Abstract
Chronic cheilitis (CC) is a spectrum of inflammatory changes of unknown etiology that affect the vermilion of the lips. This study aimed to describe the epidemiology, clinical presentations and risk factors of CC. Patients with CC were recruited from the National Clinical Research Center for Oral Disease of China. A convenience sample of inhabitants who live in the same geographical region were recruited as the control group. The lip skin transepidermal water loss (TEWL) and capacitance of CC patients were compared with that of age- and gender-matched controls. Our results demonstrated that of the 109 patients with CC, 72 (66.1%; 95% CI: 57.0–75.1%) were female. The common clinical presentations of CC consisted of desquamation (n = 99; 90.8%), and/or chapping (n = 81; 74.3%), and/or pruritus (n = 64; 58.7%). Multivariable analysis showed that allergic dermatologic diseases (P < 0.001; OR: 4.5; 95% CI: 2.4–8.4), anemia (P = 0.001; OR: 3.3; 95% CI: 1.5–7.5), and indoor/outdoor alternate working environment (P < 0.001; OR: 2.1; 95% CI: 1.5–2.8) were the significant risk factors for CC. The mean lip skin TEWL was found to be significantly higher, while the capacitance was lower in CC patients compared to that of control individuals. This study provides insights into the etiopathogenesis of CC and may help clinicians to identify the most effective management strategies.
Similar content being viewed by others
Introduction
Chronic cheilitis (CC) involves a spectrum of inflammatory changes of unknown etiology that affect the vermilion of the lips. CC has various manifestations and may present with desquamation, pruritus, chapping, or effusion. As a transitional zone between skin and mucosa, the vermilion of the lips comprises a thin stratum corneum that is devoid of both underlying salivary and sebaceous glands1. External etiological factors, such as windy and cold weather, lip licking or biting may promote dehydration of the lips, making the vermilion of the lips appear similar to CC. In addition, desquamation, pruritus or effusion may also appear as signs of other oral mucosal diseases such as oral lichen planus, orofacial granulomatosis, herpes, and oral candidiasis, which may lead to confusion in differential diagnosis CC from these conditions.
Due to the lack of a widely accepted diagnostic classification system, CC is often named after the characteristic signs and symptoms, for example, chapped lips, exfoliative cheilitis, cheilitis simplex, common cheilitis, cheilitis sicca, lip-licking cheilitis, angular cheilitis, irritant cheilitis, allergic contact cheilitis, and atopic cheilitis, etc2,3,4,5,6. The epidemiology, clinical presentations and skin barrier function of CC are poorly understood. In this study, we investigated the clinical characteristics of CC, defined the risk factors associated with CC, and assessed the skin barrier function of CC patients using a case–control study design that allowed exclusion of some confounding factors.
Methods
Study population
We recruited 109 patients with CC via the Department of Oral Medicine between December 2018 and June 2019. Migration to different geographic locations may lead to changes in the environment (including humidity, ultraviolet intensity, temperature, etc.), which might affect the risk and severity of CC. Therefore, the survey was conducted among residents who lived in Xi’an city (Longitude: 108, latitude: 34), located in central China, with an average temperature of 14.7 °C (± 14.65 °C), approximately 90 sunny days per year and semi-humid climate.
The diagnosis of CC was based on the history and clinical findings of crusting, scaling, peeling or chapping of one or both lips that had been present for at least 8 weeks, excluding the cases related to mechanical stimuli. As several variants of CC may be present at different time in the same patient, we made a unified diagnosis of chronic cheilitis, no longer distinguished chapped lips, exfoliative cheilitis, cheilitis simplex, common cheilitis, cheilitis sicca, allergic contact cheilitis, and atopic cheilitis. A biopsy is necessary for further histologic assessment to exclude granulomatous cheilitis, cheilitis glandularis, actinic cheilitis and other associated diseases, details of the diagnostic criteria used are described in Table 1.
