Abstract
Common etiologies between age-related macular degeneration (AMD) and kidney disease advocate a close link between AMD and end-stage renal disease (ESRD). However, the risk of ESRD in people with AMD was not reported. Here, we investigated the association between AMD and the risk of ESRD by using a nationwide, population-based cohort data in Korea. 4,206,862 participants aged 50 years or older were categorized by presence of AMD and visual disability. Risk of ESRD was the primary outcome. Cox regression hazard model was used to examine the hazard ratios (HRs) with adjustment for potential confounders. Stratified analyses by age, sex, baseline kidney function, and cardiometabolic comorbidities were performed. During the mean 9.95 years of follow-up, there were 21,759 incident ESRD events (0.52%). AMD was associated with 33% increased risk of ESRD (adjusted HR [aHR] 1.33, 95% confidence interval [CI] 1.24–1.44), and the risk was even higher when accompanied by visual disability (aHR 2.05, 95% CI 1.68–2.50) than when not (aHR 1.26, 95% CI 1.17–1.37). Age, baseline kidney function, and cardiometabolic comorbidities significantly interact between AMD and the risk of ESRD. Our findings have clinical implications on disease prevention and risk factor management of ESRD in patients with AMD.
Similar content being viewed by others
Introduction
End-stage renal disease (ESRD) is a significant public health problem. The worldwide number of patients who required renal replacement therapy (RRT) was 2·61 million in 2010 and is estimated to increase to 5·43 million in 20301. RRT is expensive, and easy access to healthcare facility is demanded for people who requires RRT. In addition, patients with ESRD show a higher mortality than the general population2.
Age-related macular degeneration (AMD) is a progressive and degenerative retinal disease that can influence central vision3. It is the leading cause of visual disability in developed countries, and the number of individuals with AMD worldwide is expected to reach 288 million by 20404. Therefore, addressing the comorbid conditions and health problems in AMD population is highlighted.
From earlier epidemiologic findings of AMD studies (the Blue Mountains Eye study5, Beaver Dam Eye Study6, and the US NHANES III7), and more recent investigation of genetic polymorphisms in complement factor H (CFH)8,9,10,11, emerging evidence has suggested an association between renal impairment and AMD (Supplementary Table S1). The common etiologies between chronic kidney disease (CKD) and AMD, including cardiometabolic risk factors (age, smoking, hypertension, and dyslipidemia12,13,14,15,16,17,18,19), pathogenic mechanisms (atherosclerosis, inflammation, and oxidative stress20) and similar structural, and genetic pathways between kidney and eye21,22, advocate a close link between AMD and CKD.
While most epidemiologic studies have established the association between CKD and the risk of AMD, to our best knowledge, the association between AMD and the risk of ESRD was not reported. In addition, the presence of visual disability was not considered in previous studies on the association of AMD and ESRD. Globally, the number of people with blind or with moderate to severe visual impairment caused by macular disease is approximately 2.1 million23. Visual disability is associated with broad range of chronic conditions, including cardiometabolic, neuropsychiatric, and musculoskeletal disorders24,25,26. Therefore, we conducted a retrospective, nationwide, population-based cohort study to investigate the risk of ESRD in patients with AMD, considering the visual disability status.
Results
Baseline characteristics
Of the total 4,206,862 participants enrolled in the final analysis, 53,617 participants (1.27%) had AMD at baseline, and 3858 participants (7.20% of the AMD group) had visual disability. The descriptive characteristics of the study population, classified by the presence of AMD and further by visual disability, are summarized in Table 1.
At baseline, the AMD group was older with a high proportion of women and non-smokers than non-AMD group, or participants without AMD; the average age at baseline was 67.4 ± 8.4 years, 42.5% were men and 10.8% were current smokers. The AMD group had a higher prevalence of hypertension, diabetes mellitus, and dyslipidemia, but lower levels of eGFR and hemoglobin than the non-AMD group (all P < 0.001). At baseline, the AMD with visual disability group was older with a higher proportion of men and current smokers than AMD without visual disability group; the average age at baseline was 67.9 ± 8.3 years, 48.1% were men, and 12.8% were current smoker. The AMD with visual disability group had a lower prevalence of hypertension, and dyslipidemia than the AMD without visual disability group (all P < 0.001).
