, stewardship, and dosing for both surgical prophylaxis and treatment of infection.
Similar content being viewed by others
Introduction
Antibiotic stewardship is an important strategy to prevent development of antibiotic resistant organisms1. This is the primary motivational force behind the appropriate and judicious use of surgical antibiotic prophylaxis2,3, and limiting non-essential post-operative use of antibiotics in orthopaedic surgery. This has great public health benefit. At an individual level, implementing strict antibiotic stewardship has a less obvious benefit. Surgical site infections (SSIs) and implant associated infections can have severe outcomes with a high morbidity, mortality, and a large economic burden4,5,6,7,8. This is in comparison to the adverse events associated with antibiotics including allergic reaction, organ injury, and medication intolerance9. When clinical evidence is unclear, the potential benefits of antibiotic use are perceived to outweigh the possible adverse events. This has fuelled the debate between the use of a single dose of antibiotics as surgical prophylaxis10,11 and extended antibiotic treatments to prevent or treat periprosthetic joint infection12,13,14. Antibiotic stewardship is not just proper antibiotic selection but also obtaining appropriate clinical therapeutic levels.
Proper antibiotic therapeutic levels are a critical component for appropriate surgical prophylaxis which includes dose and length of administration as determined by the area under the curve. At levels below the minimum inhibitory concentration (MIC), antibiotics have been observed to alter growth rates of many bacteria including Staphylococcus aureus, the primary organism associated with orthopaedic infection15,16,17,18,19,20,21,22,23. This is a particular concern as bone and joints are less permeable to antibiotics and have a notoriously lower level of bioavailability as compared to other tissue leading to exposure to sub-MICs of antibiotics24. This problem is further compounded by the presence of an antibiotic tolerant biofilm on prosthetic components and within the joint space. Compared to their planktonic state, bacteria in a biofilm are 1000 times more resistant to antibiotics25,26,27.
The focus of this study was to determine the effect of sub-MIC levels of vancomycin on growth and pathogenesis of S. aureus, the most common organism associated with SSIs. We hypothesized that low doses of vancomycin would increase rates of infection due to increases in bacterial growth and biofilm formation. Our results demonstrate that sub-MIC levels of vancomycin increased S. aureus planktonic growth rates and biofilm formation in vitro and was associated with increased virulence in vivo.
Methods
Bacterial strains, plasmids and growth conditions
Staphylococcus aureus MRSA (USA300 JE2) was purchased from The American Type Culture Collection (ATCC). MSSA (SH1000, Newman) and EGFP reporter plasmids were kindly provided by Dr. Niles Donegan and Dr. Ambrose Cheung. S. aureus strains were grown in trypticase soy broth (TSB) medium with shaking at 37 °C and stored as frozen stocks in 15% glycerol at – 80 °C.
Minimum inhibitory concentration (MIC) assay
All vancomycin and cefazolin (Sigma-Aldrich) minimum inhibitory concentrations (MIC) for S. aureus JE2, Newman and SH1000 were determined according to CLSI protocols28,29. Bacteria were inoculated into 5 ml TSB medium and grown overnight at 37ºC. Cultures were normalized to 1 × 106 CFU/ml using a 0.5× McFarland turbidity standard (Hardy Diagnostics) and plated in 96 well plates (Costar) containing serial dilutions of vancomycin (0.25, 0.5, 1, 2, 4, 8, 16, 32, 64 µg/ml). As an additional measure for MIC S. aureus MRSA JE2 and MSSA Newman containing an enhanced green fluorescent protein (EGFP) were tested with vancomycin E-test MIC strips (Liofilchem). A culture sample (~ 108 CFU/ml) was obtained and streaked onto a trypticase soy blood agar plate (TSA II). Next, the E-test MIC strip was applied and the plate was incubated overnight at 37 °C. MIC values were recorded where the pointed end of the inhibition ellipse intersects with the side of the strip. Newman was visualized using a Nikon TE-300 fluorescent microscope equipped with a SPOT camera.
