Abstract
Hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP) caused by carbapenem-resistant Acinetobacter baumannii (CRAB) are both associated with significant morbidity and mortality in daily clinical practice, as well as in a critical care setting. It is unclear whether colistin susceptible-only Acinetobacter baumannii (CSO AB) is a unique phenotype separate from or a subset of CRAB-associated pneumonia. The aim of this study is to investigate the prevalence of CSO AB pneumonia and compare the presentation and outcome between CSO AB and CRAB-associated pneumonia in critically ill patients. This multicenter retrospective cohort study initially recruited 955 patients with CR-GNB pneumonia. After exclusion, 575 patients left who were ICU-admitted and had CRAB nosocomial pneumonia remained. Among them, 79 patients had CSO AB pneumonia, classified as the CSO AB group. The other 496 patients were classified as the CRAB group. We compared demographic characteristics, disease severity, and treatment outcomes between the two groups. The prevalence of CSO AB among all cases of CRAB pneumonia was 13.74% (79/575). The CSO AB and CRAB groups had similar demographic characteristics and disease severities at initial presentation. The in-hospital mortality rate was 45.6% and 46.4% for CSO AB and CRAB groups, respectively (p = 0.991). The CSO AB group had significantly better clinical outcomes at day 7 (65.8% vs 52.4%, p = 0.036) but longer length of ICU stay (27 days vs 19 days, p = 0.043) compared to the CRAB group. However, other treatment outcomes, including clinical outcomes at day 14 and 28, mortality, microbiological eradication, ventilator weaning, and newly onset dialysis, were similar. In conclusion, CSO AB accounted for 13.74% of all cases of CRAB pneumonia, and the clinical presentation and treatment outcomes of CSO AB and CRAB pneumonia were similar.
Similar content being viewed by others
Introduction
Acinetobacter baumannii (A. baumannii) can cause nosocomial infections involving multiple organ systems, including bloodstream, respiratory tract, urinary tract, skin and soft tissue, and central nervous system infections, among others. Those resulted in significant morbidity and mortality in healthcare institutions around the world1. Among these, A. baumannii-associated ventilator-associated pneumonia (VAP) and bacteremia were the cause of the high mortality rate that was approximately 40–60% within one year2,3,4,5. In addition to multifactorial virulence factors and tenacity for survival in different environments, versatile resistance mechanisms threatening the antibiotic therapy makes A. baumannii infection a critical and troublesome clinical entity6. The advert of carbapenem-resistant organisms such as carbapenem-resistant Acinetobacter baumannii (CRAB), carbapenem-resistant Pseudomonas aeruginosa and carbapenem-resistant Enterobacterales breaks the fortress of carbapenem, a reliable last-resort for antimicrobial therapy, and makes a global public-healthcare problem7. In 2016, the World Health Organization (WHO) announced the priority list of drug-resistant bacteria for research into and development of effective antibiotics; CRAB was indicated as one of the bacteria with the highest priority8.
The treatment for CRAB pneumonia is usually a regimen of single or combination antibiotics, including colistin, tigecycline, sulbactam, carbapenem, amikacin, minocycline, fosfomycin, etc.; promising agents include cefiderocol and eravacycline9,10,11. In CRAB pneumonia, colistin susceptible-only Acinetobacter baumannii (CSO AB) is a subgroup that has not been thoroughly studied. Although colistin is one of the mainstay treatments for CRAB pneumonia and specifically effective for CSO AB pneumonia, CSO AB pneumonia is a clinical entity worthy of discussion. If clinicians could know the epidemiology of CSO AB pneumonia and early detect the risk factors and initial presentations of CSO AB pneumonia in healthcare institutions, early prescription of colistin for critically ill patients before the availability of antimicrobial susceptibilities may lead to better clinical outcomes. In 2007, prior antimicrobial therapy for more than 10 days and a previous VAP episode were reported by Rios to be the independent risk factors of acquiring CSO AB-associated VAP, which clues clinicians into prescribing colistin for critically ill patients relatively early in the disease course12. However, nowadays the prevalence, presentation, and prognosis of CSO AB-associated nosocomial pneumonia in intensive care unit (ICU), which are needed for more effective treatment of resistant A. baumannii infection, are still unclear. For this information gap, we conducted a multicenter retrospective cohort study to investigate the ratio of CSO in CRAB pneumonia, and to compare the clinical manifestation and outcomes between CSO AB and CRAB pneumonia in patients admitted to the ICU.
Methods
Study population and data collection
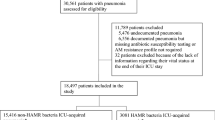
This is a retrospective study conducted in five medical centers in Taiwan13,14. We recruited ICU-admitted patients who were diagnosed with carbapenem-resistant Gram-negative bacterial (CR-GNB) associated pneumonia from Jan. 2016 to Dec. 2016. The study design has been mentioned in the article published by team members15, and we briefly described it in this method section. The CSO AB and CRAB pneumonia were derived from a CR-GNB pneumonia database. The flow diagram of this article for patient inclusion and exclusion is shown in Fig. 1. The inclusion criteria were ICU admission with a diagnosis of nosocomial pneumonia that developed more than 48 h after admission, and the culture of CR-GNB from respiratory specimens that was resistant to at least one kind of tested carbapenems. The exclusion criteria were age younger than 20 years, community-acquired pneumonia or healthcare-associated pneumonia, concomitant lung cancer with obstructive pneumonitis, and non-CRAB pathogens.
