Abstract
The association between fluid overload and survival has not been well elucidated in critically ill patients with sepsis-induced acute kidney injury (SIAKI) receiving continuous renal replacement therapy (CRRT). We investigated the optimal cutoff value of fluid overload for predicting mortality and whether minimizing fluid overload through CRRT is associated with a survival benefit in these patients. We examined 543 patients with SIAKI who received CRRT in our intensive care unit. The degree of cumulative fluid overload in relation to body weight was expressed as the percentage fluid overload (%FO). %FO was further subdivided into %FO from AKI diagnosis to CRRT initiation (%FOpreCRRT) and total fluid overload (%FOtotal). The best cutoff value of fluid overload for predicting the 28-day mortality was %FOpreCRRT > 4.6% and %FOtotal > 9.6%. Multivariable analysis demonstrated that patients with %FOpreCRRT > 4.6% and %FOtotal > 9.6% were 1.9 times and 3.37 times more likely to die than those with %FOpreCRRT ≤ 4.6% and %FOtotal ≤ 9.6%. The 28-day mortality was the highest in patients with %FOpreCRRT > 4.6% and %FOtotal > 9.6% (84.7%), followed by those with %FOpreCRRT ≤ 4.6% and %FOtotal > 9.6% (65.0%), %FOpreCRRT > 4.6% and %FOtotal ≤ 9.6% (43.6%), and %FOpreCRRT ≤ 4.6% and %FOtotal ≤ 9.6% (22%). This study demonstrated that fluid overload was independently associated with the 28-day mortality in critically ill patients with SIAKI. Future prospective studies are needed to determine whether minimizing fluid overload using CRRT improves the survival of these patients.
Similar content being viewed by others
Acute kidney injury (AKI) is a common and serious complication that occurs in over 50% of critically ill patients1. Mortality among critically ill patients with AKI has been reported to be more than 50% and as high as 80% in patients requiring renal replacement therapy (RRT)2,3,4. Sepsis is the leading cause of AKI in patients admitted to the intensive care unit (ICU), accounting for approximately 50% of all cases of AKI3,5.
In critically ill patients, hemodynamic instability requires aggressive fluid resuscitation, which leads to fluid overload. In patients with sepsis, sepsis itself contributes to the development of fluid overload. Inflammatory cascading reactions including a variety of mediators that occurs in sepsis increase microvascular permeability and capillary leakage which, in turn, result in interstitial fluid accumulation, loss of protein, and tissue edema6. Fluid overload is a common complication in critically ill patients with AKI and affects approximately two-thirds of patients with AKI requiring RRT7,8. Fluid overload has also been reported to be associated with increased mortality and reduced renal recovery in patients with AKI9,10,11,12,13,14,15. Patients with sepsis-induced AKI (SIAKI) are particularly at risk of fluid overload because early aggressive fluid resuscitation has been the mainstay of standard care for patients with severe sepsis and septic shock since the results of early goal-directed therapy (EGDT) have been published16.
Though conservative fluid management and diuretics have been generally proposed to avoid fluid overload, continuous RRT (CRRT) has been considered an essential strategy for fluid management in critically ill patients with AKI. Previous studies also showed that fluid removal using CRRT was associated with improved outcomes in critically ill patients with AKI7,8,17.
We previously reported that fluid overload was associated with increased mortality in critically ill patients with AKI receiving CRRT13. In that study, subgroup analysis showed that the adverse effect of fluid overload on survival was evident in patients with SIAKI13. However, our previous study had a limitation owing to the small number of patients with SIAKI (n = 201), and studies on the effect of fluid overload on mortality in critically ill patients with SIAKI receiving CRRT have been scarce. Based on our previous study, the present study was conducted with the following aims. Aim 1: to find the optimal cutoff value of the degree of fluid overload for predicting mortality in critically ill patients with SIAKI receiving CRRT. Aim 2: to find an independent association between fluid overload and mortality in these patients. Aim 3: to determine whether minimizing fluid overload through CRRT is associated with decreased mortality.
Methods
Study population
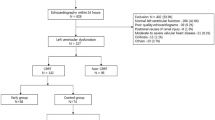
We conducted a single-center, retrospective cohort study of patients admitted to the ICU at Pusan National University Yangsan Hospital between 2015 and 2020. A total of 647 adult patients (age ≥ 18 years) with sepsis and AKI who underwent CRRT were initially recruited. The exclusion criteria were as follows: (a) end-stage renal disease on chronic dialysis or history of kidney transplantation; (b) missing data related to admission weight or fluid balance, and (c) mortality within 24 h of CRRT initiation. Finally, a total of 543 patients were examined (Supplementary Fig. S1). All research and data collection processes were conducted in accordance with the Declaration of Helsinki and current ethical guidelines. The study protocol was approved by the hospital’s institutional review board (IRB) (Pusan National University Yangsan Hospital Review Board, IRB No. 05–2021-140). All research and data collection processes were conducted in accordance with the Declaration of Helsinki and current ethical guidelines. The Institutional Review Board of Pusan National University Yangsan Hospital waived the need for informed consent due to the retrospective nature of the analysis, which only used the information available from anonymized medical charts and records.
