Abstract
Circulating protease inhibitors are important regulators of inflammation that are implicated in the pathophysiology of heart failure (HF). Secretory leukocyte protease inhibitor (SLPI) is a serine protease inhibitor which protects pulmonary tissues against inflammatory damage; however, its role in HF is not well understood. We sought to evaluate associations of circulating SLPI and genetically-mediated serum SLPI with incident HF and its subtypes in a multi-ethnic cohort of adults using clinical and genetic epidemiological approaches. Among 2,297 participants in the Multi-Ethnic Study of Atherosclerosis (MESA), each doubling of serum SLPI was independently associated with incident HF (HR 1.77; 95% CI 1.02–3.02; P = 0.04), particularly incident HF with preserved ejection fraction (HFpEF; HR 2.44; 95% CI 1.23–4.84; P = 0.01) but not HF with reduced ejection fraction (HFrEF; HR 0.95; 95% CI 0.36–2.46; P = 0.91). Previously reported circulating SLPI protein quantitative trait loci (pQTLs) were not associated with serum SLPI levels or incident HF among MESA participants. In conclusion, baseline serum SLPI levels, but not genetically-determined serum SLPI, were significantly associated with incident HF and HFpEF over long-term follow-up in a multi-ethnic cohort. Serum circulating SLPI may be a correlate of inflammation that sheds insight on the pathobiology of HFpEF.
Similar content being viewed by others
Introduction
Inflammation is a key driver of heart failure (HF) risk1. Despite this strong relationship, the mechanisms leading to HF in the setting of inflammation remain unclear. Immune cells secrete a variety of proteolytic enzymes, known as proteases, which can be detected by various methods and contribute to the progression of cardiovascular inflammation2,3,4,5,6,7. HF is characterized by low-grade systemic and cardiac inflammation with immune cell activation, and inhibition of inflammatory mast cell proteases prevents cardiac fibrosis and improves left ventricular dysfunction in animal models8. Therefore, the balance between circulating proteases and protease inhibitors may be critical in the modulation of the inflammatory response and pathophysiology of HF.
Secretory leukocyte protease inhibitor (SLPI), also known as antileukoproteinase, is a 11.7 kDa 107-amino acid non-glycosylated protein9. SLPI is primarily expressed in human epithelial cells, such as the lining of the respiratory, gastrointestinal, and genitourinary tracts. A second source of SLPI is inflammatory cells, including neutrophils, macrophages, dendritic cells, and mast cells10.
Structurally, SLPI consists of two core domains with distinct biological functions; the N-terminal domain provides antimicrobial activity while the C-terminal domain is responsible for protease inhibition11. In particular, SLPI inhibits damaging serine proteases, such as neutrophil elastase, chymotrypsin, and cathepsins. Through its anti-proteolytic and antimicrobial properties, SLPI protects local tissues against inflammatory damage and serves as an important regulator of innate and adaptive immunity. Two recent genome-wide association studies (GWAS) of the human blood plasma proteome in European ancestry cohorts identified multiple protein quantitative trait loci (pQTLs) associated with circulating plasma SLPI protein levels12,13. However, it is unclear how these SLPI pQTLs contribute to HF risk, particularly in a multi-ethnic population.
The role of serum and genetically-determined SLPI levels in incident HF is unknown. Recent studies demonstrated that elevated serum SLPI was associated with increased risk of incident low ankle-branchial index and atrial fibrillation, suggesting that increased serum SLPI may be predictive of circulatory and other cardiovascular disorders14,15. Given the important role of the protease-antiprotease balance in the regulation of inflammation, serum SLPI levels may have important implications for the development of HF, and provide new insights into the mechanisms driving this disease. We thus aimed in this study to evaluate the association of circulating SLPI levels with incident HF and its subtypes, as well as the relationship between genetically-determined serum SLPI with HF, in a multi-ethnic cohort.
Results
Participant characteristics
Baseline characteristics of the 2,297 participants in the final analytic cohort, stratified by quartile of serum SLPI, are presented in Table 1. Within the analytic cohort, median serum SLPI was 44,785 pg/mL (interquartile range: 38,671–52,340 pg/mL). Participants within the highest quartile of serum SLPI were older and more likely men, African American and Hispanic, and former smokers compared to participants in lower SLPI quartiles. Additionally, participants with higher serum SLPI had higher systolic and diastolic blood pressure, higher low-density lipoprotein cholesterol, higher triglycerides, higher fasting glucose, higher C-reactive protein (CRP) levels, higher N-terminal-pro brain natriuretic peptide (NT-proBNP), higher high sensitivity troponin T, and lower levels of estimated glomerular filtration rate (eGFR). Multi-Ethnic Study of Atherosclerosis (MESA) participants with missing serum SLPI levels or pre-existing cardiovascular disease (CVD) were excluded. Compared with participants in the final analytic cohort, MESA participants who were excluded from this analysis were older, had higher prevalence of hypertension, and more likely self-identified as White at baseline examination. In addition, excluded participants had lower eGFR, higher systolic blood pressure, and higher CRP at baseline compared to participants included in this analysis (Supplemental Fig. S1, Supplemental Table S1).
