Abstract
The poultry red mite (PRM), Dermanyssus gallinae, is arguably the most harmful, ubiquitous haematophagous ectoparasite infesting egg-laying hens. PRM is a vector of various microorganisms, with some being important for food microbiology and public health. The present study aimed to investigate the presence of specific pathogens, including Escherichia coli, Salmonella spp. and Listeria spp., carried by PRM infesting a chicken farm in Greece. Mites were caught using cardboard traps (Avivet), and 100 unwashed PRM were homogenized and used for microbiological cultures. Microbiological cultures were carried out on general and selective substrates to detect the above-mentioned bacteria. Specifically for Listeria spp., DNA was extracted from bacteria grown in Tryptone Soya Yeast Extract Agar using a commercial kit. The hly gene encoding the Listeriolysin O protein was amplified by PCR. Mites were identified as D. gallinae using morphological keys as well as by COI DNA barcoding. Microbiological cultures and PCR assays were positive for Listeria monocytogenes. No other bacteria were detected. The current study constitutes the first molecular isolation of L. monocytogenes from D. gallinae, confirming that PRM can carry this food-borne pathogen. PRM control measures and hygiene practices should be applied to minimize any possible contamination risk of poultry products with L. monocytogenes and safeguard public health.
Similar content being viewed by others
Introduction
The poultry red mite (PRM), Dermanyssus gallinae (De Geer 1778), is one of the most harmful ectoparasites in the modern egg-laying industry, having a worldwide distribution1. D. gallinae is an obligatory hematophagous mite and its blood-sucking feeding behaviour may negatively affect the welfare, health, and production of chickens2,3, effectively causing 231 million euros in losses solely in Europe4. Prevalences for the PRM are high in European laying hen farms5, even reaching 100% in Northern Greece6. Treatment options include synthetic pesticides, i.e., phoxim or fluralaner, and other biological or physical control measures2. However, PRM has developed resistance to different acaricides7,8,9 over the past decade, making its control even more difficult. Its life cycle consists of five stages. Eggs and the six-legged larvae do not feed on blood, while the eight-legged protonymphs, deutonymphs, and adults are hematophagous. Nymphs feed to moult to the next stage. Female adults feed to lay eggs, while male adults only feed periodically. Surprisingly, female mites can survive for 9 months without feeding7. Usually, the PRM feeds during the night, in darkness, for approximately 1 h every 2–4 days1,8,9. It prefers to feed on the hen’s body parts that are not covered with feathers, such as the breast and lower legs10, or from superficial veins on the neck and back11. Throughout the day, D. gallinae hides in the hens' environment, specifically cracks and crevices, under the egg belt or metal connections of cages, inside perches, or in the chickens’ nests1. They gain access to the host by travelling through the poultry house equipment and climbing up their legs or falling from the ceiling11. Unfed mites have a pale grey colour and, in contrast, engorged mites have a brown to bright red colour12. Adult females can drink 204 μg of blood, which amounts to 2.7 times their body weight13. In severe infestation cases, mites can ingest as much as 6% of the total blood volume of a hen within a day9. Under optimal conditions (30 °C temperature and 70–85% relative humidity) the life cycle can be completed in as little as six days14. As a result, population densities can increase rapidly, doubling in less than 6 days15, even reaching 150,000–200,000 mites per hen16. The PRM is more prevalent in summer than in winter, and mite populations reach their peak numbers around 5 months after the start of infestation before plateauing17. PRM of all stages are vulnerable to low (< 30%) relative humidity7,18 and are killed by washing the poultry houses19. Mites cannot withstand temperatures above 45 °C20 and below − 20 °C7. Extensive farming systems provide more hiding spots for the mites and make acaricide application difficult21. In addition, alternative systems and backyard farms exhibit higher PRM prevalence rates22.
Several pathogenic microorganisms have been isolated from the PRM including bacteria such as Escherichia coli and Pasteurella multocida4. For some of them, transmission and vector competence has also been demonstrated,, as is the case for Influenza type A virus23 and Salmonella enterica subsp. enterica serovar Enteritidis24,25. Some zoonotic pathogens are a major concern for food microbiology4, connecting many different disciplines of biological sciences such as parasitology, bacteriology and public health safety. For instance, the zoonotic bacterium Listeria monocytogenes is an emerging food-borne pathogen26 with reported listeriosis human cases27 and outbreaks28 usually attributed to contaminated poultry products instead of direct infections from infected chickens29. Contamination of poultry products (raw meat and eggs) might be caused directly by the hens or their environment30,31. Transmission can also occur through ingestion of contaminated water or airborne through contaminated soil and dust29. Clinical Listeria infections both in humans and in chickens are treated with antibiotics31. The connection between L. monocytogenes and D. gallinae up until now has been at the very least questioned32. L. monocytogenes has only been isolated once in a culture from PRM infesting wild animals and not chickens, more than 50 years ago with the original study presented in Russian and inaccessible to most researchers. Furthermore, no molecular tools were employed to confirm the pathogen’s identity33. Herein, we aim to report the first molecular detection of Listeria spp. in PRM. This finding is part of a larger study investigating the haplotypes of PRM and the presence of specific pathogens, including Escherichia coli, Salmonella spp. and Listeria spp., carried by PRM in 50 different backyard poultry farms in Greece. The current work could shed light on possible transmission routes of L. monocytogenes to chickens and consequently to humans through poultry products.
