Abstract
Item 10 of the Edinburgh Postnatal Depression Scale (EPDS) is intended to assess thoughts of intentional self-harm but may also elicit concerns about accidental self-harm. It does not specifically address suicide ideation but, nonetheless, is sometimes used as an indicator of suicidality. The 9-item version of the EPDS (EPDS-9), which omits item 10, is sometimes used in research due to concern about positive endorsements of item 10 and necessary follow-up. We assessed the equivalence of total score correlations and screening accuracy to detect major depression using the EPDS-9 versus full EPDS among pregnant and postpartum women. We searched Medline, Medline In-Process and Other Non-Indexed Citations, PsycINFO, and Web of Science from database inception to October 3, 2018 for studies that administered the EPDS and conducted diagnostic classification for major depression based on a validated semi-structured or fully structured interview among women aged 18 or older during pregnancy or within 12 months of giving birth. We conducted an individual participant data meta-analysis. We calculated Pearson correlations with 95% prediction interval (PI) between EPDS-9 and full EPDS total scores using a random effects model. Bivariate random-effects models were fitted to assess screening accuracy. Equivalence tests were done by comparing the confidence intervals (CIs) around the pooled sensitivity and specificity differences to the equivalence margin of δ = 0.05. Individual participant data were obtained from 41 eligible studies (10,906 participants, 1407 major depression cases). The correlation between EPDS-9 and full EPDS scores was 0.998 (95% PI 0.991, 0.999). For sensitivity, the EPDS-9 and full EPDS were equivalent for cut-offs 7–12 (difference range − 0.02, 0.01) and the equivalence was indeterminate for cut-offs 13–15 (all differences − 0.04). For specificity, the EPDS-9 and full EPDS were equivalent for all cut-offs (difference range 0.00, 0.01). The EPDS-9 performs similarly to the full EPDS and can be used when there are concerns about the implications of administering EPDS item 10.
Trial registration: The original IPDMA was registered in PROSPERO (CRD42015024785).
Similar content being viewed by others
Introduction
Depression is a common and disabling mental disorder among women during pregnancy and in the postpartum period1,2. A 2005 systematic review estimated that the point prevalence of major depression during pregnancy and postpartum ranged from 1 to 6% at different time points (first trimester of pregnancy to one year postpartum), based on 2–6 studies at any given time point (N = 111–2104 participants)3. A 2008 national survey from the USA with more than 14,000 participants reported 12-month period prevalence was similar among pregnant women (8%), postpartum women (9%), and similar-aged non-pregnant women (8%)4. Nonetheless, perinatal depression may have substantial adverse effects on mothers, fathers, partner relationships, and infants, including impairment of maternal function, paternal depression, premature delivery, infants with low birth weight and developmental delays, and impaired parent-infant interactions5,6,7,8.
Depression screening involves using self-report questionnaires to identify individuals who exceed a pre-defined cut-off score for further diagnostic evaluation to determine whether they have depression9,10. Guidelines from the United States Preventive Services Task Force and the Australian government recommend depression screening in pregnant and postpartum women11,12. The United Kingdom National Screening Committee and Canadian Task Force on Preventive Health Care, on the other hand, recommend against screening due to concerns about false positives, possible associated harms, and a lack of evidence from randomized controlled trials that screening leads to improved health outcomes13,14.
The 10‐item Edinburgh Postnatal Depression Scale (EPDS) is the most commonly used self‐report questionnaire for depression screening in pregnancy and postpartum15,16. It is also used to monitor symptoms among people undergoing treatment for depression and as a continuous outcome measure in research. Respondents rate how they have felt in the previous seven days17. Each item is scored 0–3, and possible total scores range from 0 to 30; higher scores indicate more severe depressive symptoms. Cut‐off values of ≥ 10 and ≥ 13 are often recommended for screening15,18,19. A 2020 individual participant data meta-analysis (IPDMA) reported that a cut-off of 11 or higher maximized the sum of sensitivity (81%) and specificity (88%), when using a semi-structured diagnostic interview as the reference standard (N = 36 studies, 9066 participants, 1330 major depression cases)20.
Although brief tools have been designed specifically to assess suicide ideation and risk in health care settings21, item 10 of the EPDS is sometimes used as a proxy of suicidal ideation. Item 10 of the EPDS is intended to assess thoughts of self-harm: “the thought of harming myself has occurred to me”15,22. A review from 2005 reported that 5–15% of pregnant and postpartum women had thoughts of self-harm (item score ≥ 1) based on this item23. However, responses to this item may not accurately reflect whether suicide ideation is present. One study compared positive responses on item 10 to item 3 of the Hamilton Depression Rating Scale (HDRS), which directly asks about suicidal ideation, among a sample of women with mood disorders during the first year postpartum; 17% (22/131) of participants who were administered the EPDS had positive responses versus 6% (9/146) on HDRS item 324. A study of 574 pregnant and postpartum women with positive responses to item-10 found that 324 (57%) women had fleeting thoughts of avoiding problems but no intent to self-harm, and 75 (13%) misunderstood the item25. One potential reason for this is that the item is not specific; and some women may misinterpret it to include unintentional injury, such as due to falls from impaired balance26,27,28, for instance. When the full EPDS is used in research studies, misinterpretation of item 10 could require follow-up with many women who endorse the item, even though most responses are false positives. This consumes substantial resources without evidence of benefit to study participants from administering the item.
