Abstract
The relationship between protein intake and mortality is still controversial. We prospectively examined the associations of dietary protein sources with all-cause mortality risk in the Isfahan cohort study (ICS). A total of 5431 participants, aged ≥ 35 years, were enrolled in the ICS, in 2001 and followed through 2013. The frequency of protein intakes from different sources was estimated through a validated food frequency questionnaire at baseline. Any new case of death was recorded over the follow-up duration. Hazard ratio (HR)s and 95% confidence interval (CI)s were estimated through Cox proportional hazards regression models. During a median follow-up of 11.3 years, 483 deaths were documented. Higher intakes of plant proteins (HR = 0.64, 95% CI 0.46, 0.91) and animal proteins (HR = 1.52, 95% CI 1.13, 2.05) were associated with a decreased and increased risk of mortality, respectively. Additional adjustment for some mediators did not considerably affect the associations for animal protein (HR = 1.55, 95% CI 1.15, 2.09), whereas led to a tendency towards lower risk for plant protein in the top quintile compared with the bottom one (HR = 0.67, 95% CI 0.48, 0.95; P trend = 0.06). Among specific major sources, higher intakes of nuts and fish were associated with a 27% (95% CI 0.58, 0.93) and 21% (95% CI 0.62, 1.01) lower risk of mortality, respectively. The inverse association between plant protein and mortality risk might be mediated by some metabolic disorders. However, our results suggest an independent positive association for animal protein and all-cause mortality.
Similar content being viewed by others
Introduction
Seventy percent of deaths occurred in world in 2013 have been attributed to chronic diseases1 which can be delayed by lifestyle modifications (i.e. dietary behaviors), even in the absence of any direct and clear biological mechanism. To date, many studies have investigated the effect of protein amount on cardiometabolic health2; however, it seems that protein type is matter much more than the quantity of protein3, given that they are consumed along with specific clusters of macronutrients, micronutrients, antioxidant, and phytochemical and convey different amino acids.
A large body of evidence supports the benefits of plant proteins in reducing risk of chronic diseases4,5,6,7,8, whereas red meat and processed meat may contribute to increased risk of various metabolic disorders9. Moreover, several prospective cohort studies have examined dietary protein sources in relation to mortality risk9,10,11,12,13,14,15,16. Although findings regarding nuts are mostly consistent and suggested an inverse association17, results for legumes, and animal sources of protein are less conclusive18,19,20. For example, legumes in most studies were not associated with mortality21,22, and a meta-analysis suggested just a slight decrease which was dependent on follow-up duration, sample size and geographic region19. Regarding red meat-mortality relation, while a meta-analysis suggested a region-specific association20, another one demonstrated very small inverse with low certainty association18. Likewise, in a recent meta-analysis23, Jayedi et al. showed a marginal inverse association; however, in their subgroup analysis according to the region of study, the association was only significant in Asian countries, but not Westerns. In contrast, higher fish consumption was not associated with the risk of mortality among Iranians in a 11-year follow-up study14.
The association of dietary protein sources with mortality may be influenced by several factors such as lifestyle, dietary pattern, and the contribution of protein sources to daily energy and protein intake. Nevertheless, to our knowledge, only a few studies have investigated these associations in developing countries, where the average per capita meat consumption is considerably lower than developed countries (25 vs. 88 kg/year)24. Therefore, we aim to further investigate the associations of dietary protein sources, including meat, fish, poultry, egg, dairy products, nuts and legumes, with all-cause mortality, using data from Isfahan cohort study (ICS).
Methods and materials
Study population
The ICS is an ongoing population-based longitudinal cohort study25, established in 2001 and includes 6504 adults (3168 men and 3336 women) aged ≥ 35 years. The ICS was conducted in three districts of central Iran and participants were recruited using stratified cluster random sampling method (2153 from Isfahan, 1028 from Najaf-Abad, and 3323 from Arak). Further detailed description about study design has been presented elsewhere25. At baseline, information about lifestyle factors, including dietary intake, was collected using face-to-face interview and participants were followed up biannually for outcomes of interest. In the absence of any cardiovascular event as the primary outcomes of ICS in biannual evaluations, all variables including lifestyle factors were assessed in the next survey after six years of follow-up (2007 and 2013). For our analysis, data from 5584 participants who attended for repeated measurements in both 2007 and 2013, and had complete information on dietary intake, and covariates were included. All participants provided a written informed consent. This study was performed in accordance with the declaration of Helsinki and approved by the Ethics Committee of the Research Council of Isfahan Cardiovascular Research Center, a World Health Organization collaborating center in Isfahan, Iran.
