Abstract
Advanced triple negative breast cancer (TNBC) is an aggressive, but initially chemo-sensitive disease. The prognosis is poor and more than three quarters of patients experience progression 12 months after the initiation of conventional first-line chemotherapy. Approximately two thirds of TNBC express epidermal growth factor receptor 1 (EGFR). We have developed an anti-EGFR targeted nanocontainer drug by inserting anti-EGFR antibody fragments into the membrane of pegylated liposomes (anti-EGFR-ILs-dox). The payload consists of doxorubicin, a standard drug for TNBC. In a first-in-human phase I trial in 26 patients with various advanced solid malignancies, anti-EGFR-ILs-dox has shown little toxicity and encouraging efficacy. In this single-arm phase II trial, we assessed the efficacy of anti-EGFR-ILs-dox as first-line therapy in patients with advanced, EGFR + TNBC. The primary endpoint was progression-free survival at 12 months (PFS12m). Secondary endpoints included overall response rate (ORR), duration of response (DOR), time to progression (TTP), overall survival (OS) and adverse events (AEs). 48 patients received anti-EGFR-ILs-dox 50 mg/m2 iv, on day one of a 28 days-cycle until progression. The Kaplan–Meier estimate for PFS12m was 13% (one-sided 90% CI 7%, 95% CI [5%, 25%]), median PFS was 3.5 months (95% CI 1.9, 5.4). The trial has not reached its primary endpoint. There were no new toxicity signals. Based on these results, anti-EGFR-ILs-dox should not be further developed for TNBC. It remains an open question whether anti-EGFR-ILs-dox would offer more opportunities in other EGFR-expressing malignancies, where targeting this receptor has already shown anticancer effects.
Trial registration: This trial was registered at clinicaltrials.gov: NCT02833766. Registered 14/07/2016.
Similar content being viewed by others
Introduction
Breast cancer (BC) is the most frequently diagnosed cancer and the leading cause of cancer death in women worldwide, accounting for 25% of all new cancer cases and 15.5% of cancer deaths1. Triple negative breast cancer (TNBC), defined by the lack of expression of the estrogen receptor (ER), the progesterone receptor (PR), and the human epidermal growth factor receptor 2 (HER2), comprises approximately 15% of all BC and is associated with the worst prognosis of all subtypes. Unlike for other breast cancer subtypes, targeted treatment options are limited for this entity and no targeted agent is currently approved in the first line treatment setting.
Immunotherapy (in combination with chemotherapy) is available for those with advanced TNBC that express PD-L1 and has shown a significant overall survival benefit in patients with CPS ≥ 10%2,3,4. However, the impact of checkpoint inhibitors (anti-PD1/PDL1 antibodies) on survival of the overall population of patients with TNBC is modest. Classic chemotherapeutic agents, such as taxanes, anthracyclines and platinum-agents are the backbone of the first-line treatment of TNBC patients. Although response is frequent, TNBC relapse rapidly, and over time resistance to chemotherapy emerges5,6,7. The only approved targeted drug in a later line treatment setting is sacituzumab govitecan, an antibody–drug conjugate, which led to improved survival in a recent phase III trial8. Overall, treatment options remain limited and long-term remissions are unfortunately not seen with TNBC. Thus, there is a great demand for novel and improved therapeutic strategies in this patient group.
Liposomal encapsulation of drugs, in particular doxorubicin, is used to alter the tissue distribution and pharmacokinetics of the drug, increasing its therapeutic index by making use of the hyperpermeability of vascular structures in the proximity of neoplastic tissue. In clinical settings, pegylated liposomal doxorubicin has shown efficacy, first in the treatment of Kaposi's sarcoma9, and subsequently in metastatic or recurrent BC, ovarian cancer, multiple myeloma and other malignancies. In patients with metastatic BC, objective response rates (ORR) ranging from 5 to 33% have been reported10.