A 9-item version of the EPDS (EPDS-9), which omits item 10, is sometimes used. A study of 371 women from the United States referred to a program serving women with or at risk of postpartum depression found that 49% of participants scored ≥ 13 on the full EPDS compared to 48% based on the EPDS-929. If differences in performance between the EPDS-9 and full EPDS are minimal, the EPDS-9 could be used for a range of purposes in research studies, where administering item 10 could have significant resource implications, including the need to follow-up on potentially large numbers of false positive responses to item 10. It might also be considered in trials of screening programs or in jurisdictions where screening is done in practice. However, no study has compared correlations between continuous scores and level of agreement in screening accuracy between the EPDS-9 and full EPDS. The objectives of the present study were to (1) evaluate the association of continuous EPDS-9 and full EPDS scores for assessing depressive symptom severity; and (2) assess the equivalence of the accuracy of the EPDS-9 and full EPDS across relevant cut-offs for screening to detect major depression.
Methods
The present study used a subset of participants from a database originally synthesized for an IPDMA on the accuracy of the full EPDS for depression screening20. The original IPDMA was registered in PROSPERO (CRD42015024785), and a protocol was published30. Results from the main IPDMA of the EPDS have been published20. To assess the equivalence of the EPDS-9 and full EPDS, we followed similar methods to those used in our previously published study that assessed the equivalence of the Patient Health Questionnaire-8 (PHQ-8) and PHQ-931. Prior to initiating the present study, we published a study-specific protocol on the Open Science Framework (https://osf.io/n9mfq/).
Study eligibility
For the main IPDMA, studies and datasets were eligible if (1) they administered the EPDS; (2) diagnostic classification for current major depressive disorder or major depressive episode was done based on a validated semi-structured or fully structured interview using Diagnostic and Statistical Manual of Mental Disorders (DSM)32,33,34 or International Classification of Diseases (ICD) criteria35; (3) participants were women aged 18 or older who completed assessments during pregnancy or within 12 months of giving birth; (4) the EPDS and diagnostic interview were conducted within two weeks; and (5) participants were not limited to people receiving psychiatric assessment or seeking psychiatric care because screening is done to identify previously unrecognized cases. Datasets where not all participants were eligible were included if primary data allowed selection of eligible participants. There were no restrictions based on language or study design. For the present study, we only included datasets from primary studies that provided individual EPDS item scores for all 10 items, because only those datasets allowed us to generate EPDS-9 scores and compare the EPDS-9 and full EPDS.
Search strategy and selection of eligible studies
A medical librarian searched Medline, Medline In-Process and Other Non-Indexed Citations, PsycINFO, and Web of Science from database inception to October 3, 2018, using a peer-reviewed search strategy (Supplementary Methods 1). Additionally, investigators reviewed reference lists of relevant reviews and queried contributing authors about non-published studies. Search results were uploaded into RefWorks (RefWorks-COS, Bethesda, MD, USA). After de-duplication, unique citations were uploaded into DistillerSR (Evidence Partners, Ottawa, Canada), which was used to store and track search results, conduct screening for eligibility, document correspondence with primary study authors, and extract study characteristics.
Two investigators independently reviewed titles and abstracts for eligibility. For publications deemed potentially eligible by either reviewer, a full-text review was done by two investigators, also independently. Disagreements between reviewers after full-text reviews were resolved by consensus and a third investigator was consulted if necessary.
Data contribution, extraction, and synthesis
Authors of eligible datasets were invited to contribute de-identified primary data. We attempted to contact corresponding authors of eligible primary studies by email up to three times, as necessary. When authors did not respond to our emails, we tried to contact them by phone and emailed co-authors. There was no time limit for how long authors had to provide data.
Two investigators independently extracted information on the diagnostic interview administered and the country of study from the published reports. Any discrepancies were resolved by consensus. Participant-level data included in the synthesized dataset included country human development index (which reflects life expectancy, education, and income of a country)36, age, pregnant or postpartum status, diagnostic interview administered, major depression classification status, and EPDS item scores. We used major depressive disorder or major depressive episode based on DSM or ICD criteria; if both were reported, we prioritized major depressive episode because screening attempts to detect episodes of depression. Clinically, additional assessment would be needed to determine if episodes were related to major depressive disorder or another psychiatric disorder (bipolar disorder, persistent depressive disorder). We also prioritized DSM over ICD because DSM is more commonly used in existing studies. We used statistical weights to reflect sampling procedures if provided in the datasets, for instance, when primary studies administered a diagnostic interview to all participants with positive screening results but only a random sample of those with negative results. Some studies used sampling procedures that merited weights but did not use weights. For those studies, we used inverse selection probabilities to generate appropriate weights.
For all datasets, we verified that participant characteristics and screening accuracy results for the full EPDS matched those that had been published. When primary data and original publications were discrepant, we identified and corrected errors when possible and resolved any outstanding discrepancies in consultation with the original investigators. We transformed all study-level and individual-level participant data into a standardized format and combined in a single synthesized dataset. For nine studies that collected data at multiple time points (four with two time points, four with three time points, and one with four time points), we selected the time point with the most participants. If the number of participants was maximized at multiple time points, we selected the one with the most women who had major depression.