Planktonic MIC growth assay
Approximately 1 × 104 CFU MRSA JE2, MSSA Newman and SH1000 were added to a 12-well plate (Costar) containing 0, 0.25, and 0.5 μg/ml vancomycin respectively (0, ¼ and ½ MIC) and incubated at 37 °C for 24, 48, and 72 h. Bacteria were serially diluted, plated onto TSA II plates, and incubated overnight at 37 °C. Colonies were counted and the bacterial concentration was determined in CFU/ml. To compare phenotypes, MSSA strains Newman and SH1000 were tested with 0, 0.0125 and 0.25 μg/ml cefazolin (0, ¼ and ½ MIC).
Titanium rod biofilm MIC assay
Titanium rods (12 mm) were placed into a 12 well tissue culture plate containing TSB with 1 × 104 CFU/ml S. aureus MRSA (JE2), MSSA Newman and SH1000 with 0, 0.25, and 0.5 μg/ml vancomycin respectively (0, ¼ and ½ MIC). The plate was incubated at 37 °C for 24, 48, and 72 h. To remove non-adherent cells, wells were replaced with fresh TSB every 24 h. At experimental endpoints, titanium rods were washed three times in 1 ml PBS and placed into 1 ml of PBS containing 0.1% tween (PBST). To break up the biofilm, samples were sonicated using a Branson model #3510 sonicating water bath for 30 min. Serial dilutions of the sonicated bacterial suspension were prepared and plated onto TSA II plates and incubated overnight at 37 °C. Colonies were counted and the biofilm bacterial burden was determined in CFU/ml.
Fibrinogen biofilm assay
A semi-quantitative adherence assay was performed with MRSA JE2 using 96-well plates. Plates were coated with 100 μl of phosphate-buffered saline (PBS) containing 5 μg/ml fibrinogen (Sigma-Aldrich) and incubated overnight at 4 °C. Plates were washed three times with PBS and blocked with 2% bovine serum albumin (BSA) (Sigma-Aldrich) for 1 h at 37 °C. Plates were washed with PBS as described above. Approximately 1 × 107 bacteria were added to appropriate wells and incubated for 24 h at 37 °C. Next, wells were washed four times with PBS. Bacteria were fixed in 10% formaldehyde (Sigma-Aldrich) for 10 min. 0.2% crystal violet (Sigma-Aldrich) was added to each well and incubated at room temperature for 10 min. The plates were washed four times with distilled water and air dried for 2 h. Crystal violet stain was dissolved in 30% acetic acid (Fisher Scientific) and absorbance was measured at 590 nm using an Infinite 200 plate reader (Tecan).
Mouse abscess model
8–12-week-old C57BL/6J female mice were purchased from The Jackson laboratory (Bar Harbor, ME). All animal protocols used for these experiments were approved by the University of Pittsburgh’s Institutional Animal Care and Use Committee. Authors complied with all the relevant guidelines and regulations and complied with ARRIVE guidelines. The weight of each C57BL/6J mouse was recorded before the start of the procedure. One hour prior to inoculation of bacteria, 0, 0.01, and 0.1 mg/g vancomycin were injected subcutaneously into mice (n = 10 per group). The in vitro and in vivo doses are related as they are below the MIC and sub-therapeutic. There is not a one-to-one correlation between in vitro and in vivo doses based on antibiotic pharmacokinetics and bioavailability. Mice were anesthetized by 2% isoflurane and the hair on the flank was removed using Nair. Next, 20 µl of S. aureus (1 × 106 CFU) was injected subcutaneously into the flank. At 3 days post infection, mice were euthanized and the length and width of the abscess was measured with a Vernier caliper. The abscess area was calculated using the formula Area = (L/2) × (W/2) × π. Each abscess was collected and placed in sterile PBS. Tissues were mechanically homogenized with a TT10 basic Ultra-TURRAX homogenizer (IKA). Next, samples were serially diluted, plated onto TSA II plates and incubated overnight at 37 °C. Colonies were counted and the bacterial burden in CFU/ml was recorded.
Infection rate and median infectious dose (ID50)
Bacterial cultures and mice were infected and treated as described above. Following the protocol described above for inoculation, serial dilutions of MRSA JE2 were injected into the flank of mice (n = 10 per group). On the 3rd day of infection, animals were euthanized, abscess were measured, harvested, and bacterial burden quantified. The number of bacteria required to infect 50% of the mice (ID50) was calculated according to Reed et al.30.
