Abstract
Oral health condition, bone mineral density, skeletal muscle mass, fall, fracture, and frailty seem to be strongly interconnected. This study aimed to investigate associations between probability of osteoporotic fractures and oral health in the elderly. In total, 2322 Korean subjects from the 2008—2009 Korea National Health and Nutritional Examination Survey aged over 65 years were included. The 10-year probabilities of major and hip fractures were calculated using the Fracture Risk Assessment (FRAX) tool. Data on anthropometry, skeletal bone mineral density, sociodemographic characteristics, physical activity, individual history of fractures and falls, parental history of osteoporosis, number of teeth, metabolic syndrome, the Decayed, Missing, and Filled permanent Teeth index, and Community Periodontal Index (CPI), were collected. Participants were classified into three groups based on FRAX score for major osteoporotic fractures. A multivariate linear regression analysis was conducted to analyze associations between FRAX scores and oral health-related factors, adjusting for confounding factors. BMI, presence of metabolic syndrome, number of teeth, dental patterns, and CPI score showed significant differences among three groups in males and females. Results from multivariate linear regression analysis demonstrated significant relationships between total tooth number and probabilities of fracture in male and female elderly. The interdisciplinary approach for handling osteoporosis and sarcopenia including dentists, physicians is necessary to facilitate a better quality of life in the elderly.
Similar content being viewed by others
Introduction
Aging is accompanied by neuromuscular, immunological, and endocrinological changes in the body that may lead to frailty, featured by weight loss, weakness, slowness, low physical activity, and reduced energy in the elderly1. Falls and fractures have been regarded as serious issues in geriatric medicine, as these may lead to frailty, which in turn may result in increased probabilities of falls and fractures2. Osteoporosis and sarcopenia are among the most common diseases in the elderly populations and are associated with the increased prevalence of falls and fractures3,4. Fall-related fractures can not only influence the quality of life but also lead to higher mortality rates and increased medical and healthcare costs. Therefore, predicting the risk factors for falls and fractures and developing strategies to minimize them in the elder populations are the main concerns of clinicians and policy makers for aged societies.
Oral health condition, bone mineral density (BMD), skeletal muscle mass, and frailty seem to be strongly interconnected5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22. The decreased number of teeth has been shown to have significant correlations with the amount of skeletal muscle mass, handgrip strength, and gait speed in the elderly8,10,17,19. Furthermore, the link between oral health status and skeletal BMD has also been discussed7,9,12,13,14,15,16,22. Finally, poor oral health can result in increased physical frailty, disability, and mortality rate5,6,11,18,21. Diverse dental problems in the elderly can result in chewing difficulties which contribute to the changes in food selection that may ultimately result in malnutrition and low bone and muscle mass20,23. The influences of poor oral conditions and occlusal support on posture stabilization and balance function, which might cause fall-related events, have been suggested24. Though the fragmentary knowledge on the association between oral health and fall- and fracture-related factors, such as BMD, muscle mass, body balance, balancing function, and frailty, has been proposed, thorough and integrated discussions about the relationships among those factors have not been fully elucidated.
Several reports have suggested links between tooth loss and an increased incidence of falls and fractures. One case–control study revealed that the number of missing teeth was related to the probability of hip fractures but this study included a small sample size, which inevitably compromised the significance of the results25. Another prospective study showed that individuals with more than 15 missing teeth had a higher risk of hip fractures26 and the other study demonstrated the relationships among tooth number, occlusal balance, and the incidence of diverse types of fractures in the elderly27. Moreover, one study showed that having 19 or fewer teeth without dentures was associated with a higher risk for incident falls in older adults28. However, none of these studies included information on other confounding factors such as skeletal BMD and muscle mass.
Currently, the fracture risk assessment (FRAX), which is a country- and ethnicity-specific instrument developed by the World Health Organization (WHO), is the most widely used fracture prediction tool for adults. In the FRAX, the 10-year probability of both major and hip fractures can be calculated using 10 clinical risk factors29,30. The aim of the present study was to investigate the associations between the 10-year probabilities of fracture and oral health-related factors in the Korean population using data from the 2008–2009 Korea National Health and Nutritional Examination Survey (KNHANES) and FRAX algorithm.