In order to achieve better efficacy and reduce toxicity, more specific delivery of liposomal doxorubicin to the target cells would be desirable. Up to 70% of TNBC express the epidermal growth factor receptor (EGFR), a tyrosine kinase receptor of the ErbB family, which is abnormally activated in many epithelial tumors11, thus making EGFR a promising target for specific delivery of anti-cancer drugs. EGFR can be targeted by cetuximab, an EGFR-binding monoclonal antibody (mAb), which is an established treatment option in patients with colorectal and head-and-neck cancer. Unfortunately, the use of anti-EGFR-directed mAbs in BC, either alone or in combination with chemotherapy, has shown disappointing results and, thus, does not play a role in clinical routine12,13.
While blocking the EGF receptor by a mAb does not lead to clinical benefit so far, we hypothesized that EGFR remains a valid target for drug delivery systems in breast cancer, due to the high frequency and expression levels of EGFR on the surface of TNBC tumor cells. Therefore, we constructed anti-EGFR targeted immunoliposomes by covalently inserting cetuximab fragments into the lipid layer of pegylated liposomal doxorubicin, creating a stable and robust drug carrier with a ligand, a mAb fragment, directing the encapsulated doxorubicin towards the target. In a series of preclinical experiments, we have shown that anti-EGFR targeted immunoliposomes may enhance drug efficacy in vivo14 and, perhaps even more importantly, overcome multidrug-resistance in EGFR-overexpressing cancer cells, including in the human breast cancer cell line MDA-MB-23115).
Based on these findings, we performed a classic dose finding phase I trial with this nanocontainer in patients with EGFR-expressing solid tumors. Toxicity was low and there were signs of clinical activity in heavily pretreated patients4,16. In the current trial, SAKK 24/14, we focused this approach on patients with advanced TNBC. TNBC is a suitable entity for targeted delivery of anti-EGFR–Ils-dox: (i) EGFR is often and robustly overexpressed in TNBC, (ii) in vitro studies have provided evidence of high efficacy of anti-EGFR-ILs-dox in EGFR overexpressing cancer cell lines14,15, and (iii) anthracyclines and doxorubicin in particular are widely accepted and active agents for first line palliative therapy in this cancer entity. Furthermore, this group of patients has (iv) a high clinical need for treatment improvements due to limited treatment options and prognosis despite of ongoing advances in the field.
The main objective of this trial, SAKK 24/14, is to determine the efficacy of anti-EGFR-ILs-dox as a first-line therapy option in this patient population.
Methods
Study sites and patient selection
This prospective, proof-of concept, open-label multicenter phase II trial (SAKK 24/14; NCT02833766) was designed with a single-stage single-arm layout. We accrued patients at 12 participating sites across Switzerland.
Patients met inclusion criteria if they presented with metastatic or locally advanced, inoperable TNBC with an EGFR expression of at least (1 +) on immunohistochemistry according to the EGFR pharmDx™ Interpretation Guidelines17. Staining was conducted with the ready-to-use K1492 EGFR pharmDx™ kit for manual use after antigen retrieval for 24 min with the CC1 buffer of Ventana/Roche and incubation for 32 min in the automated immunostainer Benchmark Ultra of Ventana/Roche. Only patients with measurable or evaluable disease, ≥ 18 years, with a WHO performance status of 0–2, and no prior systemic treatment for metastatic or inoperable disease, were considered eligible. Patients with evidence of CNS or leptomeningeal metastases (even if previously treated) or with a history of hematologic or primary solid malignancy (other than TNBC) were excluded (unless in remission for at least 5 years). Inclusion of adequately treated cervical carcinoma in situ or localized non-melanoma skin cancer was permitted. Adjuvant treatment must have been stopped at least 6 months before registration and previous treatment with anthracyclins must not have exceeded 240 mg/m2 of doxorubicin or 450 mg/m2 of epirubicin.
Measurements and procedures
At baseline, medical history and symptoms were collected. Additionally, physical examination, blood analysis (hematology, biochemistry, hepatic and renal), pregnancy test, imaging (CT scan thorax-abdomen-pelvis), echocardiography and an ECG were conducted.
For patients without disease progression, imaging was repeated every 3 months. After progression, survival status and documentation of further antineoplastic treatment was conducted every 6 months.