Statistical analysis
All graphical and statistical analysis was performed using Prism 9.0 (GraphPad, La Jolla, CA). Statistical analysis was performed using two-way ANOVA for the planktonic and biofilm data, and a two-tailed Student’s t-test for the in vivo infection data. Significance was determined at p < 0.05.
Results
Sub-MIC levels of vancomycin promote S. aureus growth
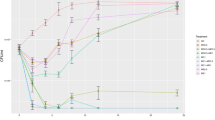
When testing MRSA JE2 with a vancomycin E-test strip, we observed increased bacterial growth along the boundary of the growth inhibition area (Fig. 1A, white box). A greater accumulation of S. aureus colonies were observed near the edge of inhibitory area at sub-MIC concentrations (Fig. 1B). When this assay was repeated using a S. aureus MSSA Newman strain containing an EGFP fluorescent reporter, a brighter green fluorescent signal was observed near the inhibitory edge of the test strip at sub-MIC ranges indicating increased bacterial growth (Fig. 1C). To expand upon these findings, we used a planktonic growth assay. Similar to the E-test results, with JE2 strain, ¼ MIC vancomycin treatment resulted in a 1.2-fold increase after 24 h of growth (p = 0.02) and a 1.1-fold increase after 72 h of growth (0.03). In the Newman strain, ½ MIC vancomycin treatment resulted a 259-fold increase after 72 h growth (p = 0.01). SH1000 phenotypes were similar with ½ MIC vancomycin treatment resulting in a 7.2-fold increase (p = 0.01) after 24 h growth, a 35-fold increase after 48 h growth (p = 0.02) and a 75-fold increase after 72 h growth (p = 0.01). When sub-MIC cefazolin was tested with Newman and SH1000 strains for comparison, the same trend was not observed. Cefazolin treatment at ¼ and ½ MIC levels resulted in decreased bacterial growth in comparison to untreated samples (Fig. 2).
Sub-MIC vancomycin promotes S. aureus planktonic growth (A) MRSA JE2 vancomycin E-test strip MIC assay. White box indicates zoomed in area for (B) a greater bacteria accumulation occurs near the edge of E-test strip inhibitory area (C) MSSA Newman strain containing an EGFP fluorescent reporter demonstrating a brighter green fluorescent signal near the edge of the vancomycin inhibitory are a indicating more bacterial growth. Sub-MIC vancomycin promotes increased planktonic growth in (D) MRSA JE2 (E) MSSA Newman and (F) SH1000. N = 4 per treatment group. Error bars represent standard deviation. *p < 0.05, **p < 0.01.
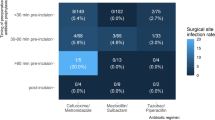
S. aureus treated with sub-MIC concentrations of vancomycin increases biofilm formation
After observing increased rates of S. aureus planktonic growth in the presence of sub-MIC levels of vancomycin in all strains tested, we hypothesized a similar phenotype would occur with biofilm formation. In JE2 biofilms, ¼ MIC vancomycin resulted in 1.3-fold increase in bacterial burden on day 2 and day 3 respectively (p = 0.03, p = 0.04, Fig. 2A). JE2 biofilms at ½ MIC vancomycin resulted in 2 and 2.3-fold increases in bacterial burden on day 2 and 3 respectively (p = 0.01p = 0.02 Fig. 3A). Similar results were observed with S. aureus Newman at ¼ MIC vancomycin with a 1.4-fold increase in bacterial burden on day 2 (p = 0.03) and ½ MIC vancomycin with 2.9, 2.6, and 2.4-fold increases in bacterial burden on days 1, 2, and 3 (Fig. 3B, p = 0.004, p = 0.002, p = 0.001). SH1000 demonstrated a similar trend with ¼ MIC vancomycin resulting in 1.6 and 1.5-fold increases in bacterial burden on days 1 and 2 (Fig. 3C, p = 0.03, p = 0.02) and ½ MIC vancomycin treatment resulting in 2.7, 2.8, and 2.4-fold increases in bacterial burden on days 1, 2, and 3 (Fig. 3C, p = 0.02, p = 0.001, p = 0.003). Similar to our biofilm results grown on titanium wires, after 1 day of growth, ½ MIC vancomycin treatment on a fibrinogen coated surface resulted in increased biofilm growth with a 1.4-fold increase in comparison to untreated controls (Fig. 3D, p = 0.02).