Incidence of ESRD by the presence of AMD and visual disability
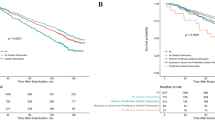
During the mean 9.95 years of follow-up, there were 21,759 (0.52%) incident ESRD events. AMD was associated with a 33% increased risk of ESRD (aHR 1.33, 95% CI 1.24–1.44, P < 0.001). Further analysis that specified AMD by visual disability status demonstrated a 1.26-fold higher risk of ESRD in AMD without visual disability (aHR 1.26, 95% CI 1.17–1.37) and 2.05-fold higher risk of ESRD in AMD with visual disability (aHR 2.05, 95% CI 1.68–2.50). In addition, there was a significant trend in the risk of ESRD among non-AMD, AMD without visual disability, and AMD with visual disability groups (P for trend < 0.001) (Table 2 and Fig. 1).
Kaplan–Meier curves displaying the estimated incidence probability of ESRD according to the presence of AMD, and VD. Kaplan–Meier analysis estimated an increased risk of ESRD in people with AMD (A); In addition, compared to non-AMD group, an increased risk of ESRD among the AMD without VD group, and an even higher risk of ESRD among the AMD and VD group were observed (B). AMD, age-related macular degeneration; VD, visual disability.
Stratified analysis
In stratified analyses according to age, sex, and comorbidity (any of hypertension, diabetes mellitus, or dyslipidemia), the AMD with visual disability group had a markedly higher risk of developing ESRD than controls (Table 3). In addition, the impact of AMD with visual disability on developing ESRD was more prominent among individuals aged 50–64 than those aged 75 or older (aHR 3.17 vs. 1.62; P for interaction < 0.001) among individuals with eGFR of same or above 60 mL/min/1.73 m2 than eGFR of less than 30 mL/min/1.73 m2 (aHR 2.62 vs. 1.63; P for interaction < 0.001) and among individuals without comorbidity than those with comorbidity (aHR 5.08 vs. 1.96; P for interaction < 0.001).
Discussion
To our best knowledge, this is the first large-scale nationwide study to establish that AMD was associated with a higher risk of ESRD, after considering various factors including age, sex, BMI, lifestyle behaviors (smoking, alcohol consumption, physical activity), and comorbidities (hypertension, diabetes mellitus, dyslipidemia). Notably, the risk was even higher for AMD patients with visual disability, reaching a nearly two-fold risk. This effect was noticeable in individuals 50–64 years old, individuals with eGFR ≥ 60 mL/min/1.73 m2, and those without cardiometabolic comorbidities.
Findings from numerous previous epidemiologic studies have suggested the association between renal impairment and AMD5,6,7,27,28,29,30,31. As no previous studies have examined the risk of ESRD in people with AMD, these findings provided initial background for our research with shared risk factors and pathophysiology between two diseases.
Our findings are supported by several plausible biologic mechanisms. First, the kidney and eye share common developmental pathways and have similar anatomical structures. Both the PAX and WT1 pathways are important in the embryogenesis of the kidney and retina22. Furthermore, both choroid and glomerulus have extensive vascular networks that are similar in structure, and the retinochoroidal junction resembles the glomerular filtration barrier32. In addition, the renin–angiotensin–aldosterone system is present in both eye and kidney21.
Second, AMD and ESRD share cardiovascular risk factors. Risk factors for AMD including old age, current smoking, and hypertension33, and pathogenic mechanisms of AMD development including atherosclerosis and oxidative stress34,35 are all implicated in the development of ESRD, which helps support our findings.
Third, growing evidence from genetic studies suggests that dysregulation of the complement system has a pathogenic role in both AMD9,36,37 and kidney diseases including atypical hemolytic uremic syndrome (aHUS)38,39, membranoproliferative glomerulonephritis (MPGN)40, IgA nephropathy41, and DM nephropathy42. Complement factor H (CFH) is a soluble complement regulator that is essential for controlling the alternative complement pathway and protects against oxidative stress. A genome-wide association study revealed a higher risk of AMD in individuals with a genetic polymorphism (Y402H) in the CFH gene9,11 of which locus is in a region that binds C-reactive protein. Therefore, we speculate that from the genetic polymorphism of CFH Y402H, reduced binding of C-reactive protein to the CFH protein limits the function of CFH, which results in the development of AMD and kidney disease.
Notably, we clearly demonstrated that the risk of ESRD was higher in AMD patients with visual disability (P for trend < 0·001). In our study, we examined the influence of visual disability status among AMD patients, which represents a novelty of our study. visual disability in AMD patients occurs when early AMD progresses to late AMD, which is classified into neovascular AMD and geographic atrophy. Therefore, advances in the pathogenic mechanism of AMD, especially regarding atherosclerosis, oxidative stress, and cardiovascular risks factors, may reinforce the risk of ESRD incidence.