Materials and methods
Study population
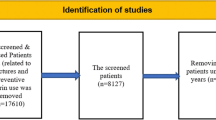
The present study adopted data from the 2008—2009 KNHANES. KNHANES is a nationwide population-based survey conducted by the Korean Center for Disease Control and Prevention. This research included 2322 Korean subjects (959 males, 1363 females) over 65-year old. To include a representative sample of the population, a clustered, multistage, and stratified probability approach was applied. This survey consisted of a nutritional survey, a general health interview, a health assessment, and an oral examination. All participants provided written informed consent following approval from the Institutional Review Board of the Korean Center of Disease Control and Prevention. The ethical approval of this research protocol was exempted by the Institutional Review Board of the tertiary University Hospital (AJIRB-MED-EXP-21–307). Data from eligible participants aged over 65 years were included, and participants with missing data in the health assessments, questionnaires, BMD measurement, and oral examination were excluded (Fig. 1).
Anthropometric measurements
Qualified staff measured the weight (kg) and height (cm) of all participants. Body mass index (BMI) was calculated by dividing the weight by the square of the height31.
BMD assessments
Whole body dual-energy X-ray absorptiometry (DXA) was applied using a QDR Discovery fan beam densitometer (Hologic, Bedford, MA, USA). The areal BMDs (aBMDs) of the total hip, femoral neck, and lumbar spine and body lean mass were assessed using DXA32. Data from DXA were analyzed on the basis of the standard techniques of the Korean Society of Osteoporosis and Hologic Discovery software (version 13.1).
Sociodemographic parameters, parental history of osteoporosis, and individual history of fractures and falls
The data on sociodemographic data and health behavior such as cigarette smoking, alcohol drinking, levels of physical activity were determined by self-administered survey from KNHANES. The monthly household income and the number of household members were collected for each participant, and the participants were then divided into the following four different categories: < 25% (the lowest quartile group), 25—49%, 50–74%, and 75—100% (the highest quartile group). Education level was also classified into four groups on the basis of the Korean education system: below primary school (≤ 6 years of institutionalized education), middle school (7—9 years of institutionalized education), high school (10—13 years of institutionalized education), and college or higher education (≥ 14 years of institutionalized education).
Cigarette smoking behavior was divided into the following three groups: nonsmokers, smokers who currently smoke and have smoked less than five packs in their entire lives, and smokers who currently smoke and have smoked equal or more than five packs in their entire lives. Alcohol drinking was classified into the following two groups: none or light drinkers (0—3 days/month) and moderate to heavy drinkers (≥ 4 days/month). Physical activity level was measured using the Korean version of the International Physical Activity Questionnaire (IPAQ) short form33. The respondents were grouped as performing high/moderate intensity physical activity more than 30 min or over 5 times/week, respectively.
Data on parental history of osteoporosis and individual history of fractures of the spine, hip, or distal radius were collected. Data on individual experiences of falls in the past one year were also included.
Metabolic syndrome
Diagnosis of metabolic syndrome was performed on the basis of the criteria suggested by previous reports34,35. Metabolic syndrome was diagnosed if participants had at least three fulfilling criteria out of the following five criteria: 1) a clinical diagnosis of diabetes treated with oral hypoglycemic medication or insulin or a fasting serum glucose level of 110 mL/dL or higher; 2) arterial blood pressure of 130/85 mm Hg or higher or current use of antihypertensive medication; 3) plasma triglyceride level of 150 mg/dL or higher; 4) high-density lipoprotein cholesterol level of ≤ 50 mg/dL for females or ≤ 40 mg/dL for males; or 5) a waist size greater than 80 cm for females or 90 cm for males.
Evaluation of the status of oral health
Oral examinations were conducted by trained dentists. Periodontal health status was determined using the Community Periodontal Index (CPI) based on the criteria given by the WHO36. CPI scores were categorized as follows: 0, healthy gingiva; 1, gingival bleeding; 2, presence of calculus; 3, pocket depth of 3.5—5.5 mm; and 4, pocket depth of 5.5 mm or more. The ten index teeth were #11, 16, 17, 26, 27, 31, 36, 37, 46, and 47. If no index tooth was present in a sextant qualifying for examination, the adjacent remaining tooth in that sextant was selected. The Decayed, Missing, and Filled permanent Teeth (DMFT) index and the number of teeth present were also measured37. Dental patterns including samples with more than 20 teeth, those with teeth number more than 0 but less than 20, and edentulous were also determined.