Association of serum SLPI levels with incident heart failure
Over a median follow-up of 13.9 years (interquartile range, 11.4–14.6 years), there were 111 total HF events. The incidence rate (per 1000 person-years) for HF was highest among participants in the highest quartile of serum SLPI (Fig. 1). On spline analysis, higher serum SLPI was linearly associated with greater risk of HF (non-linearity P = 0.68). (Supplemental Fig. S2). After adjustment for all chosen covariates, each doubling of serum SLPI was independently associated with 77% increased risk of HF (HR 1.77; 95% CI 1.02–3.02; P = 0.04) (Table 2). Among 350 participants of the analytic cohort with available NT-proBNP levels at Exam 1 or 2, there was a strong association between serum SLPI and NT-proBNP levels (β coefficient per doubling of SLPI = 0.85, standard error = 0.24, P ≤ 0.001) (Supplemental Fig. S3).
Association of serum SLPI levels with incident heart failure subtypes
Of the 111 HF events, 56 were incident hospitalization for HF with preserved ejection fraction (HFpEF), 47 were incident hospitalization for HF with reduced ejection fraction (HFrEF), and 8 were incident hospitalization for HF of unknown ejection fraction (EF). On evaluation of incident HF by EF categories, the incidence rates for both HFpEF and HFrEF were highest among individuals at the highest quartile of serum SLPI. (Fig. 1). On spline analysis, higher serum SLPI was associated with progressively greater risk of HFpEF; the effect size for risk of HFrEF appeared lower than that for HFpEF (Fig. 2).
Association of serum SLPI with heart failure subtypes. (A) Restricted cubic spline curves of the continuous association of SLPI with heart failure with preserved ejection fraction (HFpEF). (B) Restricted cubic spline curves of the continuous association of SLPI with heart failure with reduced ejection fraction (HFrEF). Log base 2 transformation of SLPI can be interpreted as “per doubling.” Horizontal red line indicates a hazard ratio (HR) of 1. Shaded areas represent 95% confidence interval (CI).
The associations of serum SLPI with risk of incident HFpEF and HFrEF are shown in Table 2. Associations of SLPI with incident HF with unknown EF are not shown due to limited number of such events. In unadjusted analyses, higher serum SLPI at baseline was associated with increased risk of incident HFpEF hospitalization, but not HFrEF. After adjustment for all chosen covariates, each doubling of SLPI was significantly associated with incident HFpEF (HR 2.44; 95% CI 1.23–4.84; P = 0.01), with higher overall magnitude of risk as all HF. Serum SLPI was not associated with risk of HFrEF (HR 0.95; 95% CI 0.36–2.46; P = 0.91) in fully adjusted models. While the association between serum SLPI and incident all HF was attenuated after additional adjustment for high-sensitivity troponin T in sensitivity analysis, the association between SLPI and incident HFpEF remained significant after adjustment for high-sensitivity troponin-T (HR 2.23; 95% CI 1.13–4.24; P = 0.02) (Supplemental Table S2). Upon subgroup analyses, the associations of serum SLPI with incident HF were consistent across pre-specified age, gender, smoking, systolic blood pressure, and CRP subgroups (Fig. 3).
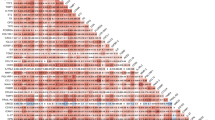
Association of serum SLPI and incident heart failure among subgroups. Cox proportional hazards models incorporating prespecified interaction terms were used to evaluate the associations of SLPI with incident heart failure in certain subgroups, including age, gender, smoking status, systolic blood pressure (SBP), and C-reactive protein (CRP). Error bars represent 95% confidence interval (CI) of hazard ratio (HR).
Association of previously reported circulating SLPI pQTLs with HF events in MESA
Two recent GWAS of the human blood plasma proteome in European ancestry cohorts identified multiple SNPs associated with circulating plasma SLPI protein levels12,13. We examined the relationships of these previously identified SLPI pQTLs with HF events in MESA. In total, we assessed three previously identified pQTLs that were either directly genotyped (rs3863292) or imputed (rs16920858, rs7205804) in MESA. There was no significant association between any of the three previously identified SLPI pQTLs with HF events in MESA participants after Bonferroni correction (Supplemental Table S3). In ancestry-specific and trans-ancestral analyses of MESA participants, we were unable to replicate the previously reported association of these variants with serum SLPI levels in MESA participants (Supplemental Table S4).
Discussion
The role of serum SLPI in incident HF is not well understood. In this multi-ethnic cohort of adults without CVD at baseline, we find substantial variation in serum SLPI levels. Participants with higher serum SLPI levels had higher systolic and diastolic blood pressure, higher low-density lipoprotein cholesterol, higher triglycerides, higher fasting glucose, higher CRP, higher NT-proBNP, and lower levels of eGFR. After adjustment for demographic and cardiovascular risk factors, baseline serum SLPI levels were significantly associated with higher risk for incident HF. On evaluation of HF subtypes, serum SLPI was strongly associated with incident HFpEF, but not HFrEF. The association of serum SLPI with incident HF was consistent across pre-specified subgroups, including inflammation as measured by CRP. Previously reported SLPI pQTLs were not associated with HF events in MESA participants, which may be due to a smaller sample size and small effect sizes of these pQTLs. Taken together, these data are consistent with the hypothesis that circulating SLPI levels may be an inflammatory correlate that sheds light upon the pathobiology of HFpEF (Fig. 4).
