Abstract
Inefficient management of resources and waiting lists for high-risk ophthalmology patients can contribute to sight loss. The aim was to develop a decision support tool which determines an optimal patient schedule for ophthalmology patients. Our approach considers available booking slots as well as patient-specific factors. Using standard software (Microsoft Excel and OpenSolver), an operations research approach was used to formulate a mathematical model. Given a set of patients and clinic capacities, the model objective was to schedule patients efficiently depending on eyecare measure risk factors, referral-to-treatment times and targets, patient locations and slot availabilities over a pre-defined planning horizon. Our decision support tool can feedback whether or not a patient is scheduled. If a patient is scheduled, the tool determines the optimal date and location to book the patients’ appointments, with a score provided to show the associated value of the decisions made. Our dataset from 519 patients showed optimal prioritization based on location, risk of serious vision loss/damage and the referral-to-treatment time. Given the constraints of available slots, managers can input hospital-specific parameters such as demand and capacity into our model. The model can be applied and implemented immediately, without the need for additional software, to generate an optimized patient schedule.
Similar content being viewed by others
Introduction
Healthcare systems are under increasing pressure due to the rising demand and expenditures for healthcare. This problem is compounded by the increase in the elderly population together with the increased global burden of vision impairment1. In Wales, UK, the total number of patients in the highest risk category waiting for an outpatient appointment was over 130,000, in January 20222. It is predicted that a 40% rise in the number of ophthalmologists will be required to meet eye care demands by 20403,4. This is due in part to the ageing population and in part to the greater availability of treatments. The COVID-19 pandemic has intensified the need to address this problem5.
As a result of the COVID-19 pandemic, there have been increased breaches in waiting time targets for ophthalmology outpatient clinics6. Prior to the pandemic, such waiting times were already undesirably high due to the backlog resulting from the vast number of patients requiring treatment, compounded by existing inefficient scheduling practices7,8. This is further complicated by the ever-present budgetary restrictions on health services. Missed or delayed appointments of high-risk patients could be mitigated by adopting a transparent and efficient scheduling process for all patients who need treatment. The management of such hospital appointments is typically implemented using a manual, inefficient and time-consuming approach to book patients into available slots.
Manual patient scheduling aims to minimize the time between referral and treatment (referral-to-treatment time; RTT9) for patients booked into available appointment slots, thus prioritizing those with longer, over those with shorter, waiting times. Such a system does not account for the risk of vision loss associated with delay10 and is subject to the potential human errors and inconsistencies associated with a manual process which can cause inefficient time slot allocation. When examined on a large scale, many patients that require immediate care may not be seen until the queue in front of them has subsided, increasing their risks associated with further delay.
Mathematical formulation has been used to provide a solution to the planning problem with input to daily scheduling, with the use of capacity-based constraints11 and incorporation of inherent uncertainty from late cancellations12. A ‘rolling horizon’ or a pre-defined time window in which to book appointments13 has also been used. Previous studies have employed computer modelling using discrete event simulation and optimization methods to improve patient scheduling14,15,16 as well as time-motion analysis to manage workflows17. Others have applied stochastic programming to patient scheduling, an optimization method which accounts for uncertain parameters18,19,20,21. Some studies have employed simulations18,21,22. One such approach showed simulations involving appointment data to allocate slots in clinics whereby the estimated length of the appointment is the main factor in determining when a patient is to be seen22. Others have proposed decision support systems that provide real-time and dynamic assistance to human schedulers based on probability23.
In contrast to previous work, the aim of our study is to optimize the scheduling of ophthalmology patients using an operational research approach that will take the available slots for treating individuals and allocate them based on their location, risk of serious vision loss/damage and the referral-to-treatment time. A tool was developed with the ability to prioritize patients based on these factors and the needs of the user to create a schedule for the patients, using the availability of treatment slots, that can be utilized in the absence of extra, clinic specific, constraints. The tool is designed for use on standard software, maximizing the usability and acceptability in practice. Another novelty of our approach is that a decision maker can find a trade off between these multiple objectives.
A problem statement is described in the methods section (see “Problem statement and algebraic model formulation”).
Results
Table 1 provides an overview of the parameters used in the study, derived from the real-world clinical data, for implementation of the scheduling tool.
