Abstract
Adenosine occasionally overestimates fractional flow reserve (FFR) values (i.e., insufficient adenosine-induced hyperemia), leading to low non-hyperemic pressure ratios (NHPR)–high FFR discordance. We investigated the impact of insufficient adenosine-induced hyperemia on NHPR–FFR discordance and the reclassification of functional significance. We measured resting distal-to-aortic pressure ratio (Pd/Pa) and FFR by using adenosine (FFRADN) and papaverine (FFRPAP) in 326 patients (326 vessels). FFRADN overestimation was calculated as FFRADN − FFRPAP. We explored determinants of low Pd/Pa − high FFRADN discordance (Pd/Pa ≤ 0.92 and FFRADN > 0.80) versus high Pd/Pa − low FFRADN discordance (Pd/Pa > 0.92 and FFRADN ≤ 0.80). Reclassification of functional significance was defined as FFRADN > 0.80 and FFRPAP ≤ 0.80. Multivariable analysis identified FFRADN overestimation (p = 0.002) and heart rate at baseline (p = 0.048) as independent determinants of the low Pd/Pa–high FFRADN discordance. In the low Pd/Pa–high FFRADN group (n = 26), papaverine produced a further decline in the FFR value in 21 vessels (81%) compared with FFRADN, and the reclassification was observed in 17 vessels (65%). Insufficient adenosine-induced hyperemia is a major determinant of the low resting Pd/Pa–high FFR discordance. Physicians should bear in mind that the presence of low NHPR–high FFR discordance may indicate a false-negative FFR result.
Similar content being viewed by others
Introduction
Measuring fractional flow reserve (FFR) has been a standard method for guiding coronary revascularization in chronic coronary syndrome1,2,3,4. To simplify physiological assessment procedures, non-hyperemic pressure ratios (NHPRs) without the need for a vasodilator were introduced5. Resting distal-to-aortic pressure ratio (Pd/Pa) during the entire cardiac cycle is available with the use of any pressure-monitoring system, providing a universal resting physiological metric. Although recent clinical guidelines recommend NHPRs as well as FFR for the selection of revascularization strategies6,7,8, one-fifth of cases demonstrate discordance of the physiological significance between NHPRs and FFR9,10,11,12,13. Since the principle of FFR is based on maximal hyperemia3,14, insufficient hyperemia (i.e. an overestimation of FFR) is a potential cause of discordance with a low NHPR and a high FFR5.
It has been demonstrated that intravenous adenosine, the vasodilator that is most commonly used for hyperemia induction1,2,3,4,14, occasionally fails to induce maximal hyperemia compared to other hyperemic stimuli, such as papaverine15,16,17,18. If low NHPR–high FFR discordance is associated with insufficient adenosine-induced hyperemia, vessels that have low NHPR–high FFR discordance may show positive FFR results when another stimulus is used, providing a false-negative result based on an adenosine-induced FFR. Conversely, high NHPR–low FFR discordance may indicate sufficient adenosine-induced hyperemia. The impact of insufficient adenosine-induced hyperemia on NHPR–FFR discordance has not been investigated. Earlier studies used only adenosine for hyperemia induction, thereby precluding an assessment of adenosine’s role in NHPR–FFR discordance19,20,21,22.
Adenosine produces hyperemia through adenosine A2a receptors in vascular smooth muscles4, whereas papaverine induces maximal hyperemia most reliably by causing a direct relaxation of the vascular smooth muscle23. In our present investigation, patients’ FFR values were measured using adenosine (FFRADN) and papaverine (FFRPAP). FFRPAP was used as a reference standard of functional significance. We sought to determine the impact of insufficient adenosine-induced hyperemia on resting Pd/Pa–FFRADN discordance and the reclassification of functional significance.
Methods
Study patients
This retrospective study included 365 patients with chronic coronary syndrome who underwent an FFR assessment for standard clinical indications. If a patient required FFR assessments for two or more vessels, only the first vessel was included in this study. All of the patients were asked to abstain from food and beverages for > 3 h before the catheterization. More prolonged caffeine abstinence was left to the physician’s discretion. The exclusion criteria consisted of any contraindications for adenosine or papaverine, patients with severe arrhythmia (e.g., frequent ectopic beats or atrial fibrillation), the presence of significant valvular disease, an ostial lesion, a prior coronary artery bypass graft, and the use of a theophylline-containing medication. Patients with insufficient pressure data quality, including a signal drift value of more than ± 0.03 after the pullback of the pressure wire and inadequate waveform tracings, were also excluded.