SLPI is not traditionally described as a systemic antiprotease. In contrast to circulating systemic antiproteases such as α1-antitrypsin and α2-macroglobulin, SLPI has classically been considered a type of “alarm antiprotease” that is produced locally in response to inflammatory cytokines and bacterial products with limited systemic expression16,17. This study suggests that significant levels of SLPI are found in the systemic circulation with sufficient variation to be used as a biomarker of disease.
We observed that participants within the highest quartile of serum SLPI were more likely men, African American and Hispanic, and former smokers compared to participants in lower SLPI quartiles. The higher levels of serum SLPI among men compared to women may be related to sex-specific differences in inflammation already present in mid-adulthood. Sex hormones have also been implicated in the regulation of SLPI expression18. The higher levels of serum SLPI among self-reported African American and Hispanics is less likely to be due to ancestral genetic variation given that previously reported SLPI pQTLs were not associated with serum SLPI levels in MESA participants in trans-ancestral or ancestry-specific analyses. Smoking is a significant risk factor for CVD and is known to transcriptionally increase SLPI expression through signal transducers and activators of transcription 1 (STAT1)19. However, the observed relationship between serum SLPI and HF was robust and independent of these potential confounders. Additionally, the associations of serum SLPI with incident HF were consistent across pre-specified age, gender, and smoking subgroups.
We demonstrate for the first time the prospective associations of baseline serum SLPI with symptomatic HF, as defined by incident HF hospitalization. The association of SLPI with HF was independent of systemic inflammation as measured by CRP levels. This suggests that SLPI may reflect cardiovascular inflammatory pathways distinct from those captured by CRP. This may be due to the different physiological responses to inflammation between CRP and SLPI20. While CRP is a hepatically-derived acute phase reactant that increases primarily in response to interleukin (IL)-6 secretion by macrophages and T cells, SLPI is transcriptionally upregulated in myeloid cells by toll-like receptor ligands and pattern recognition receptor ligands21. Additionally, SLPI mRNA expression in macrophages is upregulated by multiple interleukins, including IL-6 and IL-1022. Additional studies are needed to identify the specific inflammatory pathways that differentially upregulate CRP and SLPI in HF.
Interestingly, the association between SLPI and HF was driven by incident HFpEF but not HFrEF upon subgroup analysis. This differential association is notable because while many circulating proteins are associated with incident HFrEF, there are very few specific for incident HFpEF23,24,25,26,27,28. The SLPI-HFpEF association is also in accordance with the different contributions of inflammation to the pathophysiology of HFpEF as compared with HFrEF29. HFpEF is a systemic, multi-organ disorder, and previous work suggests that HFpEF may be the result of a comorbidity-induced systemic low-grade inflammatory state30. Consistent with this paradigm, we found that serum SLPI levels are positively correlated with multiple HFpEF comorbidities, including hypertension, diabetes, renal insufficiency, smoking, and dyslipidemia. Therefore, SLPI may partially reflect comorbidity-induced systemic inflammation in HFpEF. Meanwhile, the inflammation in HFrEF is hypothesized to be predominantly the result of direct myocardial injury and cardiomyocyte loss, which may not be sufficient to raise systemic SLPI levels. This is consistent with the GTEx database which demonstrates that SLPI is minimally expressed in the human left ventricle or atrial appendage. Additionally, on sensitivity analysis adjusting for high-sensitivity troponin T, only the association between SLPI and incident HFpEF remained consistent. In aggregate, our findings raise the possibility that SLPI-mediated anti-inflammatory pathways could be of particular therapeutic importance for HFpEF, a HF subtype that is in need of additional effective interventions.
Our clinical findings are also consistent with previous in vitro and in vivo animal models suggesting that SLPI is important for cardiac function. Overexpression of human SLPI in immortalized cardiomyocytes reduced cell death and injury in an in vitro model of ischemia/reperfusion injury31. The administration of recombinant SLPI also improved early recovery of cardiac function in a mouse model of cardiac transplantation and was associated with reduced protease activity and transforming growth factor (TGF)-β expression32. In addition to its secreted form, SLPI also has an intracellular form which has not been studied in cardiovascular models and may exert unique functions33.