Data collection
At enrolment, trained health professionals completed a general questionnaire about demographic, socioeconomic variables, lifestyle factors including dietary intakes, smoking status (current, former, or never), and physical activity, and medical history (e.g. the history of dyslipidemia, diabetes mellitus, hypertension, and medicine use) through a 30-min home interview26,27. Physical activity was assessed using a validated questionnaire28. Height and weight were measured using standard protocols, and body mass index (BMI) was measured by dividing weight in kg by height in meters squared.
Dietary assessment
The habitual dietary intake of participants over the year preceding baseline, 2007 and 2013 was assessed using a validated 48-item food frequency questionnaire (FFQ)29,30. FFQ was completed by trained health professionals through face-to-face interviews and participants were asked to report the mean frequency of consumption of each food item in an open-ended format (daily, weekly, or monthly). If one food item was never consumed or less than once a month, they chose “never/seldom” presenting “zero” for frequency of consumption. Our FFQ did not have information about portion sizes; however, our validation study of this FFQ showed that portion sizes varied less than frequencies of consumption for most food items30. Dietary intake was converted into the frequency of consumption per week. Dairy products intake included the frequency intake of milk, yogurt, and cheese. Red meat included all types of beef and lamb, poultry included chicken and turkey. For fish intake, we did not consider canned fish, because its high sodium content could possibly mislead the results.
The validity of FFQ was examined against a single 24-h recall and two food records and demonstrated significant correlation between the frequency of animal protein, plant protein, and dairy products obtained from FFQ and the mean intake values obtained from a dietary recall and records (Spearman’s rank correlation coefficient for: animal protein = 0.294; P = 0.007, plant protein = 0.480; P < 0.001, dairy products = 0.467; P < 0.001, nuts = 0.468; P < 0.001)30.
Ascertainment of deaths
Totally 483 deaths occurred after 11.3 years of follow-up. Information on mortality was gathered based on verbal autopsy from surviving close family members using a structured primary interview in which the first question was ‘is he/she alive?”.
Statistical analysis
To compare general characteristics of participants at recruitment, we categorized participants according to the quantiles of animal (including red meat, poultry, fish, egg, and dairy products), plant (nuts and seeds, and legumes and soy), and total (plant and animal) protein consumption. Continuous and categorical variables were compared using analysis of variance (ANOVA) and chi-square test across the quartiles of dietary protein sources, respectively. Continuous variables were reported as mean ± SD, and categorical variables were described as percent. Age-, sex-, and BMI-adjusted of dietary intakes across the quartiles of dietary protein sources were compared using analysis of covariance (ANCOVA) and expressed as mean ± SE.
Person-years of follow-up was calculated from recruitment until the date of death or last follow-up date (2013), which ever occurred first. Crude and multivariate-adjusted hazard ratios (HRs) and 95% CI for association between dietary protein sources and all-cause mortality were estimated using Cox proportional hazards regression. Model 1 was controlled for age at baseline and sex. Model 2 was additionally adjusted for education and lifestyle factors including smoking, physical activity and BMI. Fruit and vegetables were adjusted beside other confounders in model 3. The mediating effects of hypertension, dyslipidemia and diabetes mellitus were further controlled in model 4. In this study, we used the frequency of consumption and their range was small when various protein sources were separately analyzed. Therefore, to have enough participants in each category, analysis based on individual dietary protein sources was performed based on the tertile of consumption frequency.