Summary of models
Table 2 shows the outcome of the model using the data from Table 1, from 519 patients with their corresponding RTT and risk scores. The number of patients not scheduled computes as \(P-\left({\sum }_{p=1}^{P}{\sum }_{l=1}^{L}{\sum }_{t=1}^{T}\left({x}_{p,l,t}\right)\right)\). This means that we subtract the number of scheduled patients from the total number of patients \(P\). In order to get the remaining RTT or risk score for patients that we introduce a 1-dimensional binary auxiliary variable that indicates whether a patient has or has not been scheduled. We then multiply this vector by the patient-individual \(RT{T}_{p}\) or \({R}_{p}\) value, respectively and calculate the sum product between the auxiliary variables and the parameter vector.
The derivation of the objective functions is based on the selected factor or combination of factors from RTT, distance or risk of scheduled patients, added together to produce a summed score that is referred to as the objective. It is desirable to maximize each of the three factors associated with the patients scheduled, in order to prioritize patients with higher scores. Therefore, the higher the objective scores, the better the solution in terms of the optimization objective.
Table 2 shows the scores generated for RTT, distance and risk when the model is given the objective function, or combination objective functions, shown on the leftmost column to maximize. Using an objective function that incorporates multiple separate parameters summed together will be equivalent to deciding that these selected parameters have equal weighting that is higher than those not selected. For example, in prioritizing risk alone (labelled in Table 2 as ‘R’), the model will maximize the risk objective and produce a score of 235,940, whilst the objective functions of RTT and distance, labelled here as D, produce scores of 7334 and 8751 respectively. On the other hand, if we were to choose the objective function that assigns equal weighting to distance and risk, i.e., prioritizes distance and risk, then the three base objective functions will produce scores of 7363, 13,404 and 235,940.
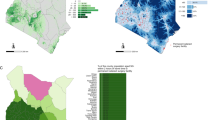
In Fig. 1, an overview of the RTT reduction is provided and broken down by each model that we solve. For example, solving the model with the objective to minimise RTT, the RTT reduction (in weeks) is 8746. In contrast, if the risk-related objective is pursued, then we have an RTT reduction of only 7344 weeks. Similarly, Figs. 2 and 3 provide an overview of the distance reduction and risk reduction, respectively. Evidently, if risk reduction is the dominating objective, and in addition, distance or RTT reduction was the secondary objective, then the decision maker should use the D + R or RTT + D model, respectively.
Note that the overall lowest risk score occurred when RTT was prioritized. Therefore, if risk factor is the objective that the user wishes to optimize, then it must be allocated a weighting that is higher than at least one other contributing factor in the model. The outcome of prioritizing all factors with equal weightings (i.e. RTT + D + R) resulted in an extremely close, but slightly lower score (235,922) as can be seen in Fig. 3.
In each case, the maximum capacity of patients was reached, as shown in Table 1 (and in Fig. S1 Supplementary Information), which can be seen by comparing the number of patients allocated by the model to the capacities in each location. The outcome implies that the solutions from each objective function are optimal as the model does not leave any spaces to be filled. By ensuring that every slot is filled we can ensure that the model cannot miss patients, which is a result of maximizing the values of each objective.
Discussion
The tool developed in this study can be used to schedule patient appointments in ophthalmology clinics, using standard software that is already available. The tool is based on real-world data and is able to create feasible schedules as long as the capacities of the clinics for each day can be reliably met. Testing of the model shows that an optimal patient appointment schedule can be met whilst accounting for the key factors of distance between patients and clinics, RTT dates and individual patients risk factors, the former is becoming increasingly important due to government guidelines concerning the delivery of care closer to home24. Utilizing this tool will help reduce the effect that these factors have on the care of patients in order of priority that is to be determined by the user, or simply all factors together at once.
In order to apply the model in practice, schedulers would use the tool similar to a rolling-horizon planning fashion25. Every day, patient requests would be collected and added to the patient waiting list. Then, at the end of the day, patients scheduled from the list would get a notification about their day and location of appointment. This can also be done on a weekly basis i.e., collecting patient requests until the end of a week and then at the beginning of the new week, patient notifications would be sent to the patients.