Control individuals were a convenience sample of community-dwelling individuals, who live in the same geographical region, or other patients visiting the Stomatological Hospital of the Fourth Military Medical University (FMMU) for routine dental exams (n = 208). Proportional gender and age matching were used to select controls for the measurement of skin barrier function, and the controls must not have signs and symptoms of CC.
Variables
Details of the demographics and medical history were collected through questionnaire. The medical histories of their skin problems and previous dermatological diagnoses were further evaluated by qualified dermatologists. Hematological data within one year were collected in participants as they were required: (1) for medical diagnostic purposes; (2) for routine examination; (3) to monitor therapeutic outcomes. For those with a confirmed diagnosis of CC, the data, including the duration of CC, presented symptoms, involved sites, and aggravating factors were recorded.
Measurements
Passive diffusion of water through the stratum corneum, also known as transepidermal water loss (TEWL), and capacitance, which reflects water content of stratum corneum are widely applied for evaluating the skin barrier function7,8. Measurement of TEWL and capacitance allows objective assessment of the functional status of the skin barrier9,10. In this study TEWL was measured with TewameterTM300 (Courage Khazaka, Germany). Capacitance was measured using the CorneometerCM825 (Courage Khazaka, Germany).
Lip measurements were performed on the lower lip vermilion, while the skin measurements were performed on the forearm. The participants applied no topical agents on their lips and skin for at least 12 h. Before the measurement, the lips of the patients were wiped using paper towels and acclimated for 30 min in the testing room. All measurements were conducted in an environment with a temperature of 22–27 °C and relative humidity of 45–50%. Control data of TEWL and capacitance were obtained from the control population by matching the patients at a ratio of 1:1 based on age and sex.
Statistical analysis
The data obtained were recorded and processed using SAS 9.4 software (SAS Institute, Cary, NC, USA). Categorical and continuous variables were compared using χ2, Fisher's exact, and t-tests, respectively. Logistic regression modeling was used to evaluate the risk factors. The interaction terms for statistically significant effect modifiers were added to the multivariate model while calculating appropriate odds ratio (OR) and 95% confidence intervals (CI). Two-sided P < 0.05 was considered statistically significant.
Ethics approval
The study protocol was reviewed and approved by the Ethics Committee of School of Stomatology, the Fourth Military Medical University (IRB number: IRB-REV-2020041). The study was carried out in accordance with the ethical standards of Helsinki Declaration and its amendments or comparable ethical standards.
Informed consent
Before starting the study, the participants were informed about the study and signed informed consent forms. The participants and any identifiable individuals consented to publication of his/her image.
Results
Demographic details of CC patients
Our study included 109 CC patients, whose median age (and range) was 27 years (5–59 years). Of the 109, 72 (66.1%; 95% CI: 57.0–75.1%) were female, with a peak in the incidence rate seen during the third and fourth decade of their life. The median age (and range) for females was 29 years (5–59 years), and for males was 26 years (8–56 years). The duration of symptoms before definitive diagnosis was over 1 year for the majority of CC patients (76.1%; 95% CI: 68.0–84.3%).
Clinical presentations of CC
Both lips were affected in 103 (94.5%; 95% CI: 90.1–98.8%) patients. Five patients had CC on the lower lip only and one patient on the upper lip only. CC displays a spectrum of clinical manifestations (Fig. 1), common clinical presentations consisted of desquamation (n = 99; 90.8%) and/or chapping (n = 81; 74.3%) and/or pruritus (n = 64; 58.7%). Additional details about the range and frequency of the presented symptoms are provided in Table 2.
For the nine surveyed factors, dryness was the most frequent aggravating factor (66.1%), followed by spicy food (53.2%), seasonal variation (49.5%), cosmetics (38.5%), and cold environment (31.2%) (Table 2).