We used the Quality Assessment of Diagnostic Accuracy Studies-2 tool (QUADAS-2)37 to assess risk of bias of included studies. No QUADAS domain items, however, were associated with outcomes in our main EPDS IPDMA20. Furthermore, QUADAS is designed to assess risk of bias in estimates of screening accuracy but not study features that might bias differences between using a full scale and a minimally shortened version of that scale. Thus, QUADAS ratings are provided in Supplementary Methods 2 but were not include in analyses.
Statistical analyses
To evaluate the association of EPDS-9 and full EPDS scores for assessing depressive symptom severity, a Pearson correlation and a 95% confidence interval (CI) were first calculated between the EPDS-9 and full EPDS scores for each study, then we generated the pooled estimate of correlations, 95% CI, and the prediction interval (PI), with a random effect model that accounted for clustering within primary studies.
To compare correlations and the screening accuracy of the EPDS-9 and full EPDS, we included all primary studies combined across type of diagnostic interview reference standards (primary analysis). There are differences in the way different types of diagnostic interviews are designed and their likelihood of classifying major depression38,39,40,41,42, but, since in each primary study, EPDS-9 and full EPDS scores are compared to the same reference standard, we did not have reason to believe that differences between the two measures would depend on the specific reference standard used. Nonetheless, we separately analyzed primary studies by the type of diagnostic interview used as the reference standard (secondary analyses), as we did in the previously published main EPDS IPDMA20.
For all studies pooled and by reference standard, for the EPDS-9 and full EPDS cut-offs ≥ 7 to ≥ 15, separately, bivariate random-effects models using an adaptive Gauss Hermite quadrature with 1 quadrature point20,43. This 2-stage meta-analytic approach models sensitivity and specificity at the same time, taking the inherent correlation between them and the precision of estimates within studies into account. A random-effects model was used as we assumed true values of sensitivity and specificity would vary across primary studies. We estimated accuracy for cut-offs from 7 to 15 to provide a range around the most commonly used cut-offs of ≥ 10 and ≥ 13, consistent with our main IPDMA of the EPDS20.
To examine the equivalence in accuracy between the EPDS-9 and full EPDS across cut-offs, overall and by reference standard, we used the results of the random-effects meta-analyses at each cut-off to construct separate empirical receiver operating characteristic (ROC) curves and areas under the curve (AUC) based on the pooled estimates. Equivalence between the EPDS-9 and full EPDS sensitivity and specificity was evaluated at each cut-off separately. This allowed us to test whether the sensitivity and specificity of the EPDS-9 were similar to the full EPDS, up to a pre-specified maximum difference, that is, an equivalence margin44. In the present study, an equivalence margin of δ = 0.05 was used, which is the same margin that was used previously to compare the PHQ-8 and PHQ-931. CIs for the differences between the EPDS-9 and full EPDS sensitivity and specificity at each cut-off were constructed via a cluster bootstrap approach45,46, with resampling at the study and subject level. For each comparison, we ran 1000 iterations of the bootstrap. For each bootstrap iteration, the bivariate random-effects model was fitted to the EPDS-9 and full EPDS data, separately, and pooled sensitivities, specificities, and difference estimates between the EPDS-9 and full EPDS were computed. We compared the CIs around the pooled sensitivity and specificity differences to the equivalence margin of δ = 0.05. If the entire CI was between − 0.05 and + 0.05 then we rejected the hypothesis that there were differences large enough to be important and concluded that equivalence was present. If the entire CI was outside of the interval, then we failed to reject the hypothesis that the EPDS-9 and full EPDS were not equivalent. When the CIs crossed the ± 0.05 threshold, findings on equivalence were deemed indeterminate.
To investigate heterogeneity across studies, by overall and reference standard, we generated forest plots for the differences in sensitivity and specificity estimates between the EPDS-9 and full EPDS for cut-offs ≥ 10, ≥ 11 and ≥ 13 for each study. We also quantified heterogeneity at cut-offs ≥ 10, ≥ 11 and ≥ 13, by reporting the estimated variances of the random effects for the differences in the EPDS-9 and full EPDS sensitivity and specificity (τ2)47,48. Additionally, the 95% prediction intervals which we calculated reflect the range of true effects that can be expected in future settings or studies49.
All analyses were run in R software (R version R 3.5.050 and R Studio version 1.1.42351 using the lme4 package52.
Ethical approval
As this study involved secondary analysis of anonymized previously collected data, the Research Ethics Committee of the Jewish General Hospital determined that this project did not require research ethics approval. However, for each included dataset, we confirmed that the original study received ethics approval and that all patients provided informed consent.
Results
Search results and characteristics of the primary data
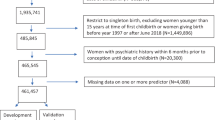
For the main IPDMA, 4434 unique titles and abstracts were identified from the electronic database searches. 4056 of these were excluded after title and abstract screening and 257 after full-text review (Supplementary Table S1), resulting in 121 eligible articles from 81 unique participant samples. Of these samples, 56 (69%) contributed datasets. Furthermore, authors of included studies contributed data from 2 unpublished studies. In total, 58 full EPDS studies were provided to the main IPDMA. For the present study, 17 studies (4626 participants, 659 major depression cases) with datasets that included full EPDS scores but not individual item scores were excluded. Thus, 41 studies (10,906 participants, 1407 major depression cases) were analyzed (Supplementary Figure S1). Characteristics of the included studies are shown in Supplementary Table S2. Characteristics of the 25 eligible studies that did not provide data and the 17 excluded studies that provided only EPDS total scores are shown in Supplementary Table S3.