Important insights into the mechanistic role of SLPI in HF may be found in prior studies of SLPI in different organ systems. In chronic obstructive pulmonary disease (COPD) and cystic fibrosis, SLPI protects against lung injury from excessive inflammatory immune responses. However, despite higher levels of SLPI in the sputum of patients with COPD, this upregulation of SLPI is ultimately insufficient to counteract the massive overproduction of proteases in advanced lung disease34. Meanwhile, inhibition of SLPI using a blocking antibody was associated with neutrophil accumulation and significantly increased lung injury35. It is possible that a similar mechanism exists in HFpEF, such that systemic SLPI expression is induced by low-level chronic inflammation, but ultimately the cardioprotective effects of endogenous SLPI production are overwhelmed by excessive inflammatory signaling in progressive HFpEF. Thus, we hypothesize that serum SLPI not only serves as a risk marker, but may also be cardioprotective, similar to B-type natriuretic peptide (BNP)32. Future studies with larger cohorts using multi-biomarker panels are also needed to definitively determine the potential role of serum SLPI as a biomarker of HFpEF risk using risk prediction modeling.
Previously reported SLPI pQTLs among Europeans were not associated with HF events in MESA participants12,13. We were also unable to replicate previously reported SLPI pQTLs among Europeans with serum SLPI levels in MESA participants. This lack of association may be explained by differences in sample size, genetic ancestry, environmental factors, or assay measurement between the previously studied European populations and participants in MESA. As such, larger studies with genetic data, serum SLPI levels, and a greater number of HF events are required to further elucidate whether genetically-mediated SLPI levels are associated with HF. These findings also underscore the importance of validating previously identified pQTLs with circulating protein levels across different population-based studies, particularly among populations of different ancestries. Given that we observed higher serum SLPI levels in participants with hypertension, hyperlipidemia, hyperglycemia, and kidney dysfunction, future analyses may also consider gene-environment interactions or epigenetic regulation of serum SLPI levels as a result of these acquired comorbidities.
Our study has several strengths. We used a combination of epidemiologic and genomic data from a large, ethnically diverse, community-based cohort that has been well characterized through longitudinal in-person examinations with a median follow up of 13.9 years to determine the development of HF. Incident HF was rigorously defined as hospitalization with evidence for imaging, treatment, or physician diagnosis of HF within the medical record, thus this definition was highly specific for symptomatic HF. Our study was the first to examine the association of SLPI with HF (including subtypes), which held true after adjusting for traditional inflammatory risk as measured by CRP. This is also the first study, to our knowledge, assessing SLPI pQTLs with incident HF in a multi-ethnic cohort.
The results of this study should be interpreted in the context of certain limitations. Although our final analytic cohort was large, several participants were excluded because of lack of serum SLPI measurement or pre-existing CVD. These excluded participants represented a slightly higher-risk group with a higher prevalence of cardiovascular risk factors, and thus our final analytic cohort may underestimate associations. Additionally, while we adjusted for various demographic, clinical, and laboratory covariates, our findings remain subject to potential residual confounding. Furthermore, incident HF hospitalizations (and their subtypes) were relatively low in this cohort, and the requirement of hospitalization for HF adjudication prevents detection of mild, outpatient cases of HF. Population-based external validation cohorts with high HF event rates are required to verify our findings of specific associations of serum SLPI with these incident CVD outcomes. While we did not adjust for NT-proBNP in our models assessing the association between SLPI and incident HF given the high degree of missingness of NT-proBNP at Exam 1 or 2 (n = 1947), elevated natriuretic peptides may mediate the association between SLPI-related inflammation and HF given the strong positive relationship between SLPI and NT-proBNP in our study. Additional investigations are also required to understand drivers of circulating SLPI expression, the role of cumulative SLPI exposure in HF risk, and clinically meaningful changes in SLPI over time.
In summary, baseline serum SLPI was significantly associated with HF over long-term follow-up in this multi-ethnic, community-based cohort. Notably, the increased risk of HF associated with SLPI was driven by incident HFpEF, but not HFrEF. The association of SLPI with HF was consistent across pre-specified subgroups, including baseline CRP level, suggesting that SLPI may reflect cardiovascular inflammatory pathways distinct from those captured by CRP. We did not observe a significant association between previously reported SLPI pQTLs and HF in MESA participants. Additionally, there was no significant association between previously reported SLPI pQTLs and serum SLPI levels in MESA participants, demonstrating importance of validating previously identified pQTLs with circulating protein levels across different population-based studies, particularly with diverse individuals. Additional molecular and larger, multi-ethnic population genomic studies are required to fully understand the potential mechanisms behind SLPI and incident HFpEF.