The coronary physiology assessment was performed as part of the routine diagnostic coronary angiography procedures for clinical purposes. All methods were performed in accordance with the relevant guidelines and regulations. Written informed consent for the invasive physiology assessment was obtained from all of the patients before the procedure. The Institutional Review Board approved this retrospective study (reference #3234/ Showa University School of Medicine; 31 August, 2021) and waived the requirement of patient approval for the use of patient data and medical records for research.
Coronary physiologic measurements
Coronary angiography was performed in a standard manner for each patient. Intracoronary isosorbide dinitrate (2 mg) was administered before the physiological assessments. With the use of a coronary-pressure guidewire (Philips Volcano or Abbott Vascular) and a 5- or 6-F guiding catheter without side holes, the distal coronary pressure (Pd) and the aortic pressure (Pa) were obtained simultaneously. The patient’s resting Pd/Pa ratio was recorded after his/her full recovery from the influence of contrast media, isosorbide dinitrate, or saline flush.
Adenosine was administered continuously via a femoral vein or a large forearm vein at 140 μg/kg/min for > 150 s3,4,14,24. In cases in which steady-state hyperemia was not achieved during the adenosine infusion, the infusion was continued for a minimum of 180 s. Papaverine was used as the last agent to obtain a reliable pull-back curve, as it induces hyperemia with minimal variations in Pd/Pa25. After confirming that Pd/Pa values had returned to the baseline level, with an interval of ≥ 5 min after the termination of adenosine infusion, intracoronary papaverine (8–10 mg in the right coronary artery or 12–15 mg in the left coronary artery) was given through the coronary catheter, followed by 5 mL of saline14,26. Approximately 20 s after the papaverine injection, an FFR pullback recording was performed manually, and the presence of pressure-wire drift was checked.
Data analysis
Resting Pd/Pa and FFR
Experienced observers blinded to the patients’ coronary angiography results and clinical data manually reviewed the pressure recordings. Pressure waveforms from ectopic beats and the adjacent beats were not included in the analysis. Resting Pd/Pa ratio was calculated as the mean Pd to the mean Pa, and ≤ 0.92 was regarded as a positive ratio5,11. FFRADN was measured during the steady-state hyperemic plateau phase > 60 s after the initiation of the adenosine infusion and > 15 s after the transition to hyperemia18,27. The lowest Pd/Pa values on a beat-to-beat basis for adenosine and papaverine were regarded as FFRADN and FFRPAP, respectively15,16,17,18,28, and ≤ 0.80 was used as the cut-off for FFRADN and FFRPAP1,2,3,29. The difference in FFR values between adenosine and papaverine was calculated as FFRADN − FFRPAP18. The reclassification of functional significance was defined as FFRADN > 0.80 and FFRPAP ≤ 0.80 (false-negative by adenosine), and reverse reclassification was defined as FFRADN ≤ 0.80 and FFRPAP > 0.80 (false-positive by adenosine). Based on the FFR pull-back curve, the physiological pattern of disease was classified as focal, diffuse, or a combination of both (mixed) by the consensus of experienced observers30.
We classified the enrolled vessels into four groups according to their resting Pd/Pa and FFRADN values: (i) high resting Pd/Pa–high FFRADN (resting Pd/Pa > 0.92 and FFRADN > 0.80), (ii) high resting Pd/Pa–low FFRADN (resting Pd/Pa > 0.92 and FFRADN ≤ 0.80), (iii) low resting Pd/Pa–high FFRADN (resting Pd/Pa ≤ 0.92 and FFRADN > 0.80), and (iv) low resting Pd/Pa–low FFRADN (resting Pd/Pa ≤ 0.92 and FFRADN ≤ 0.80). We evaluated the clinical and pathophysiological characteristics between the vessels with low resting Pd/Pa–high FFRADN discordance and the vessels with high Pd/Pa–low FFRADN discordance, based on a study of NHPR–FFR discordance22.
Coronary angiography
Quantitative coronary angiography was performed in optimal projections with a commercially available system (CAAS Workstation version 7.5, Pie Medical Imaging) by independent investigators blinded to the physiological results and clinical data. The reference diameter, minimum lumen diameter, and lesion length were measured by using the external diameter of the catheter as a scaling device, and the diameter stenosis was calculated.