In recent years factors such as ageing populations and the improved early detection of medical issues have highlighted the importance that hospital capacities are met, and new ways of solving the problem are required. With the presence of the COVID-19 pandemic, this problem is only becoming more evident amongst healthcare providers26,27,28, due to the rapid influx of patients29. Therefore, the increased use of tools, such as the one described in this study, that incorporate an operations research approach would help to streamline patient scheduling in medical departments. The tool presented here is flexible in that it can be adjusted to apply to different scenarios. It has a fast running time, within seconds, and is scalable for larger datasets.
The implementation of operations research in healthcare has received much attention in recent years30,31,32. Operations research models have been implemented previously in patient scheduling33. A common theme in such studies is that the goal is to optimize the resources of a clinic in each day34 reduces patient wait times. The tool described in the present study differs to the previous work in that it determines which patients should be seen first and can account for a backlog of patients that cannot be seen on a particular day. In this study, changing the objective that the user wishes to optimize can greatly change the final result of the model. Based on data from three hospital clinics in Wales, our results show that the optimal method of generating the highest overall score from the objective functions is to give all three factors equal weighting. In the computational study, risks R1, R2 and R3 were given values of 1000, 10 and 1, respectively. As a consequence, this objective is prioritized if the RTT or distance does not exceed 1000 (weeks or miles). Scaling these values differently may lead to different solutions. This reflects the feature that the patients who qualify for the highest risk category are those who require treatment as soon as possible, therefore the goal of prioritizing high-risk patients is upheld. Automated systems implemented in patient scheduling are advantageous relative to a manual approach11,12,16,20,35,36,37,38.
The study does not evidence the performance or need of the proposed tool. There are further limitations to this study: (1) the scheduling tool does not allow for allocating patients a specific time slot on a given date; (2) the model assumes that the number of patients that can be seen stays at the capacity and so does not account for changes in staff, for example due to sick leave; (3) if a patient misses the appointment given, re-allocation would require running the model again.
The above limitations can be overcome. Many studies have been conducted on the topic of scheduling patients to specific time slots39,40 and if the user so desired, it would be possible to create an additional model, similar to the one presented here, that is to be used after the original model has been run. This new model would use specific time slots in a day for a given clinic instead of separate days and the data would have to change from clinic capacities to the number of patients that can be seen to at the corresponding time slot.
Issues related to capacity variations would be mitigatable in the real-world application of the model by the planning of the user. This ensures that changes in the number of staff and treatment availability can be assumed to be negligible when creating a scheduling tool as accounting for such variations can add a layer of complexity to the model. Therefore, such complexity is a potential barrier to the accessibility of the tool.
To reduce the number of patients that miss their scheduled appointment date, allowing patients to select a specific date is possible within the model in this study. Alternatively, a user would be able to run the model and inform patients scheduled to the first available date before any others, in order to determine whether or not the date is acceptable, run the model again with the confirmed patients already allocated and repeat the process until the schedule is complete.
Another open question is how to scale the risk score and how to provide a normalised comparison of the risk score against RTT and distance, if the objective functions are combined. In this study, we have chosen 1, 10 and 1000 for low, medium and high risk score, respectively. In our particular case this avoids that scheduling for example 200 patients with medium risk score outweigh one patient scheduled with high risk score. Flexibility is, however, provided for low and medium risk score where we would allow multiple patients scheduled with a low risk score may outweigh patients scheduled with a medium risk score. This is, however, up to the discretion of the scheduler whether it is, from a clinical point of view, acceptable that this outweighing behaviour takes place. Another issue is the comparison between the different measures. When we combined the objectives in the case study, we gave each of the objectives the same weight. However, a healthcare organisation may have different priorities how to weight each of the objectives. For example, it might be better to give the risk reduction the highest weight, give RTT reduction the second highest weight and the distance minimization a low weight.