Results
During 11.3 years of follow-up with 57,122.7 person-years, 483 deaths were documented in the ICS. The frequency consumption of animal and plant proteins was on average 9.7 ± 5.1 and 4.6 ± 3.6 times/week, respectively. Table 1 displays general characteristics of participants at baseline across the quintiles of animal, plant and total proteins. Compared with participants who consumed lower amounts of any of the animal, plant or total protein sources, those with higher consumption were more likely to be younger, male, physically active, highly educated, and current smoker and to have lower BMI and waist circumference. In addition, diabetes mellitus (DM), hypertension (HTN) and dyslipidemia were less frequent in higher quintiles of all three animal, plant and total protein sources compared with the lowest quintile.
The age- and sex-adjusted frequencies of different food items by the categories of animal, plant and total proteins are illustrated in Table 2. Participants with higher consumption of protein from each source had higher intake of all food groups, including fruit and vegetables, cereals, red meat, processed meat, poultry, fish, white meat, high fat dairy products, egg, nuts and seeds, and legumes and soy. The one exception for these associations was poultry across three quintiles of plant protein, which did not significantly differ across quintiles.
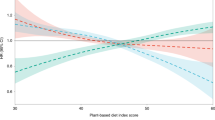
Table 3 shows the HRs and 95% CIs for all-cause mortality across the quintiles of animal, plant and total protein. In the crude model, compared with the first quintile, HRs in the highest quintile were 0.78 (95% CI 0.59, 1.04; P = 0.011) for animal protein, 0.33 (95% CI 0.24, 0.64; P < 0.0001) for plant protein and 0.53 (95% CI 0.40, 0.71; P < 0.0001) for total protein. Adjustment for age and sex, and education beside lifestyle factors including smoking, BMI and physical activity weakened the associations for all three sources and led to a non-significant association for animal and total protein. However, further control for fruit and vegetables resulted in a significant increase in the mortality risk for animal proteins when comparing the top with the bottom quintile (HR = 1.52, 95% CI 1.13, 2.05; P = 0.03). Significant inverse association was also observed between plant protein and mortality risk even after additional adjustment for fruit and vegetables (HR = 0.64, 95% CI 0.46, 0.91; P = 0.03). In model 4, adjustment for some metabolic disorders as mediators, such as diabetes, hypertension and dyslipidemia, slightly increased the association for animal sources (HR = 1.55, 95% CI 1.15, 2.09; P = 0.02), but led to a tendency towards lower risk of mortality in participants in the top quintile of plant protein compared with the bottom one (HR = 0.67, 95% CI 0.48, 0.95; P = 0.06). The association remained no longer significant for total protein in all adjusted models and just moderately changed in different models (model 4, HR for fifth quintile = 1.22, 95% CI 0.89, 1.67; P = 0.23). When animal, plant and total protein were considered a continuous variable, the same results were obtained (Table 3).
As shown in Table 4, in the crude model, a lower risk of 21% for red meat (95% CI 0.63, 0.99; P = 0.046), 58% for processed meat (95% CI 0.33, 0.53; P < 0.0001), 42% for fish (95% CI 0.46, 0.73; P < 0.0001), 24% for egg (95% CI 0.57, 1.00; P = 0.047), 63% for nuts and seeds (95% CI 0.30, 0.47; P < 0.0001) and 31% for legumes and soy (95% CI 0.56, 0.86; P < 0.0001) was seen in the top tertile compared with the first one. However, after adjustment for potential confounders, all significance disappeared except for nuts and seeds, which remained strongly correlated with lower risk of mortality (T3: HR = 0.72, 95% CI 0.56, 0.91 and T2: HR = 0.83, 95% CI 0.62, 1.11; P = 0.005). Additional adjustment for mediators did not considerably change these associations. However, the results changed for fish and led to a lower risk in the top tertile compared with the bottom one (HR = 0.79, 95% CI 0.62, 1.01; P = 0.04). Given that only high-fat dairy products were considered in our FFQ, just above 71% of participants did not consume them and therefore we were not able to examine the association for it separately across tertile. According to the median of high fat dairy products, 334 and 113 deaths occurred in the first and the second medians, respectively. In addition, those in the higher median, compared with those in the lower median, had no increased risk of death in any of the models (HR in crude model = 0.85, 95% CI 0.69, 1.05, HR in model adjusted for potential confounders = 0.94, 95% CI 0.76, 1.18, and HR in model additionally adjusted for mediators = 0.99, 95% CI 0.79, 1.24).