Fracture probability calculations
The 10-year probabilities of major and hip fractures were calculated using the FRAX tool (version 3.7, South Korean model), which calculated the probability based on age, sex, aBMD of the femoral neck, individual history of fractures, parental history of hip fractures, current tobacco use, rheumatoid arthritis, alcohol consumption (more than three units per day), secondary osteoporosis, and long-term use of glucocorticoids29. Data on individual histories of fractures, current tobacco use, rheumatoid arthritis, alcohol consumption, and secondary osteoporosis were collected from the health interview surveys. As the 2008—2009 KNHANES did not include data regarding the long-term use of glucocorticoids or parental history of hip fractures, negative answers were entered into the FRAX tool as in previous reports38,39,40.
Statistical analysis
Statistical analyses were performed on the basis of a complex design including stratification, clustering, and weighting. Sample weights were constructed for the sample participants to represent the Korean population by accounting for the survey nonresponses, complex survey design, and stratification (according to age, sex, and geographic area).
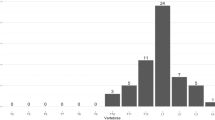
All analyses were conducted separately for males and females owing to the different amounts of skeletal muscle mass and background bone metabolism rates between the sexes. The participants were classified into three groups based on the 10-year probable risk of major fracture41. The participants whose FRAX scores were less than 10% were classified as Low-Risk group (10% > FRAX score), whose FRAX scores between 10 to 20% were as Moderate-Risk group (20 > FRAX score ≥ 10%), and whose FRAX scores above 20% were as High-Risk group (FRAX score ≥ 20%). Independent t-tests and Rao-Scott chi-square tests were applied to compare the differences in the sociodemographic, anthropometric, and behavioral factors, the number of teeth, DMFT, CPI, 10-year probabilities of major and hip fractures, lean body mass, and skeletal BMD for continuous and categorical variables, respectively. Multivariate linear regression analysis was applied to analyze the associations between the 10- year probabilities of major or hip fractures and oral health-related factors, adjusted for the potential confounders including lean body mass, presence of metabolic syndrome, parental history of osteoporosis, and recent experience of falls. Each anthropometric and sociodemographic variable with a significant association with FRAX scores in the univariate analysis was integrated into the multivariate linear regression analysis to identify interdependent contributions. The variables which included in calculation of FRAX score such as age, aBMD of the femoral neck, individual history of fractures, current smoking, and alcohol consumption were excluded in multivariate analysis. Finally, the independent variables were total teeth number, DMFT, CPI, lean body mass, incidence of metabolic syndrome, history of fall, and parental osteoporotic history and the outcome variable were major fracture probability and hip fracture probability.
Ethical approval and informed to consent
Written informed consents were obtained from all participants following approval from the Institutional Review Board of the Korean Center of Disease Control and Prevention. The ethical approval of this research protocol was exempt by the Institutional Review Board of the University Hospital (AJIRB-MED-EXP-21–307).
Results
No significant differences in the levels of household income and education, smoking status, alcohol consumption, the intensity of physical activities, parental history of osteoporosis, individual history of recent experience of falls, and history of fracture of the lumbar spine, hip, or distal radius were detected among the three groups in both male and female elderly. Significant differences in BMI, existence of metabolic syndrome, number of present teeth, dental patterns, and CPI score were observed for both males and females, whereas the DMFT showed significant differences among groups only in the female elderly. There were significant differences in the aBMDs of the femoral neck among the three groups in males. Otherwise, the aBMD of the lumbar spine and lean body mass showed significant differences among the three groups in the female elderly (Tables 1, 2).
The results from the multivariate linear regression analysis demonstrated significant relationships between total teeth number and 10-year major and hip fracture probabilities in both male and female elderly. Lean body mass did not show significant associations with FRAX score in both male and female elderly. On the other hand, the individual’s recent experience of falls interacted with the probabilities of both major and hip fractures only in the female elderly but not in the male elderly (Table 3).