Data collection
We reviewed electronic medical records. Demographic and clinical data at ICU admission, including age, sex, body weight, comorbid diseases (chronic kidney disease [CKD], hypertension, diabetes, chronic obstructive pulmonary disease [COPD], liver cirrhosis, congestive heart failure, solid cancer, and hematologic cancer), infection source (respiratory, gastrointestinal, urinary tract, and soft tissue), severity of illness (Sequential Organ Failure Assessment [SOFA] score), Acute Physiology and Chronic Health Evaluation II (APACHE II), vasopressor use, and ventilator dependency), mean arterial pressure, fever, heart rate, and oliguria (< 0.5 mL/kg per hour for 6 h before CRRT initiation), were collected. Blood examinations were performed upon ICU admission and included creatinine, blood urea nitrogen, potassium, sodium, leukocyte count, hemoglobin, platelet count, total bilirubin, albumin, prothrombin time (international normalized ratio) (PT [INR]), C-reactive protein, procalcitonin, and lactate. Finally, the intervals between AKI diagnosis and CRRT initiation, CRRT duration, and fluid overload status were investigated.
CRRT protocol
The primary indications for CRRT initiation were medically intractable volume overload, electrolyte imbalance, metabolic acidosis, oliguria with progressive azotemia, and hemodynamic instability in patients with sepsis and AKI. Decisions regarding when to initiate or terminate CRRT and the CRRT setting (target clearance, blood flow, dialysate/replacement fluid rate, and anticoagulation) were made through consultations and discussions with attending nephrologists. All patients received continuous veno-venous hemodiafiltration using Prisma or Prismaflex (Baxter, IL, USA) with an AN-69 polyacrylonitrile membrane dialyzer. A venous catheter for CRRT was inserted into the internal jugular or femoral vein. CRRT was initiated with blood flow, which was gradually increased to 150 mL/min. A CRRT dose of 35–40 mL/kg per hour was prescribed to ensure a delivered CRRT dose of ≥ 35 mL/kg per hour.
Definition and study outcome
Sepsis was defined according to the American College of Chest Physicians/Society of Critical Care Medicine consensus conference criteria18. If patients had a proven or strongly suspected bacterial infection and had at least two of the systemic inflammatory response syndrome criteria (body temperature > 38 °C or < 36 °C, heart rate > 90 bpm, respiratory rate > 20 breaths/min, PaCO2 < 32 mmHg or use of mechanical ventilation, white cell count > 12,000/mm3 or < 4000/mm3, or immature neutrophils > 10%), sepsis was diagnosed. AKI diagnosis was based on the Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guidelines for AKI (increase in serum creatinine ≥ 0.3 mg/dL within 48 h, increase in serum creatinine ≥ 1.5-times the baseline value, or urine volume < 0.5/kg/h for 6 h)19. The primary outcome was the best cutoff value of fluid overload in predicting the 28-day mortality after ICU admission in the study population. The secondary outcome was a comparison of the 28-day mortality between the groups determined according to the best cutoff value of fluid overload.
Fluid status assessment
All available input (intravenous fluid, blood product, total parenteral nutrition, or enteral feeding) and output (urine, drain, nasogastric tube, and stool volumes) data starting from AKI diagnosis to ICU discharge were used to assess fluid overload. The degree of cumulative fluid overload in relation to body weight was expressed as percent fluid overload (%FO), which was calculated using the following formula: ∑ daily (fluid intake in L − total output in L)/baseline body weight in kg) × 10012. Baseline body weight was measured upon ICU admission. Based on our previous study13, %FO was further subdivided into %FO from AKI diagnosis to CRRT initiation (%FOpreCRRT) and %FO from CRRT initiation to ICU discharge (%FOpostCRRT). Finally, total fluid overload (%FOtotal) from AKI diagnosis to ICU discharge was defined as %FOpreCRRT + %FOpostCRRT.
Statistical analysis
Continuous variables are expressed as medians with interquartile ranges and were compared using the Mann–Whitney or Kruskal–Wallis test. Categorical variables are expressed as numbers with percentages and were compared using the chi-square test. Receiver operating characteristic (ROC) curve analysis was employed to assess the area under the curve (AUC), and the Youden index was used to determine the best cutoff value of %FOpreCRRT and %FOtotal for predicting the 28-day mortality. Kaplan–Meier analysis was performed within 28 days of ICU admission and compared the survival curve between the groups, which was stratified by the best cutoff value of %FOpreCRRT and %FOtotal, using the log-rank test. To determine the independent risk factors for the 28-day mortality after ICU admission, univariable and multivariable Cox proportional hazards were used, and results are presented as hazard ratios (HR) and 95% confidence intervals (CIs). Significant variables were identified through univariable analysis (P < 0.1), and clinically important variables were considered in the multivariable analysis. Of the significant variables in the univariable analysis, variables (mean arterial pressure, platelet count, pH, and serum creatinine) included in SOFA or APACHE II scores were excluded from multivariable analysis to avoid redundant analysis. Instead, the SOFA and APACHE II scores were considered in the final multivariable analysis on behalf of those variables. Statistical significance was set at p < 0.05. All analyses were performed using SPSS version 26.0 (SPSS, Inc., Chicago, IL, USA) and MedCalc Statistical Software version 19.4.1 (MedCalc Software, Ostend, Belgium).