Visual impairment is associated with physical inactivity43,44,45 and may have additional adverse results for people with visual disability. Previous nationwide studies have demonstrated that lower physical activity levels are associated with lower kidney function46 and the incidence of ESRD47. Visual impairment can also have adverse functional consequences including social isolation, restriction of daily activities, poor quality of life, and frailty26,48,49,50,51,52,53,54,55, especially in the elderly population; this further significantly affects nutritional status, with higher prevalence of obesity and malnutrition in patients with visual impairment56. Moreover, individuals with visual disability may experience great difficulty in accessing healthcare services. Therefore, appropriate management of risk factors would be challenging. For individuals with severe central vision loss, which is typical in advanced AMD, their reduced ability to read may lead to poor compliance or even overdose problems that possibly affect renal function. From these multiple components that interplay between visual impairment and adverse health outcomes, our findings that AMD patients with visual disability have much higher risk of ESRD than non-AMD group or even AMD patients without visual disability may be explained. A further prospective study is required to elucidate the chronological order in AMD and visual disability.
Intriguingly, our findings showed that the risk of ESRD was higher in AMD patients with younger age (50–64 years old), preserved renal function (eGFR ≥ 60 mL/min/1.73 m2), and without underlying cardiometabolic comorbidity, all of which are considered to be low risk factors for ESRD. This suggests that AMD is more strongly associated with ESRD risk when there are no other risk factors of AMD, which is a common finding in this kind of stratified analyses.
Several limitations should be considered in interpreting our findings. First, we defined AMD patients based on the diagnostic code (ICD-10) from the national database. In the clinical setting, the diagnosis of AMD is usually made on the basis of ophthalmoscopy during ophthalmologic examination, and a false positive diagnosis is not common. However, AMD is often underdiagnosed if symptoms are not severe, or some people may regard it as a normal aging process that patients do not seek health care services. Therefore, some AMD patients might have been categorized into the non-AMD group, making the observed association weaker than the true association. Second, considering the ethnic difference in genetic factors related to AMD57,58,59,60, our results cannot be generalized to other ethnic groups. Lastly, other possible confounders including nutrition and dietary factors, which might be associated with both AMD and ESRD61,62 were not controlled. Therefore, careful consideration is required to extrapolate the results to other groups.
We demonstrated that AMD is associated with an increased risk of ESRD. Remarkably, much higher risks of ESRD were found for AMD with visual disability. Our findings have clinical implications on disease prevention and risk factor management of ESRD in patients with AMD, and visual disability, suggesting shared risk factors and pathogenic mechanisms between AMD and ESRD.
Materials and methods
Data source and study setting
The national health insurance service (NHIS) provides mandatory universal coverage to 97% of the Korean population; the remaining 3% are Medicaid beneficiaries. For every individual 40 years old or above, the NHIS provides a biennial national health screening program that consists of a self-questionnaire on health behavior (smoking, drinking, and past medical history), anthropometric measurements (blood pressure, body mass index), and laboratory test findings (fasting glucose, serum lipid levels). The NHIS database consists of an eligibility database (age, sex, disability type and severity, socioeconomic variables, income level, type of eligibility), a medical treatment database (based on medical bills claimed by medical service providers for their medical expense claims), and therefore this nationwide database is widely used in epidemiologic studies in Korea63.
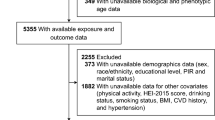
Study population
Among 4,470,729 participants (age ≥ 50) who underwent general health screenings in 2009, we first excluded 11,515 participants who had ESRD at the baseline. Next, 252,352 participants with missing data on at least one variable were excluded. Finally, a total of 4,206,862 participants were included in the analyses.
Definition of age-related macular degeneration
Individuals with AMD were identified on the basis of the International Classification of Diseases, 10th Revision (ICD-10) code for AMD (H353) by an ophthalmologist within one year before the health screening examination. This code includes early, intermediate, atrophic (geographic atrophy), and neovascular AMD. This operational definition of AMD was used in previous epidemiologic studies on AMD64,65.
Definition of visual disability
According to the National Disability Registration System in Korea, visual disability refers to a visual loss or visual field defect. Registration for disability requires the submission of the validated documentation of the results of disability diagnosis by a specialist physician66. A best-corrected visual acuity (BCVA) of 20/100 or less using the Snellen visual acuity chart is a minimal requirement to register for visual disability. In Korea, the severity of disability is graded from 1 (most severe) to 6 (least severe) (Supplementary Table S2). Several welfare benefits, including Disability Pension, have been determined using the severity67. Therefore, since almost every individual with disabilities applies for the registration, we were able to identify almost all individuals with visual disability in the National Disability Registration System in Korea.