Risk factors for CC
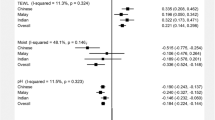
In the univariate analysis, gender, occupation, skin disease, and anemia showed odds ratios (ORs) with a significance of P < 0.05, which were entered into the multivariable analysis (Table 3). The final multivariable model demonstrated that skin disease (P < 0.001; OR: 4.5; 95% CI: 2.4–8.4), anemia (P = 0.001; OR: 3.3; 95% CI: 1.5–7.5), and indoor/outdoor alternate working environment (P < 0.001; OR: 2.1; 95% CI: 1.5–2.8) were the significant risk factors for CC (Table 3). Of the 20 CC patients with anemia, 19 (95.0%; 95% CI: 84.5–105.5%) had iron deficiency anemia and one (5.0%; 95% CI: 0–15.5%) had megaloblastic anemia. Among the total 39 CC patients with skin diseases, 16 (41.0%; 95% CI: 24.9–57.2%) had a history of urticaria, 14 (35.9%; 95% CI: 20.1–51.7%) had atopic dermatitis (AD) or eczema, and 9 patients (23.1%; 95% CI: 9.2–36.9%) had allergic contact dermatitis (ACD).
The skin barrier function of CC patients
Thirty-seven CC patients and 37 control individuals (23 female, 14 male, 28 ± 7 years vs. 27 ± 7 years; P > 0.05) had participated in the biophysical measurements in the lip and forearm skin. The TEWL and capacitance values of lip in the CC group were distributed with a mean of 66.8 g/m2·h (± 20.9 g/m2·h) and 31.0 AU (± 15.2 AU). Compared to the TEWL and capacitance values of the lip in the age and gender-matched control group, the TEWL value of the lip was significantly higher (P < 0.01) in the CC group, while the capacitance value was found to be significantly lower (P < 0.001) (Fig. 2). The TEWL and capacitance values of arm skin showed no significant differences between the two groups.
The biophysical parameter values in chronic cheilitis patients. (A) TEWL values in the lip and forearm of CC patients and control individuals, (B) capacitance values in the lip and forearm of CC patients and control individuals. CC chronic cheilitis, TEWL transepidermal water loss; **P < 0.01, ***P < 0.001.
Discussion
The data from our study of 109 CC patients showed that CC primarily affected young patients (mean age of 27 years), wherein two-thirds were female, with 94.5% of them showing involvement of both lips. Desquamation, chapping, and pruritus were the most frequently presented symptoms, however the chronic course of CC was more likely to be dynamically diverse, with the severity and distribution of CC lesions influenced by environmental factors, particularly dryness, food, and cosmetics.
Dryness was shown to be an important aggravating factor for CC in the study, which was also reflected in the influence of seasonal variation and occupation. Table 3 shows that the occupation that involved frequent indoor/outdoor environmental transition was significantly related to CC. CC patients emphasized that moving from outside to a warm room during winter had an aggravating effect on CC, which may attribute to the dramatically reduced humidity in air upon heating11. It is noted, our study showed that the population with a history of allergic dermatologic diseases including urticaria, AD and ACD, was at increased risk for CC occurrence. Likewise, previous studies demonstrated that dryness was correlated well with the severity of AD and ACD12,13 as a result of significant decrease in the skin barrier function14, which further highlight the close relationship between CC and allergic dermatologic disease. In agreement with this, a recent cross-sectional study which examined the multiple factors involved in the aetiology of CC showed that of the systemic diseases recorded among CC patients, skin diseases were noticed most frequently although the type of skin disease was not described in detail15. Another study, which investigated the prevalence of hypersensitivity in cheilitis patients demonstrated increased serum total IgE level and positive food-specific IgG in cheilitis patients compared to the healthy control16.