Results
Baseline characteristics at ICU admission
A total of 543 patients with sepsis and AKI underwent CRRT. The baseline characteristics of the study population at ICU admission stratified by the 28-day mortality are presented in Table 1. The median age of the study population was 70 years, and 325 patients were men. The most common infection source in the study population was the respiratory tract, followed by the gastrointestinal tract, urinary tract, soft tissue, and unknown. Of the 543 patients, 275 died within 28 days after ICU admission. Regarding demographics, there were no significant differences in age, sex, or body weight between survivors and non-survivors. In terms of comorbid diseases, non-survivors had a higher prevalence of COPD, liver cirrhosis, and congestive heart failure than survivors. There were no significant differences in infection sources between survivors and non-survivors. Regarding the severity of illness, non-survivors had higher SOFA and APACHE II scores and prevalence of vasopressor use and ventilator dependency than survivors. Concerning findings on ICU admission, non-survivors had lower mean arterial pressure, platelet count, and pH than survivors. Non-survivors were also likely to have a higher prevalence of oliguria, along with elevated prothrombin time, procalcitonin, and lactate levels. The interval between AKI diagnosis and CRRT initiation in non-survivors was significantly higher than that in survivors. The CRRT duration in non-survivors was significantly longer than that in survivors. There were no significant differences in the prescribed CRRT doses between the two groups. In terms of fluid overload status, non-survivors had a higher %FOpreCRRT, %FOpostCRRT, and %FOtotal than survivors.
Performance of fluid overload status for predicting the 28-day mortality
To investigate the diagnostic power of %FOpreCRRT and %FOtotal for predicting the 28-day mortality, ROC analysis was performed (Fig. 1). The AUCs were 0.826 (95% CI: 0.791–0.857, P < 0.001) for %FOpreCRRT and 0.834 (95% CI: 0.800–0.864, P < 0.001) for %FOtotal. The best cutoff value of %FOpreCRRT was > 4.6%, with an associated sensitivity of 82.5% and specificity of 73.0%. The best cutoff of %FOtotal was > 9.6%, with an associated sensitivity of 71.6% and specificity of 70.8%. Next, we divided the study subjects into those with %FOpreCRRT > 4.6% and those with %FOpreCRRT ≤ 4.6%, or those with %FOtotal > 9.6% and those with %FOtotal ≤ 9.6% according to the best cutoff value of %FOpreCRRT and %FOtotal for the 28-day mortality. Patients with %FOpreCRRT > 4.6% showed a significant decrease in survival after ICU admission compared with those with %FOpreCRRT ≤ 4.6% (28-day mortality: 37.5% vs. 62.4%, P < 0.001). There was also a significant difference in survival between patients with %FOtotal > 9.6% and those with %FOtotal ≤ 9.6% (28-day mortality: 31.3% vs. 75.6%, P < 0.001) (Fig. 2).
Receiver-operating characteristic curves of %FOpreCRRT (a) and %FOtotal (b) for predicting the 28-day mortality in the study population (n = 543). The AUCs were 0.826 (95% CI: 0.791–0.857, P < 0.001) for %FOpreCRRT and 0.834 (95% CI: 0.800–0.864, P < 0.001) for %FOtotal. The best cutoff value of %FOpreCRRT was > 4.6%, with an associated sensitivity of 82.5% and specificity of 73.0%. The best cutoff of %FOtotal was > 9.6%, with an associated sensitivity of 71.6% and specificity of 70.8%. %FOpreCRRT was defined as the percentage of fluid overload relative to baseline body weight from AKI diagnosis to ICU initiation. %FOpostCRRT was defined as the percentage of fluid overload relative to baseline body weight from CRRT initiation to ICU discharge. %FOtotal was defined as the sum of %FOpreCRRT and %FOpostCRRT. AKI, acute kidney injury; AUC, area under the curve; CI, confidence interval; CRRT, continuous renal replacement therapy; ICU, intensive care unit.
Kaplan–Meier survival estimate according to the best cutoff value of %FOpreCRRT (a) and %FOtotal (b) for 28-day mortality. There was a significant difference in survival among patients with %FOpreCRRT ≤ 4.6% or > 4.6% (28-day mortality, 37.5% vs. 62.4%, P < 0.001). There was also a significant difference in survival among patients with %FOtotal ≤ 9.6% or > 9.6% (28-day mortality, 31.3% vs. 75.6%, P < 0.001). %FOpreCRRT was defined as the percentage of fluid overload relative to baseline body weight from AKI diagnosis to ICU initiation. %FOpostCRRT was defined as the percentage of fluid overload relative to baseline body weight from CRRT initiation to ICU discharge. %FOtotal was defined as the sum of %FOpreCRRT and %FOpostCRRT. CRRT, continuous renal replacement therapy, ICU; intensive care unit.