Discussion
The prevention of falls and fractures has been regarded as one of the main issues in aged societies because those may lead to frailty and increased medical and social burdens. Many efforts have been attempted to determine the risk factors for falls and fractures. Previous studies have demonstrated the strong relationships among oral health-related factors, the incidence of falls, amount of skeletal muscle mass, frailty, skeletal BMD, physical performance, and mortality rate in the elderly population5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,27. Even though, the fragmentary associations between those factors have been reported previously, the integrated knowledge of interactions among the above factors has not been thoroughly discussed. Hence, the purpose of the present study was to investigate the association between the probabilities of major and hip fractures and oral health related factors, muscle mass, and skeletal BMD in the elder Korean population aged over 65 years using data from the KNHANES and FRAX algorithm.
The novel finding of the present study was the strong link between the probabilities of fractures and the number of teeth present in the elderly. The aforementioned results from the multivariate linear regression analysis demonstrated that the number of teeth present showed significant associations with the 10-year probabilities of major and hip fractures in both male and female elderly after adjusting for confounding factors. Losing teeth in the elderly may lead to chewing difficulty, contributing to the changes in food selection, malnutrition, and low bone and muscle mass20,23. Moreover, several previous studies have proposed the role of remaining teeth, bilateral occlusal support, and proprioception from periodontal ligaments on postural balance and incidence of falls23,24,27. Although, the precise occlusal condition could not be derived from KNHANES data, the role the remaining teeth on the risk of fracture, including keeping nutritional balance which has associations with bone and muscle mass and body balancing capability which may lead to the occurrence of falls, could be assumed.
Even though the CPI scores showed significant interactions with risk of osteoporotic fractures in univariate analysis, the elderly in high risk group did not show more severe periodontal health status than elderly in low and moderate risk group. Owing to the calculating method of CPI index, the individuals with higher number of teeth loss could have less CPI scores than those with higher remaining teeth with periodontitis or gingivitis. The results from the present study could carefully suggest that the role of number of remaining teeth in the oral cavity would be more important than the inflammatory status in periodontium on incidence of osteoporotic fracture in elderly.
One interesting point was that significant associations between the individual history of falls and FRAX scores were detected in the female elderly only. Generally, the female elderly has lower skeletal BMD and fragile microstructures of bone compared to male elderly due to hormonal changes. Therefore, the relative impact of fall down including osteoporotic fracture would be much higher in female elderly than those in male elderly with less fragile bony structure.
To the best of our knowledge, the present study is the first study to reveal the relationships between the probabilities of fractures and oral health status after adjusting for factors related to osteoporosis and sarcopenia with sufficient sample size. However, this study has several limitations. First of all, due to the cross-sectional study design, the causal relationships between oral health status and actual fracture risk could not be revealed. Secondly, lack of information about long-term glucocorticoid use and parental hip fracture history in the 2008–2009 KNHANES databases could have led to distorted results being derived from the FRAX tool. Despite these limitations, this study still has value for clinicians and policy makers, that studies with a relatively large size of samples from an authorized institution with a proper study design could provide valid and meaningful results.
Good oral health influences the quality of life in a myriad way, including social interactions, communications, self-esteem, resilience, and adequate nutritional intake. Elder adults with oral health problems may experience social isolation and functional decline. Fractures in the elderly are a complex process determined by a combination of diverse factors. As the tooth number in the elderly is an indicator of physical, mental, and social well-being, it can be considered as a potential parameter of fracture risk in elder population. Hence, the oral health related factors, particularly the number of remaining teeth, can have strong associations with fracture probabilities in elder populations. A comprehensive understanding of the necessities of oral healthcare is warranted for dentists, physicians, and even policy makers to facilitate a better quality of life in the elderly and saving social and medical costs in aged society. From this study, deriving social consensus of necessities of interdisciplinary approaches for managing falls and fracture including oral care could be expected.
Data availability
The datasets used and/or analyzed during the current study are available from the homepage of Korean Center for Disease Control and Prevention (http://knhanes.kdca.go.kr) with no restriction apply to the availability of these data.
References
Fried, L. P., Ferrucci, L., Darer, J., Williamson, J. D. & Anderson, G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J. Gerontol. A Biol. Sci. Med. Sci. 59, 255–263 (2004).