Statistical analysis
Continuous variables were presented as medians with interquartile ranges (IQRs). Categorical variables were presented as numbers and proportions. Comparisons between adenosine and papaverine were done with the Wilcoxon signed-rank test for quantitative variables and with the McNemar test for categorical variables. Correlations between two variables were assessed with Spearman’s rank correlation coefficient. Between-group comparisons were made with the unpaired-samples t-test or the Mann–Whitney U-test for quantitative variables and with the χ2 test or Fisher’s exact test for categorical variables, as appropriate. Multivariable logistic regression analysis was performed to determine factors associated with the low resting Pd/Pa–high FFR discordance versus the high resting Pd/Pa–low FFR discordance. Clinical, angiographic, and hemodynamic parameters with a univariable association of p < 0.10 and FFRADN − FFRPAP were included in the multivariable model. The results were presented as the odds ratio and 95% confidence interval. Statistical analyses were performed using JMP® Pro, ver. 16.0.0 (SAS, Cary, NC). A p-value < 0.05 was considered significant.
Results
Procedures
Among the 365 vessels in the 365 patients, 39 were eliminated from the analysis because of difficulty in advancing the pressure wire far distal to the index lesion (n = 6), side effects from adenosine (n = 8) or papaverine (n = 2), sensor drift (n = 13), or insufficient waveform tracings (n = 10). A final total of 326 vessels were included in the study. The patient and lesion characteristics are summarized in Table 1.
Resting Pd/Pa and FFR
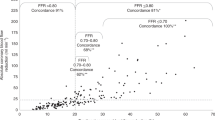
The median resting Pd/Pa was 0.93 (IQR 0.88–0.96); the median FFRADN was 0.79 (IQR 0.73–0.86), and the median FFRPAP was 0.77 (IQR 0.70–0.84). Figure 1 is a scatterplot of resting Pd/Pa and FFRADN values: there was a moderate correlation between these two indices (ρ = 0.756, p < 0.001).
Scatter plot of resting Pd/Pa and FFRADN. The vessels were classified into four groups by using the predefined cut-off values of 0.92 for resting Pd/Pa and 0.80 for FFRADN. Among 326 vessels, 68 (21%) demonstrated discordance: low resting Pd/Pa–high FFRADN in 26 vessels (8%) and high Pd/Pa–low FFRADN in 42 vessels (13%). FFRADN fractional flow reserve value associated with adenosine, Pd/Pa distal-to-aortic pressure ratio.
Using the predefined cutoff values of resting Pd/Pa and FFRADN, we observed that 258 vessels (79%) had concordant results, which consisted of the low resting Pd/Pa–low FFR in 133 vessels (41%) and the high resting Pd/Pa–high FFR in the other 125 (38%). The remaining 68 vessels (21%) demonstrated discordant results and were comprised of 26 vessels (8%) with the low resting Pd/Pa–high FFRADN and 42 vessels (13%) with the high Pd/Pa–low FFRADN.
Figure 2 compares FFRADN and FFRPAP values. As shown in a scatterplot (Fig. 2A), FFRADN and FFRPAP values were highly correlated (ρ = 0.926, p < 0.001). Bland–Altman analysis (Fig. 2B) revealed a significant bias toward the overestimation of FFR by adenosine (p < 0.001), with the mean difference of 0.02 and the 95% limits of agreements of −0.05 and 0.10.
Comparison of FFRADN and FFRPAP. (A) Scatter plot. FFRADN and FFRPAP were highly correlated (ρ = 0.926, p < 0.001). FFRADN fractional flow reserve value associated with adenosine, FFRPAP fractional flow reserve value associated with papaverine. (B) Bland–Altman plot. There was a positive bias towards the overestimation of FFR by adenosine (p < 0.001), with the mean difference of 0.02 and the 95% limits of agreements of − 0.05 and 0.10.
Comparison of the two discordant groups
Table 2 summarizes the patient and lesion characteristics in the low Pd/Pa–high FFRADN and high Pd/Pa–low FFRADN groups. Diabetes mellitus was significantly more frequent in the low Pd/Pa–high FFRADN group compared to the high Pd/Pa–low FFRADN group: 50% (13/26) vs. 26% (11/42), p = 0.046. The low Pd/Pa–high FFRADN group tended to receive hemodialysis more frequently: 6% (4/26) vs. 2% (1/42), p = 0.067. The LAD location, the quantitative coronary angiography parameters, and the physiological pattern did not differ between the two groups. Heart rate at baseline was significantly higher in the low Pd/Pa–high FFRADN group compared to the high Pd/Pa–low FFRADN group: 73 (IQR 61–81) vs. 62 (IQR 57–71), p = 0.008.
