Abstract
Early neonatal mortality occurs when a newborn dies within the first seven days of life. Despite interventions, neonatal mortality remains public health problem over time in Ethiopia (33 per 1000 live births). Determinants varies on level of neonatal mortality. The study's goal was to determine magnitude of early newborn death, as well as its determinants and causes in Newborn Intensive Care Unit of Referral hospital in Ethiopia's Somali region. Health facility based retrospective study review was conducted between May 2019 to May 2021 in Shiek Hassan Yabare Referral Hospital of Jigjiga University of Ethiopia. All neonates admitted at neonatal intensive care unit (NICU) with complete data and get registered using the new NICU registration book from May 2019 to May 2021 were included. Kobo toolkit was used for data collection and analyzed in SPSS 20. The magnitude of early neonatal mortality rate was defined as death between 0 and 7 days. Logistic regression model was used to estimate maternal and neonatal characteristics as a determinant variables on neonatal mortality. The statistical significance was considered at P-value < 0.05. The magnitude of early neonatal mortality rate of Ethiopia’s Somali region is estimated to be 130 per 1000 live births—that is say 130 newborn couldn’t celebrate their seventh day in every 1000 live births. Hypothermia, prematurity, maternal death at birth and shorter length of stay in NICU were increasing the chance of neonatal mortality at early stage while neonatal resuscitation had shown protective effect against neonatal mortality. Similarly birth asphyxia, preterm, sepsis, and congenital abnormalities were major causes of admission and death in the NICU. The magnitude of early neonatal mortality is considerable and most of the determinants are preventable. Enhancing quality of intra-partum and NICU care including infection prevention, managing hypothermia and neonatal resuscitation as per the national standard within the first golden hour is key.
Similar content being viewed by others
Introduction
Early neonatal mortality occurs when a newborn dies within the first seven days of life1.
Neonatal mortality continues to be the highest (17%) among children under the age of five worldwide, with Sub-Saharan Africa accounting for the largest share2. Low-income countries continue to have higher rates of neonatal death3,4.
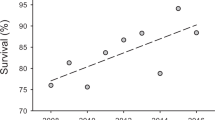
Despite interventions, newborn mortality remains public health problem in Ethiopia, it has come down from 49 to 30 and only now is 33 per 1000 live births5. However, a comprehensive study and meta-analysis found that early newborn mortality is reducing in Ethiopia, despite the high rate of early neonatal mortality (29.5 per 1000)6.
Furthermore, even newborns admitted to sub-Saharan nations' neonatal intensive care units (NICU)7,8,9,10, including Ethiopia, have a greater rate of early neonatal mortality. The causes of newborn mortality are numerous and vary depending on the situation. Prematurity and congenital anomalies1 and low APGAR score11 are the leading causes of early newborn mortality in the developed world, whereas very low birth weight9,12 sepsis13 and asphyxia7,9,10,12,14 are the leading causes in the low-income world, according to evidence from systematic reviews.
In low-income countries such as Ethiopia, early newborn mortality may also be caused by insufficient access to care7,15,16, home birth16, and issues with NICU care quality4,8.Prematurity-related problems and late breast-feeding initiation are also causes of infant death in low-income and resource-constrained countries7,13,14,17.
Furthermore, maternal illness and death, as well as a poor Apgar score, are two additional causes of neonatal mortality7,12,13,18. Maternal child spacing, on the other hand, protects against it6. Finally, duration of stay is another driver in Ethiopia, particularly in pastoralist communities, in addition to the other primary causes of newborn mortality in low-income countries like Ethiopia8,19.
The magnitude of early neonatal mortality in Ethiopia is poorly understood, and its determinants are varies in different context. The study's goal was to determine the magnitude of early newborn death, as well as its determinants and causes, in NICUs of health facilities in Ethiopia's Somali region.
Methods
All methods were carried out in accordance with relevant guidelines and regulations.