Methods
Study participants
The Multi-Ethnic Study of Atherosclerosis (MESA) study, as previously described, is a prospective cohort of 6,814 community-dwelling adults aged 45–84 years designed to understand the risk factors, prevalence, and progression of subclinical cardiovascular disease (CVD)36. In brief, participants who identified themselves as Black, Chinese, Hispanic, or non-Hispanic White were recruited between 2000 and 2002 across 6 study sites in the United States (Baltimore, MD; Chicago, IL; St. Paul, MN; Forsyth County, NC; New York, NY; and Los Angeles, CA). At the time of recruitment, participants had no history of CVD, defined as myocardial infarction, angina, stroke, transient ischemic attack, heart failure (HF), atrial fibrillation, nitroglycerin use, angioplasty, pacemaker or defibrillator, or cardiac surgery. After recruitment and a baseline in-person examination (examination 1), 5 additional follow-up in-person examinations were completed at 2–5 year intervals. Examinations included standardized questionnaires that collected information on demographics, medical history, and medication use. Resting blood pressure and blood sampling were also obtained during examinations. Diabetes mellitus was defined as self-reported diagnosis, fasting glucose ≥ 126 mg/dL, or use of antidiabetic medication. Estimated glomerular filtration rate (eGFR) was calculated by the Chronic Kidney Disease Epidemiology Collaboration equation using examination 1 serum creatinine. Baseline C-reactive protein (CRP) levels were collected at examination 1. Baseline N-terminal-pro brain natriuretic peptide (NT-proBNP) levels were collected at examination 1 or 2. Baseline high-sensitivity troponin T (hs-troponin T) levels were collected at examination 1 or 2.
For this analysis, we included participants with available serum secretory leukocyte protease inhibitor (SLPI) levels at examination 2 (conducted between 2002 and 2004) and available data on baseline covariates and follow-up. SLPI levels were measured as part of the MESA Adhesion Ancillary Study37. Of the 6814 individuals in MESA, 4517 were excluded: 4373 did not have SLPI levels drawn, 11 had CVD prior to Exam 2 (either HF or coronary heart disease), and 133 were missing covariate data at Exam 2. (Supplemental Fig. S1). Thus, the final analytic cohort for this analysis was 2297 participants. The MESA study protocol and its ancillary studies was approved by the institutional review board of each study site; all participants provided informed consent. All methods were performed in accordance with the relevant guidelines and regulations. Additional data that support the findings of this study are available from the corresponding author upon reasonable request.
SLPI measurement
At examination 2 (2002–2004), blood samples were obtained from participants after overnight fasting and were stored at − 70 °C. As part of the MESA Adhesion Ancillary Study, serum SLPI was measured by quantitative sandwich enzyme-linked immunosorbent assay (ELISA; R&D Systems, Minneapolis, MN)37. The interassay coefficient of variation was 8.9% at a mean concentration of 36,888 pg/mL and the minimum detectable level was 25 pg/mL.
Heart failure assessment
Incident hospitalized HF was adjudicated by 2 study physicians blinded to other study data through previously described medical record review36. In brief, the participants of MESA were screened for clinical events through regular telephone contact and in‐person examinations. All identified records from hospitalizations for CVD events were abstracted, and MESA personnel transmitted records of symptoms, medical history, biomarkers, electrocardiograms, echocardiograms, cardiac catheterization reports, other imaging studies, and outpatient records (if available) to the MESA coordinating center. HF events were defined as definite or probable. Both definite and probable HF events required symptoms of HF, including shortness of breath or edema. Definite HF was additionally defined on the basis of ≥ 1 of the following: pulmonary edema on chest radiography, left ventricular dilation or decreased systolic function, or evidence of diastolic dysfunction. If criteria for definite HF were not available, probable HF was defined as a physician diagnosis of HF in the clinical record and documentation of medical treatment for HF. The primary outcome of interest in this analysis was incident hospitalized HF, defined as any probable or definite HF event. We additionally evaluated HF subtypes (HF with preserved ejection fraction [HFpEF], HF with reduced ejection fraction [HFrEF], and HF with unknown ejection fraction) as secondary outcomes. HFpEF was defined as a HF event with documentation of left ventricular ejection fraction (EF) ≥ 45% on echocardiogram or radionucleotide study at time of hospitalization, and HFrEF was defined as EF < 45% at hospitalization. HF with unknown EF was defined as a HF event without documented EF on imaging study at time of hospitalization. Event ascertainment of HF in MESA has been fully updated and completed through 2017.
Genotyping and imputation
MESA participants were genotyped using the Affymetrix Genome-Wide Human SNP Array 6.0 through the MESA Candidate Gene Association Resource (CARe) and MESA SHARe projects. Of the 2297 participants in the final analytic cohort, genomic data was available for 2231 participants. The participants were stratified by self-reported race/ethnicity. Genotype imputation was performed using IMPUTE (version 2.1.0)38 and HapMap Phase I and II reference panels (release #22, National Center for Biotechnology Information Build 36 [dbSNP b126]). Black, Chinese, and Hispanic participants were imputed using the CEU + YRI + CHB + JPT reference panels and non-Hispanic White participants were imputed using the CEU reference panels.
Analyses of previously reported SLPI protein quantitative trait loci (pQTL)
A previous GWAS conducted in the Cooperative Health Research in the Region of Augsburg (KORA) Study investigating associations between SNPs and 1,124 plasma protein levels identified four SNPs associated with circulating SLPI12. Of these four SNPs, one was directly genotyped (rs3863292) and one was imputed (rs16920858) in MESA. A previous GWAS conducted in 35,559 Icelanders investigating associations between SNPs and 4719 plasma proteins identified an additional seven SNPs associated with circulating SLPI13. While none of these seven SNPs were directly genotyped in MESA, one SNP was imputed (rs7205804). We evaluated the associations of these three previously identified SNPs with HF events in trans-ancestral analyses in MESA participants. We also evaluated the associations of these three previously identified SNPs with serum SLPI levels in ancestry-specific and trans-ancestral analyses in MESA participants. A Bonferroni-corrected P < 0.0166 was considered statistically significant.