In summary, the tool created for this study will allow users to streamline their patient scheduling in order to allow for priority to be given under specified circumstances, without the need to obtain specialist software. This study used data gathered from hospital clinics in the UK to provide an example of how the tool can be implemented in a set of clinics, over a specified time horizon, to show how multiple different objectives, or weighted combinations of them, can be maximized in order to optimize the specific needs of the user. Future work involving comparing the optimization presented here with current manual scheduling will help to inform the utility, validity and sustainability of the tool, as well as the applicability to other areas of healthcare. Consideration of the cost-effectiveness of the tool would address the need for easily scalable strategies given increasing demands on services and limited resources, as well as evaluation of the potential to improve health outcomes. As a consequence, the tool has the potential to help clinics to improve their service and ensure that key patients are seen before their condition gets worse, improving the overall quality of care that can be achieved.
Methods
We approach the problem of planning the patient schedule of ophthalmology clinics using an Integer Linear Programming formulation41, in which a real-world problem is expressed in terms of linear inequalities. The model was designed using the Microsoft Excel add-in OpenSolver. Anonymized data were obtained from three National Health Service hospital eye clinics in Wales and included the capacities and patient numbers from the clinics. The protocol was approved by the Aneurin Bevan University Health Board (ref no. SA/1272/21), who granted permission for access to data and all methods were carried out in accordance with the relevant guidelines and regulations. Informed consent was not required on the basis that all data were fully anonymised.
The model includes, over a predetermined planning horizon: a given number of patients that each have an assigned referral-to-treatment time, a given distance factor between the patient and the clinics, and associated risk factor, which is to be determined by the patient’s treatment provider. The model is designed to allocate patients to time slots within clinics that have fixed patient capacities for each day. The model assumes shared electronic medical records between clinics.
In addition to the real data used by the model, further data to represent the distance travelled by each patient were sampled from a uniform distribution with lower and upper bounds of 1 and 50, respectively. These numbers represent a ‘distance score’ rather than a precise distance as it is desirable to design the model to maximize each objective function, rather than minimizing exact distances. Therefore, a higher ‘distance score’ indicates the patient is located closer to the specific clinic. In application, these scores will be replaced by the appropriate distance scores of each patient individually. The correlation between distance score and real numerical distance can be determined by the decision maker based on how far the range of patient travel distances is, i.e., in some cases patients may all be within a mile of all clinics whereas in other cases they may be within 10 miles of clinics.
The risk factor for a patient is defined in different categories by eye care services in Wales42. R1 indicates “risk of irreversible harm or significant patient adverse outcome if target date is missed”, e.g., neovascular age-related macular degeneration; R2 indicates “risk of reversible harm or adverse outcome if target date is missed”, e.g., cataract; and R3 as “no risk of significant harm or adverse outcome”, e.g., eyelid lesion with no malignancy suspected. In the model R1, R2 and R3 were represented by 1, 100 and 1000, respectively, as these values, when used in the model, give adequate numerical separation, to appropriately prioritize those in higher risk categories.
The model assumes that patients can be treated within a standard appointment duration43, allowing for the use of clinic capacities instead of minute-by-minute time scheduling. The model considers:
-
Patient referral-to-treatment (RTT) time
-
Risk factor associated with patient’s treatment being further delayed (R1, R2, or R3)
-
Clinic capacities
-
Distance score that corresponds to the distance that the patient must travel to reach the clinic
-
Relative weighting of the above objectives for prioritization, depending on the specific circumstances and user’s needs
Decisions to be made by the model
The model is able to decide the clinic and date that the patient is to be allocated within the time horizon. Consequently, the model will decide who will be seen and, if capacity is scarce, who must still wait. As the clinics have fixed capacities for each day it will be the decision of the clinic staff to provide the specific time at which the patient is to be seen. Depending on the requirements of the user, the planning horizon can be made longer or shorter. In this study, the model is applied using patient numbers that exceed clinic capacities to ensure that the prioritization of patients at greatest risk.
Objective functions and constraints
The model allows the user to maximize the score associated with a given patient’s risk factor, in order to prioritize those who have the largest risk of serious damage as compared to patients with a low eye care risk. This was undertaken using a large binary matrix that indicates for each patient whether or not they will be allocated a unique clinic. The binary values are multiplied by, depending on the objective, the RTT, distance or eye care risk score and then summed to give the final objective value. The constraints of the model ensure that patients cannot be allocated to more than one slot and that the total number of patients scheduled cannot exceed the clinic’s capacity for a given date. Although the model considers a unique objective (RTT, distance or eye care risk score), it can also allow for the user to find a trade off between the measures by using a combination of two, or all three objectives. This, in practice, meets the different demands of specific users.