Study setting and period
Health facility based retrospective study review was conducted between May 2019 to May 2021 in Shiek Hassan Yabare Referral Hospital (SHYRH) of Jigjiga University, Ethiopia. SHYRH began delivering services in 2017 and it serves about 5 million people in Somali region of Ethiopia. The hospital has 400 beds and serves 86,000 outpatients annually. It is the largest hospital with a number of specialties including neonatal intensive care unit (NICU) in Somali region, Ethiopia. The number of average deliveries per month is 400.
Eligibility criteria
Neonates died or survived were reviewed among neonates admitted in NICU of SHYRH from May 2019 to May 2021. All neonates admitted at NICU and get registered using the new NICU registration book from May 2019 to May 2021 were included. Early neonatal death was considered a newborn death within the first week of life (between 0 to 7 days) while in NICU1. Live births were evaluated up to the 7th day after birth. Admitted neonates with incomplete data were excluded.
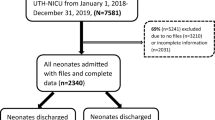
Sample size
Between April and May of 2021, an exhaustive review of the NICU registration book from May 2019 to May 2021 was conducted, with a total of 765 eligible neonates (99 deaths and 666 survivors) included in the study.
Data collection methods
The data was collected using checklist extracted from the new NICU registration book as it is comprehensive and filled properly. Two neonatal Nurse by profession have collected the data using Kobo toolbox software to prevent errors happen during data collection. Data collectors were sending the collected data per day to the server and getting on spot feedback from the supervisors.
The outcome variable of the study was early neonatal death at NICU of SHYRH while maternal and neonatal characteristics were as an independent variables. Mode of delivery, place of delivery, HIV test, Syphilis test, Hepatitis B test and maternal status were considered as maternal characteristics while sex, birth weight, temperature, APGAR score, length of stay, resuscitation, prematurity, sepsis, respiratory distress syndrome, Asphyxia, congenital malformation and Kangaroo mother care(KMC) were considered as neonatal characteristics.
Operational definition
The magnitude of early neonatal death is the proportion of neonatal death at hospital within the first 7 days of life among total live births admitted to the NICU.
Causes of neonatal mortality is any medical diagnosis that pediatricians noted after doing the required laboratory analysis and documented at patient chart as causes of neonatal death.
Kangaroo mother care (KMC) is a skin to skin contact between a mother and her newborn.
Birth weight is classified as low birth weight when it is less than 2500 g, and Overweight when it is ≥ 4000 g according to WHO.
Sepsis: any infection that was diagnosed based on clinically or laboratory investigation by health professionals in charge at NICU during the neonate's admission and is recorded on the patient chart.
Hypothermia: is any low body temperature measurement below 36.5 °C that was identified and documented on charts by physician during the admission of newborns at NICU.
Prematurity: Any live-born neonate who is delivered before 37 full weeks according to health professionals in charge at the NICU during admission of neonate and recorded at patient chart.
Birth asphyxia: when a newborn's Apgar score is below 6 in the fifth minute of life, or if the child don’t not cry right after birth, experienced respiratory difficulty, floppiness, loss of consciousness, the presence of convulsions, and loss of neonatal reflexes.
The Apgar score is a quick way for health professionals to evaluate the health of all newborns at 1 and 5 min after birth and in response to resuscitation.
Congenital malformations: structural or functional birth defects that occur during intrauterine life.
Data management and analysis
For data entry and collection, the Kobo toolkit was used. The data was cleaned with the Kobo toolkit before being analyzed with SPSS version 20. To find factors of early newborn death, researchers used bivariate and multivariable binary logistic regression. In multivariate analysis, variables having a P-value less than 0.2 in bivariate analysis, as well as other relevant determinants of early newborn mortality, were evaluated. In multivariate binary logistic regression analysis, factors having a P-value less than 0.05 were determined to have a significant relationship with the outcome variable. The odds ratio with 95 percent confidence interval was used to estimate the strength of the association. Stata version 16 with command of Prop 765 (size) 99 (outcome), exact (95% CI) was used to estimate the magnitude of early neonatal mortality rate.