Association between %FOpreCRRT or %FOtotal and the 28-day mortality
Table 2 shows the variables found to be associated with the 28-day mortality in the univariable Cox regression analysis. %FOpreCRRT > 4.6% (vs. ≤ 4.6%, HR: 1.90, 95% CI: 1.49–2.43, P < 0.001) and %FOtotal > 9.6% (vs. ≤ 9.6%, HR: 3.37; 95% CI: 2.63–4.33, P < 0.001) were significant predictors for the 28-day mortality. Furthermore, age, COPD, liver cirrhosis, congestive heart failure, SOFA score, APACHE II score, vasopressor use, ventilator use, mean arterial pressure, oliguria, platelet count, PT (INR), procalcitonin, pH, lactate, and time from AKI diagnosis to CRRT initiation were significant predictors of the 28-day mortality. Table 3 shows the results of the multivariable Cox proportional hazards analysis for the 28-day mortality after ICU admission in the study population. %FOpreCRRT > 4.6% (vs. ≤ 4.6%, HR: 1.42; 95% CI: 1.10–1.83, P < 0.001) and %FOtotal > 9.6% (vs. ≤ 9.6%, HR: 1.95, 95% CI: 1.49–2.56, P < 0.001) were significant predictors for the 28-day mortality. In addition, SOFA score (per 1 point increment, HR: 1.11, 95% CI: 1.07–1.14, P < 0.001), APACHE II score (per 1 point increment; HR: 1.05, 95% CI: 1.03–1.07, P < 0.001), oliguria before CRRT (HR: 1.48, 95% CI: 1.10–1.98, P = 0.009), lactate (per 1.0 mmol/L increment, HR: 1.05, 95% CI: 1.02–1.08, P = 0.003), and time from AKI diagnosis to CRRT initiation (per 1 day increment, HR: 1.11, 95% CI: 1.10–1.83, P = 0.047) were significantly associated with the 28-day mortality.
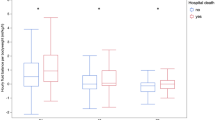
Next, we analyzed the association between fluid overload and the 28-day mortality in subgroups stratified by age, sex, diabetes, oliguria, SOFA score, and time from AKI diagnosis to CRRT initiation. First, we performed ROC analysis to determine the best cutoff value of the SOFA score and time from AKI diagnosis to CRRT initiation for predicting the 28-day mortality. Best cutoff values of the SOFA score and time from AKI diagnosis to CRRT initiation were > 14 points (AUC, 0.842; P < 0.001) and > 1.5 days (AUC, 0.808; P < 0.001), respectively (Supplementary Fig. S2). Based on the best cutoff value, we divided the study subjects into a high SOFA group (> 14 points) or low SOFA group (≤ 14 points) and late CRRT group (> 1.5 days) or early CRRT group (≤ 1.5 days). In multivariable Cox regression analysis (Fig. 3), %FOpreCRRT > 4.6% (vs. ≤ 4.6) and %FOtotal > 9.6% (vs. ≤ 9.6%) were significant predictors of the 28-day mortality irrespective of high or low SOFA scores and early or late CRRT. Independent associations between fluid overload and the 28-day mortality were consistently observed in other subgroups, including age > 65 or ≤ 65 years, male or female sex, diabetes or no diabetes, and oliguria or no oliguria.
HR plots of %FOpreCRRT (a) and %FOtotal (b) for 28-day mortality according to subgroup. %FOpreCRRT > 4.6% (vs. ≤ 4.6%) and %FOtotal > 9.6% (vs. ≤ 9.6%) was associated with an increased HR for 28-day mortality in all subgroups. The HR was analyzed with a fully adjusted Cox regression model including age, sex, COPD, liver cirrhosis, CHF. SOFA score, APACHE II score, PT (INR), procalcitonin, lactate, and time from AKI diagnosis to CRRT initiation. %FOpreCRRT was defined as a percentage of fluid overload from baseline body weight from AKI diagnosis to ICU initiation. %FOpostCRRT was defined as a percentage of fluid overload from baseline body weight from CRRT initiation to ICU discharge. %FOtotal was defined as the sum of %FOpreCRRT and %FOpostCRRT. Oliguria was defined as < 0.5 mL/kg per hour of urine output for 6 h before CRRT initiation. AKI, acute kidney injury; APACHE II, Acute Physiology and Chronic Health Evaluation II; COPD, chronic obstructive pulmonary disease; CRP, C-reactive protein; CRRT, continuous renal replacement therapy; HR, hazard ratio; ICU, intensive care unit; PT (INR), prothrombin time (international normalized ratio); SOFA, sequential organ failure assessment.
Effect of minimizing fluid overload using CRRT on the 28-day mortality
All patients were also classified into four groups to assess the effect of minimizing the fluid overload using CRRT on mortality: Group 1 (n = 182, %FOpreCRRT ≤ 4.6% and %FOtotal ≤ 9.6%; no significant fluid overload before and after CRRT application, and finally, no significant total fluid overload); Group 2 (n = 140, %FOpreCRRT > 4.6% and %FOtotal ≤ 9.6%; significant fluid overload before CRRT that was then resolved by CRRT, and finally, no significant total fluid overload); Group 3 (n = 103, %FOpreCRRT ≤ 4.6% and %FOtotal > 9.6%; no significant fluid overload before CRRT, but significant total fluid overload due to aggravation of fluid overload during CRRT); and Group 4 (n = 118, %FOpreCRRT > 4.6% and %FOtotal > 9.6%; significant fluid overload before CRRT, which was not resolved by CRRT, and finally, significant total fluid overload).
Table 4 shows the baseline characteristics of the four subgroups. There were significant differences among the four groups with respect to age, SOFA score, APACHE II score, vasopressor use, ventilator dependency, mean arterial pressure, oliguria, platelet count, procalcitonin, pH, lactate, time from AKI diagnosis to CRRT initiation, and CRRT duration. There was a significant difference in survival between the four groups; the 28-day mortality was the highest in Group 4, followed by Group 3, Group 2, and Group 1 (84.7% vs. 65.0% vs. 43.6% vs. 22.0%, respectively; P < 0.001) (Fig. 4).