Rolland, Y. et al. Frailty, osteoporosis and hip fracture: causes, consequences and therapeutic perspectives. J. Nutr. Health Aging 12, 335–346 (2008).
Yeung, S. S. Y. et al. Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle 10, 485–500 (2019).
Gauthier, A. et al. Epidemiological burden of postmenopausal osteoporosis in the UK from 2010 to 2021: Estimations from a disease model. Arch. Osteoporos 6, 179–188 (2011).
Watanabe, Y. et al. Relationship between frailty and oral function in community-dwelling elderly adults. J. Am. Geriatr. Soc. 65, 66–76 (2017).
Tanaka, T. et al. Oral frailty as a risk factor for physical frailty and mortality in community-dwelling elderly. J. Gerontol. A Biol. Sci. Med. Sci. 73, 1661–1667 (2018).
Tamut, T. et al. Effect of bone mineral density on masticatory performance and efficiency. Gerodontology 29, e83-87 (2012).
Suzuki, M. et al. Relationship between characteristics of skeletal muscle and oral function in community-dwelling older women. Arch. Gerontol. Geriatr. 79, 171–175 (2018).
Singhal, S. et al. The effect of osteoporosis on residual ridge resorption and masticatory performance in denture wearers. Gerodontology 29, e1059-1066 (2012).
Shin, H. S. Handgrip strength and the number of teeth among Korean population. J. Periodontol. 90, 90–97 (2019).
Ramsay, S. E. et al. Influence of poor oral health on physical frailty: A population-based cohort study of older British men. J. Am. Geriatr. Soc. 66, 473–479 (2018).
Pan, M.Y., Hsieh, T.C., Chen, P.H. & Chen, M.Y. Factors associated with tooth loss in postmenopausal women: A community-based cross-sectional study. Int. J. Environ. Res. Public Health 16(2019).
Laudisio, A. et al. Masticatory dysfunction is associated with osteoporosis in older men. J. Clin. Periodontol. 34, 964–968 (2007).
Kim, H. J. et al. Oral health behaviors and bone mineral density in South Korea: The 2008–2010 Korean National Health and Nutrition Examination Survey. J. Bone Miner. Metab. 34, 225–233 (2016).
Kim, C. S. et al. Relationship between bone mineral density, its associated physiological factors, and tooth loss in postmenopausal Korean women. BMC Womens Health 15, 65 (2015).
Jang, K. M. et al. Tooth loss and bone mineral density in postmenopausal South Korean women: The 2008–2010 Korea National Health and Nutrition Examination Survey. Maturitas 82, 360–364 (2015).
Iwasaki, M. et al. The association between dentition status and sarcopenia in Japanese adults aged >/=75 years. J. Oral Rehabil. 44, 51–58 (2017).
Castrejon-Perez, R. C., Borges-Yanez, S. A., Gutierrez-Robledo, L. M. & Avila-Funes, J. A. Oral health conditions and frailty in Mexican community-dwelling elderly: A cross sectional analysis. BMC Public Health 12, 773 (2012).
Lee, J. H., Lee, S. Y., Han, K. & Han, J. S. Relationship between oral health behaviour and handgrip strength: A cross-sectional study with 7589 Korean adults. Acta Odontol. Scand. 78, 438–444 (2020).
Castrejon-Perez, R. C. et al. Oral disease and 3-year incidence of frailty in Mexican older adults. J. Gerontol. A Biol. Sci. Med. Sci. 72, 951–957 (2017).
Kang, J. H. & Hong, S. W. Risk factors of frailty in patients with distal radius fractures. Geriatr. Orthop. Surg. Rehabil. 13, 21514593221094736 (2022).
Hong, S. W. & Kang, J. H. Relationship between skeletal bone mineral density and subjective masticatory difficulty. BMC Oral Health 22, 136 (2022).
Cichero, J.A.Y. Age-related changes to eating and swallowing impact frailty: Aspiration, choking risk, modified food texture and autonomy of choice. Geriatrics (Basel) 3(2018).
Gangloff, P., Louis, J. P. & Perrin, P. P. Dental occlusion modifies gaze and posture stabilization in human subjects. Neurosci. Lett. 293, 203–206 (2000).