Additional analysis revealed that after adjustment for potential confounders, each time increase in the frequency of various protein sources was not related to the risk of all-cause mortality (Table 4). The corresponding values for high-fat dairy products were: HR = 1.05, 95% CI 1.00, 1.10; P = 0.06.
Discussion
In the current prospective cohort study of Iranians, after 11 years of follow-up, we observed a positive association for animal protein but an inverse association for plant protein sources with all-cause mortality, though the association between plant protein and mortality risk was mediated by some metabolic disorders. Total protein was not significantly related to the risk of all-cause mortality. Further analyses based on the type of protein from different sources revealed inverse associations between nuts and fish intake and mortality risk which were not influenced by various confounders and mediators.
To date, several epidemiological studies have investigated the association between dietary protein sources and mortality. Consistently, in studies which protein sources were examined as plant or animal, an inverse association for plant sources and a direct association for animal sources have been reported15,31,32,33. Nevertheless, when specific major proteins sources were separately investigated in relation to mortality risk, contradictory results have been found. For example, higher red meat intake was associated with increased risk of mortality in American adults, Finish men and Swedish men and women16,33,34, but not in the Netherlands Cohort Study and the Golestan Cohort Study in Iran10,14, like our findings. While poultry10, dairy products35 and egg14 were associated with lower risk of overall mortality in some studies, there are some studies which failed to find any significant association for these sources33,36,37 which is in concordance with ours. Similar discrepancy is also observed for fish. Although an earlier study among Iranians reported a lower risk for cancer death by higher fish consumption, they found no association for fish and all-cause mortality. Similarly, in Finnish men a null association was found33 but in the Netherlands Cohort Study10, a direct association was obseved. Furthermore, nuts and legumes have been associated with lower mortality risk in some studies10,14, but not all21,22,38.
The reasons underlying different association between protein sources and overall mortality might be related to their relation with diet quality6. Consuming less than 70% of total protein from animal sources was associated with greater healthy eating index score in young adults39. Additionally, each protein source is an exclusive package of nutrients. For instance, animal protein usually comes with saturated fatty acids and detrimental amino acids including branched chain and aromatic amino acids, but plant protein is accompanied by antioxidants, phytochemicals, polyunsaturated fatty acids, fiber, and a combination of beneficial amino acids like arginine, cysteine, glutamine/glutamate, and glycine6. Besides, protein foods preference, the foods served with them6, and other health-related factors can be affected by behavioral and sociodemographic factors40,41. For example, in France, higher fish consumption was associated with better sociodemographic status, more physical activity, less smoking and eating 3 meals a day more frequently6, and in the US eating fish was associated with lower intake of dairy foods and red meat but higher intakes of vegetables42.
Despite potential mechanisms underlying the positive link between red meat and mortality, i.e. higher saturated fatty acids and heme iron content, we found no significant association. This might be explained by the low average intake of red meat in Iran compared with Western countries which mostly reported a positive link9,10,43. Red meat may also interact with other dietary factors34,44. In a Swedish cohort study, when processed meat intake was < 20 g/days, unprocessed meat was not associated with the risk of mortality44. Moreover, although higher meat intake can increase the production of carcinogenic N-nitroso compounds45, fruit and vegetables, rich in antioxidants compound, restrain their harm effects46, and may potentially affect the final risk. Therefore, it is relevant to consider the confounding effect of these factors. However, despite a null association between various sources of animal proteins and mortality, we found a direct link for animal protein sources that might be owing to the combined effect of red meat and egg.