Methods
Backyard chicken farm history and sampling
The backyard poultry farm was located in Central Macedonia, Northern Greece and employed a free-range system. Sample collection was performed in October 2021. Prior to sampling, the farmer gave permission to take samples and filled in a questionnaire providing all appropriate information regarding farming practices. Based on the answers, the owner had more than 30 years of experience as a poultry farmer. Thirty-five hens of different ages were kept on the poultry farm, with most of them being 52 weeks old and belonging to the Lohmann brown breed. Even though PRM had been infesting the farm for many years, the owner believed that PRM did not affect hen health and that egg production was on the expected level. However, the chickens only produced eight eggs per day, despite their age. All hens were vaccinated with commercial vaccines against Salmonella spp. and Marek's disease virus. Mites were visible on the walls (flat surfaces), but the eggs did not have any blood spots (from crushed mites). Moreover, the owner complained of feeling PRM bites on the skin and itching.
The hen house was primarily made of wood with some bricks. On the outside, trees with other birds’ nests, such as swallows and pigeons, surrounded it. Chickens roamed freely in the farm's backyard and sometimes fed on the owner's home-grown vegetables. The owner did not use any egg cartons but instead collected the eggs in a bucket. Chickens did not receive any treatment for PRM, such as fluralaner, deltamethrin, diatomaceous earth, desiccant dust, or other formulations. Only cold water was used once every 3 months to wash the hen house, but with no visible effect on PRM populations. Furthermore, no monitoring devices such as cardboards were employed to assess fluctuations in PRM numbers. In order to catch the PRM, ten specially designed cardboard traps, the AviVet Red Mite Trap™, (Avivet, adVee Dierenartsen, Heeswijk Dinther, The Netherlands) were used34 that were placed inside various cracks, perches, and nests, where mites usually hide during the day1. The traps covered the entirety of the hen house and were left for one week before being collected again to maximise the number of PRM caught. Consequently, traps were placed inside plastic sealed bags and transported to the School of Veterinary Medicine, Faculty of Health Sciences, Aristotle University of Thessaloniki for further examination.
Mite identification
A few drops of lactophenol were used to soften and clarify the mites before examining them at 100 × and 400 × magnification under an optical microscope (Olympus, CX21 Microscope). The genomic DNA of three separate mites was extracted using a commercial kit (QIAamp DNA mini kit Extraction Kit, Qiagen, Hilden, Germany) as previously described35. The synthetic oligonucleotide primers COI1Fyuw114 and COI1Ryuw11435 were used in this study to amplify a partial mitochondrial Cytochrome C Oxidase subunit I (COI) gene segment, 681 base pairs (bps) in length. PCR reaction was carried out in a 30 μL volume comprising 3 μL of 10 × Buffer (Qiagen), 1.2 μL (2.5 mM) MgCl2 (Qiagen), 0.3 μL (100 µM) of each oligonucleotide primer, 0.75 μL (2 mM) dNTPs, 0.45 μL (0.05 U) of Taq polymerase (Qiagen) and 5 μL (100 ng) of genomic DNA. PCR amplification was achieved using an Eppendorf Mastercycler (Eppendorf, Hamburg, Germany) with the following cycling program: initial denaturation (5 min, 95 °C), 35 denaturation cycles (30 s each, 95 °C), annealing (45 s, 58 °C), and extension (40 s, 72 °C) prior to a final extension cycle (7 min, 72 °C). Both positive and negative controls were employed, and the resulting PCR products were analysed by agarose gel electrophoresis (AppliChem, Darmstadt, Germany) and visualised using ultraviolet light. Amplicons purification, sequencing and alignment of the derived sequences were carried out as described in a previous work of our lab35.