Kaplan–Meier survival estimate among the four groups categorized by the best cutoff value of %FOpreCRRT and %FOtotal for 28-day mortality. There was a significant difference in survival between the four groups. Twenty-eight-day mortality was the highest in Group 4, followed by Group 3, Group 2, and Group 1 (84.7% vs. 65.0% vs. 43.6% vs. 22.0%, P < 0.001). Group 1 (n = 182): %FOpreCRRT ≤ 4.6% and %FOtotal ≤ 9.6%; Group 2 (n = 140): %FOpreCRRT > 4.6% and %FOtotal ≤ 9.6%; Group 3 (n = 103): %FOpreCRRT ≤ 4.6% and %FOtotal > 9.6%; Group 4 (n = 118): %FOpreCRRT > 4.6% and %FOtotal > 9.6% %FOpreCRRT was defined as the percentage fluid overload relative to baseline body weight from AKI diagnosis to ICU initiation. %FOpostCRRT was defined as the percentage fluid overload relative to baseline body weight from CRRT initiation to ICU discharge. %FOtotal was defined as the sum of %FOpreCRRT and %FOpostCRRT. CRRT, continuous renal replacement therapy, ICU; intensive care unit.
We further analyzed the 28-day mortality according to the four groups using the multivariable Cox proportional hazards analysis (Table 5). In the univariable analysis (model 1), Group 4 (HR: 6.06, 95% CI: 4.19–8.78, P < 0.001), Group 3 (HR: 4.01, 95% CI: 2.71–5.95, P < 0.001), and Group 2 (HR: 2.18, 95% CI: 1.46–3.25, P < 0.001) had a significantly higher risk of the 28-day mortality than Group 1. These associations were significant after adjustment for sex, age, SOFA score, APACHE II score, oliguria, and time from AKI diagnosis to CRRT initiation (model 2) (Group 4 [HR: 3.00, 95% CI: 2.03–4.45, P < 0.001], Group 3 [HR: 2.12, 95% CI: 1.40–3.20, P < 0.001], and Group 2 [HR: 1.59, 95% CI: 1.06–2.39, P = 0.025] compared with Group 1). These associations also remained significant after further adjustment for liver cirrhosis, COPD, congestive heart failure, prothrombin time, procalcitonin, and lactate (model 3) (Group 4 [HR: 2.90, 95% CI: 1.95–4.32, P < 0.001], Group 3 [HR: 2.11, 95% CI: 1.39–3.21, P < 0.001], and Group 2 [HR: 1.52, 95% CI: 1.01–2.30, P = 0.046] compared with Group 1).
Discussion
Sepsis, especially severe sepsis and septic shock, is a condition of hypoperfusion in the setting of infection and is associated with high mortality and morbidity, including end-organ dysfunction and failure20. In the management of sepsis, EGDT has been adopted either completely or at least in components in many ICUs worldwide since it showed a survival benefit in patients with severe sepsis and septic shock16, and the guidelines recommend the EGDT protocol21. EGDT requires initial aggressive fluid resuscitation to avoid hypovolemia and its associated complications, including hypotension, kidney injury, and multiorgan failure20. However, beyond the threshold needed for acute resuscitation, excessive fluid accumulation leads to harmful consequences, such as hypertension, pulmonary edema, respiratory failure, and increased cardiac demand20. Indeed, previous studies comparing EGDT and usual care with conservative fluid administration in patients with septic shock demonstrated that EGDT did not reduce all-cause mortality when compared with usual care22,23,24. Furthermore, some studies reported that fluid overload was associated with increased mortality in patients with severe sepsis and septic shock and recommended a more cautious approach to fluid resuscitation25,26,27. However, several studies reported no difference in mortality among the patients who received restricted fluid therapy and those who received liberal fluid therapy28,29,30,31. A meta-analysis including the 637 patients with sepsis found no statistically significant difference between lower vs. higher fluid volume in all-cause mortality30. Furthermore, a recent randomized controlled study including 1,554 patients showed that restricted fluid therapy did not result in fewer deaths at 90 days than standard fluid therapy among patients with septic shock in ICU31. Thus, optimal management of fluid balance in patients with severe sepsis or septic shock still needs to be investigated.
SIAKI is the first cause of AKI in the ICU, and 15–20% of patients with SIAKI require RRT32. Though SIAKI is a multifactorial syndrome with inflammatory, nephrotoxic, and ischemic insults33, acute tubular necrosis due to decreased kidney perfusion is known as the main pathophysiological factor of SIAKI. Thus, in line with management for patients with severe sepsis and septic shock, fluid therapy has been an essential component of care for patients with SIAKI to prevent further ischemic kidney damage. However, recent studies suggest that, in addition to decreased renal perfusion, renal inflammation and microvascular dysfunction play pivotal roles in SIAKI33,34. Inflammatory mediators derived from bacterial or immune cells are filtered in the glomerulus, enter the tubular space, and can subsequently injure the tubular cells by binding to their respective receptors34. Furthermore, cytokines, damage-associated molecular patterns (DAMPs), and pathogen-associated molecular patterns (PAMPs) are released from extravasated leukocytes and can activate tubular cells from the interstitial side. The activation of cytokines or DAMPs/PAMPs receptors induces apoptosis or cell cycle arrest34.
