Abstract
The aim of this study was to determine whether Post-acute Sequelae of SARS-CoV-2 Infection (PASC) are associated with physical inactivity in COVID-19 survivors. This is a cohort study of COVID-19 survivors discharged from a tertiary hospital in Sao Paulo, Brazil. Patients admitted as inpatients due to laboratory-confirmed COVID-19 between March and August 2020 were consecutively invited for a follow-up in-person visit 6 to 11 months after hospitalization. Ten symptoms of PASC were assessed using standardized scales. Physical activity was assessed by questionnaire and participants were classified according to WHO Guidelines. 614 patients were analyzed (age: 56 ± 13 years; 53% male). Frequency of physical inactivity in patients exhibiting none, at least 1, 1–4, and 5 or more symptoms of PASC was 51%, 62%, 58%, and 71%, respectively. Adjusted models showed that patients with one or more persistent PASC symptoms have greater odds of being physically inactive than those without any persistent symptoms (OR: 1.57 [95% CI 1.04–2.39], P = 0.032). Dyspnea (OR: 2.22 [1.50–3.33], P < 0.001), fatigue (OR: 2.01 [1.40–2.90], P < 0.001), insomnia (OR: 1.69 [1.16–2.49], P = 0.007), post-traumatic stress (OR: 1.53 [1.05–2.23], P = 0.028), and severe muscle/joint pain (OR: 1.53 [95% CI 1.08–2.17], P = 0.011) were associated with greater odds of being physically inactive. This study suggests that PASC is associated with physical inactivity, which itself may be considered as a persistent symptom among COVID-19 survivors. This may help in the early identification of patients who could benefit from additional interventions tailored to combat inactivity (even after treatment of PASC), with potential beneficial impacts on overall morbidity/mortality and health systems worldwide.
Similar content being viewed by others
Introduction
COVID-19 pandemic is raising a devastating impact on public health, resulting in millions of hospitalizations and deaths globally1. Among survivors, the high occurrence of patients reporting post-acute sequelae of SARS-CoV-2 (PASC) is a great cause of concern, as it threatens health systems worldwide. This condition, also known as “long COVID”, is defined as the illness that occurs in people who have a history of probable or confirmed SARS-CoV-2 infection, usually within 3 months from the onset of COVID-19, with symptoms and effects that last for at least 2 months2. Early reports revealed that around 76% of patients reported at least 1 persistent symptom 6 months following hospital discharge3, with fatigue, dyspnea, cough, headache, loss of taste or smell, and cognitive or mental health impairments (e.g., anxiety or depression) being the most commonly reported symptoms4,5,6,7.
Physical inactivity (i.e., < 150 min/week at moderate-to-vigorous physical activity) is widely recognized as an independent risk factor for impaired functional status8, musculoskeletal disorders9, anxiety and depression10, and all-cause mortality11. Only a single study showed that patients who experienced persistent symptoms 6 months after COVID-19 reported lower physical activity levels compared to the pre-infection period12. Considering the detrimental effects that physical inactivity may have upon overall health status and quality of life in COVID-19 survivors, it is of public health importance to determine the risk factors related to PASC that may predispose to physical inactivity and help to early identify individuals that are more likely to be physically inactive.
Therefore, we aimed to determine whether PASC are associated with physical inactivity in a cohort of 614 COVID-19 survivors who underwent in-person multidisciplinary assessments conducted 6–11 months following hospitalization in a tertiary hospital in Brazil.
Results
A total of 749 eligible individuals attended the in-person follow-up assessment; 614 had complete data and were included in the analysis. Table 1 shows the characteristics of these patients. The sample comprised patients of both sexes (53% male) aged 56 ± 13 years. The frequency of low, middle, and high socioeconomic status was 9%, 50% and 40%, respectively. This is a similar profile to that of the city of Sao Paulo, according to the National Household Sample Survey (Pesquisa Nacional por Amostra de Domicílio—PNADC—2021) from the Brazilian Institute of Geography and Statistics13. Thirty-seven percent of the patients were smoking at baseline. Prevalence of current hypertension, type 2 diabetes, and obesity were 58%, 35%, and 17%, respectively. Fifty five percent of the patients required intensive care and 37% used invasive mechanical ventilation. Only 40% of the patients met the physical activity recommendations. Table 2 shows the prevalence of physical inactivity according to sex and age.