In both of the discordance groups, adenosine resulted in higher FFR values compared to papaverine: 0.79 (IQR 0.76–0.82) vs. 0.77 (IQR 0.72–0.79), p < 0.001 for all; 0.82 (IQR 0.81–0.84) vs. 0.79 (IQR 0.74–0.81), p < 0.001 for the low Pd/Pa–high FFRADN group; and 0.77 (IQR 0.74–0.79) vs. 0.75 (IQR 0.72–0.78), p = 0.002 for the high Pd/Pa–low FFRADN group. Figure 3 demonstrates the groups’ distributions of FFRADN − FFRPAP. FFRADN − FFRPAP was significantly greater in the low Pd/Pa–high FFRADN group compared to the high Pd/Pa–low FFRADN group: 0.04 (IQR 0.01–0.09) vs. 0.01 (IQR 0–0.03), p = 0.004. FFRADN − FFRPAP ≥ 0.05 was significantly more frequently observed in the low Pd/Pa–high FFRADN group compared to the high Pd/Pa–low FFRADN group: 46% (12/26) vs. 7% (3/42), p < 0.001.
Comparison of FFRADN overestimation between low Pd/Pa–high FFRADN and high Pd/Pa–low FFRADN groups. Distributions of FFRADN overestimation with box-and-whisker plots are shown. FFRADN overestimation was defined as FFRADN– FFRPAP. FFRADN fractional flow reserve value associated with adenosine, FFRPAP fractional flow reserve value associated with papaverine, Pd/Pa distal-to-aortic pressure ratio.
Factors associated with the low resting Pd/Pa–high FFRADN discordance
Based on the results of the univariable analysis (Table 3A), we entered FFRADN − FFRPAP (p = 0.002), diabetes mellitus (p = 0.049), hemodialysis (p = 0.080), and heart rate at baseline (p = 0.008) into the multivariable model. The multivariable logistic regression analysis identified FFRADN − FFRPAP (odds ratio 1.34 per 0.01 increase, 95% confidence interval: 1.14–1.68, p = 0.002) and heart rate at baseline (odds ratio 1.07 per 1 beat/min increase, 95% confidence interval: 1.00–1.13, p = 0.048) as independent factors associated with the low resting Pd/Pa–high FFRADN discordance (Table 3B).
Reclassification of functional significance by papaverine
Figure 4 depicts individual patients’ resting Pd/Pa, FFRADN, and FFRPAP values. In the low Pd/Pa–high FFRADN group (Fig. 4A), papaverine produced a further decline in the FFR value in 21 vessels (81%) compared with the FFRADN value. Of the 26 vessels with the low Pd/Pa–high FFRADN discordance, the reclassification of functional significance by papaverine (FFRADN > 0.80 and FFRPAP ≤ 0.80) was observed in 17 vessels (65%). Of these, 11 vessels showed FFRADN − FFRPAP ≥ 0.05, and 8 had an FFRPAP value below the gray zone (≤ 0.75).
Individual resting Pd/Pa, FFRADN, and FFRPAP values in the low Pd/Pa − high FFRADN and high Pd/Pa − low FFRADN groups. (A) Low Pd/Pa − high FFRADN group (resting Pd/Pa > 0.92 and FFRADN ≤ 0.80). (B) High Pd/Pa − low FFRADN group (resting Pd/Pa ≤ 0.92 and FFRADN > 0.80). FFRADN fractional flow reserve value associated with adenosine, FFRPAP fractional flow reserve value associated with papaverine, IQR interquartile range, Pd/Pa distal-to-aortic pressure ratio.
Among the 42 vessels with the high Pd/Pa–low FFRADN discordance (Fig. 4B), reverse reclassification (FFRADN ≤ 0.80 and FFRPAP > 0.80) was observed in only 7% (3/42) of the cases. All of the cases with reverse reclassification had a borderline FFRADN value (0.78–0.80), with a small difference from the FFRPAP value (≤ 0.03).
Discussion
Our evaluation of resting Pd/Pa and FFR measured using adenosine and papaverine revealed the following: (1) the overestimation of FFR by adenosine (i.e., insufficient adenosine-induced hyperemia) was the strongest determinant of the low Pd/Pa–high FFRADN discordance, and (2) in two-thirds of the vessels with low Pd/Pa–high FFRADN discordance, functional significance was reclassified from a negative result by adenosine (FFRADN > 0.80) to a positive result by papaverine (FFRPAP ≤ 0.80). This study is first to demonstrate that insufficient adenosine-induced hyperemia is a major determinant of NHPR–FFR discordance and to clarify its influence on the reclassification of functional significance.