Problem statement and algebraic model formulation
In order to state the problem, we introduce the sets, indices, and other parameters to algebraically state the problem. Let \({\mathcal{P}}\) denote the set of patients and let \({\mathcal{T}}\) denote the set of days with \(T\) representing the last day in the planning horizon in which patients can be assigned to clinics. For example, \({\mathcal{T}}: = \left\{ {1,2,3 \ldots ,T} \right\}\) represents the set of days labeled as day 1, day 2 etc. until the last day \(T\). Next, we have a set of locations \({\mathcal{L}}\) where clinics take place. We also introduce \({C}_{l,t}\) as the capacity of a clinic at location \(l\in {\mathcal{L}}\) at day \(t\in {\mathcal{T}}\). Patient-dependent parameters are \(RT{T}_{p}\) which denote the referral-to-treatment time of patient \(p\in {\mathcal{P}}\). Furthermore, \({R}_{p}\) denotes the eye-care risk measure of patient \(p\in {\mathcal{P}}\). Finally, \({D}_{p,l}\) denotes the distance (score) that patient \(p\in {\mathcal{P}}\) has to travel if their appointment is scheduled at location \(l\in {\mathcal{L}}\).
We introduce binary decision variables \({x}_{p,l,t}\)=1 if patient \(p\in {\mathcal{P}}\) has a scheduled appointment at location \(l\in {\mathcal{L}}\) at day \(t\in {\mathcal{T}}\) and 0 otherwise.
We consider three objective functions to schedule patients based on their RTT value, their risk measure, and distance to the clinics denoted as RTT, Risk, and Distance, respectively:
The constraints are:
Constraints (1) ensure that a patient is not scheduled more than once at a location while Constraints (2) ensure that the location- and day-dependent capacity is not exceeded. Expression (3) are the decision variables and the domains.
Fig. S2 (Supplementary Information) shows how the objective function and constraints are entered into the solver. There is the possibility to use either one objective or to aggregate multiple objectives. The objective cell will be the value that we want to maximize, such as reduction in the total of patient risk factor values. In this iteration of the model the user has the option of seven objectives, as shown in Fig. 4.
As can be seen, the model uses binary values to represent the decision variables. These are then aggregated in the individual objective function. These objectives are the sum of different values, i.e., the relevant values are added together. The RTT, Distance, and Risk can also be explained as follows:
-
RTT—the RTT number associated with each patient that has been scheduled summed.
-
Distance—the sum of the distances the patients travel to the slot/clinic that they have been assigned.
-
Risk—the total risk score that a clinic accumulates in each day by scheduling patients is calculated.
The model is able to provide a solution which allows for prioritization of each of the above objectives, in addition to a combination of any two, or all three, of these, giving seven possible prioritization outcomes/ combinations to choose from. The user can decide which of these seven objectives they wish to use by changing the objective cell in the model.
The variable cells will be the cells that correspond to where the patients will be allocated. The data should be structured in Microsoft Excel such that, a row is allocated to each patient and a column to each possible allocation location (see Fig. S3 in Supplementary Information). Constraints will determine as to the values that the model can generate for these cells and these cells in turn will give the objective functions when combined with the relevant data in the objective function formulas.
In the example ‘Solver’ outcome in Fig. S3, each row represents a different patient and each column is a possible allocation for the patient, i.e. clinics A, B and C on dates 1,…,6. The objective function then aggregates all decisions i.e. whether patients are scheduled or not and multiplies them with the corresponding RTT, risk or distance measure.
The first constraint ensures that the values in the variable cells will be ‘1’, i.e., the patient is allocated this slot, or ‘0’, i.e., no allocation. The second constraint ensures that a patient cannot be given more than one appointment and the final constraint ensures that the number of patients scheduled to a clinic on a specific date cannot exceed the given capacity. Here, the number of patients scheduled is the sum of values in each column. As a result of the first two constraints, each patient can have at most a single ‘1’ in each row.
Data availability
The dataset generated during the current study is available from the corresponding author on reasonable request.