Intervention
Patients were treated with anti-EGFR-IL loaded with doxorubicin 50 mg/m2 iv on day one of a 28-day cycle. Treatment continued until progression. Anti-EGFR targeted nanocontainer drug compounds were produced by inserting anti-EGFR antibody fragments into the membrane of pegylated liposomes (anti-EGFR-ILs-dox) with the payload consisting of doxorubicin, a standard drug for breast cancer, including TNBC. The GMP-compliant preparation was previously described18.
Efficacy and safety endpoints and statistical considerations
The total accrual duration was expected to be 30 months. The minimum follow-up time after the inclusion of the last patient for the primary analysis is 12 months. The primary analysis was time-driven and planned to take place after at least 42 months from start of the trial. The primary endpoint for this trial was progression-free survival at 12 months (PFS12m). PFS was calculated from the date of registration until progression according to RECIST v1.1 or death of any cause, whichever occurred first. Secondary endpoints include: objective response rate (ORR)—defined as proportion of patients achieving CR or PR (RECIST v1.1) during trial treatment; duration of response (DOR)—defined as time from CR or PR (RECIST v1.1) achievement with investigational therapy, until documented progression, relapse, or death due to disease progression; time to progression (TTP)—defined as time from registration until progression (RECIST v1.1) or death due to PD (equivalent to PFS as all deaths were considered as cancer-related); PFS; overall survival (OS)—defined as time from registration until death from any cause; adverse events (AE).
For an alpha = 0.1 with 80% power 47 patients were needed to test the null hypothesis of ≤ 25% of patients to be progression-free at 12 months against the alternative hypothesis of ≥ 40% of patients being progression free at 12 months [with the reference of 25% for the null hypothesis taken from the TNBC subgroup of the ATHENA trial n = 585 TNBC patients19. For the primary endpoint, the Kaplan–Meier estimator, one-sided 90% confidence interval (CI) and 95% CI are presented. All efficacy endpoints were analyzed based on the full analysis set (FAS, all registered patients, who received at least one dose of trial treatment excluding patients with major eligibility violations). All safety endpoints were analyzed based on the safety set (all patients, who received any dose of trial treatment). Pre-defined subgroup analyses for all efficacy endpoints were repeated for EGFR + versus EGFR++/+++ patients as defined by immunohistochemistry assessment. All analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA) and R 4.0.3 (The R Foundation; www.r-project.org).
GCP statement
This trial was conducted in compliance with the protocol, the current version of the Declaration of Helsinki20, the ICH-GCP21 or ISO EN 14155 (as far as applicable) as well as all national legal and regulatory requirements.
Ethics approval and consent to participate
The study was approved by the ethics committee, EC number 2016-01006, Lead EC Site: Luzerner Kantonsspital Luzern, Switzerland. All participating patients were adults and provided written informed consent.
Results
Patients and treatment
Between October 28, 2016 and October 8, 2019, a total of 48 patients were registered. All 48 patients were female with a median age of 59.5 years at time of registration. 9 patients (19%) had previously received doxorubicin whereas 15 patients (31%) had previously received epirubicin in the adjuvant setting. The patients` baseline characteristics can be found in Table 1.
All 48 patients started treatment (consort diagram in Fig. 1). 35 patients stopped treatment due to progressive disease (PD) (72.9%), 4 patients died (8.3%) and 9 (18.8%) patients stopped treatment due to other reasons, such as patient refusal [2 (4%)], start of a treatment not permitted on trial [2 (4%)], unacceptable toxicity [2 (4%)] and withdrawal by the physician [3 (6%)].
The trial was terminated 2 years after the inclusion of the last patient. The last follow-up visit of the last patient included into the trial was 2.2 years after the patient had been included in the trial. A total of 238 cycles had been administered. In 36 cycles (15%) dose reductions were recorded. 16 patients (33%) received at least one cycle with dose reduction, this was due to toxicity in 11 cases (23%), physician’s decision in 2 cases (4%), patient`s decision in 1 case (2%) and other reasons in 3 cases (6%). The median number of cycles was 4 (1 to 21); the median treatment duration was 12.0 weeks (0.1 to 84.6). The median follow-up time was 3.9 years (95% CI [2.6, 4.5]). Up to the time of analysis, 44 patients underwent follow-up, 37 died during this time (84.1%), 6 patients were alive (13.6%). One patient was lost to follow-up (2.3%) (Fig. 1). 8/48 patients (17%) were EGFR + , 40/48 patients (83%) EGFR++/+++ as defined by immunohistochemistry assessment.