Previously, atopic cheilitis manifesting as exfoliative cheilitis was described in cases of AD17, some cheilitis cases (known as allergic cheilitis) were regarded as an allergic contact eczema of the lips in reaction to an exogenous substance5,18. However, the association between CC and dermatologic disease has not yet been validated in CC patients. In the current case–control study, allergic dermatologic disease (OR: 4.5; 95% CI: 2.4–8.4) was confirmed as a potential risk factor for occurrence of CC. We found that urticaria was the most frequent (41.0%) dermatologic disease associated with CC, followed by AD/eczema (35.9%) and ACD (23.1%).
AD, urticaria, and ACD represent three important allergic dermatologic diseases, the pathogenesis of them is not completely understood. Studies emphasized Th2 cytokines as the primary stimuli for the “atopy” of AD19, and that ACD is a type IV cutaneous cell-mediated hypersensitivity reaction triggered by environmental allergens20, whereas urticaria is an IgE-mediated allergic dermatologic disease21. However, their pathophysiology is likely multifactorial, and an intricate relationship exists among these diseases, which involves immune, skin barrier and environmental factors22,23,24. ACD is often included in the differential diagnosis for AD as they can be similar in their clinical presentations, and AD was considered an important risk factor for the occurrence of urticaria25. Among inflammatory mediators of urticaria, some are also implicated in the pathogenesis of AD26.
Skin barrier dysfunction plays a crucial role in the pathogenesis of AD27. Moreover, studies have shown that an increased skin permeability induced by an impaired skin barrier could provide an opportunity to effectively access the allergens in the viable epidermis. This evokes innate signaling pathways during the sensitization phase, which is required for the activation of the immune response. Thus, skin barrier dysfunction enhances the acquisition of allergic dermatologic diseases28,29,30,31,32. We measured TEWL and capacitance in the lower lip and forearm skin, and found that compared to the TEWL and capacitance of lip in the control group, TEWL in the CC group was significantly higher while the capacitance was significantly lower, indicating an impaired skin barrier function in the lip of the CC patients. These findings were consistent with the observations made in the skin lesions of AD and ACD patients33,34. However, the TEWL and capacitance of arm skin showed no significant differences between the two groups. Hence, the possibility that the defective skin barrier function of the lip is mediated by the inflammatory reaction cannot be excluded35. The mechanism associated with this phenomenon warrants further investigation.
The association between atopic disorders (ie, asthma, eczema and food allergy) and anemia was reported previously. From a survey that included 207,007 children and adolescents in US, atopic disorders were shown to be associated with increased odds of anemia, and the odds of anemia increased with the number of atopic disorders present36. Nevertheless, there is a paucity of data explaining such association. A recent study using animal model demonstrated anemia was associated with decreased epithelial barrier function due to down-regulation of tight junction proteins37, which is in agreement with the survey and our study. But our findings still indicate a need for careful evaluation of the implications of anemia in CC.
In summary, use of case definition to improve diagnostic specificity yielded consistent results, allowing us to study the risk factors for CC. To our knowledge, this is the first study to examine the skin barrier function of CC patients, which increases our understating of the disease. This study also has limitations. The positive association of CC with allergic dermatologic diseases was confirmed in the case–control study, however patch test, biopsy or serum cytokine test were not performed for most of the patients, and more detailed data were not collected, which might demonstrate additional systematic risk factors linked to CC.
Conclusion
The morbidity of CC is closely associated with allergic dermatologic diseases, and the lip lesion of CC is characterized by impaired skin barrier function. The study provides insight into the etiopathogenesis of CC and may help clinicians to identify the most effective management strategies.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Rogers, R. S. 3rd. & Bekic, M. Diseases of the lips. Semin. Cutan. Med. Surg. 16, 328–336 (1997).
Lugovic-Mihic, L. et al. Diagnostic management of cheilitis: An approach based on a recent proposal for cheilitis classification. Acta Dermatovenerol. Alp. Pannonica Adriat. 29, 67–72 (2020).
Van Baelen, A., Kerre, S. & Goossens, A. Allergic contact cheilitis and hand dermatitis caused by a toothpaste. Contact Dermatitis 74, 187–189 (2016).