Statistical analysis
Demographic and clinical characteristics at baseline examination 2 (2002–2004) were compared by quartile of SLPI using χ2 tests for categorical variables and univariate general linear models for continuous variables. Multivariable Cox proportional hazards regression models were used to evaluate the associations of SLPI with incident HF and its subtypes (HFpEF and HFrEF). We evaluated SLPI as a continuous variable after log base 2 transformation, which can be interpreted as “per doubling.” Exam 2, the time of SLPI measurement, was defined as the time origin for this analysis. The proportionality of hazards assumption was confirmed by Schoenfeld goodness-of-fit procedures. We first assessed the potential nonlinear associations of SLPI and hazard of incident HF using separate restricted cubic splines with 3 knots in Cox proportional hazards regression. We assessed the associations of SLPI as a continuous variable (per doubling) with incident HF and its subtypes. We evaluated the time to first HF subtype event using separate Cox proportion hazards models with censoring on the opposing type. The hazard ratio is interpreted as per one unit on the log base 2 scale of SLPI measurement. For all Cox regression models, covariates were obtained at examination 2, except for eGFR and CRP, which were obtained at examination 1. Model 1 adjusted for age, race, and sex. Model 2 further adjusted for body mass index (BMI), systolic blood pressure, antihypertensive medication treatment, diabetes mellitus, smoking, total cholesterol, and eGFR. Model 3 additionally adjusted for CRP. In sensitivity analysis, we further adjusted for hs-troponin T in addition to Model 3 covariates. We assessed for effect modification of age, sex, smoking status, systolic blood pressure, and CRP on the association of SLPI with incident HF using interaction terms for age (above vs. below median), sex, smoking status (current/former vs. never), systolic blood pressure (above vs. below median), and CRP (above vs. below median). A two‐tailed P < 0.05 was considered statistically significant. Statistical analysis was performed using R version 4.0.2 (Vienna, Austria).
Data availability
The genomic dataset analyzed during the current study are publicly available in the dbGAP repository (Study Accession: phs000209.v13.p3). The ELISA dataset analyzed during the current study are publicly available in the NHLBI’s Biologic Specimen and Data Repository Information Coordinating Center repository (https://biolincc.nhlbi.nih.gov/studies/mesa).
Abbreviations
- CRP:
-
C-reactive protein
- CVD:
-
Cardiovascular disease
- HF:
-
Heart failure
- HFpEF:
-
Heart failure with preserved ejection fraction
- HFrEF:
-
Heart failure with reduced ejection fraction
- MESA:
-
Multi-Ethnic Study of Atherosclerosis
- pQTL:
-
Protein quantitative trait loci
- SLPI:
-
Secretory leukocyte protease inhibitor
- SNP:
-
Single nucleotide polymorphism
References
Willerson, J. T. & Ridker, P. M. Inflammation as a cardiovascular risk factor. Circulation 109, 2–10. https://doi.org/10.1161/01.CIR.0000129535.04194.38 (2004).
Hua, Y. & Nair, S. Proteases in cardiometabolic diseases: Pathophysiology, molecular mechanisms and clinical applications. Biochim. Biophys. Acta 195–208, 2015. https://doi.org/10.1016/j.bbadis.2014.04.032 (1852).
Alibakhshikenari, M. et al. Bandwidth and gain enhancement of composite right left handed metamaterial transmission line planar antenna employing a non foster impedance matching circuit board. Sci. Rep. 11, 7472. https://doi.org/10.1038/s41598-021-86973-x (2021).
Alibakhshikenari, M. et al. Optimum power transfer in RF front end systems using adaptive impedance matching technique. Sci. Rep. 11, 11825. https://doi.org/10.1038/s41598-021-91355-4 (2021).
Alibakhshikenari, M. et al. An innovative antenna array with high inter element isolation for sub-6 GHz 5G MIMO communication systems. Sci. Rep. 12, 7907. https://doi.org/10.1038/s41598-022-12119-2 (2022).
Alibakhshikenari, M. et al. High-isolation antenna array using SIW and realized with a graphene layer for sub-terahertz wireless applications. Sci. Rep. 11, 10218. https://doi.org/10.1038/s41598-021-87712-y (2021).
Fakharian, M. M., Alibakhshikenari, M., See, C. H. & Abd-Alhameed, R. A high gain multiband offset MIMO antenna based on a planar log-periodic array for Ku/K-band applications. Sci. Rep. 12, 4044. https://doi.org/10.1038/s41598-022-07866-1 (2022).
Matsumoto, T. et al. Chymase inhibition prevents cardiac fibrosis and improves diastolic dysfunction in the progression of heart failure. Circulation 107, 2555–2558. https://doi.org/10.1161/01.CIR.0000074041.81728.79 (2003).