Study outcomes and follow-up
The endpoints of the study were incident ESRD. Newly diagnosed ESRD was defined by the combination of an ICD-10 code (N18-19, Z49, Z94.0, and Z99.2) and a special code (V code) that indicates required hemodialysis (V001), peritoneal dialysis (V003), or kidney transplantation (V005). All medical expenses for dialysis are reimbursed using the Korean Health Insurance Review and Assessment Service database. These patients are also registered as special medical aid beneficiaries. Therefore, we were able to identify every patient with ESRD in the entire Korean population and to analyze the data for all patients with ESRD who underwent dialysis68. Codes for treatment or medical expense claims included V005 for kidney transplantation, V001 for hemodialysis, and V003 for peritoneal dialysis. We excluded individuals without previous CKD who had a transplant or dialysis code on the same date as an acute renal failure code. Subjects on continuous renal replacement therapy or acute peritoneal dialysis were also excluded. The participants were followed from the date of health screening examination in 2009 to the date of incident ESRD, death, or until the end of the study period (December 31, 2019), whichever came first.
Covariates
During the health screening, participants provided information on lifestyle behaviors using standardized questionnaires69. Smoking status was categorized as non-, ex-, and current smoking. Alcohol consumption was categorized as none, mild, and heavy drinking; heavy drinking was defined as ≥ 30 g of alcohol consumption per day. Regular physical activity was defined as strenuous exercise ≥ one time/week for at least 20 min per session. Household income was dichotomized by the lowest 20 percentile according to the health insurance premium (in the social health insurance system in Korea, insurance premium is determined by income status, not by health status). Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared.
Fasting serum glucose level, serum hemoglobin level, and estimated glomerular filtration rate (eGFR) were also assessed. Hypertension was defined as any of the following: systolic blood pressure ≥ 140 mmHg; diastolic blood pressure ≥ 90 mmHg; or treatment with an antihypertensive medication that was linked to hypertension ICD-10 codes (I10-I13 and I15) and resulted in at least one claim in a year. Diabetes mellitus was defined as a blood glucose level ≥ 126 mg/dL or history of a hypoglycemic medication prescription that was linked to diabetes mellitus ICD-10 code (E11-E14) and resulted in at least one claim in a year. Dyslipidemia was defined as total cholesterol ≥ 240 mg/dL or history of a lipid-lowering medication that was associated with an ICD-10 code (E78). Charlson comorbidity index (CCI) was calculated based on diagnosis code70.
Statistical analysis
The comparison of baseline characteristics by the presence of AMD and visual disability was conducted using t-test for continuous variables or the chi-square test for categorical variables. The incidence rates of ESRD were calculated by the number of incident cases divided by 100,000 person-years. Cox hazard regression model was used to examine the hazard ratios (HRs) of ESRD. Multivariable analyses were adjusted for age and sex in model 2 and for age, sex, household income, area of residence, body mass index, smoking, alcohol consumption, and regular exercise in model 3. In our final model (model 4), fasting serum glucose level, serum hemoglobin level, estimated glomerular filtration rate (eGFR), hypertension, diabetes mellitus, dyslipidemia, and Charlson comorbidity index (CCI) were included in addition to every adjusting variable used in model 3. P for trend was calculated among the hazard ratios of control, AMD without visual disability, and AMD with visual disability. Kaplan–Meier curves were presented as cumulative incidence probabilities of ESRD. Finally, to evaluate the potential effect modification by age, sex, eGFR, and comorbidity status, P for interaction was calculated using stratified analyses.
All statistical analyses were performed using SAS version 9·4 (SAS Institute Inc., Cary, NC, USA). P < 0·05 were considered to be statistically significant.
Ethic statement
This study was reviewed and approved by the Institutional Review Board of Samsung Medical Center (SMC IRB no. 2022-03-060) and waived the requirement to obtain any informed consent because anonymized and de-identified information in compliance with the confidentiality guidelines was used for analyses. This study adhered to the tenets of the Declaration of Helsinki.
Data availability
The datasets generated and/or analyzed during the current study are available in the Korean National Health Insurance Sharing Service database repository, (https://nhiss.nhis.or.kr). The datasets used and/or analyzed during the current study available from the NHIS on reasonable request.
References
Liyanage, T. et al. Worldwide access to treatment for end-stage kidney disease: A systematic review. Lancet 385, 1975–1982. https://doi.org/10.1016/s0140-6736(14)61601-9 (2015).
Choi, H. et al. Excess mortality among patients on dialysis: Comparison with the general population in Korea. Kidney Res. Clin. Pract. 33, 89–94. https://doi.org/10.1016/j.krcp.2014.04.001 (2014).
Keenan, T. D. L., Cukras, C. A. & Chew, E. Y. Age-related macular degeneration: Epidemiology and clinical aspects. Adv. Exp. Med. Biol. 1256, 1–31. https://doi.org/10.1007/978-3-030-66014-7_1 (2021).