Determinants of low NHPR–high FFR discordance
Due to the differences in physiologic backgrounds between resting and hyperemic conditions, the discordance between NHPR and FFR is not surprising. Coronary flow characteristics and/or microvascular resistance were demonstrated to be associated with NHPR–FFR discordance20,21. In vessels with preserved microvascular function (i.e., high coronary flow reserve and low microcirculatory resistance), increased coronary flow during hyperemia produces a greater pressure gradient across stenosis compared to vessels with microvascular dysfunction, leading to high NHPR–low FFR discordance. Conversely, in the presence of impaired microvascular function (i.e., low coronary flow reserve and high microcirculatory resistance), the trans-stenotic pressure gradient during hyperemia is less evident than in vessels with preserved microvascular function, leading to low NHPR–high FFR discordance.
Interestingly, we observed large overestimations of FFR by adenosine (≥ 0.05, which exceeds 2 standard deviations between repeated FFRADN measurements)27 in as many as 42% of the vessels with low Pd/Pa–high FFRADN discordance, but in only 7% of vessels with high Pd/Pa–low FFRADN discordance. This result suggests that the standard 140 μg/kg/min dose of intravenous adenosine may not be sufficient to induce maximal hyperemia in the presence of microvascular dysfunction. The microvascular dysfunction in vessels with low NHPR–high FFR discordance described in previous studies might be attributable in part to submaximal adenosine-induced hyperemia. Further research is necessary to address this possibility.
Insufficient adenosine-induced hyperemia due to caffeine remaining in the blood could also account for the low Pd/Pa–high FFRADN discordance. Caffeine competitively antagonizes adenosine by blocking adenosine A2a receptor activity31. In the presence of serum caffeine, adenosine overestimated FFR in a linear concentration–response manner, compared with papaverine without involving the adenosine receptors18. Despite the lack of systematic pre-procedure caffeine abstinence in our present study population, the patient series reflected real-world clinical situations. Matsumoto et al. reported the associations of the duration of caffeine abstinence with serum caffeine level and FFRADN − FFRPAP17. Even after caffeine abstinence for 12–24 h, as recommended by non-invasive imaging guidelines32,33, serum caffeine was still detectable in most patients17. The mean difference between FFRADN and FFRPAP (0.02) observed in the present study is similar to that after caffeine abstinence for 12–24 h17. More prolonged caffeine avoidance for > 48 h was shown to achieve zero serum caffeine levels in most cases and to result in comparable FFR values between adenosine and papaverine17; however, such strict caffeine control for all patients undergoing invasive angiography is impractical in routine care. Consequently, the frequency of low Pd/Pa–high FFRADN discordance in the present investigation was consistent with that of the low NHPR–high FFRADN discordance in earlier investigations that used adenosine or adenosine triphosphate11,19,20,21,22. Although it is unclear whether the patients abstained from caffeine in the prior studies11,19,20,21,22, caffeine antagonism might have contributed, in part, to their low NHPR–high FFRADN discordance.
Our analyses also identified the patient’s heart rate at baseline as an independent determinant of low Pd/Pa–high FFRADN discordance. This result is reasonable from a physiological point of view. The resting coronary flow increases with a higher heart rate, producing a larger resting pressure gradient34.
Reclassification of functional significance
Although there is no doubt regarding the revascularization of lesions with both a low NHPR and a low FFR, it remains unclear whether or not lesions with NHPR–FFR discordance should be revascularized. Lee et al. reported that major adverse cardiovascular events were increased only when both NHPR and FFR were positive35. Notably, in two-thirds of the present cases of low Pd/Pa–high FFRADN discordance, the physiological significance was reclassified from a negative result by adenosine to a positive result by papaverine; that is, false-negative FFR results were provided by adenosine. In addition, two-thirds of these false-negative adenosine-induced FFR results were attributed to a large overestimation of FFR by adenosine, i.e., ≥ 0.05. Patients with false-negative results that are due specifically to large overestimations of FFR miss the opportunity to receive benefits from revascularization, which may lead to adverse outcomes. Other investigations have indicated that when the patients are treated with medical therapy alone, their FFR values, even around the cut-off value, demonstrated a continuous relationship with subsequent adverse coronary events36,37.
Based on landmark FFR studies (DEFER, FAME I, and FAME II) in which mainly intravenous adenosine was used for hyperemia induction1,2,38, the rate of major adverse cardiac events in deferred lesions was considered to be approximately 1% per year3. In a recent large-scale prospective observational trial (the J-CONFIRM registry), major adverse cardiac events occurred less frequently, in as few as 0.4% of deferred lesions39. Although none of the reports of these trials provided information on serum caffeine levels or the length of caffeine abstinence, the lower incidence of major adverse cardiac events in the J-CONFIRM trial might have occurred in part because hyperemic stimuli other than adenosine (e.g., papaverine or nicorandil) that do not involve the adenosine receptors were used in more than half of their study patients39. Further investigation is necessary to confirm the prognostic values of papaverine- and nicorandil-induced FFR.