References
Flaxman, S. R. et al. Vision Loss Expert Group of the Global Burden of Disease Study. Global causes of blindness and distance vision impairment 1990–2020: A systematic review and meta-analysis. Lancet Glob. Health. 5, 1221–1234 (2017).
StatsWales. Patients waiting for an ophthalmology outpatient appointment. 2022. https://statswales.gov.wales/Catalogue/Health-and-Social-Care/NHS-Hospital-Waiting-Times/Eye-care/eyecaremeasuresfornhsoutpatients. Accessed October 2022.
The Royal College of Ophthalmologists. New RCOphth Workforce Census illustrates the severe shortage of eye doctors in the UK. 2021. https://www.rcophth.ac.uk/2019/01/new-rcophth-workforce-census-illustrates-the-severe-shortage-of-eye-doctors-in-the-uk/. Accessed October 2022.
The Royal College of Ophthalmologists. The Way Forward Resources - The Royal College of Ophthalmologists. 2021. https://www.rcophth.ac.uk/standards-publications-research/the-way-forward/. Accessed October 2022.
Wickham, L. et al. The impact of COVID policies on acute ophthalmology services—experiences from Moorfields Eye Hospital NHS Foundation Trust. Eye 34, 1189–1192 (2020).
Ting, D. S. J., Deshmukh, R., Said, D. G. & Dua, H. S. The impact of COVID-19 pandemic on ophthalmology services: Are we ready for the aftermath?. Ther. Adv. Ophthalmol. 12, 2515841420964099 (2020).
Xie, Z. & Or, C. Associations between waiting times, service times, and patient satisfaction in an endocrinology outpatient department: A time study and questionnaire survey. Inquiry J. HealthC. Org. Provision Financ. 54, 3952 (2017).
Walker, K. et al. Displaying emergency patient estimated wait times: A multi-centre, qualitative study of patient, community, paramedic and health administrator perspectives. Emerg. Med. Australas. 33, 425–433 (2020).
NHS Wales. RTT Patient perspective what is it? What do I need to know? 2021. http://www.wales.nhs.uk/sitesplus/documents/866/Final-RTT-rules-Patient-perspective-only-April-2017.pdf. Accessed October 2022.
Foot, B. & MacEwen, C. Surveillance of sight loss due to delay in ophthalmic treatment or review: Frequency, cause and outcome. Eye (Lond) 31, 771–775 (2017).
Turkcan, A., Zeng, B. & Lawley, M. Chemotherapy operations planning and scheduling. IIE Trans. Healthcare Syst. Eng. 2, 31–49 (2012).
Benzaid, M., Lahrichi, N. & Rousseau, L. M. Chemotherapy appointment scheduling and daily outpatient-nurse assignment. Health Care Manag. Sci. 23, 34–50 (2020).
Rohleder, T. R. & Klassen, K. J. Rolling horizon appointment scheduling: A simulation study. Health Care Manag. Sci. 5, 201–209 (2002).
Hribar, M. et al. Data-driven scheduling for improving patient efficiency in ophthalmology clinics. Ophthalmology 126, 347–354 (2019).
Ahmadi-Javid, A., Jalali, Z. & Klassen, K. J. Outpatient appointment systems in healthcare: A review of optimization studies. Eur. J. Oper. Res. 258, 3–34 (2017).
Santibáñez, P. et al. Operations research methods improve chemotherapy patient appointment scheduling. Jt Comm. J. Qual. Patient Saf. 38, 541–553 (2012).
Baxter, S. et al. Time requirements of paper-based clinical workflows and after-hours documentation in a multispecialty academic ophthalmology practice. Am. J. Ophthalmol. 206, 161–167 (2019).
Berg, B. P., Denton, B. T., Erdogan, S. A., Rohleder, T. & Huschka, T. Optimal booking and scheduling in outpatient procedure centers. Comput. Oper. Res. 50, 24–37 (2014).
Mancilla, C. & Storer, R. A sample average approximation approach to stochastic appointment sequencing and scheduling. IIE Trans. 44, 655–670 (2012).
Oh, H. J., Muriel, A., Balasubramanian, H. & Atkinson, K. Ptaszkiewicz T Guidelines for scheduling in primary care under different patient types and stochastic nurse and provider service times. IIE Trans. Healthc. Syst. Eng. 3, 263–279 (2013).