Wong, W. L. et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob. Health 2, e106-116. https://doi.org/10.1016/s2214-109x(13)70145-1 (2014).
Liew, G., Mitchell, P., Wong, T. Y., Iyengar, S. K. & Wang, J. J. CKD increases the risk of age-related macular degeneration. J. Am. Soc. Nephrol. 19, 806–811. https://doi.org/10.1681/asn.2007080844 (2008).
Klein, R., Knudtson, M. D., Lee, K. E. & Klein, B. E. Serum cystatin C level, kidney disease markers, and incidence of age-related macular degeneration: The beaver dam eye study. Arch. Ophthalmol. 127, 193–199. https://doi.org/10.1001/archophthalmol.2008.551 (2009).
Weiner, D. E., Tighiouart, H., Reynolds, R. & Seddon, J. M. Kidney function, albuminuria and age-related macular degeneration in NHANES III. Nephrol. Dial. Transpl. 26, 3159–3165. https://doi.org/10.1093/ndt/gfr022 (2011).
Thompson, C. L. et al. Complement factor H and hemicentin-1 in age-related macular degeneration and renal phenotypes. Hum. Mol. Genet. 16, 2135–2148. https://doi.org/10.1093/hmg/ddm164 (2007).
Fritsche, L. G. et al. A large genome-wide association study of age-related macular degeneration highlights contributions of rare and common variants. Nat. Genet. 48, 134–143. https://doi.org/10.1038/ng.3448 (2016).
Sofat, R. et al. Complement factor H genetic variant and age-related macular degeneration: Effect size, modifiers and relationship to disease subtype. Int. J. Epidemiol. 41, 250–262. https://doi.org/10.1093/ije/dyr204 (2012).
Klein, R. J. et al. Complement factor H polymorphism in age-related macular degeneration. Science 308, 385–389. https://doi.org/10.1126/science.1109557 (2005).
Snow, K. K. & Seddon, J. M. Do age-related macular degeneration and cardiovascular disease share common antecedents?. Ophthalmic Epidemiol. 6, 125–143. https://doi.org/10.1076/opep.6.2.125.1558 (1999).
Tan, J. S., Mitchell, P., Smith, W. & Wang, J. J. Cardiovascular risk factors and the long-term incidence of age-related macular degeneration: The blue mountains eye study. Ophthalmology 114, 1143–1150. https://doi.org/10.1016/j.ophtha.2006.09.033 (2007).
Delcourt, C. et al. Associations of cardiovascular disease and its risk factors with age-related macular degeneration: The POLA study. Ophthalmic Epidemiol. 8, 237–249. https://doi.org/10.1076/opep.8.4.237.1613 (2001).
Cackett, P. et al. Smoking, cardiovascular risk factors, and age-related macular degeneration in Asians: The Singapore malay eye study. Am. J. Ophthalmol. 146, 960-967.e961. https://doi.org/10.1016/j.ajo.2008.06.026 (2008).
Lüdtke, L., Jürgens, C., Ittermann, T., Völzke, H. & Tost, F. Age-related macular degeneration and associated risk factors in the population-based study of health in pomerania (SHIP-Trend). Med. Sci. Monit. 25, 6383–6390. https://doi.org/10.12659/msm.915493 (2019).
Cheung, C. M. G. et al. Plasma lipoprotein subfraction concentrations are associated with lipid metabolism and age-related macular degeneration. J. Lipid. Res. 58, 1785–1796. https://doi.org/10.1194/jlr.M073684 (2017).
Erke, M. G. et al. Cardiovascular risk factors associated with age-related macular degeneration: The Tromsø study. Acta Ophthalmol. 92, 662–669. https://doi.org/10.1111/aos.12346 (2014).
Hsu, C. Y., Iribarren, C., McCulloch, C. E., Darbinian, J. & Go, A. S. Risk factors for end-stage renal disease: 25-year follow-up. Arch. Intern. Med. 169, 342–350. https://doi.org/10.1001/archinternmed.2008.605 (2009).
Wong, C. W., Wong, T. Y., Cheng, C. Y. & Sabanayagam, C. Kidney and eye diseases: Common risk factors, etiological mechanisms, and pathways. Kidney Int. 85, 1290–1302. https://doi.org/10.1038/ki.2013.491 (2014).
Wilkinson-Berka, J. L., Agrotis, A. & Deliyanti, D. The retinal renin-angiotensin system: Roles of angiotensin II and aldosterone. Peptides 36, 142–150. https://doi.org/10.1016/j.peptides.2012.04.008 (2012).