Sub-MIC treatment of vancomycin increases S. aureus pathogenicity in vivo
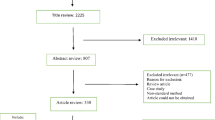
To test the phenotype of sub-MIC vancomycin treatment in vivo, we used an SSI abscess mouse model. No differences in abscess volume were observed for any of the treatment groups (Fig. 4A). However, a significantly greater bacterial burden (1.2-fold increase) was observed in mice treated with sub-therapeutic vancomycin dosing in comparison to untreated controls (Fig. 4B, p = 0.009).
Sub-MIC vancomycin increases bacterial growth and infection in vivo. Mouse abscess model inoculated with 1 × 107 CFU/ml JE2. S. aureus and treated with sub-MIC vancomycin (0.01 mg/g) for 3 days. (A) There were no differences between treatment groups for total abscess area n = 10 per group. (B) For bacterial burden, the abscess burden was significantly greater in the sub-MIC group at 3 days post infection n = 10 per group. (C) Sub-MIC vancomycin treatment results in a higher infection rate in mice. Results are from 5 independent experimental trials. Error bars represent standard deviation. *p < 0.05.
Infection rates are greater in mice treated with sub-MIC concentrations of vancomycin
Rates of bacterial growth and biofilm formation are important phenotypes for pathogenesis. If sub-MIC ranges of vancomycin increased S. aureus growth, biofilm formation, and bacterial burden in our mouse model, we hypothesized that treatment with sub-therapeutic levels of vancomycin would result in increased rates of infection. In comparison to untreated controls (41.5% infection rate), a greater infection rate (62.5%) was observed in the sub-therapeutic vancomycin treatment group (Fig. 4C, p = 0.03, 95% CI 4.941 to 37.06).
Discussion
The clear benefits of antibiotic stewardship at a public health level in preventing multidrug resistant bacteria are not as obvious at the patient level. In the post-operative period, antibiotics have a low risk profile to the patient as compared to the large possible benefit at preventing surgical infection. When the clinical evidence is unclear, the potential benefits of antibiotics from a surgeon perspective are perceived to outweigh the risk of antibiotic overuse and possible adverse events. This has fueled the debate on whether perioperative antibiotics should continue to be administered as surgical prophylaxis, especially with the use of arthroplasty implants10,11. Sir John Charnley noted avoiding surgical antibiotic prophylaxis because “it had been suggested that a higher rate of wound infection occurs with prophylactic antibiotics than without31”. In 2006, The Centers for Disease Control (CDC) along with the Centers for Medicare & Medicaid Services created the Surgical Care Improvement Project (SCIP) guidelines that recommend (1) prophylactic antibiotics given within 60–120 min prior to surgery, (2) proper antibiotic selection based on procedures, and (3) no additional prophylactic antibiotics after closure of the surgical incision3.
In the present study, we observed sub-therapeutic levels of vancomycin increased S. aureus planktonic growth and biofilm formation in vitro and in vivo, an important step in the initiation of surgical infection. Increased biofilm formation in the presence of sub-MIC antibiotics has been demonstrated in S. aureus and other microorganisms known to cause SSIs including coagulase negative Staphylococci, Staphylococcus epidermidis, and Pseudomonas aeruginosa15,16,17,32. This phenotype was observed in our animal model where sub-therapeutic levels of vancomycin increased bacterial burden and infection rate. Combined, these data have important implications for surgical prophylaxis, proper antibiotic selection, and dosing which includes the actual dose and timing. Our manuscript suggests that not achieving clinical therapeutic levels of antibiotics such as with shorter duration of surgical prophylaxis as recommended by the CDC may potentially increase the risk for surgical infection.
First generation cephalosporins are the preferred choice for antibiotic prophylaxis in orthopaedic surgery33. Patients who receive an alternative treatment to cephalosporins have been shown to have an increased risk for developing SSI, including with MRSA34,35. Our data provide additional support for cefazolin use as a perioperative antibiotic as sub-MIC treatment did not demonstrate increased bacterial growth. Concerns for penicillin allergy and cross reactivity can lead surgeons to select other options including vancomycin33. Multiple studies have demonstrated that cefazolin is safe and effective when a distant history of penicillin allergy is reported36. Over time, many patients no longer suffer a penicillin allergy and are skin test negative within a 10 year period37. When a self-reported allergic response is recent, antibiotic allergy testing is recommended38.