Bacterial cultures
Microbiological cultures were performed for E. coli, Salmonella spp. and L. monocytogenes using selective media. In detail, L. monocytogenes was isolated from the samples using the methodology based on EN ISO 11290-1:2017. Approximately 100 unwashed bodies of D. gallinae mites were pooled from the traps and homogenised in 0.9 ml of half Fraser broth (Biolife, Milan, Italy) using Biomasher II disposable homogeniser tubes (Nippi Inc, Tokyo, Japan) and incubated at 30 °C for 24 h. For the secondary enrichment, 0.1 ml of the culture was transferred to a tube containing 10 ml of Fraser broth (Biolife) and incubated at 37 °C for 24 h. Consequently, a loopful (10 μl) from Fraser broth was streaked onto Agar Listeria acc. to Ottaviani and Agosti (ALOA) (Biolife) and Listeria Palcam agar (Biolife) (37 °C, 48 h). Five suspected L. monocytogenes colonies were streaked on Tryptone Soya Yeast Extract (TSYE) agar (Merck, Darmstadt, Germany) (24 h, 37 °C) for conducting the confirmation tests (Beta-haemolysis, L-Rhamnose, D-Xylose).
DNA extraction from cultures
DNA was extracted from bacterial colonies grown in TSYE agar using the Nucleospin Tissue extraction kit (Macherey–Nagel, Duren, Germany). In detail, bacterial colonies were removed from TSYE Agar plates and suspended in 1 ml phosphate-buffered saline (pH 7.4). Consequently, 0.2 ml of the above suspension was used for DNA extraction following the instructions of the selected kit.
PCR assay and primers for L. monocytogenes
The synthetic oligonucleotide primers (working solution 10 μM) used in this study and the size of the amplified selected fragment are listed in Table 136. This primer pair amplifies a species-specific PCR product in L. monocytogenes, whereas no product is amplified in other Listeria spp. or other bacterial genera) and therefore can reliably distinguish the presence of L. monocytogenes37.
The amplification was performed in a total volume of 20 μL containing 2 μL of DNA sample, 1.5 mM MgCl2, 0.2 mM (each) dNTPs, 0.2 μM of each primer, and 0.2 U/reaction of Taq DNA polymerase (KAPA Biosystems, Germany). PCR assays were performed with a model T100 thermal cycler (Bio-Rad, California, USA) under the following conditions: 95 °C for 3 min and then 35 cycles consisting of denaturation at 95 °C for 30 s, annealing at 55 °C for 30 s, and extension at 72 °C for 1 min with a final extension step at 72 °C for 7 min. Five microliters of the reaction mixture were mixed with 2 μl of loading buffer and separated on a 1.5% agarose gel in a TBE buffer (90 mM Trizma base, 90 mM boric acid, 2 mM EDTA, pH 8.3). The PCR product was visualised by ethidium bromide staining on a UV transilluminator (Cleaver Scientific Ltd, Warwickshire, UK).
This research was carried out under the approval from the Ethics Committee of the Aristotle University of Thessaloniki (639/13-07-2020). All experiments were performed in accordance with relevant guidelines and regulations. Informed consent was obtained from all the participants to participate in this study. Also, the farmer gave permission to publish any relevant information arising from the study.
Ethics approval and consent to participate
There was no interaction with the chickens or harm caused to them. This research was carried out under the approval from the Ethics Committee of the Aristotle University of Thessaloniki (639/13-07-2020).
Results
Mite identification results
In the Laboratory of Parasitology and Parasitic Diseases, mites were identified as D. gallinae based on morphological criteria38. The resulting PCR products from the 3 separate mites were 681 bps long based on gel electrophoresis and transillumination. DNA sequencing was successful in all 3 individual mite samples, and all 3 mites had one identical haplotype that was 520-bps long (GenBank accession number: ON597616). The haplotype identified in the current study was 99.81% similar to other PRM haplotypes previously identified in Japan39, further confirming that mites belonged to the species D. gallinae.
Bacterial cultures and PCR for L. monocytogenes
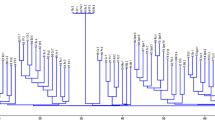
Microbiological cultures and confirmation tests were only positive for L. monocytogenes (Fig. 1) and negative for E. coli and Salmonella spp. DNA was successfully extracted from TSYE agar and amplified using PCR. The resulting PCR product was 520 bps long based on gel electrophoresis and transillumination (Fig. 2), further confirming the presence of L. monocytogenes.
Transillumination under ultraviolet light of the 520 base pairs (bps) long PCR product after agarose gel electrophoresis and ethidium bromide staining, confirming the presence of Listeria monocytogenes on Dermanyssus gallinae. The sampled DNA was extracted from bacterial colonies grown in TSYE agar, and the primers used targeted the hly gene that encodes the Listeriolysin O protein. Abbreviations: PCR, Polymerase chain reaction; TSYE, Tryptone soya yeast extract.