Insufficient adenosine-induced hyperemia and/or reclassification of functional significance will not be identified unless another hyperemic stimulus is used. Given the present high incidence (two-thirds) of false-negative FFRADN results, low NHPR–high FFRADN discordance mismatch may alert operators to insufficient adenosine-induced hyperemia. In the presence of low NHPR–high FFRADN discordance, the use of other hyperemic stimuli that do not involve the adenosine A2a receptors (e.g., papaverine and nicorandil) should be considered to avoid misinterpretations of physiological significance.
Instead of wire-derived physiological indices, wire-free angiography-derived computational indices of FFR, such as quantitative flow ratio, have been introduced40. Quantitative flow ratio was also reported to show discordance with FFR41. Considering that both NHPRs and quantitative flow ratio are measured under non-hyperemic conditions, insufficient hyperemia would cause low quantitative flow ratio–high FFR discordance. In other words, all non-hyperemic physiological indices may provide a clue about insufficient hyperemia.
Study limitations
Several limitations should be acknowledged. First, the number of cases of low Pd/Pa–high FFRADN discordance was relatively small. Second, the prognostic relevance of low Pd/Pa–high FFRADN discordance and/or reclassification could not be identified in this study, because some of the vessels with low Pd/Pa–high FFRADN discordance were revascularized based on positive FFRPAP (≤ 0.80) results. Further research is warranted to address whether NHPR–FFR discordance due to insufficient adenosine-induced hyperemia is associated with adverse outcomes. Third, microvascular function was not assessed. Microcirculatory resistance cannot be accurately evaluated by adenosine in the presence of insufficient adenosine-induced hyperemia. Lastly, the order of hyperemic agents was fixed (papaverine last) because papaverine was used to obtain a reliable pullback curve. Although papaverine was administered after confirming that Pd/Pa values had returned to the baseline level, adenosine’s carry-over effect cannot be excluded.
Conclusions
Insufficient adenosine-induced hyperemia is a major determinant of the low resting Pd/Pa–high FFR discordance. Physicians should bear in mind that the presence of a low non-hyperemic pressure ratio but a high adenosine-induced FFR may indicate a false-negative FFR result.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- FFR:
-
Fractional flow reserve
- FFRADN :
-
Fractional flow reserve value associated with adenosine
- FFRPAP :
-
Fractional flow reserve value associated with papaverine
- IQR:
-
Interquartile range
- LAD:
-
Left anterior descending coronary artery
- NHPR:
-
Non-hyperemic pressure ratio
- Pa:
-
Aortic pressure
- Pd:
-
Distal coronary pressure
- Pd/Pa:
-
Distal-to-aortic pressure ratio
References
Tonino, P. A. et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N. Engl. J. Med. 360, 213–224. https://doi.org/10.1056/NEJMoa0807611 (2009).
De Bruyne, B. et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N. Engl. J. Med. 367, 991–1001. https://doi.org/10.1056/NEJMoa1205361 (2012).
Pijls, N. H., Tanaka, N. & Fearon, W. F. Functional assessment of coronary stenoses: Can we live without it?. Eur. Heart J. 34, 1335–1344. https://doi.org/10.1093/eurheartj/ehs436 (2013).
Layland, J., Carrick, D., Lee, M., Oldroyd, K. & Berry, C. Adenosine: Physiology, pharmacology, and clinical applications. JACC Cardiovasc. Interv. 7, 581–591. https://doi.org/10.1016/j.jcin.2014.02.009 (2014).
van de Hoef, T. P. et al. Non-hyperaemic coronary pressure measurements to guide coronary interventions. Nat. Rev. Cardiol. https://doi.org/10.1038/s41569-020-0374-z (2020).
Patel, M. R. et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 Appropriate Use Criteria for Coronary Revascularization in Patients With Stable Ischemic Heart Disease: A Report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J. Am. Coll. Cardiol. 69, 2212–2241. https://doi.org/10.1016/j.jacc.2017.02.001 (2017).
Correction. J. Am. Coll. Cardiol. 71, 2279–2280. https://doi.org/10.1016/j.jacc.2018.03.453 (2018).
Knuuti, J. et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. https://doi.org/10.1093/eurheartj/ehz425 (2019).
Escaned, J. et al. Prospective assessment of the diagnostic accuracy of instantaneous wave-free ratio to assess coronary stenosis relevance: Results of ADVISE II International, Multicenter Study (ADenosine Vasodilator Independent Stenosis Evaluation II). JACC Cardiovasc. Interv. 8, 824–833. https://doi.org/10.1016/j.jcin.2015.01.029 (2015).