There were 24 included primary studies (5412 participants, 803 major depression cases) that used semi-structured diagnostic interviews to assess major depression, 4 (3189 participants, 228 major depression cases) that used fully structured diagnostic interviews other than the Mini International Neuropsychiatric Interview (MINI), and 13 (2305 participants, 376 major depression cases) that used the MINI. The Structured Clinical Interview for DSM Disorders (SCID) was the most used semi-structured interview (22 studies, 5157 participants, 765 major depression cases), and the Composite International Diagnostic Interview was the most commonly used fully structured interview (3 studies, 2963 participants, 196 major depression cases). Characteristics of participants are shown in Table 1.
EPDS-9 and item 10 scores
As shown in Table 2, among participants in all studies, 1% of participants screened negative at an EPDS-9 cut-off of ≥ 10 but had a non-zero EPDS item 10 score. This percentage was also 1% at a cut-off of ≥ 11 and increased to 2% at a cut-off of ≥ 13. The correlation between the EPDS-9 and full EPDS scores was 0.998 (95% PI: 0.991, 0.999). The forest plot is shown in Supplementary Figure S2.
Screening accuracy of the EPDS-9 and full EPDS
ROC curves that compare sensitivity and specificity estimates of the EPDS-9 and full EPDS for cut-offs ≥ 7 to ≥ 15 are shown in Fig. 1, overall and separately by semi-structured, fully structured, and MINI reference standards. The ROC curves for the EPDS-9 and full EPDS were highly overlapping for overall and each reference standard. The AUC of the EPDS-9 and full EPDS for all interviews combined was 0.906 versus 0.910. By interview type, it was 0.905 versus 0.910 for semi-structured interviews, 0.924 versus 0.926 for fully structured interviews (excluding the MINI), and 0.902 versus 0.907 for the MINI.
Comparisons of sensitivity and specificity estimates between the EPDS-9 and full EPDS at cut-offs ≥ 7 to ≥ 15 for all reference standards combined are shown in Table 3. At cut-off ≥ 11, which maximized the sum of sensitivity and specificity of the full EPDS in the main IPDMA20, sensitivity was 0.78 (95% CI 0.71, 0.84) and specificity was 0.87 (95% CI 0.83, 0.90) for the EPDS-9 versus 0.80 (95% CI 0.74, 0.86) and 0.87 (95% CI 0.83, 0.90) for the full EPDS. Comparisons of sensitivity and specificity estimates between the EPDS-9 and full EPDS for cut-offs ≥ 7 to ≥ 15 across the three different reference standard categories are shown in Supplementary Table S4.
Overall, among all 41 primary studies, across cut-offs ≥ 7 to ≥ 15, sensitivity was between 1 percent higher and 4 percent lower for the EPDS-9 compared to the full EPDS (Table 3). At cut-off ≥ 10, the difference was − 0.02 (95% CI − 0.04, − 0.00), at cut-off ≥ 11, the difference was − 0.02 (95% CI − 0.04, − 0.01), and at cut-off ≥ 13, the difference was − 0.04 (95% CI − 0.08, − 0.02). The EPDS-9 and full EPDS were equivalent for cut-offs ≥ 7 to ≥ 12 and the equivalence was indeterminate for cut-offs ≥ 13 to ≥ 15. For specificity, the differences between the EPDS-9 and full EPDS were within 0.01 for all cut-offs. The EPDS-9 and full EPDS were equivalent for all cut-offs. As shown in Supplementary Table S4, in comparisons stratified by different reference standards, sensitivity estimates were similarly equivalent or indeterminate, and specificity estimates were equivalent at all cut-offs.
Forest plots illustrating the difference in sensitivity and specificity estimates between the EPDS-9 and full EPDS for the most used cut-offs ≥ 10, ≥ 11, and ≥ 13 are shown in Fig. 2. At cut-offs of ≥ 10, ≥ 11, and ≥ 13, low heterogeneity existed in the differences across all 41 studies; τ2 was < 0.01 for both differences in sensitivity and specificity, and the widest 95% prediction intervals were − 0.01 to 0.01 for differences in sensitivity and − 0.00 to 0.00 for differences in specificity. Forest plots of the differences of sensitivity and specificity estimates for cut-offs ≥ 10, ≥ 11 and ≥ 13 between the EPDS-9 and full EPDS among studies by reference standard category are shown in Supplementary Figure S3.
Discussion
The present study had two major findings. First, the scores between the continuous EPDS-9 and the full EPDS were highly correlated (0.998, 95% PI 0.991, 0.999). Second, across cut-offs, including the commonly used cut-offs of ≥ 10, ≥ 11, and ≥ 13, compared with the full EPDS, the EPDS-9 had similar sensitivity and specificity in screening major depression among pregnant and postpartum women, across all studies and for all three types of reference standard categories. In analyses pooled across reference standards, sensitivity was equivalent for cut-offs ≥ 7 to ≥ 12 and indeterminate for cut-offs ≥ 13 to ≥ 15. Specificity was equivalent for all cut-offs. Low heterogeneity in differences show that results were consistent across included studies.