Despite advances in medical interventions, including CRRT, SIAKI has been reported to be associated with a high mortality rate of 50–60%3,32. Until now, most studies on the effect of CRRT on mortality in patients with SIAKI have focused on the timing and dose of CRRT32 and little research has been conducted on the association between survival and fluid overload in patients with SIAKI receiving CRRT. In this study, we investigated the association between fluid overload and survival in patients receiving CRRT considering the important role of fluid balance in patients with SIAKI.
Most previous studies on fluid overload in patients with AKI receiving or not receiving RRT have included a heterogeneous population of patients with AKI, including both SIAKI and non-SIAKI9,10,11,12,13,14,15, whereas only patients with SIAKI were included in the present study. To the best of our knowledge, the present study is the first to investigate the association between fluid overload and survival in patients with SIAKI receiving CRRT. Previous studies confirming the adverse effects of fluid overload on survival in patients with AKI used various definitions of the degree of fluid overload, including a percentage of fluid accumulation > 10% over the baseline weight12,13,15. However, fluid overload > 10% over the baseline weight was arbitrarily defined without any basis for its definition, and the best cutoff value of the degree of fluid overload for predicting mortality was unknown. In this study, we divided fluid overload into fluid overload from AKI diagnosis to CRRT initiation (%FOpreCRRT) and total fluid overload from AKI diagnosis to ICU discharge (%FOtotal, %FOpreCRRT + %FOpostCRRT) and found that %FOpreCRRT > 4.6% (AUC, 0.826; P < 0.001) and %FOtotal > 9.6% (AUC, 0.834; P < 0.001) were the best cutoff values of the degree of fluid overload for predicting the 28-day mortality. We believe that these cutoff values could help guide fluid management in critically ill patients with SIAKI receiving CRRT and conduct further research on the association between fluid overload and survival in these patients.
In the present study, we demonstrated that both %FOpreCRRT and %FOtotal were independent risk factors for the 28-day mortality in patients with SIAKI receiving CRRT, and the results of our study are in line with those of previous studies. However, most previous studies have only assessed fluid accumulation either before RRT10,14,15 or during the period of ICU or hospital stay11,12. In contrast, the present study assessed both %FOpreCRRT, in which initial fluid resuscitation was implemented in patients with SIAKI, and %FOtotal, in which the effect of CRRT on fluid overload was reflected. Thus, our study clarified the association between fluid overload and survival in these patients. Finally, the multivariable analysis of our study demonstrated that patients with %FOpreCRRT > 4.6% and %FOtotal > 9.6% were 1.9- and 3.37-times more likely to die within 28 days after ICU admission than those with %FOpreCRRT ≤ 4.6% and %FOtotal ≤ 9.6%. Furthermore, this association between survival and fluid overload was consistent across various subgroups, including the high SOFA group (> 14 points) or low SOFA group (≤ 14 points), late CRRT group (> 1.5 days) or early CRRT group (≤ 1.5 days), age > 65 or ≤ 65 years, male or female sex, diabetes or no diabetes, and oliguria or no oliguria, suggesting a robust effect of fluid overload on survival in patients with SIAKI receiving CRRT.
One of the major findings is that minimizing fluid overload by CRRT reduced mortality in critically ill patients with SIAKI. In previous studies, the randomized evaluation of normal versus augmented level (RENAL) of replacement therapy study investigators showed that negative fluid balance during CRRT was associated with decreased mortality in patients with AKI (n = 1453)7. Murugan et al. showed that achieving a high intensity of net ultrafiltration (> 25 mL/kg/day) through CRRT or intermittent RRT was associated with lower 1-year risk-adjusted mortality in patients with AKI (n = 1075), confirming the importance of RRT in fluid management in these patients8. Recently, Hall et al. demonstrated that a decline in fluid accumulation through CRRT was associated with a lower risk of mortality in critically ill patients with AKI (n = 820)17. In the present study, the 28-day mortality was the highest in Group 4 (84.7%, %FOpreCRRT > 4.6% and %FOtotal > 9.6%), followed by Group 3 (65.0%, %FOpreCRRT ≤ 4.6% and %FOtotal > 9.6%), Group 2 (43.6%, %FOpreCRRT > 4.6% and %FOtotal ≤ 9.6%), and Group 1 (22%, %FOpreCRRT ≤ 4.6% and %FOtotal ≤ 9.6%). The multivariable analysis also showed that people in Group 4, Group 3, and Group 2 were nearly six times, four times, and two times more likely to die than those in Group 1. These findings showed that minimizing the fluid overload using CRRT is associated with reduced mortality in critically ill patients with SIAKI. One can argue that tolerating fluid removal using CRRT is a sign of less severe illness, such as hemodynamic stability. Thus, our results need to be interpreted cautiously regarding whether the beneficial effect of fluid removal using CRRT on mortality is owing to its direct therapeutic effect or the fact that patients with less severe illness could tolerate fluid removal. However, our multivariable analysis showed that the association between survival and fluid overload remained significant after adjustment for disease severity indices such as SOFA score, APACHE II score, vasopressor use, ventilator dependency, and oliguria, suggesting that disease severity alone may not account for our findings. Finally, in clinical practice, clinicians are inevitably confronted with fluid overload during the management of patients with SIAKI, and the results of our study suggest that efforts are needed to maintain %FOpreCRRT ≤ 4.6% and %FOtotal ≤ 9.6% as much as possible to improve the survival of patients with SIAKI receiving CRRT.