Saremi, A., Jula, P., ElMekkawy, T. & Wang, G. G. Appointment scheduling of outpatient surgical services in a multistage operating room department. Int. J. Prod. Econ. 141, 646–658 (2013).
Srinivas, S. & Salah, H. Consultation length and no-show prediction for improving appointment scheduling efficiency at a cardiology clinic: A data analytics approach. Int. J. Med. Informatics 145, 104290 (2021).
Millhiser, W. P. & Veral, E. A. A decision support system for real-time scheduling of multiple patient classes in outpatient services. Health Care Manag. Sci. 22, 180–195 (2019).
Welsh Government. A healthier Wales: long term plan for health and social care (2021). https://gov.wales/healthier-wales-long-term-plan-health-and-social-care. Accessed October 2022.
Gartner, D. & Padman, R. Flexible hospital-wide elective patient scheduling. J. Oper. Res. Soc. 71, 878–892 (2020).
World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) (2021). https://www.who.int/publications/i/item/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19). Accessed October 2022.
Weissman, G., Crane-Droesch, A., Chivers, C., Mikkelsen, M. & Halpern, S. Locally informed simulation to predict hospital capacity needs during the COVID-19 pandemic. Ann. Intern. Med. 173, 680–681 (2020).
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 395, 1054–1062 (2020).
Healthcare in the United Kingdom (2021). https://coronavirus.data.gov.uk/details/healthcare. Accessed October 2022.
Bradley, B. et al. Operations research in global health: A scoping review with a focus on the themes of health equity and impact. Health Res. Policy Syst. 15, 32 (2017).
Monks, T. Operational research as implementation science: definitions, challenges and research priorities. Implement. Sci. 11, 81 (2015).
Reuter-Oppermann, M., Nickel, S. & Steinhäuser, J. Operations research meets need related planning: Approaches for locating general practitioners’ practices. PLoS ONE 14, 0208003 (2019).
Luo, L. et al. A discrete event simulation approach for reserving capacity for emergency patients in the radiology department. BMC Health Serv. Res. 18, 452 (2018).
Fitzgerald, K., Pelletier, L. & Reznek, M. A queue-based monte carlo analysis to support decision making for implementation of an emergency department fast track. J. Healthc. Eng. 2017, 6536523 (2017).
Boone, C. E., Celhay, P., Gertler, P., Gracner, T. & Rodriguez, J. How scheduling systems with automated appointment reminders improve health clinic efficiency. J. Health Econ. 82, 102598 (2022).
Paré, G., Raymond, L., Castonguay, A., Grenier Ouimet, A. & Trudel, M. C. Assimilation of medical appointment scheduling systems and their impact on the accessibility of primary care: Mixed methods study. JMIR Med. Inform. 16, e30485 (2021).
Tan, E. et al. Improving the patient booking service to reduce the number of missed appointments at East London NHS Foundation trust community musculoskeletal physiotherapy service. BMJ Open Qual. 6, e000093 (2017).
Woodcock, E. Barriers and facilitators to automated self-scheduling: Consensus from a Delphi Panel of key stakeholders. Perspect. Health Inf. Manag. 19, 1m (2022).
People and technology in the workplace. Washington (National Academy Press, 1991).
Vieira, B. et al. Radiotherapy treatment scheduling: Implementing operations research into clinical practice. PLoS ONE 16, 0247428 (2021).
Gass, S. Linear programming (McGraw-Hill, 1986).
Eye care measures for NHS outpatients (2021). https://gov.wales/sites/default/files/statistics-and-research/2019-06/eye-care-measures-for-nhs-outpatients-quality-report.pdf. Accessed October 2022.
Lee, R. & Bunting, H. Appointment duration in the eye clinic: The same across different subspecialties?. Eye 27, 1224–1225 (2013).
Author information
Authors and Affiliations
Contributions
All authors contributed to writing the main manuscript text, L.E. prepared all the figures. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Evans, L., Acton, J.H., Hiscott, C. et al. An operations research approach to automated patient scheduling for eye care using a multi-criteria decision support tool. Sci Rep 13, 553 (2023). https://doi.org/10.1038/s41598-022-26755-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-26755-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.