Priebe, J., Wermers, R. A., Sems, S. A., Viozzi, C. F. & Koka, S. Relationship of number of missing teeth to hip fracture in elderly patients: A cohort pilot study. J. Prosthodont. 28, 258–263 (2019).
Wakai, K. et al. Tooth loss and risk of hip fracture: A prospective study of male Japanese dentists. Community Dent. Oral Epidemiol. 41, 48–54 (2013).
Ito, W. et al. Relationship between oral health and fractures in community-dwelling older Japanese adults. J. Am. Med. Dir. Assoc. 22, 1184–1189 (2021).
Yamamoto, T., et al. Dental status and incident falls among older Japanese: a prospective cohort study. BMJ Open 2(2012).
Kanis, J. A. et al. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int. 18, 1033–1046 (2007).
Kanis, J. A. et al. Case finding for the management of osteoporosis with FRAX–assessment and intervention thresholds for the UK. Osteoporos Int. 19, 1395–1408 (2008).
Executive summary of the clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Arch Intern. Med. 158, 1855–1867 (1998).
Kendler, D. L. et al. The official positions of the international society for clinical densitometry: Indications of use and reporting of DXA for body composition. J. Clin. Densitom. 16, 496–507 (2013).
Chun, M. Y. Validity and reliability of korean version of international physical activity questionnaire short form in the elderly. Korean J Fam Med 33, 144–151 (2012).
Moy, F. M. & Bulgiba, A. The modified NCEP ATP III criteria maybe better than the IDF criteria in diagnosing Metabolic Syndrome among Malays in Kuala Lumpur. BMC Public Health 10, 678 (2010).
Zimmet, P. Z., Alberti, K. G. & Shaw, J. E. Mainstreaming the metabolic syndrome: A definitive definition. Med. J. Aust. 183, 175–176 (2005).
Organization, W.H. World Health Organization: Oral Health Surveys: Basic Methods, (Geneva, 2013).
Organization, W.H. World Health Organization: Oral Health Surveys: Basic Methods, (World Health Organization, 1997).
Lee, K. M. et al. Factors associated with bone mineral density and risk of fall in Korean adults with type 2 diabetes mellitus aged 50 years and older. J. Clin. Endocrinol. Metab. 99, 4206–4213 (2014).
Kim, J.W.K., J-M.; Park, J. H.; Chang, J. S. Validation of FRAX without BMD: An age-related analysis of the Fifth Korean National Health and Nutrition Examination Survey (KNHANES V-1, 2010). Bone 75, 27–31 (2015).
Kang, K. Y., Kwok, S.-K., Ju, J. H., Hong, Y. S. & Park, S. H. Assessment of fracture risk in patients with axial spondyloarthritis: a case–control study using the fifth Korean National Health and Nutrition Examination Survey (KNHANES V). Scand. J. Rheumatol. 45, 23–31 (2016).
Siminoski, K. et al. Recommendations for bone mineral density reporting in Canada. Can. Assoc. Radiol. J. 56, 178–188 (2005).
Funding
This study was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (2020R1I1A1A01071537).
Author information
Authors and Affiliations
Contributions
Conception and design: S.W.H., J.H.K. Collection and assembly of clinical data: S.W.H., J.Y.L. Collection of experimental data: J.H.K. Data analysis: S.W.H., J.Y.L., J.H.K. Manuscript writing: S.W.H., J.H.K. Editing and final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declared no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hong, S.W., Lee, J. & Kang, JH. Associations between oral health status and risk of fractures in elder adults. Sci Rep 13, 1361 (2023). https://doi.org/10.1038/s41598-023-28650-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-28650-9
This article is cited by
-
The mediating effect of nutrition on oral frailty and fall risk in community-dwelling elderly people
BMC Geriatrics (2024)
-
Complex interplay of oral health, muscle and bone metabolism, and frailty in older individuals
Clinical Oral Investigations (2024)
-
Untreated osteoporosis and higher FRAX as risk factors for tooth loss: a 5-year prospective study
Journal of Bone and Mineral Metabolism (2023)
-
Association between dental diseases and oral hygiene care and the risk of vertebral fracture: a nationwide cohort study
Osteoporosis International (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.