In the case of MRSA infection, vancomycin is the antibiotic of choice; however this can be difficult to appropriately dose based on bioavailability and poor penetration into musculoskeletal tissues24,39 and has been shown to have severe side effects from intravenous dosing including nephrotoxicity40,41,42,43,44,45,46,47. In 2020, the American Society of Health-System Pharmacists, the Infectious Disease Society of America, the Pediatric Infectious Diseases Society and the Society of Infectious Disease Pharmacists collaboratively worked together in order to create new consensus guidelines for therapeutic monitoring of vancomycin for severe MRSA infections48. Prior to these newer recommendations, vancomycin trough levels were considered surrogate markers for measuring the area under the curve (AUC), with an AUC goal of ≥ 400 mcg h/ml deemed sufficient to achieve a clinical therapeutic level of vancomycin based on done and duration. The newer guidelines however no longer recommend using vancomycin troughs as surrogates for AUC, based on a meta-analysis of 14 observational cohort studies that showed vancomycin troughs ≥ 15 were not associated with improved outcomes49. In addition, a subsequent meta-analysis of 15 studies assessing the impact of vancomycin trough concentrations on vancomycin induced nephrotoxicity found that there was an approximately 300% increased risk of nephrotoxicity when troughs were at or greater than 15 mcg/ml44. Given these findings, as well as a recent meta-analysis study that showed a 32% decrease in risk when AUC-guided dosing was employed over standard trough monitoring for vancomycin50, the current guidelines suggest AUC-guided vancomycin dosing over trough monitoring, with AUC goals of 400–600 mcg h/ml. These guideline changes aim to improve overall patient safety, particularly by lowering the risk of vancomycin induced nephrotoxicity, while simultaneously providing more consistent efficacy in the treatment of serious MRSA infections.
The present study is not without limitations. For our SSI model, animals were dosed prophylactically with sub-MIC vancomycin 1-h prior to bacterial inoculation. This is within the SCIP guidelines for perioperative administration, but vancomycin and fluoroquinolones can be given up to 120 min prior to inoculation3. In addition, no vancomycin MIC dose was tested for comparison as well as different antibiotic dosing routes. This was not completed as MIC dosing and higher values would be considered appropriate dosing.
Conclusion
Finally, there is not a direct correlation between in vitro levels and in vivo levels. microbe dynamics, (bacterial load, genetics, persistence, contamination of the wound, implanted material, etc.) and antibiotic dynamics. Here, in vitro dosing was below the MIC and the clinical therapeutic level was below the AUC in our in vivo models.
Our investigation demonstrates the importance of proper antibiotic selection and dosing. Inappropriate dosing of vancomycin resulted in greater bacterial burden, disease severity, and higher infection rates. These results highlight the importance of proper antibiotic stewardship by achieving the needed clinical therapeutic antibiotic levels with appropriate and perioperative dosing to prevent bacterial infections.
Data availability
The data generated and analyzed during this study may be available from the corresponding author on a reasonable request to the corresponding author or the corresponding author’s delegate.
References
Sandegren, L. Selection of antibiotic resistance at very low antibiotic concentrations. Ups J. Med. Sci. 119, 103–107. https://doi.org/10.3109/03009734.2014.904457 (2014).
Ryan, S. P. et al. Is there a difference in infection risk between single and multiple doses of prophylactic antibiotics? A meta-analysis. Clin. Orthop. Relat. Res. 477, 1577–1590. https://doi.org/10.1097/CORR.0000000000000619 (2019).
Tan, T. L. et al. Perioperative antibiotic prophylaxis in total joint arthroplasty: A single dose is as effective as multiple doses. J. Bone Jt. Surg. Am. 101, 429–437. https://doi.org/10.2106/JBJS.18.00336 (2019).
Urish, K. L. et al. A multicenter study of irrigation and debridement in total knee arthroplasty periprosthetic joint infection: Treatment failure is high. J. Arthroplasty 33, 1154–1159. https://doi.org/10.1016/j.arth.2017.11.029 (2018).