Furthermore, to have a better knowledge of neonatal death, a frequency distribution table was employed to discover the causes of early neonatal mortality. The causes of neonatal death with highest proportions in the frequency distribution was reported as the top causes of neonatal mortality.
Ethical consideration
The study was ethically approved by ethical committee of college of medicine and health science of Jigjiga University, Ethiopia. Since data was collected from NICU registration book of SHYRH, an official consent was obtained from Hospital administration.
Results
Newborn characteristics at NICU
A total of eligible 765 neonates with complete data were reviewed and included in the study to estimate the rate of early neonatal mortality in Ethiopia's Somali region based on neonates admitted to the Shiek Hassen Referral Hospital's NICU. Among 765(between 0 and 7 days) reviewed, 99 died early and 666 survived. Higher proportion 41/99 (41.4%) of small babies (below 2000 g) died relative to 184/666 (27.6%) survived. similarly, 88/99 (88.9%) and 72/99 (72.7%) of the 99 neonates who died early were hypothermic and not resuscitated respectively. Regarding the first minute APGAR scores, mortality were higher among neonates with lower score 88/99 (88.9%) compared to those with higher score 11/99 (11.1%) which is expected.
Survival rate was lower among neonates admitted with premature 63/666 (9.5%), asphyxia 143/666 (21.5%) and congenital anomalies 65/666 (9.8%) compared to counterparts. Lastly, early neonatal mortality was lower 13/99 (13.1%) among neonates received KMC compared to those not received 86/99 (86.9%) (Table 1). In addition, to assess the level of KMC utilization of the study Hospital, cross tabulation of Hypothermia and KMC was done and the result shows that a total of 504 hypothermic neonates, only 64 (12.3%) have received KMC which is very low.
Magnitude of early neonatal mortality
The magnitude of early neonatal mortality rate of Ethiopia’s Somali region was estimated to be 130; 95% CI (106–154) per 1000 live births. That is 130 newborn couldn’t celebrate its sevens day in every 1000 live births. It was estimated from 765 live births admitted throughout the study period, with 99 deaths occurring during the first 7 days.
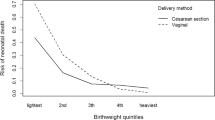
Maternal characteristics of neonates admitted to NICU of referral hospital
Many maternal characteristics were taken into account as determinants. Survival rate was lower among neonates born at home, by instrumental delivery and their mother died during childbirth relative to counterparts (Table 2).
Top causes of early neonatal mortality at NICU of Shiek Hassen referral hospital, Somali, Ethiopia.
Prenatal Asphyxia was the major cause of early neonatal mortality, followed by prematurity, with 32 (32.3%) and 31 (31.3%) deaths, respectively. Sepsis and congenital anomalies were the third and fourth causes of early neonatal mortality, respectively, 24 (24.2%) and 8 (8.1%) (Table 3).
Determinants of early neonatal mortality at NICU of Shiek Hassen Referral hospital
All newborn and maternal characteristics with a P-value less than 0.2 were considered in multivariable analysis. However; maternal mortality, preterm, newborn resuscitation, hyperthermia, and newborn shorter length of stay in NICU were revealed to be determinants of early neonatal mortality. When compared to those whose moms were alive, newborns whose mothers died during childbirth were considerably more likely to die early at neonatal age [adjusted odd ratio (AOR) 29.3; 95% CI 9.3, 92.1]. Similarly, the neonatal mortality were highest within the first 24 h after birth significantly AOR 72.5; 95% CI (6.3, 834.2) compared to deaths beyond the first 24 h till 7 days of live. Furthermore, compared to term born newborns and neonate with normal temperature, premature and hypothermic babies were almost four times more likely to die early at neonatal age (AOR 3.6; 95% CI (1.7, 8) and AOR 3.8; 95% CI (1.8, 8.1) respectively. Newborn resuscitation, on the other hand, has a protective effect and reduces early newborn death by 70% AOR 0.3; (0.2, 0.8) (Table 4).