One of the strengths of our study is the inclusion of time from AKI diagnosis to CRRT initiation in the multivariable analysis. We found that a 1-day increase in the time between AKI diagnosis and CRRT initiation was associated with an 11% increased risk of the 28-day mortality in our study population. Whether early initiation of CRRT improves mortality in critically ill patients with SIAKI remains controversial, and previous studies have reported inconsistent results. Several retrospective studies have shown that early initiation of CRRT has survival benefits in critically ill patients with SIAKI35,36,37,38. However, two randomized clinical trials reported that early application of CRRT is deleterious39 or there was no difference in mortality between early and late RRT initiation in these patients40. This discrepancy between the results of previous studies might be owing to an unstandardized definition for early and late initiation of CRRT. Furthermore, the optimal timing to initiate CRRT remains undefined in patients with SIAKI. In the present study, we found that the best cutoff value for the time from AKI diagnosis to CRRT initiation for predicting the 28-day mortality was > 1.5 day, with a sensitivity of 71.3% and specificity of 75.6% (AUC, 0.808; P < 0.001). The Kaplan–Meier curve also showed a significant difference in the 28-day mortality between the late CRRT group (> 1.5 days) and early CRRT group (≤ 1.5 days) (Supplementary Fig. S3). Despite the retrospective design of our study, this observation suggests that CRRT initiation within 1.5 days from AKI diagnosis, if possible, should be encouraged to improve the survival of critically ill patients with SIAKI.
Despite its strengths, our study had some limitations. First, owing to its retrospective design, it is not possible to discern whether fluid overload is solely a marker of more severe illness or a causal contributor to mortality in our study subjects. However, as discussed above in the present study, we attempted to adjust for the disease severity indices, such as the SOFA score, APACHE II score, vasopressor use, and ventilator dependency, and found that fluid overload during CRRT was independently associated with the 28-day mortality, suggesting that fluid overload is a potentially modifiable risk factor for mortality in patients with SIAKI receiving CRRT. Second, we included a specific subset of critically ill patients, namely those with SIAKI who received CRRT. Thus, selection bias could not be avoided, and the results of our study might not be generalizable to other populations of critically ill patients with AKI. Third, fluid management using CRRT was implemented through discussion and consultation with the attending nephrologist without a standardized protocol. Thus, variations in fluid management might have affected the effect of fluid overload on survival in the present study.
In conclusion, our study demonstrated that %FOpreCRRT > 4.6% and %FOtotal > 9.6% were the best cutoff values of the degree of fluid overload for predicting the 28-day mortality in critically ill patients with SIAKI receiving CRRT. Both %FOpreCRRT and %FOtotal were independent risk factors for the 28-day mortality. Future randomized controlled studies are needed to confirm whether fluid overload is solely a marker of more severe illness or a causal contributor to mortality and whether minimizing fluid overload using CRRT improves survival in critically ill patients with SIAKI.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Mandelbaum, T. et al. Outcome of critically ill patients with acute kidney injury using the Acute Kidney Injury Network criteria. Crit. Care Med. 39(12), 2659–2664 (2011).
Mehta, R. L. et al. Spectrum of acute renal failure in the intensive care unit: the PICARD experience. Kidney Int. 66(4), 1613–1621 (2004).
Uchino, S. et al. Acute renal failure in critically ill patients: A multinational, multicenter study. JAMA 294(7), 813–818 (2005).
Tolwani, A. Continuous renal-replacement therapy for acute kidney injury. N. Engl. J. Med. 367(26), 2505–2514 (2012).
Hoste, E. A. et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 41(8), 1411–1423 (2015).
Marx, G. Fluid therapy in sepsis with capillary leakage. Eur. J. Anaesthesiol. 20(6), 429–442 (2003).
Investigators, R. R. T. S. et al. An observational study fluid balance and patient outcomes in the randomized evaluation of normal vs. augmented level of replacement therapy trial. Crit. Care Med. 40(6), 1753–1760 (2012).
Murugan, R. et al. Net ultrafiltration intensity and mortality in critically ill patients with fluid overload. Crit. Care 22(1), 223 (2018).
Goldstein, S. L. et al. Outcome in children receiving continuous venovenous hemofiltration. Pediatrics 107(6), 1309–1312 (2001).
Sutherland, S. M. et al. Fluid overload and mortality in children receiving continuous renal replacement therapy: The prospective pediatric continuous renal replacement therapy registry. Am. J. Kidney Dis. 55(2), 316–325 (2010).
Payen, D. et al. A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit. Care 12(3), R74 (2008).
Bouchard, J. et al. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 76(4), 422–427 (2009).
Kim, I. Y. et al. Fluid overload and survival in critically ill patients with acute kidney injury receiving continuous renal replacement therapy. PLoS ONE 12(2), e0172137 (2017).
Jhee, J. H. et al. Cumulative fluid balance and mortality in elderly patients with acute kidney injury requiring continuous renal-replacement therapy: A multicenter prospective cohort study. Kidney Res Clin Pract 39(4), 414–425 (2020).
Woodward, C. W. et al. Fluid overload associates with major adverse kidney events in critically ill patients with acute kidney injury requiring continuous renal replacement therapy. Crit. Care Med. 47(9), e753–e760 (2019).