Shah, M. Q. et al. Surgical site infection in orthopaedic implants and its common bacteria with their sensitivities to antibiotics, in open reduction internal fixation. J. Ayub Med. Coll. Abbottabad 29, 50–53 (2017).
Sugarman, B. Infections and prosthetic devices. Am. J. Med. 81, 78–84. https://doi.org/10.1016/0002-9343(86)90517-6 (1986).
Izakovicova, P., Borens, O. & Trampuz, A. Periprosthetic joint infection: Current concepts and outlook. EFORT Open Rev. 4, 482–494. https://doi.org/10.1302/2058-5241.4.180092 (2019).
Zimmerli, W., Trampuz, A. & Ochsner, P. E. Prosthetic-joint infections. N. Engl. J. Med. 351, 1645–1654. https://doi.org/10.1056/NEJMra040181 (2004).
Mohsen, S., Dickinson, J. A. & Somayaji, R. Update on the adverse effects of antimicrobial therapies in community practice. Can. Fam. Phys. 66, 651–659 (2020).
Berrios-Torres, S. I. et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. 152, 784–791. https://doi.org/10.1001/jamasurg.2017.0904 (2017).
Leaper, D. J. & Edmiston, C. E. World Health Organization: Global guidelines for the prevention of surgical site infection. J. Hosp. Infect. 95, 135–136. https://doi.org/10.1016/j.jhin.2016.12.016 (2017).
Inabathula, A. et al. Extended oral antibiotic prophylaxis in high-risk patients substantially reduces primary total hip and knee arthroplasty 90-day infection rate. J. Bone Jt. Surg. Am. 100, 2103–2109. https://doi.org/10.2106/JBJS.17.01485 (2018).
Frank, J. M. et al. The Mark Coventry, MD, Award: Oral antibiotics reduce reinfection after two-stage exchange: A multicenter, randomized controlled trial. Clin. Orthop. Relat. Res. 475, 56–61. https://doi.org/10.1007/s11999-016-4890-4 (2017).
Shah, N. B. et al. Benefits and adverse events associated with extended antibiotic use in total knee arthroplasty periprosthetic joint infection. Clin. Infect. Dis. 70, 559–565. https://doi.org/10.1093/cid/ciz261 (2020).
Schadow, K. H., Simpson, W. A. & Christensen, G. D. Characteristics of adherence to plastic tissue culture plates of coagulase-negative staphylococci exposed to subinhibitory concentrations of antimicrobial agents. J. Infect. Dis. 157, 71–77. https://doi.org/10.1093/infdis/157.1.71 (1988).
Wang, Q. et al. Enhancement of biofilm formation by subinhibitory concentrations of macrolides in icaADBC-positive and -negative clinical isolates of Staphylococcus epidermidis. Antimicrob. Agents Chemother. 54, 2707–2711. https://doi.org/10.1128/AAC.01565-09 (2010).
Cargill, J. S. & Upton, M. Low concentrations of vancomycin stimulate biofilm formation in some clinical isolates of Staphylococcus epidermidis. J. Clin. Pathol. 62, 1112–1116. https://doi.org/10.1136/jcp.2009.069021 (2009).
Hoffman, L. R. et al. Aminoglycoside antibiotics induce bacterial biofilm formation. Nature 436, 1171–1175. https://doi.org/10.1038/nature03912 (2005).
Boehm, A. et al. Second messenger signalling governs Escherichia coli biofilm induction upon ribosomal stress. Mol. Microbiol. 72, 1500–1516. https://doi.org/10.1111/j.1365-2958.2009.06739.x (2009).
Majtan, J., Majtanova, L., Xu, M. & Majtan, V. In vitro effect of subinhibitory concentrations of antibiotics on biofilm formation by clinical strains of Salmonella enterica serovar Typhimurium isolated in Slovakia. J. Appl. Microbiol. 104, 1294–1301. https://doi.org/10.1111/j.1365-2672.2007.03653.x (2008).
Drenjancevic, D., Vranes, J., Bedenic, B. & Sakic-Zdravcevic, K. In vitro effect of subinhibitory concentrations of ceftazidime and meropenem on the serum sensitivity of Pseudomonas aeruginosa strains. Coll. Antropol. 31, 221–225 (2007).