Our findings about the EPDS-9 and full EPDS among pregnant and postpartum women are similar to results from a similar IPDMA on the equivalency of the screening accuracy of the PHQ-8 and PHQ-9, where the item removed in the shorter version also assessed self-harm. In that IPDMA, the screening accuracy between the PHQ-8 and PHQ-9 were similar across all cut-offs for detecting major depression31. Differences in sensitivity between the PHQ-8 and PHQ-9 were between 0.00 to 0.05, suggesting the sensitivity may be minimally reduced with the PHQ-8, although differences were deemed indeterminant. Specificity was equivalent for all cut-offs. We did not report positive predictive values in the present study, but these have been previously documented in our main IPDMA for the full EPDS20. For major depression prevalence values of 5–25%, positive predictive values for a cutoff of ≥ 11 compared to semi-structured interviews, for instance, ranged from 26 to 69%, and negative predictive values ranged from 93 to 99%. These would be similar for the EPDS-9.
Previous studies indicate that item 10 of the full EPDS overestimates the risk of suicidal ideation and identified substantially more people as at risk than scales designed to assess suicidal ideation risk24,28. Ideally, if researchers wish to assess suicide risk, a method designed specifically for that purpose, such as the P4 would be used given the limitations of EPDS item 1021. Potentially negative ramifications of using item 10 in research studies involve both resources and messaging to study participants. Ethically, all participants who score ≥ 1 on the item would need to be followed up with risk assessments, even though very few would be at risk, which could require substantial resources. Additionally, there is risk in impairing relationships with some women who must undergo these interviews even though they are not at risk. There are similar ramifications in clinical settings, where follow-up interviews would be needed for all women with positive EPDS screens and women with a non-zero item 10 score but negative screens overall.
The present study is the first meta-analysis using a large individual participant dataset to compare the measurement performance of the EPDS-9 and full EPDS, which is a major strength. The large sample size enabled us to generate precise estimates of correlations and equivalence for screening accuracy between the two versions of the EPDS. Furthermore, we compared results for the EPDS-9 and full EPDS from all studies and three different reference standard categories with all cut-offs, rather than just published cut-offs, which may result in bias due to selective cut-off reporting when individual participant data are not available53.
Limitations also need to be considered. First, we restricted meta-analysis to studies with complete data for full EPDS individual item scores (71%, 41 from 58 eligible studies) and were not able to include all studies. We do not know of any reason why studies that did and did not record item-level data might differ in the association between full EPDS and EPDS-9 scores. Secondly, although we categorized studies based on the interview administered, interviews might not have always been used as originally designed; for instance, it is possible that some interviewers may not have had the experience or training required to administer semi-structured interviews. The low heterogeneity in the main analysis, though, suggests that results are applicable across different diagnostic interviews. Third, we conducted a secondary analysis of data collected up to 2018 for a previously published IPDMA. Based on prediction intervals, which were all between − 0.01 to 0.01 for differences in sensitivity and − 0.00 to 0.00 for differences in specificity, however, additional data would not likely influence results meaningfully. It would not be a good use of resources to conduct additional studies on this research question. Fourth, we did not track inter-rater agreement for assessing eligibility at the title and abstract and full-text review levels.
In summary, this IPDMA showed that the EPDS-9 performs similarly to the full EPDS for assessing depressive symptom severity. The two EPDS versions also had similar screening accuracy in screening for major depression. The negative ramifications of false positive responses on item 10 suggest that using the EPDS-9 instead of the full EPDS should be considered as measurement performance is similar to the full EPDS.
Data availability
Data contribution agreements with primary study authors do not include permission to make their data publicly available, although the dataset used in this study will be archived through a McGill University repository (Borealis, https://borealisdata.ca/dataverse/depressdproject/). The R codes used for the analysis will be made publicly available through the same repository. Requests to access the dataset to verify study results but not for other purposes can be sent to the corresponding authors via the “Access Dataset” function on the repository website.
References
Stewart, D. E. & Vigod, S. N. Postpartum depression: Pathophysiology, treatment, and emerging therapeutics. Annu. Rev. Med. 70, 183–196 (2019).
Zeng, Y. et al. Retinoids, anxiety and peripartum depressive symptoms among Chinese women: A prospective cohort study. BMC Psychiatry 17, 278 (2017).
Gavin, N. I. et al. Perinatal depression: A systematic review of prevalence and incidence. Obstet. Gynecol. 106, 1071–1083 (2005).
Vesga-López, O. et al. Psychiatric disorders in pregnant and postpartum women in the United States. Arch. Gen. Psychiatry 65, 805–815 (2008).
Howard, L. M. et al. Non-psychotic mental disorders in the perinatal period. Lancet 384, 1775–1788 (2014).
Letourneau, N. L., Dennis, C., Cosic, N. & Linder, J. The effect of perinatal depression treatment for mothers on parenting and child development: A systematic review. Depress. Anxiety 34, 928–966 (2017).
Paulson, J. F. & Bazemore, S. D. Prenatal and postpartum depression in fathers and its association with maternal depression: A meta-analysis. JAMA 303, 1961–1969 (2010).
Stewart, D. E. & Vigod, S. Postpartum depression. N. Eng. J. Med. 375, 2177–2186 (2016).
Thombs, B. D. et al. Rethinking recommendations for screening for depression in primary care. CMAJ 184, 413–418 (2012).
Thombs, B. D. & Ziegelstein, R. C. Does depression screening improve depression outcomes in primary care?. BMJ 348, g1253 (2014).