Discussion
L. monocytogenes is a ubiquitous Gram-positive facultative pathogenic saprophyte with an intracellular life cycle40 that can persist in the environment at temperatures between 0 °C and 45 °C31. It can replicate under refrigerator conditions31 and survive in high moisture environments for many years29. L. monocytogenes is the primary aetiologic agent of listeriosis, an infectious disease affecting humans and birds, among other animals26,31. Although most bird infections are subclinical and adult chickens rarely display clinical signs, listeriosis outbreaks have been reported in backyard poultry farms41. Young chicks are typically more susceptible29, and clinical signs include diarrhoea, encephalitis, septicaemia, lower egg production41, and mortality29. Like the sampled farm in the current study, chickens living in humid and low-temperature environments with wet litter have a higher risk of infection29. Other predisposing risk factors that can increase environmental contamination with L. monocytogenes at the farm level include lack of sanitary measures, no vermin control programs, use of nipples without cups as a watering system, presence of other animals at the farm, and inadequate disposal of faeces42. Noteworthy, the current backyard farm sampled had all these risk factors.
The bacterium consists of four distinct lineages40 and, until now, 14 serotypes have been identified43. Human listeriosis cases can be primarily attributed to lineage I and secondarily to lineage II, with the latter mainly being isolated in food and food production facilities40. Listeriolysin O (LLO) is a cholesterol-dependent cytotoxin found in L. monocytogenes and is encoded by the hly gene44. The LLO peptide significantly increases the strain's virulence45 and is linked with human listeriosis outbreaks44,46, although other genes have also been reported to affect virulence31. LLO-positive strains are 5-logs more virulent and spread more quickly than LLO-negative strains46. PCR is a fast and sensitive technique that can amplify the hly gene to confirm the presence of L. monocytogenes from selective growth media29, as carried out in the present study. Determination of the infecting lineage and serotype is vital in human infections in the One Health approach47 since listeriosis is an emerging food-borne zoonotic disease29. Virtually all L. monocytogenes infections are food-borne40. Chickens with listeriosis can infect humans, and the disease can result in the patient's death in just two days29. Humans can also exhibit cutaneous lesions after direct contact with infected chickens or contaminated soil29. Contamination of poultry products, mainly chicken carcasses, is caused by poor hygiene measures and unsafe handling practices, i.e., not washing hands or cutting boards and not separating raw and cooked meat27,48. In our study, the specific L. monocytogenes strain was positive for the LLO protein, based on the successfully amplified hly gene.
D. gallinae in the specific poultry farm probably acquired L. monocytogenes when moving inside the poultry house49. Chickens can serve as natural reservoirs for the specific pathogen50 and excrete L. monocytogenes with their faeces51 and other secretions29. The farm’s environment, such as dust52, litter53, soil31, grass54, water, feed55, decomposing vegetation41, nests, walls, floors, faeces, and other matrices can be contaminated with L. monocytogenes29,30. Transmission occurs when chickens ingest these contaminated sources, when their wounds get contaminated or when they inhale the pathogen29. L. monocytogenes is common in poultry in Greece and, in the past, has been isolated from 38% of poultry samples in a slaughterhouse56. Since mites were not washed before performing the bacteriological culture, we cannot distinguish if L. monocytogenes was harboured inside the PRM or just mechanically carried outside on its cuticle. In our study, the mites were processed according to published methodology (without washing them)57,58,59, though in some other studies mites were washed for example with 4% paraformaldehyde60,61. Mites were internally infected or externally contaminated (i.e., in their dorsal shield, genitoventral shield, legs, and chelicerae)38 from apparently healthy chickens or other environmental sources. As demonstrated in previous studies, not washing the PRMs before processing provides more information and all-round knowledge on the vectorial potential of D. gallinae59. According to our results, the PRM can be added to the list of L. monocytogenes vectors, alongside carriers such as rodents, insects, and flies that can disseminate the pathogen on a farm29. D. gallinae can actively or passively move between facilities (i.e., poultry houses and slaughterhouses) using humans as transport hosts (hair, shoes, clothes) or through tools and equipment (egg containers, pallets, crates, and brooms, among others)19. In this backyard farm, chickens were mainly kept for eggs, but occasionally, some were slaughtered for their meat. The farm also had no sanitary measures in effect. Therefore, Listeria-carrying D. gallinae could suck blood from chickens and infect their wounds or get eaten by them, which represent the two most common pathogen transmission routes from PRM to hens62,63. Moreover, the farm had a heavy PRM infestation, as evident by the mite populations caught in the traps and mites walking on equipment that could significantly enhance the likelihood of mechanical transmission64 and help spread L. monocytogenes. Contamination of poultry products was a real possibility that could threaten public health65. Suggestions were made to the farmer regarding disinfection of the farm for L. monocytogenes and treatment of hens with a licensed product for PRM.