Bisognano, C., Vaudaux, P. E., Lew, D. P., Ng, E. Y. & Hooper, D. C. Increased expression of fibronectin-binding proteins by fluoroquinolone-resistant Staphylococcus aureus exposed to subinhibitory levels of ciprofloxacin. Antimicrob. Agents Chemother. 41, 906–913 (1997).
Carsenti-Etesse, H. et al. Effects of subinhibitory concentrations of vancomycin and teicoplanin on adherence of staphylococci to tissue culture plates. Antimicrob. Agents Chemother. 37, 921–923. https://doi.org/10.1128/aac.37.4.921 (1993).
Bassetti, M. et al. Current antibiotic management of prosthetic joint infections in Italy: The “Udine strategy”. J. Antimicrob. Chemother. 69(Suppl 1), i41–i45. https://doi.org/10.1093/jac/dku251 (2014).
Urish, K. L. et al. Antibiotic-tolerant Staphylococcus aureus biofilm persists on arthroplasty materials. Clin. Orthop. Relat. Res. 474, 1649–1656. https://doi.org/10.1007/s11999-016-4720-8 (2016).
Mandell, J. B. et al. Large variations in clinical antibiotic activity against Staphylococcus aureus biofilms of periprosthetic joint infection isolates. J. Orthop. Res. 37, 1604–1609. https://doi.org/10.1002/jor.24291 (2019).
Ma, D. et al. The toxin-antitoxin MazEF drives Staphylococcus aureus biofilm formation, antibiotic tolerance, and chronic infection. mBio 10, 19. https://doi.org/10.1128/mBio.01658-19 (2019).
Clinical and Laboratory Standards Institute. M100: Performance Standards for Antimicrobial Susceptibility Testing.
Clinical and Laboratory Standards Institute. M07: Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically (2018).
Reed, L. J. A simple method of estimating fifty per cent endpoints. Am. J. Hygeine 27, 493–497 (1938).
Charnley, J. & Eftekhar, N. Postoperative infection in total prosthetic replacement arthroplasty of the hip-joint. With special reference to the bacterial content of the air of the operating room. Br. J. Surg. 56, 641–649. https://doi.org/10.1002/bjs.1800560902 (1969).
Cirioni, O. et al. In vitro and in vivo effects of sub-MICs of pexiganan and imipenem on Pseudomonas aeruginosa adhesion and biofilm development. Infez. Med. 21, 287–295 (2013).
Wyles, C. C. et al. 2019 John Charnley Award: Increased risk of prosthetic joint infection following primary total knee and hip arthroplasty with the use of alternative antibiotics to cefazolin: The value of allergy testing for antibiotic prophylaxis. Bone Jt. J. 101, 9–15 (2019).
Blumenthal, K. G. et al. The impact of a reported penicillin allergy on surgical site infection risk. Clin. Infect. Dis. 66, 329–336. https://doi.org/10.1093/cid/cix794 (2018).
Blumenthal, K. G. et al. Risk of meticillin resistant Staphylococcus aureus and Clostridium difficile in patients with a documented penicillin allergy: Population based matched cohort study. BMJ 361, k2400. https://doi.org/10.1136/bmj.k2400 (2018).
Macy, E. & Poon, K. Y. T. Self-reported antibiotic allergy incidence and prevalence: Age and sex effects. Am. J. Med. 122, 778. https://doi.org/10.1016/j.amjmed.2009.01.034 (2009).
Trubiano, J. A., Adkinson, N. F. & Phillips, E. J. Penicillin allergy is not necessarily forever. JAMA 318, 82–83. https://doi.org/10.1001/jama.2017.6510 (2017).
Macy, E., Khan, D. A., Castells, M. C. & Lang, D. M. Penicillin allergy testing: A key component of antibiotic stewardship. Clin. Infect. Dis. 64, 531–532. https://doi.org/10.1093/cid/ciw795 (2017).
Estes, K. S. & Derendorf, H. Comparison of the pharmacokinetic properties of vancomycin, linezolid, tigecyclin, and daptomycin. Eur. J. Med. Res. 15, 533–543. https://doi.org/10.1186/2047-783x-15-12-533 (2010).