Prevalence of physical inactivity in patients exhibiting none, at least 1, 1–4, and 5 or more PASC symptoms were 51%, 62%, 58%, and 71%, respectively. The frequency of physical inactivity in patients reporting different PASC were: dyspnea (77%), fatigue (69%), severe muscle/joint pain (66%), insomnia (66%), post-traumatic stress disorder (65%), memory impairments (65%), anxiety (65%), taste (65%) and smell (63%) loss, and depression (62%). Table 3 details the prevalence of physical inactivity according to the presence of post-acute sequelae of SARS-CoV-2.
The adjusted model controlling for confounders (i.e., age [< 60 and ≥ 60 years old], sex [male or female], intensive care unit admission [yes or no], invasive mechanical ventilation [yes or no], hospital length of stay [< 15 and ≥ 15 days], hypertension [yes or no], type 2 diabetes [yes or no], and obesity [BMI < 30 or BMI ≥ 30]) showed that patients with one or more persistent symptoms have greater odds of being physically inactive than those who did not experience any persistent symptoms (OR: 1.57 [95% CI 1.04–2.39], P = 0.032) (Fig. 1). In addition, patients reporting 5 or more persistent symptoms showed greater odds of being physically inactive than those without persistent symptoms (OR: 2.38 [95% CI 1.44–3.97], P = 0.001) (Fig. 1).
Adjusted models also showed that severe muscle/joint pain (OR: 1.53 [95% CI 1.08–2.17], P = 0.011), fatigue (OR: 2.01 [1.40–2.90], P < 0.001), post-traumatic stress (OR: 1.53 [1.05–2.23], P = 0.028), insomnia (OR: 1.69 [1.16–2.49], P = 0.007), and dyspnea (OR: 2.22 [1.50–3.33], P < 0.001) were associated with greater odds of being physically inactive (all P < 0.05; Fig. 2). Importantly, fatigue and dyspnea remained as statistically significant predictors of physical inactivity, even after adjusting P-value for multiple comparisons (both P < 0.005; Fig. 2). Conversely, memory impairments, depression, anxiety, taste, and smell loss did not significantly associate with physical activity (all P > 0.05) (Fig. S1).
Multivariate-adjusted logistic regression analyses (odds ratio [(95% CI]) of the association between persistent symptoms related to COVID-19 (Severe muscle/joint pain, fatigue, post-traumatic stress, insomnia, dyspnea, memory impairments, depression, anxiety, taste loss, and smell loss) with physical inactivity (< 150 min/week of moderate-to-vigorous activity). *Unadjusted P < 0.05; # adjusted P < 0.005 (Bonferroni correction).
Discussion
The aim of this study was to examine the associations between PASC and physical inactivity in a cohort of COVID-19 survivors (most of them admitted at ICU with pre-existing comorbidities) 6–11 months following hospitalization. The main findings are severalfold: (i) The frequency of physical inactivity was substantive among patients with PASC (60%); (ii) PASC was associated with 57% greater odds of physical inactivity; (iii) the presence of ≥ 5 persistent symptoms vs. none increased the odds of physical inactivity by 138%; (iv). Namely, dyspnea (132%), fatigue (101%), insomnia (69%), post-traumatic stress (53%), and severe muscle/joint pain (53%) were associated with greater odds of physical inactivity. This study provides novel data suggesting that PASC is associated with physical inactivity, which itself may be considered an expected persistent feature among COVID-19 survivors.