Future research should focus on elucidating possible transmission routes of Listeria spp. Between mites and hens and detecting the same genotype in mites and meat after slaughter. That should be done on much more numerous samples (different timepoints and farms) to assess the PRM vectorial role for the specific pathogen. Nevertheless, the current work constitutes a preliminary study that helps to solidify the broad spectrum of D. gallinae as a vector of different pathogens.
Conclusions
The current work describes the first molecular isolation of L. monocytogenes from PRM, confirming that D. gallinae can carry this food-borne pathogen, which has only been questionably isolated once in the past. Control measures are required to reduce PRM populations in chicken farms, and farmers should additionally apply hygiene and sanitisation practices to minimise any possible contamination risk of poultry products with L. monocytogenes. Since antibiotics are used to treat listeriosis in hens and humans, combating D. gallinae in poultry houses could prevent transmission of L. monocytogenes, and reduce the need for antibiotics while protecting public health. The finding of L. monocytogenes further expands the vectorial role of D. gallinae highlighting how the PRM could impact other sectors, outside the sampled farm, such as food production facilities threatening public health safety. Overall, the PRM may severely affect hen health both through its haematophagous action and its ability to transmit pathogens.
Data availability
The nucleotide sequence data of the 520-bps long identical haplotype identified in all 3 individual mite samples has been deposited in GenBank (GenBank Accession Number: ON597616).
Abbreviations
- Bps:
-
Base pairs
- COI:
-
Cytochrome oxidase subunit 1
- DNA:
-
Deoxyribonucleic acid
- LLO:
-
Listeriolysin O
- PCR:
-
Polymerase chain reaction
- PRM:
-
Poultry red mite
- TSYE:
-
Tryptone soya yeast extract
References
Chauve, C. The poultry red mite Dermanyssus gallinae (De Geer, 1778): Current situation and future prospects for control. Vet. Parasitol. 79, 239–245 (1998).
Decru, E. et al. Possibilities for IPM strategies in European laying hen farms for improved control of the poultry red mite (Dermanyssus gallinae): Details and state of affairs. Front. Vet. Sci. 7, 1–19 (2020).
Sleeckx, N. et al. Production losses in laying hens during infestation with the poultry red mite Dermanyssus gallinae. Avian Pathol. 48, S17–S21. https://doi.org/10.1080/03079457.2019.1641179 (2019).
Sigognault Flochlay, A., Thomas, E. & Sparagano, O. Poultry red mite (Dermanyssus gallinae) infestation: A broad impact parasitological disease that still remains a significant challenge for the egg-laying industry in Europe. Parasites Vectors 10, 4–9 (2017).
Sparagano, O. et al. Prevalence and key figures for the poultry red mite Dermanyssus gallinae infections in poultry farm systems. Exp. Appl. Acarol. 48, 3–10 (2009).
Arsenopoulos, K., Angelou, A. & Papadopoulos, E. Dermanyssus gallinae—A ghost ectoparasite for Greek laying hen industry: Results of a preliminary study. In 4th Panhellenic Conf Vet Product Anim food Hyg. (2017).
Nordenfors, H., Höglund, J. & Uggla, A. Effects of temperature and humidity on oviposition, molting, and longevity of Dermanyssus gallinae (Acari: Dermanyssidae). J. Med. Entomol. 36, 68–72 (1999).
Kirkwood, A. Longevity of the mites Dermanyssus gallinae and Liponyssus sylviarum. Exp. Parasitol. 14, 358–366 (1963).
Wernery, U. Infectious diseases. In Avian Med 3rd edn (ed. Samour, J.) 434–521 (Elsevier, 2016).
Axtell, R. C. & Arends, J. J. Ecology and management of arthropod pests of poultry. Annu. Rev. Entomol. 35, 101–126 (1990).
Maurer, V., Bieri, M. & Fölsch, D. W. Das suchverhalten von Dermanyssus gallinae in Hühnerställen. Arch für Geflügelkd 52, 209–215 (1988).
Wang, C. et al. An efficient rearing system rapidly producing large quantities of poultry red mites, Dermanyssus gallinae (Acari: Dermanyssidae), under laboratory conditions. Vet. Parasitol. 258, 38–45. https://doi.org/10.1016/j.vetpar.2018.06.003 (2018).