Primary endpoint
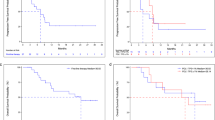
Until the time of analysis, 42 events (5 deaths and 37 disease progressions) had occurred and 5 patients were censored due to starting a second line treatment outside of the trial. The Kaplan–Meier estimator for PFS12m was 13% with a one-sided 90% CI of 7%. The corresponding 95% CI is [5%, 25%].
As the lower boundary of the one-sided 90% confidence interval was smaller than 0.25, the null hypothesis cannot be rejected and the primary endpoint was not reached. Median PFS was 3.5 months, 95% CI [1.9, 5.4] (Fig. 2).
This was also observed in the subgroup analysis according to EGFR expression: PFS12m was 13%, 95% CI [1%, 42%] in the EGFR + subgroup and 13%, 95% CI [4%, 26%] in the EGFR++/+++ subgroup (Fig. 3).
Secondary endpoints
The results of the analyses conducted to assess the secondary endpoints are comprised in Table 2.
Assessment of the ORR showed no complete response (CR). 7/48 patients achieved a partial response (15%), and the majority of patients either had stable disease (SD) or disease progression (PD), regardless of EGFR expression status. Similarly, median OS did not differ between the FAS, the EGFR+ and EGFR++/+++ subgroup.
Safety evaluation
Over the whole course of therapy, treatment-related grade 1, 2, 3 and 4 AEs were observed in 16.7%, 25.0%, 33.3% and 8.3% of the patients, respectively. 16.7% of patients didn’t develop any treatment-related AEs. Serious AEs (SAEs) occurred in the blood and lymphatic system, the gastrointestinal system, or presented as multiorgan failure, disease progression or affections of the nervous and the vascular system (Table 3). Lower grade adverse events occurred in the blood and lymphatic system, the nervous system, the vascular system, the gastrointestinal and respiratory system, in form of skin changes and immune system disorders, infections/infestations, as elevation of the transaminases and as anorexia and fatigue.
At the time of the analysis, 41 patients had died, 4 of them during treatment and 37 during the follow-up. 35/41 (85.4%) died from PD, 2/41 (4.9%) died of other (non-drug related) reasons and in 4/41 (9.8%) reason of death was unknown. One trial patient was diagnosed with myelodysplastic syndrome (MDS) about 3.5 years after completing 10 cycles on anti-EGFR-ILs-dox. We interpreted this as a secondary malignancy related to the study drug. The patient started treatment with azacytidine and venetoclax in november 2021. The patient was still alive and the event reported as resolved by the investigator on 10.03.2022. We have no further follow-up information. Otherwise, there were no new toxicity signals compared to the previous phase 1 trial assessing anti-EGFR ILs-dox.
Discussion
Incorporating technological advances, in particular the use of targeted delivery of potent cytotoxic chemotherapy, is under exploration in the treatment of metastatic TNBC. Especially for antibody drug conjugates, outcome benefits for this patient group have been reported: Sacituzumab govitecan, an antibody–drug conjugate coupling a topoisomerase I inhibitor with a humanized antitrophoblast cell-surface antigen 2 (Trop 2) mAbhRS7 IgG1κ, led to improved PFS and OS in patients with previously treated TNBC when compared to the investigator’s choice of treatment8. Despite these advances, there is actually no compound, which promises long-term remission in this hard-to-treat cancer entity.