There is a growing body of knowledge calling the attention to a high prevalence of PASC worldwide4,5,6,7. Indeed, a significant proportion of COVID-19 survivors may still present with physical, mental, or cognitive symptoms 6–12 months after the acute infection, particularly in those following ICU treatment4,14,15,16,17,18. Whether PASC are risk factors predisposing to a physically inactive lifestyle was so far unexplored.
In our cohort of patients followed 6–11 months after hospitalization in a tertiary hospital, roughly 60% were physically inactive, which exceeds inactivity estimates of 47% for individuals of similar age observed in a population-based study in Brazil19. Interestingly, adjusted models suggested that PASC may predispose to physical inactivity, particularly when multiple symptoms are present. We were also able to identify specific symptoms predicting physical inactivity: severe muscle/joint pain, fatigue, post-traumatic stress, insomnia, and dyspnea. Importantly, fatigue and dyspnea remained as significant predictors even after adjusting P-value using a highly conservative approach (i.e., Bonferroni correction). These results are of relevance as both fatigue and dyspnea are very frequent PASC and, therefore, may increase the odds to physical inactivity and, ultimately, the risk of poor health outcomes. Some caution should be taken when interpreting these findings, as the design of this study does not allow causative inferences, however plausibility does exist to conjecture that these symptoms, especially when combined, may prevent one from achieving the recommended levels of physical activity.
To the best of our knowledge, this study is the first to investigate associations between individual PASC symptoms with physical inactivity. The adjusted regression models showed that not all PASC symptoms were associated with physical inactivity. The significant associations between specific PASC symptoms (i.e. fatigue, pain, dyspnea, and insomnia) and reduced physical activity could be mediated by different COVID-related pathologies, including persistent pulmonary20, renal21 or cardiovascular22 dysfunction. A proportion of PASC cases may also exhibit a form of myalgic encephalomyelitis/chronic fatigue syndrome 23, which is directly associated with signs of persistent systemic inflammation24 and can potentially lead to hypoactivity. Regarding mental symptoms, the finding that post-traumatic stress was more related to physical inactivity than depression or anxiety is also potentially interesting, indicating that there may be specific psychiatric manifestations that predispose to physical inactivity in PASC.
Independently of the pathophysiological bases underlying the presence of physical inactivity in association with PASC, an inactive lifestyle is a risk factor that has the potential to increase the demand on health systems worldwide, through increasing both the incidence and aggravation of chronic conditions11. Moreover, physical inactivity is an independent risk factor strongly associated with increased mortality; estimates using population attributed fractions suggested that physical inactivity can be responsible for 9% of all-cause mortality worldwide25. Importantly, distinct clinical populations have demonstrated a sustained decline in physical activity level after hospital discharge26,27. For instance, patients with chronic obstructive pulmonary disease hospitalized to treat acute exacerbation showed a reduction of physical activity levels 1 month after hospital discharge, especially those with more pronounced muscle weakness at the end of the hospitalization period26.Recently, a study observed a significant decrease in self-reported walking time 6 months after the onset of symptoms of COVID-1912. In this scenario, if COVID-19, and notably PASC, can result in sustained physical inactivity, patients’ survival may be also impacted. Given the multiple types of organ system dysfunctions that may contribute to PASC, further studies are warranted to investigate which of those pathologies may most significantly impact on the emergence of PASC-related physical inactivity—an emerging risk factor that may lead to higher rates of morbidity and mortality. Of relevance, the reversal of inactivity has the potential to attenuate physical, mental and cognitive symptoms that encompass PASC. Therefore, early identification of individuals that could benefit from interventions specifically tailored to promote physical activity may be key to mitigate, at least partially, the burden associated with PASC. Further studies are also warranted to investigate the accurate prevalence and prognostic value of physical inactivity among COVID-19 survivors, and the potential role of vaccination (and perhaps other therapies) on the prevention of inactivity, as seen with other PASC symptoms25.