Hennigan, B. et al. Discordance Between Resting and Hyperemic Indices of Coronary Stenosis Severity: The VERIFY 2 Study (A Comparative Study of Resting Coronary Pressure Gradient, Instantaneous Wave-Free Ratio and Fractional Flow Reserve in an Unselected Population Referred for Invasive Angiography). Circ. Cardiovasc. Interv. 9, 1. https://doi.org/10.1161/CIRCINTERVENTIONS.116.004016 (2016).
Jeremias, A. et al. Multicenter core laboratory comparison of the instantaneous wave-free ratio and resting Pd/Pa with fractional flow reserve: The RESOLVE study. J. Am. Coll. Cardiol. 63, 1253–1261. https://doi.org/10.1016/j.jacc.2013.09.060 (2014).
Lee, J. M. et al. Physiological and clinical assessment of resting physiological indexes. Circulation 139, 889–900. https://doi.org/10.1161/CIRCULATIONAHA.118.037021 (2019).
De Rosa, S., Polimeni, A., Petraco, R., Davies, J. E. & Indolfi, C. Diagnostic performance of the instantaneous wave-free ratio: Comparison with fractional flow reserve. Circ Cardiovasc Interv 11, e004613. https://doi.org/10.1161/CIRCINTERVENTIONS.116.004613 (2018).
Toth, G. G. et al. Standardization of fractional flow reserve measurements. J. Am. Coll. Cardiol. 68, 742–753. https://doi.org/10.1016/j.jacc.2016.05.067 (2016).
Matsumoto, H. et al. Feasibility of intracoronary nicorandil for inducing hyperemia on fractional flow reserve measurement: Comparison with intracoronary papaverine. Int. J. Cardiol. https://doi.org/10.1016/j.ijcard.2020.05.013 (2020).
Matsumoto, H. et al. Effect of caffeine on intravenous adenosine-induced hyperemia in fractional flow reserve measurement. J. Invasive Cardiol. 26, 580–585 (2014).
Matsumoto, H. et al. Is caffeine abstention necessary before adenosine-induced fractional flow reserve measurement?. J. Am. Coll. Cardiol. 66, 1943–1945. https://doi.org/10.1016/j.jacc.2015.08.034 (2015).
Tanaka, H. et al. Linear concentration-response relationship of serum caffeine with adenosine-induced fractional flow reserve overestimation: A comparison with papaverine. EuroIntervention https://doi.org/10.4244/EIJ-D-21-00453 (2021).
Echavarria-Pinto, M. et al. Combining baseline distal-to-aortic pressure ratio and fractional flow reserve in the assessment of coronary stenosis severity. JACC Cardiovasc. Interv. 8, 1681–1691. https://doi.org/10.1016/j.jcin.2015.09.002 (2015).
Lee, S. H. et al. Physiologic characteristics and clinical outcomes of patients with discordance between FFR and iFR. JACC Cardiovasc. Interv. 12, 2018–2031. https://doi.org/10.1016/j.jcin.2019.06.044 (2019).
Cook, C. M. et al. Fractional flow reserve/instantaneous wave-free ratio discordance in angiographically intermediate coronary stenoses: An analysis using doppler-derived coronary flow measurements. JACC Cardiovasc. Interv. 10, 2514–2524. https://doi.org/10.1016/j.jcin.2017.09.021 (2017).
Warisawa, T. et al. Physiological pattern of disease assessed by pressure-wire pullback has an influence on fractional flow reserve/instantaneous wave-free ratio discordance. Circ. Cardiovasc. Interv. 12, e007494. https://doi.org/10.1161/CIRCINTERVENTIONS.118.007494 (2019).
Wilson, R. F. & White, C. W. Intracoronary papaverine: An ideal coronary vasodilator for studies of the coronary circulation in conscious humans. Circulation 73, 444–451 (1986).
Seto, A. H., Tehrani, D. M., Bharmal, M. I. & Kern, M. J. Variations of coronary hemodynamic responses to intravenous adenosine infusion: implications for fractional flow reserve measurements. Catheter Cardiovasc. Interv. 84, 416–425. https://doi.org/10.1002/ccd.25305 (2014).
Mizukami, T. et al. Duration of hyperemia with intracoronary administration of papaverine. J. Am. Heart Assoc. 10, e018562. https://doi.org/10.1161/JAHA.120.018562 (2021).
Pijls, N. H. & Sels, J. W. Functional measurement of coronary stenosis. J. Am. Coll. Cardiol. 59, 1045–1057. https://doi.org/10.1016/j.jacc.2011.09.077 (2012).