Agar, N. & Freeman, S. Cheilitis caused by contact allergy to cocamidopropyl betaine in “2-in-1 toothpaste and mouthwash”. Australas J. Dermatol. 46, 15–17 (2005).
HitzLindenmuller, I., Itin, P. H. & Fistarol, S. K. Dermatology of the lips: Inflammatory diseases. Quintessence Int. 45, 875–883 (2014).
Lugovic-Mihic, L., Pilipovic, K., Crnaric, I., Situm, M. & Duvancic, T. Differential diagnosis of cheilitis—How to classify cheilitis?. Acta Clin. Croat. 57, 342–351 (2018).
Cork, M. J. et al. Epidermal barrier dysfunction in atopic dermatitis. J. Invest. Dermatol. 129, 1892–1908 (2009).
Berardesca, E. EEMCO guidance for the assessment of stratum corneum hydration: Electrical methods. Skin Res. Technol. 3, 126–132 (1997).
Montero-Vilchez, T. et al. Skin barrier function in psoriasis and atopic dermatitis: Transepidermal water loss and temperature as useful tools to assess disease severity. J. Clin. Med. 10, 359 (2021).
Schmitt, J. et al. Assessment of clinical signs of atopic dermatitis: A systematic review and recommendation. J. Allergy Clin. Immunol. 132, 1337–1347 (2013).
Uter, W., Gefeller, O. & Schwanitz, H. J. An epidemiological study of the influence of season (cold and dry air) on the occurrence of irritant skin changes of the hands. Br. J. Dermatol. 138, 266–272 (1998).
Sato, J., Denda, M., Nakanishi, J. & Koyama, J. Dry condition affects desquamation of stratum corneum in vivo. J. Dermatol. Sci. 18, 163–169 (1998).
Denda, M., Sato, J., Tsuchiya, T., Elias, P. M. & Feingold, K. R. Low humidity stimulates epidermal DNA synthesis and amplifies the hyperproliferative response to barrier disruption: Implication for seasonal exacerbations of inflammatory dermatoses. J. Invest. Dermatol. 111, 873–878 (1998).
Engebretsen, K. A., Johansen, J. D., Kezic, S., Linneberg, A. & Thyssen, J. P. The effect of environmental humidity and temperature on skin barrier function and dermatitis. J. Eur. Acad. Dermatol. Venereol. 30, 223–249 (2016).
Blagec, T. et al. Cheilitis: A cross-sectional study-multiple factors involved in the aetiology and clinical features. Oral Dis. https://doi.org/10.1111/odi.14359 (2022).
Cai, L. et al. Predisposition of hypersensitivity in patients with exfoliative cheilitis. J. Dent. Sci. 17, 476–481 (2022).
De, D., Kanwar, A. J. & Handa, S. Comparative efficacy of Hanifin and Rajka’s criteria and the UK working party’s diagnostic criteria in diagnosis of atopic dermatitis in a hospital setting in North India. J. Eur. Acad. Dermatol. Venereol. 20, 853–859 (2006).
Lim, J. T., Ng, S. K. & Goh, C. L. Contact cheilitis in Singapore. Contact Dermatitis 27, 263–264 (1992).
Furue, M. et al. Atopic dermatitis: Immune deviation, barrier dysfunction, IgE autoreactivity and new therapies. Allergol. Int. 66, 398–403 (2017).
Krasteva, M. et al. Dual role of dendritic cells in the induction and down-regulation of antigen-specific cutaneous inflammation. J. Immunol. 160, 1181–1190 (1998).
Zuberbier, T. et al. The EAACI/GA(2)LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy 73, 1393–1414 (2018).
Long, H., Zhang, G., Wang, L. & Lu, Q. Eosinophilic skin diseases: A comprehensive review. Clin. Rev. Allergy Immunol. 50, 189–213 (2016).