Rivers, E. et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N. Engl. J. Med. 345(19), 1368–1377 (2001).
Hall, A. et al. Fluid removal associates with better outcomes in critically ill patients receiving continuous renal replacement therapy: a cohort study. Crit. Care 24(1), 279 (2020).
Bone, R. C. et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101(6), 1644–1655 (1992).
Kellum, J. A., Lameire, N., KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: A KDIGO summary (Part 1). Critical care 17, 1–15 (2013).
Kelm, D. J. et al. Fluid overload in patients with severe sepsis and septic shock treated with early goal-directed therapy is associated with increased acute need for fluid-related medical interventions and hospital death. Shock 43(1), 68–73 (2015).
Dellinger, R. P. et al. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 39(2), 165–228 (2013).
Peake, S. L. et al. Goal-directed resuscitation for patients with early septic shock. N. Engl. J. Med. 371(16), 1496–1506 (2014).
Yealy, D. M. et al. A randomized trial of protocol-based care for early septic shock. N. Engl. J. Med. 370(18), 1683–1693 (2014).
Mouncey, P. R. et al. Trial of early, goal-directed resuscitation for septic shock. N. Engl. J. Med. 372(14), 1301–1311 (2015).
Boyd, J. H., Forbes, J., Nakada, T. A., Walley, K. R. & Russell, J. A. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med 39(2), 259–265 (2011).
Genga, K. & Russell, J. A. Early liberal fluids for sepsis patients are harmful. Crit. Care Med. 44(12), 2258–2262 (2016).
Marik, P. E., Linde-Zwirble, W. T., Bittner, E. A., Sahatjian, J. & Hansell, D. Fluid administration in severe sepsis and septic shock, patterns and outcomes: An analysis of a large national database. Intensive Care Med. 43(5), 625–632 (2017).
Smith, S. H. & Perner, A. Higher vs. lower fluid volume for septic shock: Clinical characteristics and outcome in unselected patients in a prospective, multicenter cohort. Crit. Care 16(3), R76 (2012).
Cronhjort, M. et al. Association between fluid balance and mortality in patients with septic shock: A post hoc analysis of the TRISS trial. Acta Anaesthesiol. Scand. 60(7), 925–933 (2016).
Meyhoff, T. S. et al. Lower vs. higher fluid volumes during initial management of sepsis: A systematic review with meta-analysis and trial sequential analysis. Chest 157(6), 1478–1496 (2020).
Meyhoff, T. S. et al. Restriction of intravenous fluid in ICU patients with septic shock. N. Engl. J. Med. 386(26), 2459–2470 (2022).
Romagnoli, S., Ricci, Z. & Ronco, C. CRRT for sepsis-induced acute kidney injury. Curr. Opin. Crit. Care 24(6), 483–492 (2018).
Gomez, H. et al. A unified theory of sepsis-induced acute kidney injury: Inflammation, microcirculatory dysfunction, bioenergetics, and the tubular cell adaptation to injury. Shock 41(1), 3–11 (2014).
Zarbock, A., Gomez, H. & Kellum, J. A. Sepsis-induced acute kidney injury revisited: Pathophysiology, prevention and future therapies. Curr. Opin. Crit. Care 20(6), 588–595 (2014).
Oh, H. J. et al. Early initiation of continuous renal replacement therapy improves patient survival in severe progressive septic acute kidney injury. J. Crit. Care 27(6), 743–749 (2012).
Chon, G. R. et al. A comparison of the time from sepsis to inception of continuous renal replacement therapy versus RIFLE criteria in patients with septic acute kidney injury. Shock 38(1), 30–36 (2012).
Oh, H. J. et al. Can early initiation of continuous renal replacement therapy improve patient survival with septic acute kidney injury when enrolled in early goal-directed therapy?. J. Crit. Care 35, 51–56 (2016).
Yoon, B. R., Leem, A. Y., Park, M. S., Kim, Y. S. & Chung, K. S. Optimal timing of initiating continuous renal replacement therapy in septic shock patients with acute kidney injury. Sci. Rep. 9(1), 11981 (2019).
Payen, D. et al. Impact of continuous venovenous hemofiltration on organ failure during the early phase of severe sepsis: A randomized controlled trial. Crit. Care Med. 37(3), 803–810 (2009).
Barbar, S. D. et al. Timing of renal-replacement therapy in patients with acute kidney injury and sepsis. N. Engl. J. Med. 379(15), 1431–1442 (2018).
Author information
Authors and Affiliations
Contributions
I.Y.K. and S.B.L. designed the study. I.Y.K., S.K., B.M.Y., M.J.K., S.R.K., H.J.K., and H.R. analyzed and interpreted data. I.Y.K. and S.B.L. wrote the manuscript. S.H.S., E.Y.S., D.W.L., and S.B.L. supervised the study. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, I.Y., Kim, S., Ye, B.M. et al. Effect of fluid overload on survival in patients with sepsis-induced acute kidney injury receiving continuous renal replacement therapy. Sci Rep 13, 2796 (2023). https://doi.org/10.1038/s41598-023-29926-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-29926-w
This article is cited by
-
Prognostic value of Doppler waveform analysis of common femoral vein in septic patients: a prospective cohort study
Journal of Ultrasound (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.