This study has several limitations. First, to assess dietary intakes, we used a FFQ without portion sizes which does not allow us to determine the exact amount of protein foods as well as energy intake. Therefore, it was not possible to us to control the confounding effect of energy but to deal with this issue, we adjusted BMI as surrogate. Second, despite using a validated FFQ in this study, measurement errors due to recall bias of habitual intake may occur which can attenuate associations47. Moreover, all the Spearman correlation coefficients are less than 0.5 in our study population. This means that observed associations are weaker and somewhat conservative than those achieved by true nutrient indices measured by gold standard methods, such as weighted food records or biomarkers48. Third, although we adjusted our results for various confounders, the confounding effect of residual or bias related to unknown or unmeasured factors cannot be completely ruled out. Fourth, adjustment for some mediating factors like metabolic disorders in the last model may be an over adjustment and underestimates the true association. Finally, alcohol consumption was not adjusted in the present study, however, since this study was conducted on a Muslim population. Its consumption cannot be concern. Besides, our study has its own strengths including its large sample size, longitudinal design and the high between-individual variety in various specific major proteins sources. In addition, data were collected from both rural and urban areas in three different counties which can, at least to some extent, reveal dietary diversity, especially those related to the frequency consumption of various dietary proteins sources, in this population. This, consequently, improve the generalizability of our findings to populations with similar characteristics to our population.
In summary, this prospective cohort study indicates an inverse association for fish and nuts with all-cause mortality even after control for potential confounders. In addition, despite a tendency toward lower risk of all-cause mortality in individuals with higher plant protein consumption after adjustment for metabolic disorders, the direct association for animal protein remained strongly significant. Further well designed randomized clinical trial studies are suggested to examine casualty effects of protein intake on death and confirm our findings.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015(385), 117–171 (2014).
Wycherley, T. P., Moran, L. J., Clifton, P. M., Noakes, M. & Brinkworth, G. D. Effects of energy-restricted high-protein, low-fat compared with standard-protein, low-fat diets: A meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 96(6), 1281–1298 (2012).
Rutherfurd-Markwick, K. J. Food proteins as a source of bioactive peptides with diverse functions. Br. J. Nutr. 108(Suppl 2), S149–S157 (2012).
Fan, M., Li, Y., Wang, C., Mao, Z., Zhou, W., Zhang, L., et al. Dietary protein consumption and the risk of type 2 diabetes: ADose-response meta-analysis of prospective studies. Nutrients. 11(11) (2019).
Viguiliouk, E. et al. Effect of replacing animal protein with plant protein on glycemic control in diabetes: A systematic review and meta-analysis of randomized controlled trials. Nutrients 7(12), 9804–9824 (2015).
Mariotti, F. Animal and plant protein sources and cardiometabolic health. Adv. Nutr. 10(4), S351–S366 (2019).
Shang, X. et al. Dietary protein from different food sources, incident metabolic syndrome and changes in its components: An 11-year longitudinal study in healthy community-dwelling adults. Clin. Nutr. 36(6), 1540–1548 (2017).
Tielemans, S. M., Kromhout, D., der Altorf-van Kuil, W. & Geleijnse, J. M. Associations of plant and animal protein intake with 5-year changes in blood pressure: The Zutphen Elderly Study. Nutr. Metab. Cardiovasc. Dis. 24(11), 1228–1233 (2014).
Key, T. J. et al. Consumption of meat, fish, dairy products, and eggs and risk of ischemic heart disease. Circulation 139(25), 2835–2845 (2019).
van den Brandt, P. A. Red meat, processed meat, and other dietary protein sources and risk of overall and cause-specific mortality in The Netherlands Cohort Study. Eur. J. Epidemiol. 34(4), 351–369 (2019).
Budhathoki, S. et al. Association of animal and plant protein intake with all-cause and cause-specific mortality. JAMA Intern. Med. 179(11), 1509–1518 (2019).
Tharrey, M. et al. Patterns of plant and animal protein intake are strongly associated with cardiovascular mortality: The Adventist Health Study-2 cohort. Int. J. Epidemiol. 47(5), 1603–1612 (2018).
Li, H., Li, J., Shen, Y., Wang, J. & Zhou, D. Legume consumption and all-cause and cardiovascular disease mortality. Biomed. Res. Int. 2017, 8450618 (2017).
Farvid, M. S. et al. Dietary protein sources and all-cause and cause-specific mortality: The Golestan Cohort Study in Iran. Am. J. Prev. Med. 52(2), 237–248 (2017).
Song, M. et al. Association of animal and plant protein intake with all-cause and cause-specific mortality. JAMA Intern. Med. 176(10), 1453–1463 (2016).