Sikes, R. K. & Chamberlain, R. W. Laboratory observations on three species of bird mites. J. Parasitol. 40, 691–697 (1954).
Tucci, E. C., Prado, A. P. & Araújo, R. P. Development of Dermanyssus gallinae (Acari: Dermanyssidae) at different temperatures. Vet. Parasitol. 155, 127–132 (2008).
Maurer, V. & Baumgärtner, J. Temperature influence on life table statistics of the chicken mite Dermanyssus gallinae (Acari: Dermanyssidae). Exp. Appl. Acarol. 15, 27–40 (1992).
Kilpinen, O. et al. Influence of Dermanyssus gallinae and Ascaridia galli infections on behaviour and health of laying hens (Gallus gallus domesticus). Br. Poult. Sci. 46, 26–34 (2005).
Nordenfors, H. & Höglund, J. Long term dynamics of Dermanyssus gallinae in relation to mite control measures in aviary systems for layers. Br. Poult. Sci. 41, 533–540 (2000).
Cox, M., De Baere, K., Vervaet, E., Zoons, J. & Fiks-Van Niekerk, T. Red mites: Monitoring method and treatment. In Proceedings of the 8th European Symposium on Poultry Welfare 83 (2009).
Mul, M. F. & Koenraadt, C. J. M. Preventing introduction and spread of Dermanyssus gallinae in poultry facilities using the HACCP method. Exp. Appl. Acarol. 48, 167–181 (2009).
Mul, M. F., van Vugt, S. M. A., Goselink, Y. S. M. & van den Brand, H. Effects of heating laying hen houses between consecutive laying cycles on the survival of the poultry red mite Dermanyssus gallinae. Vet. Parasitol. 288, 109307. https://doi.org/10.1016/j.vetpar.2020.109307 (2020).
Chirico, J. & Tauson, R. Traps containing acaricides for the control of Dermanyssus gallinae. Vet. Parasitol. 110, 109–116 (2002).
Hoglund, J., Nordenfors, H. & Uggla, A. Prevalence of the poultry red mite, Dermanyssus gallinae, in different types of production systems for egg layers in Sweden. Poult. Sci. 74, 1793–1798 (1995).
Sommer, D., Heffels-Redmann, U., Köhler, K., Lierz, M. & Kaleta, E. F. Rolle der Roten Vogelmilbe (Dermanyssus gallinae) bei der Übertragung von aviärem Influenza-A-Virus. Tierarztl Prax Ausgabe G Grosstiere Nutztiere 44, 26–33 (2016).
Douifi, M., Ouchene, N. & Rahal, K. Dermanyssus gallinae in laying hens farms in Algeria: Infestation prevalence and molecular detection of Salmonella. Agricultura 105, 145–150 (2018).
Valiente Moro, C., Chauve, C. & Zenner, L. Experimental infection of Salmonella Enteritidis by the poultry red mite, Dermanyssus gallinae. Vet. Parasitol. 146, 329–336 (2007).
Dhama, K. et al. Listeria monocytogenes infection in poultry and its public health importance with special reference to food borne zoonoses. Pak. J. Biol. Sci. 16, 301–308 (2013).
Goh, S. G. et al. Listeria monocytogenes in retailed raw chicken meat in Malaysia. Poult. Sci. 91, 2686–2690 (2012).
McLauchlin, J. et al. Listeria monocytogenes in Cooked Chicken: Detection of an outbreak in the United Kingdom (2016 to 2017) and analysis of L. monocytogenes from unrelated monitoring of foods (2013 to 2017). J Food Prot. 83, 2041–2052 (2020).
Dhama, K. et al. Listeriosis in animals, its public health significance (food-borne zoonosis) and advances in diagnosis and control: A comprehensive review. Vet. Q. 35, 211–235 (2015).
Rothrock, M. J. et al. Listeria occurrence in poultry flocks: Detection and potential implications. Front. Vet. Sci. 4, 125 (2017).
Jamshidi, A. & Zeinali, T. Significance and characteristics of Listeria monocytogenes in poultry products. Int. J. Food Sci. 2019, 7835253 (2019).
Sparagano, O. & Giangaspero, A. Parasitism in egg production systems: The role of the red mite (Dermanyssus gallinae). In Improving the Safety and Quality of Eggs. Egg Products Egg Chemistry, Production and Consumption (Woodhead Publishing Limited, 2011).
Grebenyuk, R. V., Chirov, P. A. & Kadysheva, A. M. The role of wild animals and blood-sucking arthropods in the epizootiology of infection with Listeria. Rol’ Dikikh Zhivotnykh i Krovososushchikh Chlenistonogikh v Epizootol. List. Frunze, Kirghiz SSR; Izd. Ilim. Inst. Biol. Akad. Nauk Kirg. SSR, Frunze, Kirghiz, SSR. Kirghiz, SSR (1972).