Izzedine, H., Bodaghi, B., Launay-Vacher, V. & Deray, G. Eye and kidney: From clinical findings to genetic explanations. J. Am. Soc. Nephrol. 14, 516–529. https://doi.org/10.1097/01.asn.0000051705.97966.ad (2003).
Jonas, J. B., Cheung, C. M. G. & Panda-Jonas, S. Updates on the epidemiology of age-related macular degeneration. Asia Pac. J. Ophthalmol. 6, 493–497. https://doi.org/10.22608/apo.2017251 (2017).
Kolli, A. et al. Longitudinal associations between vision impairment and the incidence of neuropsychiatric, musculoskeletal, and cardiometabolic chronic diseases. Am. J. Ophthalmol. 235, 163–171. https://doi.org/10.1016/j.ajo.2021.09.004 (2022).
Crews, J. E., Chou, C. F., Sekar, S. & Saaddine, J. B. The prevalence of chronic conditions and poor health among people with and without vision impairment, aged ≥ 65 years, 2010–2014. Am. J. Ophthalmol. 182, 18–30. https://doi.org/10.1016/j.ajo.2017.06.038 (2017).
Zhu, Z. et al. Association of visual impairment with risk for future Parkinson’s disease. EClinicalMedicine 42, 101189. https://doi.org/10.1016/j.eclinm.2021.101189 (2021).
Choi, J., Moon, J. W. & Shin, H. J. Chronic kidney disease, early age-related macular degeneration, and peripheral retinal drusen. Ophthalmic Epidemiol. 18, 259–263. https://doi.org/10.3109/09286586.2011.602509 (2011).
Nitsch, D., Evans, J., Roderick, P. J., Smeeth, L. & Fletcher, A. E. Associations between chronic kidney disease and age-related macular degeneration. Ophthalmic Epidemiol. 16, 181–186. https://doi.org/10.1080/09286580902863064 (2009).
Chen, C. Y. et al. Association between macular degeneration and mild to moderate chronic kidney disease: A nationwide population-based study. Medicine (Baltimore) 96, e6405. https://doi.org/10.1097/md.0000000000006405 (2017).
Chong, E. W. et al. Is renal function associated with early age-related macular degeneration?. Optom. Vis. Sci. 91, 860–864. https://doi.org/10.1097/opx.0000000000000288 (2014).
Boon, C. J., van de Ven, J. P., Hoyng, C. B., den Hollander, A. I. & Klevering, B. J. Cuticular drusen: Stars in the sky. Prog. Retin. Eye Res. 37, 90–113. https://doi.org/10.1016/j.preteyeres.2013.08.003 (2013).
Savige, J., Ratnaike, S. & Colville, D. Retinal abnormalities characteristic of inherited renal disease. J. Am. Soc. Nephrol. 22, 1403–1415. https://doi.org/10.1681/asn.2010090965 (2011).
Chakravarthy, U. et al. Clinical risk factors for age-related macular degeneration: A systematic review and meta-analysis. BMC Ophthalmol. 10, 31. https://doi.org/10.1186/1471-2415-10-31 (2010).
Klein, R., Peto, T., Bird, A. & Vannewkirk, M. R. The epidemiology of age-related macular degeneration. Am. J. Ophthalmol. 137, 486–495. https://doi.org/10.1016/j.ajo.2003.11.069 (2004).
Friedman, E. The role of the atherosclerotic process in the pathogenesis of age-related macular degeneration. Am. J. Ophthalmol. 130, 658–663. https://doi.org/10.1016/s0002-9394(00)00643-7 (2000).
Saksens, N. T. et al. Rare genetic variants associated with development of age-related macular degeneration. JAMA Ophthalmol. 134, 287–293. https://doi.org/10.1001/jamaophthalmol.2015.5592 (2016).
de Jong, S. et al. Systemic complement levels in patients with age-related macular degeneration carrying rare or low-frequency variants in the CFH gene. Hum. Mol. Genet. 31, 455–470. https://doi.org/10.1093/hmg/ddab256 (2022).
Dragon-Durey, M. A. et al. Heterozygous and homozygous factor h deficiencies associated with hemolytic uremic syndrome or membranoproliferative glomerulonephritis: Report and genetic analysis of 16 cases. J. Am. Soc. Nephrol. 15, 787–795. https://doi.org/10.1097/01.asn.0000115702.28859.a7 (2004).
de Jong, S. et al. Functional analysis of variants in complement factor I identified in age-related macular degeneration and atypical hemolytic uremic syndrome. Front. Immunol. 12, 789897. https://doi.org/10.3389/fimmu.2021.789897 (2021).