Discussion
In present study, the magnitude of institutional early neonatal mortality rate was 130; 95% CI (106–154) per 1000 live births in a NICU of SHYRH of Jigjiga University in Ethiopia's Somali region. Maternal mortality, prematurity, newborn resuscitation, hypothermia, and newborn short duration (< 24 h) in NICU are the determinants of early neonatal mortality. The magnitude of early neonatal mortality rate of the current is very high and mainly defines the quality of obstetric and NICU care in the study facility. However, this has to be carefully interpreted as the neonatal death delivered in a facility, but who die outside the facility in the first 7 days of life is not captured and not included in the calculation of this death rate. The major causes of admission and death in the newborn Intensive Care Unit include birth asphyxia, prematurity, sepsis, and congenital abnormalities. This is in line with the findings of other investigations10,17,20,21.
The magnitude of early neonatal mortality rate of the current is very high and mainly defines the quality of obstetric and NICU care in the study facility. It is by far higher than a study in Afghanistan that showed 1.4 percent22, Northern Ethiopia (1.86%)23, Bukinafaso [2.6%]24, Nigeria (3.8%)25 and shaanxi province, China (7.9%)26. This might be due to different sample size and quality of obstetric and newborn care across context.
Prematurity was discovered to be a significant determinant of early newborn mortality. This is in line with the fact that preterm newborns have a greater mortality rate than term newborns27. Organ failure, neurodevelopmental and learning disabilities, vision problems, and long-term cardiovascular and non-communicable diseases are all risks for preterm babies28,29. The findings of this study are likewise consistent with those of Ethiopian and Sub-Saharan African studies7,8,10,18.
Another important determining factor that exhibited a protective effect against early neonatal mortality was neonatal resuscitation. This may be due to the fact that resuscitation is helping neonates with perinatal Asphyxia which is one of the top causes of neonatal mortality in the study setting. As studies in low income countries including systematic review suggested, appropriate help baby birth or resuscitation increases survival of first day of life but not all neonatal mortality30,31,32. This means in addition to resuscitation, other neonatal interventions are needed to prevent neonatal mortality30. It is also in line with findings of a Delphi panel of 18 experts, who indicated that urgent newborn facility-based resuscitation would avoid an additional 10% of preterm deaths, while community-based resuscitation would prevent an additional 20% of intrapartum-related and 5% of preterm fatalities33. Several other studies of neonatal resuscitation in low- and middle-income countries have shown that it has the potential to save newborn lives34,35,36.
Hypothermia (lower than normal body temperature) has also been linked to early newborn death. This is consistent with researches conducted in Ethiopia and elsewhere, which found that neonatal admission hypothermia dramatically increases the chance of death37,38. Hypothermia during NICU admission increased the risk of early newborn death, according to another study39,40. This could be linked to procedures such as delivering babies at < 25 °C (delivery room temperature), providing respiratory assistance with cold air during transfer to the NICU, and not using a cap on newborns, as well as unnecessary delays in skin-to-skin contact, preterm, and significant bacterial infection40,41,42.
Furthermore, the majority (442, or 87.7%) of hypothermic neonates admitted to the study hospital did not receive Kangroo mother care (KMC), which protects the newborn from infection, effectively treats hypothermia, improves gastrointestinal function and cardiorespiratory stability, and encourages breast feeding43 and thus reduces early neonatal mortality44,45.
The neonatal mortality were highest within the first 24 h after birth significantly AOR 72.5; 95% CI (6.3, 834.2) compared to deaths beyond 24 h. The risk of dying is highest in the first day of life in low income countries as systematic review on when do newborns die shows46. The finding is also consistent with researches that show majority of neonatal deaths occur in the first week of life, particularly in the first 24 h7,8,9,47,48. During the neonatal era, the risk of death is highest at the time of birth and gradually diminishes over the following days and weeks. Within the first 24 h of delivery, up to 36% of neonates die, and approximately 73% die within the first week of life49. Thus establishing NICU at Hospital is not enough but quality of care interventions given at birth and immediately after birth is very critical for neonatal survival50. This finding is also in line with research in Jimma of Ethiopia (< 7 days) and eastern Ethiopia (< 3 days) which found that shorter duration are associated with higher neonatal mortality10,51.