Austin, M. P., Highet, N. & Expert Working Group. Mental health care in the perinatal period: Australian clinical practice guideline. Centre of Perinatal Excellence, 2017. Available at https://www.clinicalguidelines.gov.au/portal/2586/mental-health-care-perinatal-period-australian-clinical-practice-guideline.
Siu, A. L. et al. Screening for depression in adults: US preventive services task force recommendation statement. JAMA 315, 380–387 (2016).
Hill, C. An evaluation of screening for postnatal depression against NSC criteria. National Screening Committee, 2010. Available at https://legacyscreening.phe.org.uk/policydb_download.php?doc=140.
Joffres, M. et al. Recommendations on screening for depression in adults. CMAJ 185, 775–782 (2013).
Cox, J. L., Holden, J. M. & Sagovsky, R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 150, 782–786 (1987).
Hewitt, C. et al. Methods to identify postnatal depression in primary care: An integrated evidence synthesis and value of information analysis. Health Technol. Assess. 13(1–145), 147–230 (2009).
Cox, J. Thirty years with the Edinburgh Postnatal Depression Scale: Voices from the past and recommendations for the future. Br. J. Psychiatry 214, 127–129 (2019).
Gibson, J., McKenzie-McHarg, K., Shakespeare, J., Price, J. & Gray, R. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr. Scand. 119, 350–364 (2009).
O’Connor, E., Rossom, R. C., Henninger, M., Groom, H. C. & Burda, B. U. Primary care screening for and treatment of depression in pregnant and postpartum women: Evidence report and systematic review for the US Preventive Services Task Force. JAMA 315, 388–406 (2016).
Levis, B. et al. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: Systematic review and meta-analysis of individual participant data. BMJ 371, m4022 (2020).
Dube, P., Kroenke, K., Bair, M. J., Theobald, D. & Williams, L. S. The P4 screener: Evaluation of a brief measure for assessing potential suicide risk in 2 randomized effectiveness trials of primary care and oncology patients. Prim. Care Companion J. Clin. Psychiatry 12, PCC.10m00978 (2010).
Wisner, K. L. et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiat. 70, 490–498 (2013).
Lindahl, V., Pearson, J. L. & Colpe, L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment. Health 8, 77–87 (2005).
Pope, C. J., Xie, B., Sharma, V. & Campbell, M. K. A prospective study of thoughts of self-harm and suicidal ideation during the postpartum period in women with mood disorders. Arch Womens Ment. Health 16, 483–488 (2013).
Kim, J. J. et al. Suicide risk among perinatal women who report thoughts of self-harm on depression screens. Obstet. Gynecol. 125, 885–893 (2015).
Brouwers, E. P., van Baar, A. L. & Pop, V. J. Does the Edinburgh Postnatal Depression Scale measure anxiety?. J. Psychosom. Res. 51, 659–663 (2001).
Edge, D. What do Black Caribbean women think about screening with the EPDS? In Screening for Perinatal Depression (eds C. Henshaw & S. Elliott) 162–170 (Jessica Kingsley Publishers, London, 2005).
Loyal, D., Sutter, A.-L. & Rascle, N. Screening beyond postpartum depression: Occluded anxiety component in the EPDS (EPDS-3A) in french mothers. Matern. Child Health J. 24, 369–377 (2020).
Daly-Cano, M. R. Refining the Edinburgh Postpartum Depression screening: Is there a distinct role for anxiety? University of Rhode Island, 2018. Available at https://digitalcommons.uri.edu/oa_diss/857/.
Thombs, B. D. et al. Diagnostic accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for detecting major depression in pregnant and postnatal women: Protocol for a systematic review and individual patient data meta-analyses. BMJ Open 5, e009742 (2015).
Wu, Y. et al. Equivalency of the diagnostic accuracy of the PHQ-8 and PHQ-9: A systematic review and individual participant data meta-analysis. Psychol. Med. 50, 1368–1380 (2020).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-III, 3rd edn, revised (1987).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV, 4th edn. (1994).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV, 4th edn revised (2000).
World Health Organization. The ICD-10 Classifications of Mental and Behavioural Disorder. Clinical Descriptions and Diagnostic Guidelines (1992).
United Nations. International Human Development Indicators (2021). Available at http:// hdr.undp.org/en/countries.
Whiting, P. F. et al. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 155(8), 529–536 (2011).
Brugha, T. S., Bebbington, P. E. & Jenkins, R. A difference that matters: Comparisons of structured and semi-structured psychiatric diagnostic interviews in the general population. Psychol. Med. 29(5), 1013–1020 (1999).
Levis, B. et al. Probability of major depression diagnostic classification using semi-structured vs. fully structured diagnostic interviews. Br. J. Psychiatry 212, 377–85 (2018).
Levis, B. et al. Comparison of major depression diagnostic classification probability using the SCID, CIDI and MINI diagnostic interviews among women in pregnancy or postpartum: An individual participant data meta-analysis. Int. J. Methods Psychiatr. Res. 28, e1803 (2019).
Wu, Y. et al. Probability of major depression diagnostic classification based on the SCID, CIDI and MINI diagnostic interviews controlling for Hospital Anxiety and Depression Scale—Depression subscale scores: An individual participant data meta-analysis of 73 primary studies. J. Psychosom. Res. 129, 109892 (2020).