Lammers, G. A., Bronneberg, R. G. G., Vernooij, J. C. M. & Stegeman, J. A. Experimental validation of the AVIVET trap, a tool to quantitatively monitor the dynamics of Dermanyssus gallinae populations in laying hens. Poult. Sci. 96, 1563–1572 (2017).
Sioutas, G. et al. Case of human infestation with dermanyssus gallinae (Poultry red mite) from swallows (hirundinidae). Pathogens 10, 1–10 (2021).
Golsteyn Thomas, E. J., King, R. K., Burchak, J. & Gannon, V. P. J. Sensitive and specific detection of Listeria monocytogenes in milk and ground beef with the polymerase chain reaction. Appl. Environ. Microbiol. 57, 2576–2580 (1991).
Chen, J. Q., Healey, S., Regan, P., Laksanalamai, P. & Hu, Z. PCR-based methodologies for detection and characterization of Listeria monocytogenes and Listeria ivanovii in foods and environmental sources. Food Sci. Hum. Wellness 6, 39–59. https://doi.org/10.1016/j.fshw.2017.03.001 (2017).
Di Palma, A., Giangaspero, A., Cafiero, M. A. & Germinara, G. S. A gallery of the key characters to ease identification of Dermanyssus gallinae (Acari: Gamasida: Dermanyssidae) and allow differentiation from Ornithonyssus sylviarum (Acari: Gamasida: Macronyssidae). Parasites Vectors 5, 1–10 (2012).
Chu, T. T. H., Murano, T., Uno, Y., Usui, T. & Yamaguchi, T. Molecular epidemiological characterization of poultry red mite, Dermanyssus gallinae, in Japan. J Vet Med Sci. 77, 1397–1403 (2015).
Orsi, R. H., de Bakker, H. C. & Wiedmann, M. Listeria monocytogenes lineages: Genomics, evolution, ecology, and phenotypic characteristics. Int. J. Med. Microbiol. 301, 79–96. https://doi.org/10.1016/j.ijmm.2010.05.002 (2011).
Crespo, R., Garner, M. M., Hopkins, S. G. & Shah, D. H. Outbreak of Listeria monocytogenes in an urban poultry flock. BMC Vet. Res. 9, 1–5 (2013).
Aury, K. et al. Risk factors for Listeria monocytogenes contamination in French laying hens and broiler flocks. Prev. Vet. Med. 98, 271–278. https://doi.org/10.1016/j.prevetmed.2010.11.017 (2011).
Li, F. et al. Mining of novel target genes through pan-genome analysis for multiplex PCR differentiation of the major Listeria monocytogenes serotypes. Int. J. Food Microbiol. 339, 109026. https://doi.org/10.1016/j.ijfoodmicro.2020.109026 (2021).
Quereda, J. J., Andersson, C., Cossart, P., Johansson, J. & Pizarro-Cerdá, J. Role in virulence of phospholipases, listeriolysin O and listeriolysin S from epidemic Listeria monocytogenes using the chicken embryo infection model. Vet. Res. 49, 1–9. https://doi.org/10.1186/s13567-017-0496-4 (2018).
Sabet, C., Lecuit, M., Cabanes, D., Cossart, P. & Bierne, H. LPXTG protein InlJ, a newly identified internalin involved in Listeria monocytogenes virulence. Infect. Immun. 73, 6912–6922 (2005).
Nguyen, B. N., Peterson, B. N. & Portnoy, D. A. Listeriolysin O: A phagosome-specific cytolysin revisited. Cell Microbiol. 21, 1–22 (2019).
Zeinali, T., Jamshidi, A., Bassami, M. & Rad, M. Serogroup identification and Virulence gene characterization of Listeria monocytogenes isolated from chicken carcasses. Iran J. Vet. Sci. Technol. 7, 9–19 (2015).
Goh, S. G. et al. Transmission of Listeria monocytogenes from raw chicken meat to cooked chicken meat through cutting boards. Food Control 37, 51–55. https://doi.org/10.1016/j.foodcont.2013.08.030 (2014).
Di Palma, A. & Mul, M. F. How can Dermanyssus gallinae (De Geer 1778) (Acari: Anactinotrichida: Dermanyssidae) walk upwards on slippery surfaces?. Avian Pathol. 48, S10–S16. https://doi.org/10.1080/03079457.2019.1608909 (2019).
Njagi, L. W. et al. Carrier status for Listeria monocytogenes and other Listeria species in free range farm and market healthy indigenous chickens and ducks. East Afr. Med. J. 81, 529–533 (2004).