The other determinant of early newborn mortality discovered in this study was maternal death; newborns whose mothers died were more likely to die; the early post-natal period is a dangerous time for both mothers and their babies, and is strongly related to labor, intra-partum, and immediate new-born care practices. Studies have found a handful of maternal factors for early newborn death, such as hemorrhage and pregnancy-induced hypertension7,52,53,54,55,56. Furthermore, poor-quality care is responsible for 61% of neonatal deaths and half of maternal mortality50. This is because newborn care cannot be offered in isolation; it must be provided in conjunction with high-quality maternal care, which is also critical in saving lives. The health of mothers and their babies is intertwined, and providing appropriate interventions has the potential to save 71 percent of newborn fatalities, 33 percent of stillbirths, and 54 percent of maternal deaths if implemented fully57.
This study has the advantage of reviewing all newborns admitted to the hospital's NICU from 2019 to 2021, eliminating any potential sampling error. However, limitations of the study are related to the fact that facility-based studies do not reflect much of the neonatal deaths happening at community level and existence of poor-quality documentation for deaths.
Conclusion
The magnitude of early neonatal mortality at Neonatal Intensive Care Unit is very high and this magnitude is generalizable only to health facilities in setting. The determinants are maternal and neonatal related factors which are preventable. Maternal mortality, prematurity, newborn resuscitation, hypothermia are determining the early neonatal mortality in the study setting. In addition, the risk of newborn dying is higher in the first day of life after birth in NICU. Enhancing quality of obstetric and essential care for newborn babies as per the national standard including prevention of infection and hypothermia within the first golden hour is supper important of the Hospital.
Data availability
The dataset is available at supplementary S1 file. SPSS dataset.
Abbreviations
- NICU:
-
Neonatal intensive care unit
- RDS:
-
Respiratory Distress Syndrome
- CS:
-
Cesarean section
- KMC:
-
Kangaroo mother care
- LBW:
-
Low birth weight
- SHYRH:
-
Shiek Hassan Yabare Referral Hospital (SHYRH) of Jigjiga University
References
Lehtonen, L., Gimeno, A., Parra-Llorca, A., Vento, M. (eds) Early neonatal death: A challenge worldwide. In Seminars in Fetal and Neonatal Medicine (Elsevier, 2017).
UNICEF. United nations inter-agency group for child mortality estimation (UN IGME). Monit. Situat. Child. Women. 386, 2276–2286 (2019).
Armstrong, C. E., Magoma, M. & Ronsmans, C. Magnitude of maternal and neonatal mortality in Tanzania: A systematic review. Int. J. Gynecol. Obstet. 130(1), 98–110 (2015).
Gage, A. D., Fink, G., Ataguba, J. E. & Kruk, M. E. Hospital delivery and neonatal mortality in 37 countries in sub-Saharan Africa and South Asia: An ecological study. PLoS Med. 18(12), e1003843 (2021).
Mini, E., Demographic, E. Health Survey 2019: Key Indicators Report. (The DHS Program ICF, 2019).
Jena, B. H., Biks, G. A., Gelaye, K. A. & Gete, Y. K. Magnitude and trend of perinatal mortality and its relationship with inter-pregnancy interval in Ethiopia: A systematic review and meta-analysis. BMC Pregnancy Childbirth 20(1), 1–13 (2020).
Alebel, A. et al. Neonatal mortality in the neonatal intensive care unit of Debre Markos referral hospital, Northwest Ethiopia: A prospective cohort study. BMC Pediatr. 20(1), 1–11 (2020).
Elmi Farah, A., Abbas, A. H. & Tahir, A. A. Trends of admission and predictors of neonatal mortality: A hospital based retrospective cohort study in Somali region of Ethiopia. PLoS ONE 13(9), e0203314 (2018).