This study is not free of limitations. The observational cross-sectional design hampers establishing cause-and-effect relationships as previously noted, and it may lead to reverse causation bias (i.e., physically inactive individuals may also be prone to PASC, such as fatigue, muscle/joint pain, dyspnea etc.). Physical activity levels were assessed through a questionnaire and reflect the week prior to follow-up assessments. Moreover, the use of questionnaire to assess physical activity is prone to recall bias and overreporting.
In conclusion, among a cohort of COVID-19 survivors showing a high frequency of PASC 6–11 months following hospitalization, the number and type of PASC was predictive of physical inactivity. The novel data provided by this study warrant further investigations to ascertain which COVID-related organ system pathologies may most significantly contribute to the emergence of physical inactivity and help in the early identification of recovering COVID-19 patients who might benefit from interventions to combat inactivity. Considering the potential impact of this risk factor on overall morbidity and mortality and, hence, health systems, healthcare professionals and policy makers should be concerned about COVID-related physical inactivity.
Methods
Study design and participants
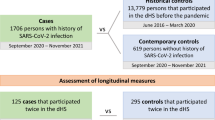
This study is part of HCFMUSP PASC Initiative, which is a prospective, multidisciplinary cohort study of COVID-19 survivors discharged from the largest tertiary hospital of Latin America (Clinical Hospital, School of Medicine of the University of Sao Paulo).
All patients aged ≥ 18 years who had been admitted (for at least 24 h) as inpatients to our hospital due to laboratory-confirmed COVID-19 between March and August 2020 were consecutively invited for a follow-up in-person visit between October 2020 and April 2021. Exclusion criteria were: previous diagnosis of dementia or end-stage cancer, nosocomial COVID-19 infection, living in long-term care facilities or with insufficient mobility to leave home, and suspected reinfection at the time of follow-up assessment. The details on the study protocol and planned measures have been thoroughly described elsewhere28.
This study was approved by the local Ethics Committee (Ethics Committee Approval Number (approval numbers: 4.270.242, 4.502.334, 4.524.031, 4.302.745 and 4.391.560) and registered at the Brazilian Registry of Clinical Trials (https://ensaiosclinicos.gov.br/). All patients provided written informed consent before entering the study. This manuscript was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement. Furthermore, all methods were performed in accordance with the relevant guidelines and regulations.
Data collection
All patients were evaluated between 6 and 11 months following hospitalization. In brief, patients underwent semi-structured interviewing regarding sociodemographic characteristics, occupational history, lifestyle habits (tobacco and physical activity levels), and self-evaluated health and medical history (with emphasis on previous and present comorbidities, cardiopulmonary symptoms, and medication regimen), and completed a multidisciplinary battery of objective physical assessments and laboratory tests conducted by clinicians and trained non-medical research workers (see reference28 for details). Smoking status refers to follow-up assessment (6–11 months after hospital discharge), while pre-existing conditions refers to assessments at the time of hospital admission.
Data from interviews, scales and complementary examinations were captured and stored using real-time web-based case report forms developed on a Research Electronic Data Capture (REDCap) system hosted at the hospital29. A team of REDCap experts managed the database and provided access for the different research groups to conduct interim and final statistical analyses.
Physical inactivity
Physical activity was assessed during the in-person follow-up visits by experienced researchers using The International Physical Activity Questionnaire-Short Form (IPAQ). In brief, IPAQ inquiries about physical activity in the past 7 days. Time spent in each activity was calculated as the number of days multiplied by the number of hours reported. Participants were classified as physically inactive according to WHO Guidelines (i.e., < 150 min/week of moderate-to-vigorous intensity physical activity).
Post-acute sequelae of SARS-CoV-2 infection
For the present investigation, we used data regarding ten self-reported symptoms deemed as relevant to PASC9,30 which were evaluated using standardized scales applied by specialized teams during the in-person visits, including: post-traumatic stress disorder31, anxiety and depression32, insomnia33, subjective memory impairment34, fatigue35, dyspnea36, severe muscle/joint pain36, and taste and smell loss)37. For all dependent variables, validated scale cutoffs were used to generate categorical ‘yes–no’ variables. For all variables but post-traumatic stress, subjects were asked about the presence of symptoms before hospitalization, in order to confirm that the onset of symptoms occurred after COVID-19.