We have developed anti-EGFR immunoliposomes for the targeted delivery of doxorubicin to EGFR-overexpressing cells. Directed immunoliposomes loaded with a cytotoxic agent follow the same principle as antibody–drug conjugates offering a targeted delivery of a potent drug; however, due to the liposomal encapsulation they alter the tissue distribution and pharmacokinetics of the drug, increasing its therapeutic index, thus providing a unique feature, which could help evolve the landscape of targeted treatments in cancer patients. In addition, the payload carried by an anti-EGFR-ILs nanocarrier is considerably larger than the number of drug molecules used in antibody–drug conjugates. This could potentially further increase the therapeutic efficacy of the compound. In the present trial, we have investigated an anti-EGFR-ILs-dox in a cohort of patients with advanced TNBC. Liposomal encapsulation of doxorubicin and targeted delivery of the compound to EGFR overexpressing breast cancer cells was hypothesized to improve efficacy while at the same time causing less safety signals in comparison to free and untargeted application. This is a novel approach, which, to our knowledge, has not yet been assessed in this entity. While the safety profile of the new compound was acceptable and did not differ from previous results with liposomal doxorubicin, the efficacy of anti-EGFR-ILs-dox in the assessed TNBC population was lower than expected. Thus, this trial did not reach its primary endpoint.
Whether the observed limited efficacy of anti-EGFR-ILs-dox in TNBC is due to the compound itself or to the biology of the disease, remains unclear. In metastatic HER2 + BC a greater efficacy of antibody–drug conjugates depending on the cytotoxic agent was observed, suggesting the importance of the drug delivered by directed therapies22. Doxorubicin is a cytotoxic agent classically used in the first line systemic treatment of TNBC, suggesting that the delivered cytotoxic agent used in this trial should be able to elicit a solid treatment response. If we assume that doxorubicin is active, this leads to the question whether EGFR is a suitable target for delivery within this entity. Possibly, tumor heterogeneity might lead to an under- or overestimation of EGFR-expression and thus to a suboptimal delivery of the compound in vivo. In addition, immunohistochemistry as the method of assessment of EGFR expression might not differentiate the biological characteristics, in particular its density on the cell surface and the recirculation of the target in the interior of the cell, with adequate accuracy, thus, making the correlation between EGFR expression and treatment response elusive.
Taken together, there are no signals of efficacy to motivate further development pf anti-EGFR-ILs-dox for treatement of TNBC.
The question arises whether anti-EGFR-ILs-dox would offer more opportunities in other EGFR-expressing malignancies, where targeting EGFR has already shown anticancer effects. This was assessed by our group in glioblastoma (GBM)23, where EGFR alterations are found in nearly half of the cases. While treatment with a TKI targeting EGFR has not shown convincing results in GBM patients, some efficacy was reported for an antibody–drug conjugate comprising depatuximab—an IgG1 mAb—coupled to the tubulin inhibitor monomethyl auristatin F (MMAF)24. Unfortunately, this could not be confirmed in a first-line trial in combination with temozolomide25.
Anti-EGFR-ILs-dox, however, uses immunoliposomes and, thus has a more extensive payload carrying capacity than other drug conjugates. Indeed, we have recently demonstrated that anti-EGFR-ILs-dox can be safely used to deliver cytotoxic molecules to GBM tissue in patients with relapsed GBM (n = 9) harboring an EGFR gene amplification23. This may warrant further clinical exploration.