Roro, E. M., Tumtu, M. I. & Gebre, D. S. Predictors, causes, and trends of neonatal mortality at Nekemte Referral Hospital, east Wollega Zone, western Ethiopia (2010–2014). Retrospective cohort study. PLoS ONE 14(10), e0221513 (2019).
Seid, S. S. et al. Causes and factors associated with neonatal mortality in neonatal intensive care unit (NICU) of Jimma University medical center, Jimma, South West Ethiopia. Pediatr. Health Med. Ther. 10, 39 (2019).
Cnattingius, S., Johansson, S. & Razaz, N. Apgar score and risk of neonatal death among preterm infants. N. Engl. J. Med. 383(1), 49–57 (2020).
Eyeberu, A., Shore, H., Getachew, T., Atnafe, G. & Dheresa, M. Neonatal mortality among neonates admitted to NICU of Hiwot Fana specialized university hospital, eastern Ethiopia, 2020: A cross-sectional study design. BMC Pediatr. 21(1), 1–9 (2021).
Bitew, Z. W., Alemu, A., Ayele, E. G., Jember, D. A., Haile, M. T., Worku, T. Incidence density rate of neonatal mortality and predictors in Sub-Saharan Africa: A systematic review and meta-analysis. Int. J. Pediatr. 2020 (2020).
Girma, B. & Nigussie, J. Magnitude of preterm hospital neonatal mortality and associated factors in northern Ethiopia: A cross-sectional study. BMJ Open 11(12), e051161 (2021).
McKinnon, B., Harper, S., Kaufman, J. S. & Abdullah, M. Distance to emergency obstetric services and early neonatal mortality in Ethiopia. Trop. Med. Int. Health 19(7), 780–790 (2014).
Yaya, Y., Eide, K. T., Norheim, O. F. & Lindtjørn, B. Maternal and neonatal mortality in south-west Ethiopia: Estimates and socio-economic inequality. PLoS One 9(4), e96294 (2014).
Mersha, A., Bante, A. & Shibiru, S. Neonatal mortality and its determinates in public hospitals of Gamo and Gofa zones, southern Ethiopia: Prospective follow up study. BMC Pediatr. 19(1), 1–8 (2019).
Aynalem, Y. A., Mekonen, H., Akalu, T. Y., Gebremichael, B., Shiferaw, W. S. Preterm neonatal mortality and its predictors in Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia: A retrospective cohort study. Ethiopian J. Health Sci. 31(1) (2021).
Woday Tadesse, A., Mekuria Negussie, Y. & Aychiluhm, S. B. Neonatal mortality and its associated factors among neonates admitted at public hospitals, pastoral region, Ethiopia: A health facility based study. PLoS One 16(3), e0242481 (2021).
Chou, D., Daelmans, B., Jolivet, R. R., Kinney, M. & Say, L. Ending preventable maternal and newborn mortality and stillbirths the bmj. BMJ 351, 351 (2015).
Mitiku, H. D. Neonatal mortality and associated factors in Ethiopia: A cross-sectional population-based study. BMC Womens Health 21(1), 1–9 (2021).
Kibria, G. M. A. et al. Determinants of early neonatal mortality in Afghanistan: An analysis of the Demographic and Health Survey 2015. Glob. Health 14(1), 1–12 (2018).
Yirgu, R., Molla, M. & Sibley, L. Determinants of neonatal mortality in rural Northern Ethiopia: A population based nested case control study. PLoS ONE 12(4), e0172875 (2017).
Diallo, A., Meda, N., Ouedraogo, W., Cousens, S. & Tylleskar, T. A prospective study on neonatal mortality and its predictors in a rural area in Burkina Faso: Can MDG-4 be met by 2015?. J. Perinatol. 31(10), 656–663 (2011).
Akinyemi, J. O., Bamgboye, E. A. & Ayeni, O. Trends in neonatal mortality in Nigeria and effects of bio-demographic and maternal characteristics. BMC Pediatr. 15(1), 1–12 (2015).
Li, C., Yan, H., Zeng, L., Dibley, M. J. & Wang, D. Predictors for neonatal death in the rural areas of Shaanxi Province of Northwestern China: A cross-sectional study. BMC Public Health 15(1), 1–8 (2015).