Sinha, R., Cross, A. J., Graubard, B. I., Leitzmann, M. F. & Schatzkin, A. Meat intake and mortality: A prospective study of over half a million people. Arch. Intern. Med. 169(6), 562–571 (2009).
Chen, G. C. et al. Nut consumption in relation to all-cause and cause-specific mortality: A meta-analysis 18 prospective studies. Food Funct. 8(11), 3893–3905 (2017).
Zeraatkar, D. et al. Red and processed meat consumption and risk for all-cause mortality and cardiometabolic outcomes: A systematic review and meta-analysis of cohort studies. Ann. Intern. Med. 171(10), 732–741 (2019).
Schwingshackl, L. et al. Food groups and risk of all-cause mortality: A systematic review and meta-analysis of prospective studies. Am. J. Clin. Nutr. 105(6), 1462–1473 (2017).
Wang, X. et al. Red and processed meat consumption and mortality: Dose–response meta-analysis of prospective cohort studies. Public Health Nutr. 19(5), 893–905 (2016).
van den Brandt, P. A. The impact of a Mediterranean diet and healthy lifestyle on premature mortality in men and women. Am. J. Clin. Nutr. 94(3), 913–920 (2011).
Bongard, V. et al. Food groups associated with a reduced risk of 15-year all-cause death. Eur. J. Clin. Nutr. 70, 715–722 (2016).
Jayedi, A., Shab-Bidar, S., Eimeri, S. & Djafarian, K. Fish consumption and risk of all-cause and cardiovascular mortality: a dose-response meta-analysis of prospective observational studies. Public Health Nutr. 21(7), 1297–1306 (2018).
http://www.fao.org/3/y4252e/y4252e05b.htm. Accessed 7.17.2021.
Sarrafzadegan, N. et al. The Isfahan cohort study: Rationale, methods and main findings. J. Hum. Hypertens. 25(9), 545–553 (2011).
Sarrafzadegan, N. et al. Do lifestyle interventions affect dietary diversity score in the general population?. Public Health Nutr. 12(10), 1924–1930 (2009).
Sarrafzadegan, N. et al. Outcomes of a comprehensive healthy lifestyle program on cardiometabolic risk factors in a developing country: The Isfahan Healthy Heart Program. Arch Iran Med. 16(1), 4–11 (2013).
Talaei, M. et al. Physical activity, sex, and socioeconomic status: A population based study. ARYA Atheroscler. 9(1), 51–60 (2013).
Mohammadifard, N. et al. Using factor analysis to identify dietary patterns in Iranian adults: Isfahan Healthy Heart Program. Int. J. Public Health. 57(1), 235–241 (2012).
Mohammadifard, N. et al. Validation of a simplified food frequency questionnaire for the assessment of dietary habits in Iranian adults: Isfahan Healthy Heart Program, Iran. ARYA Atheroscler. 11(2), 139–146 (2015).
Naghshi, S., Sadeghi, O., Willett, W. C. & Esmaillzadeh, A. Dietary intake of total, animal, and plant proteins and risk of all cause, cardiovascular, and cancer mortality: Systematic review and dose-response meta-analysis of prospective cohort studies. BMJ 370, m2412 (2020).
Qi, X. X. & Shen, P. Associations of dietary protein intake with all-cause, cardiovascular disease, and cancer mortality: A systematic review and meta-analysis of cohort studies. Nutr. Metab. Cardiovasc. Dis. 30(7), 1094–1105 (2020).
Virtanen, H. E. K. et al. Dietary proteins and protein sources and risk of death: The Kuopio Ischaemic Heart Disease Risk Factor Study. Am. J. Clin. Nutr. 109(5), 1462–1471 (2019).
Bellavia, A., Stilling, F. & Wolk, A. High red meat intake and all-cause cardiovascular and cancer mortality: Is the risk modified by fruit and vegetable intake?. Am. J. Clin. Nutr. 104(4), 1137–1143 (2016).
Mazidi, M. et al. Consumption of dairy product and its association with total and cause specific mortality—A population-based cohort study and meta-analysis. Clin. Nutr. 38(6), 2833–2845 (2019).