Conclusions
In summary, this trial investigated the role of anti-EGFR-ILs-dox in TNBC. The main limitation of this study is its one-armed design. We addressed this by using previous data from the ATHENA trial as a comparator, which is, however, a historical data set. Although safe, based on the negative efficacy results of this trial, anti-EGFR-ILs-dox should not be further developed for TNBC. Its potential role in other EGFR-expressing malignancies, such as head and neck cancer and colorectal cancer, will need further assessment in other clinical trials.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AE:
-
Adverse Event
- Anti-EGFR-IL-dox:
-
Anti-EGFR immunoliposomes loaded with doxorubicin
- CI:
-
Confidence Interval
- CNS:
-
Central Nervous System
- CR:
-
Complete Response
- CT:
-
Computed Tomography
- DOR:
-
Duration of Response
- ECG:
-
Electrocardiogram
- EGFR:
-
Epidermal Growth Factor Receptor
- ER:
-
Estrogen Receptor
- FAS:
-
Full Analysis Set
- GMB:
-
Glioblastoma
- GMP:
-
Good Manufacturing Practice
- HER2:
-
Human Epidermal Growth Factor Receptor 2
- mAb:
-
Monoclonal Antibodies
- MDS:
-
Myelodysplastic Syndrome
- MMF:
-
Monomethyl Auristan F
- ORR:
-
Objective Response Rate
- OS:
-
Overall Survival
- PD:
-
Progressive Disease
- PD-L1:
-
Programmed Cell Death Ligand 1
- PFS:
-
Progression-Free Survival
- PR:
-
Progesteron Receptor
- SAE:
-
Serious Adverse Event
- SD:
-
Stable Disease
- TKI:
-
Tyrosin Kinase Inhibitor
- TNBC:
-
Triple Negative Breast Cancer
- TTP:
-
Time to Progression
- WHO:
-
World Health Organization
References
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424 (2018).
Cortes, J. et al. KEYNOTE-355 Investigators. Pembrolizumab plus chemotherapy in advanced triple-negative breast cancer. N. Engl. J. Med. 387(3), 217–226 (2022).
Schmid, P. et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N. Engl. J. Med. 379, 2108–2121 (2018).
Cortes, J. et al. Pembrolizumab plus chemotherapy versus placebo plus chemotherapy for previously untreated locally recurrent inoperable or metastatic triple-negative breast cancer (KEYNOTE-355): A randomised, placebo-controlled, double-blind, phase 3 clinical trial. Lancet 396(10265), 1817–1828 (2020).
Liedtke, C. et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J. Clin. Oncol. 26, 1275–1281 (2008).
Foulkes, W. D. et al. Triple-negative breast cancer. N. Engl. J. Med. 363(20), 1938–48.363 (2010).
Dent, R. et al. Triple-negative breast cancer: Clinical features and patterns of recurrence. Clin. Cancer Res. 13(15 Pt 1), 4429–4434 (2007).
Bardia, A. et al. Sacituzumab govitecan in metastatic triple-negative breast cancer. N. Engl. J. Med. 384, 1529–1541 (2021).
Udhrain, A., Skubitz, K. M. & Northfelt, D. W. Pegylated liposomal doxorubicin in the treatment of AIDS-related Kaposi’s sarcoma. Int. J. Nanomed. 2(3), 345–352 (2007).
Verma, S. et al. Metastatic breast cancer: The role of pegylated liposomal doxorubicin after conventional anthracyclines. Cancer Treat. Rev. 34(5), 391–406 (2008).
Zakaria, Z. et al. Epidermal growth factor receptor (EGFR) gene alteration and protein overexpression in Malaysian triple-negative breast cancer (TNBC) cohort. Onco Targets Ther. 12, 7749–7756 (2019).
O’Donovan, N. & Crown, J. EGFR and HER2 antagonists in breast cancer. Anticancer Res. 27, 1285–1294 (2007).
Carey, L. A. et al. TBCRC 001: randomized phase II study of cetuximab in combination with carboplatin in stage IV triple-negative breast cancer. J. Clin. Oncol. 30(21), 2615–2623 (2012).
Mamot, C. et al. Epidermal growth factor receptor-targeted immunoliposomes significantly enhance the efficacy of multiple anticancer drugs in vivo. Cancer Res. 65(24), 11631–11638 (2005).
Mamot, C. et al. Immunoliposomal delivery of doxorubicin can overcome multidrug resistance mechanisms in EGFR-overexpressing tumor cells. J. Drug Target. 20(5), 422–432 (2012).
Mamot, C. et al. Tolerability, safety, pharmacokinetics, and efficacy of doxorubicin-loaded anti-EGFR immunoliposomes in advanced solid tumours: A phase 1 dose-escalation study. Lancet Oncol. 13(12), 1234–1241 (2012).