Mengesha, H. G., Lerebo, W. T., Kidanemariam, A., Gebrezgiabher, G. & Berhane, Y. Pre-term and post-term births: Predictors and implications on neonatal mortality in Northern Ethiopia. BMC Nurs. 15(1), 1–11 (2016).
Behrman, R. E., Butler, A. S. Preterm Birth: Causes, Consequences, and Prevention. (2007).
Villar, J. et al. International standards for newborn weight, length, and head circumference by gestational age and sex: The Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 384(9946), 857–868 (2014).
Versantvoort, J. M. et al. Helping babies breathe and its effects on intrapartum-related stillbirths and neonatal mortality in low-resource settings: A systematic review. Arch. Dis. Child. 105(2), 127–133 (2020).
Weldearegay, H. G., Abrha, M. W., Hilawe, E. H., Gebrekidan, B. A. & Medhanyie, A. A. Quality of neonatal resuscitation in Ethiopia: Implications for the survival of neonates. BMC Pediatr. 20(1), 1–9 (2020).
Hadgu, F. B., Gebretsadik, L. G., Mihretu, H. G. & Berhe, A. H. Prevalence and factors associated with neonatal mortality at Ayder Comprehensive Specialized Hospital, Northern Ethiopia. A cross-sectional study. Pediatr. Health Med. Ther. 11, 29 (2020).
Lee, A. C. et al. Neonatal resuscitation and immediate newborn assessment and stimulation for the prevention of neonatal deaths: A systematic review, meta-analysis and Delphi estimation of mortality effect. BMC Public Health 11(3), 1–19 (2011).
Newton, O. & English, M. Newborn resuscitation: Defining best practice for low-income settings. Trans. R. Soc. Trop. Med. Hyg. 100(10), 899–908 (2006).
Singhal, N. & Niermeyer, S. Neonatal resuscitation where resources are limited. Clin. Perinatol. 33(1), 219–228 (2006).
Wall, S. N. et al. Neonatal resuscitation in low-resource settings: What, who, and how to overcome challenges to scale up?. Int. J. Gynecol. Obstet. 107, S47–S64 (2009).
Ibrahim, A. M., Farah, A. M., Osman, M. O. & Hashi, A. The effect of admission hypothermia for neonatal death among neonates admitted to neonatal intensive care unit at Sheik Hassan Yabare Jigjiga University Referral Hospital in Jigjiga City, Somali Region, Eastern Ethiopia. Res. Rep. Neonatol. 11, 43–55 (2021).
McManus, I., Dewberry, C., Nicholson, S. & Dowell, J. S. The UKCAT-12 study: Educational attainment, aptitude test performance, demographic and socio-economic contextual factors as predictors of first year outcome in a cross-sectional collaborative study of 12 UK medical schools. BMC Med. 11(1), 1–25 (2013).
Chou, D., Daelmans, B., Jolivet, R. R., Kinney, M. & Say, L. Ending preventable maternal and newborn mortality and stillbirths. BMJ 351, h4255 (2015).
de Almeida, M. F. B. et al. Hypothermia and early neonatal mortality in preterm infants. J. Pediatr. 164(2), 271–275 (2014).
Organization WH, Health WHOR, Health WHODoR. Pregnancy, Childbirth, Postpartum, and Newborn Care: A Guide for Essential Practice (World Health Organization, 2003).
Yitayew, Y. A., Aitaye, E. B., Lechissa, H. W., Gebeyehu, L. O. Neonatal hypothermia and associated factors among newborns admitted in the neonatal intensive care unit of Dessie Referral Hospital, Amhara Region, Northeast Ethiopia. Int. J. Pediatr. 2020 (2020).
Organization, W. H. World Report on Ageing and Health (World Health Organization, 2015).
Lawn, J. E., Mwansa-Kambafwile, J., Horta, B. L., Barros, F. C. & Cousens, S. ‘Kangaroo mother care’ to prevent neonatal deaths due to preterm birth complications. Int. J. Epidemiol. 39(suppl 1), i144–i154 (2010).