Iatropoulos, P. et al. Complement gene variants determine the risk of immunoglobulin-associated MPGN and C3 glomerulopathy and predict long-term renal outcome. Mol. Immunol. 71, 131–142. https://doi.org/10.1016/j.molimm.2016.01.010 (2016).
Medjeral-Thomas, N. R. et al. Circulating complement factor H-related proteins 1 and 5 correlate with disease activity in IgA nephropathy. Kidney Int. 92, 942–952. https://doi.org/10.1016/j.kint.2017.03.043 (2017).
Flyvbjerg, A. The role of the complement system in diabetic nephropathy. Nat. Rev. Nephrol. 13, 311–318. https://doi.org/10.1038/nrneph.2017.31 (2017).
Nguyen, A. M., Arora, K. S., Swenor, B. K., Friedman, D. S. & Ramulu, P. Y. Physical activity restriction in age-related eye disease: A cross-sectional study exploring fear of falling as a potential mediator. BMC Geriatr. 15, 64. https://doi.org/10.1186/s12877-015-0062-8 (2015).
Willis, J. R., Jefferys, J. L., Vitale, S. & Ramulu, P. Y. Visual impairment, uncorrected refractive error, and accelerometer-defined physical activity in the United States. Arch. Ophthalmol. 130, 329–335. https://doi.org/10.1001/archopthalmol.2011.1773 (2012).
van Landingham, S. W., Willis, J. R., Vitale, S. & Ramulu, P. Y. Visual field loss and accelerometer-measured physical activity in the United States. Ophthalmology 119, 2486–2492. https://doi.org/10.1016/j.ophtha.2012.06.034 (2012).
Hawkins, M. S. et al. Association between physical activity and kidney function: National health and nutrition examination survey. Med. Sci. Sports Exerc. 43, 1457–1464. https://doi.org/10.1249/MSS.0b013e31820c0130 (2011).
Jung, H. W. et al. Association between physical performance and incidence of end-stage renal disease in older adults: A national wide cohort study. BMC Nephrol. 22, 85. https://doi.org/10.1186/s12882-021-02291-4 (2021).
Crews, J. E., Chou, C. F., Zhang, X., Zack, M. M. & Saaddine, J. B. Health-related quality of life among people aged ≥ 65 years with self-reported visual impairment: Findings from the 2006–2010 behavioral risk factor surveillance system. Ophthalmic Epidemiol. 21, 287–296. https://doi.org/10.3109/09286586.2014.926556 (2014).
Langelaan, M. et al. Impact of visual impairment on quality of life: A comparison with quality of life in the general population and with other chronic conditions. Ophthalmic Epidemiol. 14, 119–126. https://doi.org/10.1080/09286580601139212 (2007).
Vu, H. T., Keeffe, J. E., McCarty, C. A. & Taylor, H. R. Impact of unilateral and bilateral vision loss on quality of life. Br. J. Ophthalmol. 89, 360–363. https://doi.org/10.1136/bjo.2004.047498 (2005).
Crews, J. E. & Campbell, V. A. Vision impairment and hearing loss among community-dwelling older Americans: Implications for health and functioning. Am. J. Public Health 94, 823–829. https://doi.org/10.2105/ajph.94.5.823 (2004).
Ramrattan, R. S. et al. Prevalence and causes of visual field loss in the elderly and associations with impairment in daily functioning: The Rotterdam Study. Arch. Ophthalmol. 119, 1788–1794. https://doi.org/10.1001/archopht.119.12.1788 (2001).
Wallhagen, M. I., Strawbridge, W. J., Shema, S. J., Kurata, J. & Kaplan, G. A. Comparative impact of hearing and vision impairment on subsequent functioning. J. Am. Geriatr. Soc. 49, 1086–1092. https://doi.org/10.1046/j.1532-5415.2001.49213.x (2001).
Bookwala, J. & Lawson, B. Poor vision, functioning, and depressive symptoms: A test of the activity restriction model. Gerontologist 51, 798–808. https://doi.org/10.1093/geront/gnr051 (2011).
Klein, B. E., Klein, R., Knudtson, M. D. & Lee, K. E. Relationship of measures of frailty to visual function: The beaver dam eye study. Trans. Am. Ophthalmol. Soc. 101, 196–199 (2003).
Jones, N. & Bartlett, H. The impact of visual impairment on nutritional status: A systematic review. Br. J. Vis. Impair. 36, 17–30. https://doi.org/10.1177/0264619617730860 (2018).
DeAngelis, M. M. et al. Genetics of age-related macular degeneration (AMD). Hum. Mol. Genet. 26, R45-r50. https://doi.org/10.1093/hmg/ddx228 (2017).