Gaudinski, M. R. & Milner, J. D. Atopic dermatitis and allergic urticaria: Cutaneous manifestations of immunodeficiency. Immunol. Allergy Clin. N. Am. 37, 1–10 (2017).
Ferrucci, S., Benzecry, V., Berti, E. & Asero, R. Rapid disappearance of both severe atopic dermatitis and cold urticaria following dupilumab treatment. Clin. Exp. Dermatol. 45, 345–346 (2020).
Kitsioulis, N. A. et al. Assessment of atopic dermatitis as a risk factor for chronic spontaneous urticaria in a pediatric population. Allergy Asthma Proc. 39, 445–448 (2018).
Kaplan, A. P., Horakova, Z. & Katz, S. I. Assessment of tissue fluid histamine levels in patients with urticaria. J. Allergy Clin. Immunol. 61, 350–354 (1978).
Peng, W. & Novak, N. Pathogenesis of atopic dermatitis. Clin. Exp. Allergy 45, 566–574 (2015).
Bilimoria, S. N. & Lio, P. A. Biologics for allergic dermatologic diseases. Curr. Allergy Asthma Rep. 20, 35 (2020).
Jensen, J. M. & Proksch, E. The skin’s barrier. G. Ital. Dermatol. Venereol. 144, 689–700 (2009).
Jakasa, I., Thyssen, J. P. & Kezic, S. The role of skin barrier in occupational contact dermatitis. Exp. Dermatol. 27, 909–914 (2018).
Kasemsarn, P., Bosco, J. & Nixon, R. L. The role of the skin barrier in occupational skin diseases. Curr. Probl. Dermatol. 49, 135–143 (2016).
Thyssen, J. P., McFadden, J. P. & Kimber, I. The multiple factors affecting the association between atopic dermatitis and contact sensitization. Allergy 69, 28–36 (2014).
Polanska, A. et al. Nonlesional skin in atopic dermatitis is seemingly healthy skin—Observations using noninvasive methods. Wideochir. Inne Tech. Maloinwazyjne 8, 192–199 (2013).
Laudanska, H., Reduta, T. & Szmitkowska, D. Evaluation of skin barrier function in allergic contact dermatitis and atopic dermatitis using method of the continuous TEWL measurement. Rocz Akad. Med. Bialymst 48, 123–127 (2003).
Gschwandtner, M. et al. Histamine suppresses epidermal keratinocyte differentiation and impairs skin barrier function in a human skin model. Allergy 68, 37–47 (2013).
Drury, K. E., Schaeffer, M. & Silverberg, J. I. Association between atopic disease and anemia in US children. JAMA Pediatr. 170, 29–34 (2016).
MohanKumar, K. et al. Severe neonatal anemia increases intestinal permeability by disrupting epithelial adherens junctions. Am. J. Physiol. Gastrointest. Liver Physiol. 318, G705–G716 (2020).
Acknowledgements
We would like to thank Professor Hua Ge for her precious suggestion on dermatology, clinical data analyses and comments on the work. This work was supported by grants from the State Key Laboratory of Military Stomatology (2018ZB01).
Funding
This work were supported by the National Clinical Research Center for Oral Disease of China (Grant No. LCA202008) and the State Key Laboratory of Military Stomatology (Grant No. 2018ZB01).
Author information
Authors and Affiliations
Contributions
Y.Y.W. and L.Q.L. drafted the manuscript. X.W.W. designed the study and edited the manuscript. L.Q.L., Y.Y.W. and X.W.W. performed the statistical analysis. R.Y. performed the statistical analysis and edited the manuscript. Y.H.W., M.H.W., J.W. and Y.C. collected the data and contributed to the analysis of the results. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Y., Lin, L., Wang, Y. et al. Analysis of clinical presentations, lip transepidermal water loss and associated dermatological conditions in patients with chronic cheilitis. Sci Rep 12, 22497 (2022). https://doi.org/10.1038/s41598-022-27115-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-27115-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.