Johnson, N. P. et al. Repeatability of fractional flow reserve despite variations in systemic and coronary hemodynamics. JACC Cardiovasc. Interv. 8, 1018–1027. https://doi.org/10.1016/j.jcin.2015.01.039 (2015).
De Luca, G., Venegoni, L., Iorio, S., Giuliani, L. & Marino, P. Effects of increasing doses of intracoronary adenosine on the assessment of fractional flow reserve. JACC Cardiovasc. Interv. 4, 1079–1084. https://doi.org/10.1016/j.jcin.2011.08.004 (2011).
Smits, P. C. et al. Fractional flow reserve-guided multivessel angioplasty in myocardial infarction. N. Engl. J. Med. 376, 1234–1244. https://doi.org/10.1056/NEJMoa1701067 (2017).
Collet, C. et al. Measurement of hyperemic pullback pressure gradients to characterize patterns of coronary atherosclerosis. J. Am. Coll. Cardiol. 74, 1772–1784. https://doi.org/10.1016/j.jacc.2019.07.072 (2019).
van Dijk, R., Ties, D., Kuijpers, D., van der Harst, P. & Oudkerk, M. Effects of caffeine on myocardial blood flow: A systematic review. Nutrients 10, 1. https://doi.org/10.3390/nu10081083 (2018).
Kramer, C. M. et al. Standardized cardiovascular magnetic resonance (CMR) protocols 2013 update. J. Cardiovasc. Magn. Reson. 15, 91. https://doi.org/10.1186/1532-429X-15-91 (2013).
Dorbala, S. et al. Single photon emission computed tomography (SPECT) myocardial perfusion imaging guidelines: instrumentation, acquisition, processing, and interpretation. J. Nucl. Cardiol. 25, 1784–1846. https://doi.org/10.1007/s12350-018-1283-y (2018).
de Bruyne, B. et al. Simultaneous coronary pressure and flow velocity measurements in humans: Feasibility, reproducibility, and hemodynamic dependence of coronary flow velocity reserve, hyperemic flow versus pressure slope index, and fractional flow reserve. Circulation 94, 1842–1849. https://doi.org/10.1161/01.cir.94.8.1842 (1996).
Lee, J. M. et al. Clinical outcomes according to fractional flow reserve or instantaneous wave-free ratio in deferred lesions. JACC Cardiovasc. Interv. 10, 2502–2510. https://doi.org/10.1016/j.jcin.2017.07.019 (2017).
Johnson, N. P. et al. Prognostic value of fractional flow reserve: Linking physiologic severity to clinical outcomes. J. Am Coll. Cardiol. 64, 1641–1654. https://doi.org/10.1016/j.jacc.2014.07.973 (2014).
Adjedj, J. et al. Significance of intermediate values of fractional flow reserve in patients with coronary artery disease. Circulation 133, 502–508. https://doi.org/10.1161/CIRCULATIONAHA.115.018747 (2016).
Pijls, N. H. et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J. Am. Coll. Cardiol. 49, 2105–2111. https://doi.org/10.1016/j.jacc.2007.01.087 (2007).
Kuramitsu, S. et al. Two-year outcomes after deferral of revascularization based on fractional flow reserve: The J-CONFIRM registry. Circ. Cardiovasc. Interv. 13, e008355. https://doi.org/10.1161/CIRCINTERVENTIONS.119.008355 (2020).
Tu, S. et al. Diagnostic accuracy of fast computational approaches to derive fractional flow reserve from diagnostic coronary angiography: The international multicenter FAVOR pilot study. JACC Cardiovasc. Interv. 9, 2024–2035. https://doi.org/10.1016/j.jcin.2016.07.013 (2016).
Westra, J. et al. Evaluation of coronary artery stenosis by quantitative flow ratio during invasive coronary angiography: The WIFI II Study (Wire-Free Functional Imaging II). Circ. Cardiovasc. Imaging 11, e007107. https://doi.org/10.1161/CIRCIMAGING.117.007107 (2018).
Author information
Authors and Affiliations
Contributions
Contributions of authors: H.M., conception, design, data collection, analysis of data, and drafting the manuscript; S.H., analysis of data, critical revision of the manuscript; H.T., data collection, analysis of data; R.M., data collection, analysis of data; S.K., data collection, analysis of data; H.T. data collection, analysis of data; T.S., critical revision of the manuscript, and final approval of submission. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Matsumoto, H., Higuchi, S., Tanaka, H. et al. Insufficient adenosine-induced hyperemia is a major determinant of discordance between non-hyperemic pressure ratio and fractional flow reserve. Sci Rep 13, 729 (2023). https://doi.org/10.1038/s41598-023-27929-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-27929-1
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.