Hermsen, E. D. et al. Clinical outcomes and nephrotoxicity associated with vancomycin trough concentrations during treatment of deep-seated infections. Expert Opin. Drug Saf. 9, 9–14. https://doi.org/10.1517/14740330903413514 (2010).
Jeffres, M. N., Isakow, W., Doherty, J. A., Micek, S. T. & Kollef, M. H. A retrospective analysis of possible renal toxicity associated with vancomycin in patients with health care-associated methicillin-resistant Staphylococcus aureus pneumonia. Clin. Ther. 29, 1107–1115. https://doi.org/10.1016/j.clinthera.2007.06.014 (2007).
Kralovicova, K. et al. Do vancomycin serum levels predict failures of vancomycin therapy or nephrotoxicity in cancer patients? J. Chemother. 9, 420–426. https://doi.org/10.1179/joc.1997.9.6.420 (1997).
Pritchard, L. et al. Increasing vancomycin serum trough concentrations and incidence of nephrotoxicity. Am. J. Med. 123, 1143–1149. https://doi.org/10.1016/j.amjmed.2010.07.025 (2010).
van Hal, S. J., Paterson, D. L. & Lodise, T. P. Systematic review and meta-analysis of vancomycin-induced nephrotoxicity associated with dosing schedules that maintain troughs between 15 and 20 milligrams per liter. Antimicrob. Agents Chemother. 57, 734–744. https://doi.org/10.1128/AAC.01568-12 (2013).
Wong-Beringer, A., Joo, J., Tse, E. & Beringer, P. Vancomycin-associated nephrotoxicity: A critical appraisal of risk with high-dose therapy. Int. J. Antimicrob. Agents 37, 95–101. https://doi.org/10.1016/j.ijantimicag.2010.10.013 (2011).
Rodriguez Colomo, O. et al. Impact of administration of vancomycin or linezolid to critically ill patients with impaired renal function. Eur. J. Clin. Microbiol. Infect. Dis. 30, 635–643. https://doi.org/10.1007/s10096-010-1133-6 (2011).
Rybak, M. J. et al. Therapeutic monitoring of vancomycin in adults summary of consensus recommendations from the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Pharmacotherapy 29, 1275–1279. https://doi.org/10.1592/phco.29.11.1275 (2009).
Rybak, M. J. et al. Therapeutic monitoring of vancomycin for serious methicillin-resistant Staphylococcus aureus infections: A revised consensus guideline and review by the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists. Am. J. Health Syst. Pharm. 77, 835–864. https://doi.org/10.1093/ajhp/zxaa036 (2020).
Prybylski, J. P. Vancomycin trough concentration as a predictor of clinical outcomes in patients with Staphylococcus aureus bacteremia: A meta-analysis of observational studies. Pharmacotherapy 35, 889–898. https://doi.org/10.1002/phar.1638 (2015).
Aljefri, D. M. et al. Vancomycin area under the curve and acute kidney injury: A meta-analysis. Clin. Infect. Dis. 69, 1881–1887. https://doi.org/10.1093/cid/ciz051 (2019).
Funding
Dr. Kenneth Urish is supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS R01AR082167; K08AR071494; R03AR077602), the Orthopaedic Research and Education Foundation, and the Musculoskeletal Tissue Foundation.
Author information
Authors and Affiliations
Contributions
K.M.B., D.M.P., M.T., D.M., J.B.M., and K.L.U. designed the study; K.M.B., D.M.P., M.T., D.M., J.B.M., L.L.T. performed the experiments and gathered the data; K.M.B., D.M., N.B.S., V.K.B., and K.L.U. wrote the paper; K.M.B., N.B.S., V.K.B., and K.L.U. critically reviewed the data interpretation and the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brothers, K.M., Parker, D.M., Taguchi, M. et al. Dose optimization in surgical prophylaxis: sub-inhibitory dosing of vancomycin increases rates of biofilm formation and the rates of surgical site infection. Sci Rep 13, 4593 (2023). https://doi.org/10.1038/s41598-023-30951-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-30951-y
This article is cited by
-
Prophylactic use of vancomycin powder on postoperative infection after total joint arthroplasty
BMC Musculoskeletal Disorders (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.