Zhang, Y., DeWitt, D. L., McNeely, T. B., Wahl, S. M. & Wahl, L. M. Secretory leukocyte protease inhibitor suppresses the production of monocyte prostaglandin H synthase-2, prostaglandin E2, and matrix metalloproteinases. J. Clin. Invest. 99, 894–900. https://doi.org/10.1172/JCI119254 (1997).
Jin, F. Y., Nathan, C., Radzioch, D. & Ding, A. Secretory leukocyte protease inhibitor: A macrophage product induced by and antagonistic to bacterial lipopolysaccharide. Cell 88, 417–426. https://doi.org/10.1016/s0092-8674(00)81880-2 (1997).
Doumas, S., Kolokotronis, A. & Stefanopoulos, P. Anti-inflammatory and antimicrobial roles of secretory leukocyte protease inhibitor. Infect. Immun. 73, 1271–1274. https://doi.org/10.1128/IAI.73.3.1271-1274.2005 (2005).
Suhre, K. et al. Connecting genetic risk to disease end points through the human blood plasma proteome. Nat. Commun. 8, 14357. https://doi.org/10.1038/ncomms14357 (2017).
Ferkingstad, E. et al. Large-scale integration of the plasma proteome with genetics and disease. Nat. Genet. 53, 1712–1721. https://doi.org/10.1038/s41588-021-00978-w (2021).
Berardi, C. et al. Elevated levels of adhesion proteins are associated with low ankle-brachial index. Angiology 68, 322–329. https://doi.org/10.1177/0003319716659178 (2017).
Mendez, I. J. et al. Adhesion pathway proteins and risk of atrial fibrillation in the multi-ethnic study of atherosclerosis. BMC Cardiovasc. Disord. 21, 436. https://doi.org/10.1186/s12872-021-02241-w (2021).
Xu, W. et al. Epithelial cells trigger frontline immunoglobulin class switching through a pathway regulated by the inhibitor SLPI. Nat. Immunol. 8, 294–303. https://doi.org/10.1038/ni1434 (2007).
Ashcroft, G. S. et al. Secretory leukocyte protease inhibitor mediates non-redundant functions necessary for normal wound healing. Nat. Med. 6, 1147–1153. https://doi.org/10.1038/80489 (2000).
Bonds, R. S. & Midoro-Horiuti, T. Estrogen effects in allergy and asthma. Curr. Opin. Allergy Clin. Immunol. 13, 92–99. https://doi.org/10.1097/ACI.0b013e32835a6dd6 (2013).
Meyer, M. et al. Regulation and activity of secretory leukoprotease inhibitor (SLPI) is altered in smokers. Am. J. Physiol. Lung Cell Mol. Physiol. 306, L269-276. https://doi.org/10.1152/ajplung.00290.2013 (2014).
Wilson, C., Heads, A., Shenkin, A. & Imrie, C. W. C-reactive protein, antiproteases and complement factors as objective markers of severity in acute pancreatitis. Br. J. Surg. 76, 177–181. https://doi.org/10.1002/bjs.1800760224 (1989).
Braunwald, E. Biomarkers in heart failure. N. Engl. J. Med. 358, 2148–2159. https://doi.org/10.1056/NEJMra0800239 (2008).
van Wetering, S. et al. Regulation of SLPI and elafin release from bronchial epithelial cells by neutrophil defensins. Am. J. Physiol. Lung Cell Mol. Physiol. 278, L51-58. https://doi.org/10.1152/ajplung.2000.278.1.L51 (2000).
de Boer, R. A. et al. Association of cardiovascular biomarkers with incident heart failure with preserved and reduced ejection fraction. JAMA Cardiol. 3, 215–224. https://doi.org/10.1001/jamacardio.2017.4987 (2018).
Chirinos, J. A. et al. Multiple plasma biomarkers for risk stratification in patients with heart failure and preserved ejection fraction. J. Am. Coll. Cardiol. 75, 1281–1295. https://doi.org/10.1016/j.jacc.2019.12.069 (2020).
Carnes, J. & Gordon, G. Biomarkers in heart failure with preserved ejection fraction: an update on progress and future challenges. Heart Lung Circ. 29, 62–68. https://doi.org/10.1016/j.hlc.2019.05.180 (2020).
Duprez, D. A. et al. Predictive value of collagen biomarkers for heart failure with and without preserved ejection fraction: MESA (multi-ethnic study of atherosclerosis). J. Am. Heart Assoc. https://doi.org/10.1161/JAHA.117.007885 (2018).
Jang, S. et al. Association of the novel inflammatory marker GlycA and incident heart failure and its subtypes of preserved and reduced ejection fraction: The multi-ethnic study of atherosclerosis. Circ. Heart Fail. 13, e007067. https://doi.org/10.1161/CIRCHEARTFAILURE.120.007067 (2020).
Watson, C. J. et al. Biomarker profiling for risk of future heart failure (HFpEF) development. J. Transl. Med. 19, 61. https://doi.org/10.1186/s12967-021-02735-3 (2021).