DAKO. EGFR pharmDx TM interpretation manual pathology for in vitro diagnostic use. FDA-approved as an aid in identifying colorectal cancer patients eligible for treatment with Erbitux ® (cetuximab) and Vectibix TM (panitumumab). EGFR pharmDxTM Interpretation Manual. https://www.agilent.com/cs/library/usermanuals/public/08052_egfr_pharmdx_interpretation_manual.pdf, accessed 12 Sept 2022.
Wicki, A., Ritschard, R. & Loesch, U. Deuster S et al Large-scale manufacturing of GMP-compliant anti-EGFR targeted nanocarriers: Production of doxorubicin-loaded anti-EGFR-immunoliposomes for a first-in-man clinical trial. Int. J. Pharm. 484, 8–15 (2015).
Thomssen, C. et al. First-line bevacizumab-containing therapy for triple-negative breast cancer: Analysis of 585 patients treated in the ATHENA study. Oncology 82(4), 218–227 (2012).
World Medical Association (WMA). WMA declaration of Helsinki-ethical principles for medical research involving human subjects. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/, accessed 12 Sept 2022.
International council for Harmonisation of technical requirements for pharmaceuticals for human use (ICH). ICH Harmonised Guideline Integrated Addendum to ICH E6(R1): Guideline for good clinical practicee6(R2). https://database.ich.org/sites/default/files/E6_R2_Addendum.pdf (2016), accessed 12 Sept 2022.
Cortés, J. et al. Trastuzumab deruxtecan versus trastuzumab emtansine for breast cancer. N. Engl. J. Med. 386, 1143–1154 (2022).
Kasenda, B. et al. Targeting immunoliposomes to EGFR-positive glioblastoma. ESMO Open 7(1), 100365 (2022).
Van Den Bent, M. et al. INTELLANCE 2/EORTC 1410 randomized phase II study of Depatux-M alone and with temozolomide vs temozolomide or lomustine in recurrent EGFR amplified glioblastoma. Neuro Oncol. 22, 684–693 (2020).
Narita, Y. et al. Safety and efficacy of depatuxizumab mafodotin in Japanese patients with malignant glioma: A nonrandomized, phase 1/2 trial. Cancer Sci. 112, 5020–5033 (2021).
Acknowledgements
Merrimack has provided liposomal doxorubicin for this trial. The trial was run on behalf of the Swiss Group of Clinical Cancer Research (SAKK).
Funding
The trial was supported by Merrimack and research agreements with the following institutions: Swiss State Secretary for Education, Research and Innovation (SERI), Swiss Cancer Research Foundation (SCS) and Swiss Cancer League (SCL), and a grant by The Rising Tide Foundation.
Author information
Authors and Affiliations
Contributions
A.W. conception and design of the study, grant applications for third-party funding, production of the interventional compound, interpretation of the data and substantial review of the work, writing of the article. C.M. conception and design of the study, grant applications for third-party funding, production of the interventional compound, interpretation of the data and substantial review of the work, writing of the article. C.R. conception and design of the study, interpretation of the data and substantial review of the work, writing of the article. R.W. conception and design of the study, interpretation of the data and substantial review of the work, writing of the article. A.T. and E.C.O. immunohistochemically stained the study cases for EGFR and morphologically analyzed its expression according to the EGFR pharmDx criteria, review of the work. Q.L. and L.H.: conception of design of the study, statistical analysis of data, writing of the article. D.B.: conception of design of the study, interpretation of data. R.R., S.D. and M.S.: production of the investigational compound, quality assurance of the compound. L.B., U.H.S., S.R., K.Z., R.v.M., K.J.D., U.N., A.B., C.A., V.M.A., Z.U., C.C.: interpretation of data, writing or substantial review of the article. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
K. Dedes: advisory honoraria: AstraZeneca, Daiichi, Novartis. The other authors declare that they have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mamot, C., Wicki, A., Hasler-Strub, U. et al. A multicenter phase II trial of anti-EGFR-immunoliposomes loaded with doxorubicin in patients with advanced triple negative breast cancer. Sci Rep 13, 3705 (2023). https://doi.org/10.1038/s41598-023-30950-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-30950-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.