Statistical analyses
Characteristics of patients 6–11 months following hospitalization are presented as absolute (n) and relative (%) frequency. The association of the outcome of interest (physical inactivity) was assessed by means of multivariable logistic regression adjusted by age [< 60 and ≥ 60 years old], sex [male or female], intensive care unit admission [yes or no], invasive mechanical ventilation [yes or no], hospital length of stay [< 15 and ≥ 15 days] and pre-existing conditions (hypertension [yes or no], type 2 diabetes [yes or no], and obesity [BMI < 30 or BMI ≥ 30]). Confounders were selected based on a Direct Acyclic Graph (DAG, www.dagitty.net), which is a causal diagram based on causal relations between the exposure, outcome, and potential confounders38. The DAG was developed from a priori knowledge to identify a minimum yet sufficient set of covariates to remove confounding factors from the statistical analysis39 (Fig. S1). Odds ratios were calculated along their corresponding 95% confidence intervals (95% CI). For associations between each PASC (i.e., post-traumatic stress disorder, anxiety and depression, insomnia, memory impairment, fatigue, dyspnea, severe muscle/joint pain, and taste and smell loss) and physical inactivity, significance level was set at P ≤ 0.005 (according to Bonferroni correction for multiple tests). All other significance levels were set at P ≤ 0.05. All analyses were performed in the statistical environment R (version 3.5.3; R Core Team 2020).
Data availability
All background information on individuals and clinical information for patients included in this study are available from corresponding author on reasonable request.
References
Dong, E., Du, H. & Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 20, 533–534. https://doi.org/10.1016/S1473-3099(20)30120-1 (2020).
WHO/2019-nCoV/Post_COVID-19_condition/Clinical_case_definition/2021.1.
Meeting the challenge of long COVID. Nat. Med. 26, 1803, https://doi.org/10.1038/s41591-020-01177-6 (2020).
Lopez-Leon, S. et al. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 11, 16144. https://doi.org/10.1038/s41598-021-95565-8 (2021).
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395, 497–506. https://doi.org/10.1016/S0140-6736(20)30183-5 (2020).
Nalbandian, A. et al. Post-acute COVID-19 syndrome. Nat. Med. 27, 601–615. https://doi.org/10.1038/s41591-021-01283-z (2021).
Damiano, R. F. et al. Post-COVID-19 psychiatric and cognitive morbidity: Preliminary findings from a Brazilian cohort study. Gen. Hosp. Psychiatry 75, 38–45. https://doi.org/10.1016/j.genhosppsych.2022.01.002 (2022).
Paterson, D. H. & Warburton, D. E. Physical activity and functional limitations in older adults: A systematic review related to Canada’s physical activity guidelines. Int. J. Behav. Nutr. Phys. Act. 7, 38. https://doi.org/10.1186/1479-5868-7-38 (2010).
Heesch, K. C., Miller, Y. D. & Brown, W. J. Relationship between physical activity and stiff or painful joints in mid-aged women and older women: A 3-year prospective study. Arthr. Res. Ther. 9, R34. https://doi.org/10.1186/ar2154 (2007).
Chekroud, S. R. et al. Association between physical exercise and mental health in 1.2 million individuals in the USA between 2011 and 2015: a cross-sectional study. Lancet Psychiatry 5, 739–746. https://doi.org/10.1016/S2215-0366(18)30227-X (2018).
Hamer, M., O’Donovan, G. & Stamatakis, E. Lifestyle risk factors, obesity and infectious disease mortality in the general population: Linkage study of 97,844 adults from England and Scotland. Prev. Med. 123, 65–70. https://doi.org/10.1016/j.ypmed.2019.03.002 (2019).
Delbressine, J. M. et al. The impact of Post-COVID-19 Syndrome on self-reported physical activity. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph18116017 (2021).