Simmonds, S. J., Cuijpers, I., Heymans, S. & Jones, E. A. V. Cellular and Molecular differences between HFpEF and HFrEF: A step ahead in an improved pathological understanding. Cells https://doi.org/10.3390/cells9010242 (2020).
Sanders-van Wijk, S. et al. Proteomic evaluation of the comorbidity-inflammation paradigm in heart failure with preserved ejection fraction: Results from the PROMIS-HFPEF study. Circulation 142, 2029–2044. https://doi.org/10.1161/CIRCULATIONAHA.120.045810 (2020).
Prompunt, E., Nernpermpisooth, N., Sanit, J. & Kumphune, S. Overexpression and pre-treatment of recombinant human secretory leukocyte protease inhibitor (rhSLPI) reduces an in vitro ischemia/reperfusion injury in rat cardiac myoblast (H9c2) cell. Biomol. Concepts 9, 17–32. https://doi.org/10.1515/bmc-2018-0004 (2018).
Schneeberger, S. et al. The effect of secretory leukocyte protease inhibitor (SLPI) on ischemia/reperfusion injury in cardiac transplantation. Am. J. Transplant. 8, 773–782. https://doi.org/10.1111/j.1600-6143.2008.02158.x (2008).
Majchrzak-Gorecka, M., Majewski, P., Grygier, B., Murzyn, K. & Cichy, J. Secretory leukocyte protease inhibitor (SLPI), a multifunctional protein in the host defense response. Cytokine Growth Factor Rev. 28, 79–93. https://doi.org/10.1016/j.cytogfr.2015.12.001 (2016).
Persson, L. J. et al. Antimicrobial peptide levels are linked to airway inflammation, bacterial colonisation and exacerbations in chronic obstructive pulmonary disease. Eur. Respir. J. 49, 1601328. https://doi.org/10.1183/13993003.01328-2016 (2017).
Lentsch, A. B. et al. Inhibition of NF-kappaB activation and augmentation of IkappaBbeta by secretory leukocyte protease inhibitor during lung inflammation. Am. J. Pathol. 154, 239–247. https://doi.org/10.1016/s0002-9440(10)65270-4 (1999).
Bild, D. E. et al. Multi-ethnic study of atherosclerosis: objectives and design. Am. J. Epidemiol. 156, 871–881. https://doi.org/10.1093/aje/kwf113 (2002).
Christoph, M. J. et al. Impact of adiposity on cellular adhesion: The multi-ethnic study of atherosclerosis (MESA). Obesity 24, 223–230. https://doi.org/10.1002/oby.21245 (2016).
Marchini, J., Howie, B., Myers, S., McVean, G. & Donnelly, P. A new multipoint method for genome-wide association studies by imputation of genotypes. Nat. Genet. 39, 906–913. https://doi.org/10.1038/ng2088 (2007).
Acknowledgements
MESA and the MESA SHARe project are conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with MESA investigators. Support for MESA is provided by Contracts 75N92020D00001, HHSN268201500003I, N01-HC-95159, 75N92020D00005, N01-HC-95160, 75N92020D00002, N01-HC-95161, 75N92020D00003, N01-HC-95162, 75N92020D00006, N01-HC-95163, 75N92020D00004, N01-HC-95164, 75N92020D00007, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168, N01-HC-95169, UL1-TR-000040, UL1-TR-001079, UL1-TR-001420, UL1-TR-001881, and DK063491. Funding for SHARe genotyping was provided by NHLBI Contract N02-HL-64278. Genotyping was performed at Affymetrix (Santa Clara, California, USA) and the Broad Institute of Harvard and MIT (Boston, Massachusetts, USA) using the Affymetrix Genome-Wide Human SNP Array 6.0. The MESA CARe data used for the analyses described in this manuscript were obtained through Genetics (accession numbers). Funding for CARe genotyping was provided by NHLBI Contract N01-HC-65226. We would like to thank the other investigators, the staff, and the participants of the MESA for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Funding
This research was supported by T32-HL069771, KL2-TR001424, UL1‐TR‐000040, UL1‐TR‐001079, and UL1‐TR‐001420 from the National Institutes of Health. Funding for adhesion protein levels was supported by R01HL98077 from the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
K.T.S. contributed to the conceptualization, data curation, formal analysis, validation, investigation, methodology, and writing of the manuscript. D.R.N. contributed to the data curation, formal analysis, validation, investigation, and methodology of the manuscript. S.J.B., N.B.L., D.L.J., B.P., K.D.T., S.J.S., L.R.T., J.T.W., and E.M.M. contributed to the critical review and editing of the manuscript. R.B.P. contributed to the conceptualization, supervision, funding acquisition, data curation, formal analysis, and critical review and editing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sawicki, K.T., Nannini, D.R., Bielinski, S.J. et al. Secretory leukocyte protease inhibitor and risk of heart failure in the Multi-Ethnic Study of Atherosclerosis. Sci Rep 13, 604 (2023). https://doi.org/10.1038/s41598-023-27679-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-27679-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.