Mazidi, M., Katsiki, N., Mikhailidis, D. P., Pencina, M. J. & Banach, M. Egg consumption and risk of total and cause-specific mortality: An individual-based cohort study and pooling prospective studies on behalf of the lipid and blood pressure meta-analysis collaboration (LBPMC) Group. J. Am. Coll. Nutr. 38(6), 552–563 (2019).
Zamora-Ros, R. et al. Moderate egg consumption and all-cause and specific-cause mortality in the Spanish European Prospective into Cancer and Nutrition (EPIC-Spain) study. Eur. J. Nutr. 58, 2003–2010 (2019).
Gopinath, B., Flood, V. M., Burlutksy, G. & Mitchell, P. Consumption of nuts and risk of total and cause-specific mortality over 15 years. Nutr. Metab. Cardiovasc. Dis. 25(12), 1125–1131 (2015).
Sokolowski, C. M., Higgins, S., Vishwanathan, M. & Evans, E. M. The relationship between animal and plant protein intake and overall diet quality in young adults. Clin. Nutr. 39(8), 2609–2616 (2020).
Gavelle, E., Huneau, J.F., Mariotti, F. Patterns of protein food intake are associated with nutrient adequacy in the general French adult population. Nutrients. 10(2) (2018).
Touvier, M. et al. Variations in compliance with recommendations and types of meat/seafood/eggs according to sociodemographic and socioeconomic categories. Ann. Nutr. Metab. 56(1), 65–73 (2010).
Ascherio, A., Rimm, E. B., Stampfer, M. J., Giovannucci, E. L. & Willett, W. C. Dietary intake of marine n-3 fatty acids, fish intake, and the risk of coronary disease among men. N. Engl. J. Med. 332(15), 977–982 (1995).
Sun, Y. et al. Association of major dietary protein sources with all-cause and cause-specific mortality: Prospective cohort study. J. Am. Heart Assoc. 10(5), e015553 (2021).
Bellavia, A., Larsson, S. C., Bottai, M., Wolk, A. & Orsini, N. Differences in survival associated with processed and with nonprocessed red meat consumption. Am. J. Clin. Nutr. 100, 924–929 (2014).
Hughes, R., Cross, A. J., Pollock, J. R. & Bingham, S. Dose-dependent effect of dietary meat on endogenous colonic N-nitrosation. Carcinogenesis 22(1), 199–202 (2001).
Abraham, S. K. & Khandelwal, N. Ascorbic acid and dietary polyphenol combinations protect against genotoxic damage induced in mice by endogenous nitrosation. Mutat. Res. 757(2), 167–172 (2013).
Park, Y. M. et al. Obesity mediates the association between mediterranean diet consumption and insulin resistance and inflammation in US adults. J. Nutr. 147(4), 563–571 (2017).
Rosner, B. & Gore, R. Measurement error correction in nutritional epidemiology based on individual foods, with application to the relation of diet to breast cancer. Am. J. Epidemiol. 154(9), 827-835.s (2001).
Acknowledgements
We greatly appreciate the help from Mrs. Mansoureh Boshtam with her assistance in data collection. We would like to express our thanks to the staff of surveillance department that assisted us to find death records. The baseline survey was supported by Grant number 31309304. The Isfahan Cardiovascular Research Center, affiliated to Isfahan University of Medical Sciences funded the biannual follow-ups.
Funding
The baseline survey was supported by Grant number 31309304. The Isfahan Cardiovascular Research Center, affiliated to Isfahan University of Medical Sciences funded the biannual follow-ups.
Author information
Authors and Affiliations
Contributions
The authors’ responsibilities were as follows— N.M., J.N., M.S., H.R., and N.S.: contributed to the study concepts and design, data collection, and draft of the manuscript; F.H. and P.Z.: contributed to the statistical analysis; F.H. and N.M. contributed to data interpretation, and manuscript draft; N.M. and N.S. supervised the study; and all authors: approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Haghighatdoost, F., Mohammadifard, N., Zakeri, P. et al. Differences in all-cause mortality risk associated with animal and plant dietary protein sources consumption. Sci Rep 13, 3396 (2023). https://doi.org/10.1038/s41598-023-30455-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-30455-9
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.