IBGE. Pesquisa Nacional por Amostra de Domicílio: PNAD, https://www.ibge.gov.br/ (2021).
Huang, C. et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 397, 220–232. https://doi.org/10.1016/S0140-6736(20)32656-8 (2021).
Writing Committee for the CSG. Four-month clinical status of a cohort of patients after hospitalization for COVID-19. JAMA 325, 1525–1534. https://doi.org/10.1001/jama.2021.3331 (2021).
Logue, J. K. et al. Sequelae in adults at 6 months after COVID-19 infection. JAMA Netw Open 4, e210830. https://doi.org/10.1001/jamanetworkopen.2021.0830 (2021).
Carfi, A., Bernabei, R. & Landi, F. Gemelli against, C.-P.-A. C. S. G. persistent symptoms in patients after acute COVID-19. JAMA 324, 603–605. https://doi.org/10.1001/jama.2020.12603 (2020).
Heesakkers, H. et al. Clinical outcomes among patients With 1-year survival following intensive care unit treatment for COVID-19. JAMA https://doi.org/10.1001/jama.2022.0040 (2022).
BRASIL. in vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico : estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 estados brasileiros e no Distrito Federal em 2020 (ed Departamento de Análise em Saúde e Vigilância de Doenças não Transmissíveis) 124p (2020).
Andersson, M., Stridsman, C., Ronmark, E., Lindberg, A. & Emtner, M. Physical activity and fatigue in chronic obstructive pulmonary disease: A population based study. Respir. Med. 109, 1048–1057. https://doi.org/10.1016/j.rmed.2015.05.007 (2015).
Sheshadri, A., Kittiskulnam, P. & Johansen, K. L. Higher physical activity is associated with less fatigue and insomnia among patients on hemodialysis. Kidney Int. Rep. 4, 285–292. https://doi.org/10.1016/j.ekir.2018.10.014 (2019).
Xie, Y., Xu, E., Bowe, B. & Al-Aly, Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med. https://doi.org/10.1038/s41591-022-01689-3 (2022).
Wong, T. L. & Weitzer, D. J. Long COVID and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)-a systemic review and comparison of clinical presentation and symptomatology. Medicina https://doi.org/10.3390/medicina57050418 (2021).
Morris, G. et al. Myalgic encephalomyelitis/chronic fatigue syndrome: From pathophysiological insights to novel therapeutic opportunities. Pharmacol. Res. 148, 104450. https://doi.org/10.1016/j.phrs.2019.104450 (2019).
Lee, I. M. et al. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 380, 219–229. https://doi.org/10.1016/S0140-6736(12)61031-9 (2012).
Pitta, F. et al. Physical activity and hospitalization for exacerbation of COPD. Chest 129, 536–544. https://doi.org/10.1378/chest.129.3.536 (2006).
Reid, R. D. et al. Determinants of physical activity after hospitalization for coronary artery disease: The tracking exercise after cardiac hospitalization (TEACH) study. Eur. J. Cardiovasc. Prev. Rehabilit.: Off. J. Eur. Soc. Cardiol. Work Groups Epidemiol. Prev. Card. Rehabilit. Exerc. Physiol. 13, 529–537. https://doi.org/10.1097/01.hjr.0000201513.13343.97 (2006).
Busatto, G. F. et al. Post-acute sequelae of SARS-CoV-2 infection (PASC): A protocol for a multidisciplinary prospective observational evaluation of a cohort of patients surviving hospitalisation in Sao Paulo, Brazil. BMJ Open 11, e051706. https://doi.org/10.1136/bmjopen-2021-051706 (2021).
Harris, P. A. et al. Research electronic data capture (REDCap): A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381. https://doi.org/10.1016/j.jbi.2008.08.010 (2009).
Nasserie, T., Hittle, M. & Goodman, S. N. Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: A systematic review. JAMA Netw. Open 4, e2111417. https://doi.org/10.1001/jamanetworkopen.2021.11417 (2021).