Yismaw, A. E. & Tarekegn, A. A. Proportion and factors of death among preterm neonates admitted in University of Gondar comprehensive specialized hospital neonatal intensive care unit, Northwest Ethiopia. BMC Res. Notes. 11(1), 1–7 (2018).
Sankar, M. J. et al. When do newborns die? A systematic review of timing of overall and cause-specific neonatal deaths in developing countries. J. Perinatol. 36(1), S1-1 (2016).
Mekonnen, Y., Tensou, B., Telake, D. S., Degefie, T. & Bekele, A. Neonatal mortality in Ethiopia: Trends and determinants. BMC Public Health 13(1), 1–14 (2013).
Worku, B., Kassie, A., Mekasha, A., Tilahun, B. & Worku, A. Predictors of early neonatal mortality at a neonatal intensive care unit of a specialized referral teaching hospital in Ethiopia. Ethiop. J. Health Dev. 26(3), 200–207 (2012).
Oza, S., Cousens, S. N. & Lawn, J. E. Estimation of daily risk of neonatal death, including the day of birth, in 186 countries in 2013: A vital-registration and modelling-based study. Lancet Glob. Health 2(11), e635–e644 (2014).
Kruk, M. E. et al. High-quality health systems in the sustainable development goals era: Time for a revolution. Lancet Glob. Health 6(11), e1196–e1252 (2018).
Desalew, A. et al. Cause and predictors of neonatal mortality among neonates admitted to neonatal intensive care units of public hospitals in eastern Ethiopia: A facility-based prospective follow-up study. BMC Pediatr. 20(1), 1–11 (2020).
Ananth, C. V. & Basso, O. Impact of pregnancy-induced hypertension on stillbirth and neonatal mortality in first and higher order births: A population-based study. Epidemiology 21(1), 118 (2010).
Berhe, A. K., Ilesanmi, A. O., Aimakhu, C. O. & Mulugeta, A. Effect of pregnancy induced hypertension on adverse perinatal outcomes in Tigray regional state, Ethiopia: A prospective cohort study. BMC Pregnancy Childbirth 20(1), 1–11 (2020).
Endeshaw, G. & Berhan, Y. Perinatal outcome in women with hypertensive disorders of pregnancy: A retrospective cohort study. Int. Sch. Res. Notices. 2015, 1–8 (2015).
van Esch, J. J., van Heijst, A. F., de Haan, A. F. & van der Heijden, O. W. Early-onset preeclampsia is associated with perinatal mortality and severe neonatal morbidity. J. Matern. Fetal Neonatal Med. 30(23), 2789–2794 (2017).
Vogel, J. P. et al. Maternal complications and perinatal mortality: findings of the World Health Organization Multicountry Survey on Maternal and Newborn Health. BJOG Int. J. Obstet. Gynaecol. 121, 76–88 (2014).
Bhutta, Z. et al. Lancet Newborn Interventions Review Group; Lancet Every Newborn Study Group. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost. Lancet 384(9940), 347–370 (2014).
Acknowledgements
We appreciate the assistance of SHYR Hospital officials and NICU nurses throughout data collecting. We also appreciate the help of data collectors, supervisors, and Jigjiga University during data collecting.
Author information
Authors and Affiliations
Contributions
Conceptualization: A.T.A., A.E.F., H.N.A. Data curation: A.T.A., A.E.F. Formal analysis: A.T.A., A.E.F. Methodology: A.T.A. Supervision: A.T.A., H.N.A., M.O.I. Writing—original draft: A.T.A., A.E.F. Writing—review and editing: A.T.A., A.E.F., H.N.A., M.O.I. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahmed, A.T., Farah, A.E., Ali, H.N. et al. Determinants of early neonatal mortality (hospital based retrospective cohort study in Somali region of Ethiopia). Sci Rep 13, 1114 (2023). https://doi.org/10.1038/s41598-023-28357-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-28357-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.