Kalender, H. Detection of Listeria monocytogenes in faeces from chickens, sheep and cattle in Elaziǧ Province. Turk. J. Vet. Anim. Sci. 27, 449–451 (2003).
Chemaly, M., Toquin, M. T., Le Nôtre, Y. & Fravalo, P. Prevalence of Listeria monocytogenes in poultry production in France. J. Food Prot. 71, 1996–2000 (2008).
Roberts, B. N., Bailey, R. H., McLaughlin, M. R., Miles, D. M. & Brooks, J. P. Spatial and temporal analysis of microbial populations in production broiler house litter in the southeastern United States. J. Appl. Poult. Res. 22, 759–770 (2013).
Milillo, S. R. et al. Listeria monocytogenes and hemolytic Listeria innocua in poultry. Poult. Sci. 91, 2158–2163 (2012).
Fenlon, D. R. Wild birds and silage as reservoirs of Listeria in the agricultural environment. J. Appl. Bacteriol. 59, 537–543 (1985).
Sakaridis, I. et al. Prevalence and antimicrobial resistance of Listeria monocytogenes isolated in chicken slaughterhouses in Northern Greece. J. Food Prot. 74, 1017–1021 (2011).
Pugliese, N. et al. Circulation dynamics of Salmonella enterica subsp. enterica ser. Gallinarum biovar Gallinarum in a poultry farm infested by Dermanyssus gallinae. Med. Vet. Entomol. 33, 162–170 (2019).
Hamidi, A. et al. Dermanyssus gallinae in layer farms in Kosovo: A high risk for salmonella prevalence. Parasites Vectors 4, 2–4 (2011).
Oh, S. I., Do, Y. J., Kim, E., Yi, S. W. & Yoo, J. G. Prevalence of poultry red mite (Dermanyssus gallinae) in Korean layer farms and the presence of avian pathogens in the mite. Exp. Appl. Acarol. 81, 223–238. https://doi.org/10.1007/s10493-020-00502-5 (2020).
Cocciolo, G. et al. Evidence of vector borne transmission of Salmonella enterica enterica serovar Gallinarum and fowl typhoid disease mediated by the poultry red mite, Dermanyssus gallinae (De Geer, 1778). Parasites Vectors 13, 1–10. https://doi.org/10.1186/s13071-020-04393-8 (2020).
Schiavone, A., Pugliese, N., Circella, E. & Camarda, A. Association between the poultry red mite Dermanyssus gallinae and potential avian pathogenic Escherichia coli (APEC). Vet. Parasitol. 284, 109198. https://doi.org/10.1016/j.vetpar.2020.109198 (2002).
Valiente Moro, C. et al. Colonization and organ invasion in chicks experimentally infected with Dermanyssus gallinae contaminated by Salmonella Enteritidis. Avian Pathol. 36, 307–311 (2007).
Moro, C. V. et al. Experimental studies on the potential role of the poultry red mite, Dermanyssus gallinae, as a vector of Salmonella serotype Enteritidis. Trends Acarol. https://doi.org/10.1007/978-90-481-9837-5_89 (2010).
Marquardt, W. C. Chapter 14: Natural cycles of vector-borne pathogens. In The Biology of Disease Vectors 2nd edn (eds Higgs, S. & Beaty, B. J.) 175 (Academic Press, 2004).
Schlech, W. F. Foodborne listeriosis. Clin. Infect. Dis. 31, 770–775 (2000).
Acknowledgements
The research work was supported by the Hellenic Foundation for Research and Innovation (HFRI) under the 3rd Call for HFRI PhD Fellowships (Fellowship Number: 5949).
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
G.S., E.V.P., K.P., I.S., I.A.G. and E.P. conceptualised and designed the study. G.S. collected and prepared the samples for analysis. E.V.P., K.P. and G.S. performed the bacterial cultures. G.S., S.M., K.P. and A.T. performed the molecular work. E.V.P., K.P., E.P. and A.T. contributed reagents/materials/analysis tools. G.S., E.V.P., S.M., A.T., and E.P. analysed the data. E.V.P., G.S., S.M. and K.P. wrote the manuscript, E.P., G.S., I.A.G. and A.T. revised the manuscript. All authors read and approved the final version of the manuscript. Written informed consent has been obtained from the farm owner to publish this article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sioutas, G., Petridou, E., Minoudi, S. et al. Isolation of Listeria monocytogenes from poultry red mite (Dermanyssus gallinae) infesting a backyard chicken farm in Greece. Sci Rep 13, 685 (2023). https://doi.org/10.1038/s41598-023-27862-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-27862-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.