Weathers, F., Litz, B. & Herman, D. in Proceedings of the 9th Annual Meeting of the International Society for Traumatic Stress Studies (ISTSS).
Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiatr. Scand 67, 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x (1983).
Bastien, C. H., Vallières, A. & Morin, C. M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2, 297–307. https://doi.org/10.1016/s1389-9457(00)00065-4 (2001).
Vale, F. A. C., Balieiro, A. P. Jr. & Silva-Filho, J. H. Memory complaint scale (MCS). Proposed tool for active systematic search. Dement. Neuropsychol. 6, 212–218. https://doi.org/10.1590/S1980-57642012DN06040004 (2012).
Boonstra, A. M., Schiphorst Preuper, H. R., Balk, G. A. & Stewart, R. E. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 155, 2545–2550. https://doi.org/10.1016/j.pain.2014.09.014 (2014).
Webster, K., Cella, D. & Yost, K. The functional assessment of chronic illness therapy (FACIT) measurement system: Properties, applications, and interpretation. Health Qual Life Outcomes 1, 79. https://doi.org/10.1186/1477-7525-1-79 (2003).
Bell, M. L. et al. Post-acute sequelae of COVID-19 in a non-hospitalized cohort: Results from the Arizona CoVHORT. PLoS One 16, e0254347. https://doi.org/10.1371/journal.pone.0254347 (2021).
Joffe, M., Gambhir, M., Chadeau-Hyam, M. & Vineis, P. Causal diagrams in systems epidemiology. Emerg. Themes Epidemiol. 9, 1. https://doi.org/10.1186/1742-7622-9-1 (2012).
Robins, J. M. Data, design, and background knowledge in etiologic inference. Epidemiology 12, 313–320. https://doi.org/10.1097/00001648-200105000-00011 (2001).
Acknowledgements
The authors are thankful to the task force of HCFMUSP COVID-19 Study Group: Rosemeire Keiko, Danielle Pedroni de Moraes, Renato Madrid Baldassare, Antônio José Pereira, Elizabeth de Faria, Gisele Pereira, Lucila Pedroso da Cruz, Marcelo, Cristiano de Azevedo Ramos, Vilson Cobello Junior.
Funding
The authors acknowledge the support by the Sao Paulo Research Foundation (FAPESP 2017/13552-2). H.R. is supported by grants from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq 308307/2021-6). S.G. is supported by a grant from the Sao Paulo Research Foundation (FAPESP 2020/08091-9).
Author information
Authors and Affiliations
Consortia
Contributions
The authors’ contributions were as follows: Designed research: S.G., B.G., R.F.D., F.P., M.I., V.R., E.K., L.R.B., O.V.F., C.R.R.C., G.F.B., H.R.; Conducted research: S.G., A.L.A., G.N.O.J.; Provided essential materials: R.F.D., F.P., M.I., V.R., E.K., L.R.B., O.V.F., C.R.R.C., G.F.B.; Analyzed data/Statistical analysis: S.G., B.G., H.R.; Wrote paper: S.G., B.G., H.R.; Writing—review and editing: A.L.A., G.N.O.J., R.F.D., F.P., M.I., V.R., E.K., L.R.B., O.V.F., C.R.R.C., G.F.B. Primary responsibility for final content: HR. All authors: read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gil, S., Gualano, B., de Araújo, A.L. et al. Post-acute sequelae of SARS-CoV-2 associates with physical inactivity in a cohort of COVID-19 survivors. Sci Rep 13, 215 (2023). https://doi.org/10.1038/s41598-022-26888-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-26888-3
This article is cited by
-
Device-assessed physical activity and sleep quality of post-COVID patients undergoing a rehabilitation program
BMC Sports Science, Medicine and Rehabilitation (2024)
-
Association of physical symptoms with accelerometer-measured movement behaviors and functional capacity in individuals with Long COVID
Scientific Reports (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.