Wu, Y. et al. Probability of major depression classification based on the SCID, CIDI and MINI diagnostic interviews: A synthesis of three individual participant data meta-analyses. Psychother. Psychosom. 90, 28–40 (2021).
Riley, R. D., Dodd, S. R., Craig, J. V., Thompson, J. R. & Williamson, P. R. Meta-analysis of diagnostic test studies using individual patient data and aggregate data. Stat. Med. 27, 6111–6136 (2008).
Walker, E. & Nowacki, A. S. Understanding equivalence and noninferiority testing. J. Gen. Intern. Med. 26, 192–196 (2011).
van der Leeden, R., Busing, FMTA & Meijer, E. Bootstrap methods for two-level models. Technical Report PRM 97–04. Leiden University, Department of Psychology: Leiden, The Netherlands (1997).
van der Leeden, R., Meijer, E. & Busing, FMTA. Chapter 11: Resampling multilevel models. In Handbook of Research Methods in Abnormal and Clinical Psychology (D. McKay). (ed. J. Leeuw, & E. Meijer) 401–433 (Springer, New York, 2008).
Fagerland, M. W., Lydersen, S. & Laake, P. Recommended tests and confidence intervals for paired binomial proportions. Stat. Med. 33, 2850–2875 (2014).
Higgins, J. P. T. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
IntHout, J., Ioannidis, J. P. A., Rovers, M. M. & Goemen, J. J. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open 6, e010247 (2016).
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, 2020. Available at https://www.R-project.org/.
RStudio Team. RStudio: Integrated Development for R. RStudio, Inc., Boston, MA, 2020. Available at http://www.rstudio.com/.
Bates, D., Maechler, M., Bolker, B. M. & Walker, S. C. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 67, 1–48 (2015).
Neupane, D. et al. Selective cutoff reporting in studies of the accuracy of the Patient Health Questionnaire-9 and Edinburgh Postnatal Depression Scale: Comparison of results based on published cutoffs versus all cutoffs using individual participant data meta-analysis. Int. J. Methods Psychiatr. Res. 30, e1873 (2021).
Funding
This study was funded by the Canadian Institutes of Health Research (CIHR, KRS-140994). Dr. Qiu was supported by a scholarship from the China Scholarship Council. Drs. Wu and Levis were supported by Fonds de recherche du Québec—Santé (FRQ-S) Postdoctoral Training Fellowships. Dr. Benedetti was supported by a Fonds de recherche du Québec – Santé (FRQS) researcher salary award. Dr. Thombs was supported by a Tier 1 Canada Research Chair. Ms. Rice was supported by a Vanier Canada Graduate Scholarship. The primary study by Alvarado et al. was supported by the Ministry of Health of Chile. The primary study by Barnes et al. was supported by a grant from the Health Foundation (1665/608). The primary study by Beck et al. was supported by the Patrick and Catherine Weldon Donaghue Medical Research Foundation and the University of Connecticut Research Foundation. The primary study by Helle et al. was supported by the Werner Otto Foundation, the Kroschke Foundation, and the Feindt Foundation. The primary study by Figueira et al. was supported by the Brazilian Ministry of Health and by the National Counsel of Technological and Scientific Development (CNPq) (Grant no.403433/2004-5). The primary study by Couto et al. was supported by the National Counsel of Technological and Scientific Development (CNPq) (Grant no. 444254/2014-5) and the Minas Gerais State Research Foundation (FAPEMIG) (Grant no. APQ-01954-14). The primary study by Chorwe-Sungani et al. was supported by the University of Malawi through grant QZA-0484 NORHED 2013. The primary study by de Figueiredo et al. was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo. The primary study by Tissot et al. was supported by the Swiss National Science Foundation (grant 32003B 125493). The primary study by Fernandes et al. was supported by grants from the Child: Care Health and Development Trust and the Department of Psychiatry, University of Oxford, Oxford, UK, and by the Ashok Ranganathan Bursary from Exeter College, University of Oxford. Dr. Fernandes is supported by a University of Southampton National Institute for Health Research (NIHR) academic clinical fellowship in Paediatrics. The primary study by van Heyningen et al. was supported by the Medical Research Council of South Africa (fund no. 415865), Cordaid Netherlands (Project 103/10002 G Sub 7) and the Truworths Community Foundation Trust, South Africa. Dr. van Heyningen was supported by the National Research Foundation of South Africa and the Harry Crossley Foundation. VHYTHE001/1232209. The primary study by Tendais et al. was supported under the project POCI/SAU-ESP/56397/2004 by the Operational Program Science and Innovation 2010 (POCI 2010) of the Community Support Board III and by the European Community Fund FEDER. The primary study by Fisher et al. was supported by a grant under the Invest to Grow Scheme from the Australian Government Department of Families, Housing, Community Services and Indigenous Affairs. The primary study by Green et al. was supported by a grant from the Duke Global Health Institute (453-0751). The primary study by Howard et al. was supported by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research Programme (Grant Reference Numbers RP-PG-1210-12002 and RP-DG-1108-10012) and by the South London Clinical Research Network. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. The primary study by Kettunen et al. was supported with an Annual EVO Financing (Special government subsidies from the Ministry of Health and Welfare, Finland) by North Karelia Central Hospital and Päijät-Häme Central Hospital. The primary study by Phillips et al. was supported by a scholarship from the National Health and Medical and Research Council (NHMRC). The primary study by Roomruangwong et al. was supported by the Ratchadaphiseksomphot Endowment Fund 2013 of Chulalongkorn University (CU-56-457-HR). The primary study by Martínez et al. was supported by Iniciativa Científica Milenio, Chile, process # IS130005 and by Fondo Nacional de Desarrollo Científico y Tecnológico, Chile, process # 1130230. The primary study by Nakić Radoš et al. was supported by the Croatian Ministry of Science, Education, and Sports (134-0000000-2421). The primary study by Usuda et al. was supported by Grant-in-Aid for Young Scientists (A) from the Japan Society for the Promotion of Science (primary investigator: Daisuke Nishi, MD, PhD), and by an Intramural Research Grant for Neurological and Psychiatric Disorders from the National Center of Neurology and Psychiatry, Japan. The primary study by Pawlby et al. was supported by a Medical Research Council UK Project Grant (number G89292999N). The primary study by Rochat et al. was supported by grants from the University of Oxford (HQ5035), the Tuixen Foundation (9940), the Wellcome Trust (082384/Z/07/Z and 071571), and the American Psychological Association. Dr. Rochat receives salary support from a Wellcome Trust Intermediate Fellowship (211374/Z/18/Z). The primary study by Rowe et al. was supported by the diamond Consortium, beyondblue Victorian Centre of Excellence in Depression and Related Disorders. The primary study by Comasco et al. was supported by funds from the Swedish Research Council (VR: 521-2013-2339, VR:523-2014-2342), the Swedish Council for Working Life and Social Research (FAS: 2011-0627), the Marta Lundqvist Foundation (2013, 2014), and the Swedish Society of Medicine (SLS-331991). The primary study by Smith-Nielsen et al. was supported by a grant from the charitable foundation Tryg Foundation (Grant ID no 107616). The primary study by Prenoveau et al. was supported by The Wellcome Trust (grant number 071571). The primary study by Stewart et al. was supported by Professor Francis Creed’s Journal of Psychosomatic Research Editorship fund (BA00457) administered through University of Manchester. The primary study by Su et al. was supported by grants from the Department of Health (DOH94F044 and DOH95F022) and the China Medical University and Hospital (CMU94-105, DMR-92-92 and DMR94-46). The primary study by Tandon et al. was funded by the Thomas Wilson Sanitarium. The primary study by Tran et al. was supported by the Myer Foundation who funded the study under its Beyond Australia scheme. Dr. Tran was supported by an early career fellowship from the Australian National Health and Medical Research Council. The primary study by Vega-Dienstmaier et al. was supported by Tejada Family Foundation, Inc, and Peruvian-American Endowment, Inc. The primary study by Yonkers et al. was supported by a National Institute of Child Health and Human Development grant (5 R01HD045735). No other authors reported funding for primary studies or for their work on this study. No funder had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Consortia
Contributions
X.Q., Y.W., Y.S., B.L., J.T.B., P.C., J.P.A.I., S.M., R.C.Z., S.N.V., A.B., and B.D.T. were responsible for the study conception and design. Y.W., Y.S., B.L., and B.D.T. contributed to data extraction, coding, evaluation of included studies, and data synthesis. X.Q., Y.W., J.T., A.B., and B.D.T. contributed to data analysis and interpretation. X.Q., Y.W., Y.S., B.L., A.B. and B.D.T. drafted the manuscript.
Members of the DEPRESSD EPDS Group contributed: To data extraction, coding, and synthesis: CH, AK, PMB, DNeupane, ZN, MI, DBR, MA, MJC, KER. Via the design and conduct of database searches: LAK. As members of the DEPRESSD Steering Committee, including conception and oversight of collaboration: SG, SBP. As a knowledge user consultant: NDM. By contributing included datasets: RA, JB, CTB, CB, HC, TceC, GCS, VE, NF, EF, GF, MF, SF, BF, JRWF, EPG, SH, LMH, PAK, JK, ZK, AAL, MM, PM, SNR, Dnishi, SJP, TJR, HJR, DJS, Askalkidou, JSN, Astein, KPS, ISP, MT, SDT, IT, AT, TDT, Ktrevillion, Kturner, MSV, TvH, JMVD, KW, KAY. All authors, including group authors, provided a critical review and approved the final manuscript. AB and BDT contributed equally as co-senior authors and are the guarantors; they had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analyses. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding authors
Ethics declarations
Competing interests
All authors have completed the ICJME uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years with the following exceptions: Dr. Beck declares that she receives royalties for her Postpartum Depression Screening Scale published by Western Psychological Services. Dr. Howard declares that she has received personal fees from NICE Scientific Advice, outside the submitted work. Dr. Sundström-Poromaa declares that she has served on advisory boards and acted as invited speaker at scientific meetings for MSD, Novo Nordisk, Bayer Health Care, and Lundbeck A/S. Dr. Yonkers declares that she receives royalties from UpToDate, outside the submitted work. All other authors declare no other relationships or activities that could appear to have influenced the submitted work. No funder had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Qiu, X., Wu, Y., Sun, Y. et al. Individual participant data meta-analysis to compare EPDS accuracy to detect major depression with and without the self-harm item. Sci Rep 13, 4026 (2023). https://doi.org/10.1038/s41598-023-29114-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-29114-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.