Spencer, K. L., Glenn, K., Brown-Gentry, K., Haines, J. L. & Crawford, D. C. Population differences in genetic risk for age-related macular degeneration and implications for genetic testing. Arch. Ophthalmol. 130, 116–117. https://doi.org/10.1001/archopthalmol.2011.1370 (2012).
Restrepo, N. A. et al. Genetic determinants of age-related macular degeneration in diverse populations from the PAGE study. Invest. Ophthalmol. Vis. Sci. 55, 6839–6850. https://doi.org/10.1167/iovs.14-14246 (2014).
Kondo, N., Bessho, H., Honda, S. & Negi, A. Complement factor H Y402H variant and risk of age-related macular degeneration in Asians: A systematic review and meta-analysis. Ophthalmology 118, 339–344. https://doi.org/10.1016/j.ophtha.2010.06.040 (2011).
Swenor, B. K. et al. Visual impairment and incident mobility limitations: The health, aging and body composition study. J. Am. Geriatr. Soc. 63, 46–54. https://doi.org/10.1111/jgs.13183 (2015).
Gorusupudi, A., Nelson, K. & Bernstein, P. S. The age-related eye disease 2 study: Micronutrients in the treatment of macular degeneration. Adv. Nutr. 8, 40–53. https://doi.org/10.3945/an.116.013177 (2017).
Lee, Y. H., Han, K., Ko, S. H., Ko, K. S. & Lee, K. U. Data analytic process of a nationwide population-based study using national health information database established by national health insurance service. Diabetes Metab. J. 40, 79–82. https://doi.org/10.4093/dmj.2016.40.1.79 (2016).
Tsai, D. C., Chen, S. J., Huang, C. C., Yuan, M. K. & Leu, H. B. Age-related macular degeneration and risk of degenerative dementia among the elderly in Taiwan: A population-based cohort study. Ophthalmology 122, 2327-2335.e2322. https://doi.org/10.1016/j.ophtha.2015.07.033 (2015).
Choi, S., Jahng, W. J., Park, S. M. & Jee, D. Association of age-related macular degeneration on alzheimer or parkinson disease: A retrospective cohort study. Am. J. Ophthalmol. 210, 41–47. https://doi.org/10.1016/j.ajo.2019.11.001 (2020).
Shin, D. W. et al. Disparities in cervical cancer screening among women with disabilities: A national database study in South Korea. J. Clin. Oncol. 36, 2778–2786. https://doi.org/10.1200/jco.2018.77.7912 (2018).
Number of registered persons with disabilities and disability pension recipients (Issue: April 5, 2022), Ministry of Health and Welfare, Republic of Korea. (2022).
Hui Bae, E. et al. Effects of blood pressure according to age on end-stage renal disease development in patients with patients with diabetes: A nationwide population-based cohort study. Hypertension 79, 1765–1776. https://doi.org/10.1161/hypertensionaha.121.18881 (2022).
Shin, D. W., Cho, J., Park, J. H. & Cho, B. National general health screening program in Korea: History, current status, and future direction. Precis. Future Med. 6, 9–31. https://doi.org/10.23838/pfm.2021.00135 (2022).
Kim, K. H. Comparative study on three algorithms of the ICD-10 Charlson comorbidity index with myocardial infarction patients. J. Prev. Med. Public Health 43, 42–49. https://doi.org/10.3961/jpmph.2010.43.1.42 (2010).
Acknowledgements
This research was partially supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant Number: HI20C1073), which was received by Dong Wook Shin; and by a grant from the National Research Foundation of Korea, funded by Ministry of Education, Republic of Korea (NRF-2021R1C1C1007795), which was received by Dong Hui Lim.
Author information
Authors and Affiliations
Contributions
Conceptualization, W.J., H.R.J., J.M.Y., D.H.L. and D.W.S.; Data curation, W.J., J.P., K.H. and B.K.; Formal analysis, W.J., K.H. and B.K.; Funding acquisition, D.H.L. and D.W.S.; Investigation, W.J., D.H.L. and D.W.S.; Methodology, W.J., H.R.J., J.J., K.H., J.M.Y. and D.W.S.; Project administration, D.H.L. and D.W.S.; Software, K.H. and B.K.; Supervision, D.W.S.; Writing—original draft, W.J.; Writing—review & editing, W.J., H.R.J., J.J., J.M.Y., D.H.L. and D.W.S.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jung, W., Park, J., Jang, H.R. et al. Increased end-stage renal disease risk in age-related macular degeneration: a nationwide cohort study with 10-year follow-up. Sci Rep 13, 183 (2023). https://doi.org/10.1038/s41598-022-26964-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-26964-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.