The baseline characteristics, disease severities and clinical outcomes were retrieved from the medical records of the five teaching hospitals as listed on the affiliation. The disease severities of recruited patients were assessed by the Sequential Organ Failure Assessment (SOFA) score on the day of ICU admission and pneumonia index date, and the Acute Physiology and Chronic Health Evaluation (APACHE) II score on the day of ICU admission. We also analyzed the parameters associated with the organ dysfunction, including septic shock, PaO2/FiO2 (P/F) ratio, use of mechanical ventilator, and renal replacement therapy, and the laboratory studies including plasma leukocyte, C-reactive protein, albumin and creatinine on the pneumonia index date. Septic shock was defined according to the International Sepsis Definitions Conference in 200116.
Diagnosis of nosocomial pneumonia
Pneumonia was diagnosed upon discovery of new or progressive infiltration, consolidation or patch opacity on chest x ray with at least two clinical observations, including fever (> 38 °C) or hypothermia (< 36 °C), cough, copious or purulent phlegm secretion, leukocytosis (plasma leukocyte > 10,000/mm3), leukopenia (plasma leukocyte < 4000/mm3), or percentage of band form leukocyte > 10%. In this study, we recruited patients with nosocomial pneumonia including hospital-acquired pneumonia which was defined as pneumonia that occurred more than 48 h after hospital admission, and VAP which was defined as pneumonia that developed more than 48 h after endotracheal intubation. We just recorded and collected the first episode of HAP or VAP caused by CRAB infection for subsequent analysis. Eligible specimens were collected from sputum (semi-quantitative method), tracheal aspirates (semi-quantitative method), or bronchoalveolar lavage fluid with a CR-GNB concentration > 104 colony forming units per ml (CFU/mL). We defined the date of specimen collection as the pneumonia index date (pneumonia onset day).
Microbiological tests and therapeutic regimens
The antibiotic susceptibility of the causative A. baumannii was determined based on the Clinical and Laboratory Standards Institute (CLSI) recommendations. Either the BD Phoenix™ system or the VITEK® 2 system was used for antimicrobial susceptibility tests in this study. The antibiotics tested for susceptibility included piperaci/tazoba, ampicillin/sulbactam, cefepime, ceftazidime, levofloxacin, ciprofloxacin, fosfomycin, meropenem, imipenem, doripenem, gentamicin, amikin, tigecycline and colistin. Antimicrobial susceptibility such as colistin, tigecycline, ampicillin/sulbactam, and amikacin for each CRAB was recorded for analysis. A. baumannii was defined as carbapenem-resistant (CRAB) when A. baumannii was resistant to at least one kind of tested carbapenems (meropenem, imipenem, doripenem); A. baumannii was defined as colistin susceptible-only (CSO) when A. baumannii was resistant to all tested antibiotics but only susceptible to colistin. We recorded the antibiotics commonly prescribed for CRAB treatment for baseline characteristic analysis, including carbapenem, colistin (intravenous or inhaled), tigecycline, sulbactam, and amikacin, that should be administered for at least 2 days within 7 days of the pneumonia index date; antibiotics that were administered less than 2 days were not recorded in this study.
Outcomes evaluations
The mortality rate, favorable clinical outcome, and microbiological response at days 7, 14, and 28 were the primary outcomes in the present study. We followed up the patients to discharge and outpatient-department visit according to medical record (retrospectively). We classified the clinical response to treatment as either cure (discontinuation of antibiotic and resolution of symptoms), improvement (continuation of antibiotics treatment and partial resolution of symptoms), or failure (persisted symptoms or decease). The symptoms for the assessment of clinical response included fever or hypothermia, cough, copious or purulent phlegm secretion. The combination of cure and improvement were defined as favorable clinical outcome. We classified the microbiological response as either eradication (no yield of causative pathogens in two or more consecutive respiratory specimens), persistence (persistent yield of causative pathogens in respiratory specimens), recurrence (isolation of causative pathogens again within 14 days of eradication), or undetermined (no follow-up specimen or only one specimen without pathogen growth). We defined the microbiological eradication rate as the ratio between the cases with eradiation and the cases with eradiation, persistence, or recurrence (undetermined was not included).
The 28-day ventilator weaning, newly onset dialysis, length of ICU and hospital stay, and length of stay before and after pneumonia index day were the secondary outcomes. We evaluated nephrotoxicity based on the new need and implementation of dialysis, including hemodialysis (HD) or continuous venovenous hemodialysis (CVVHD) during hospitalization after the pneumonia index date. The analysis of the length of ICU and hospital stays, and length of stay before and after pneumonia index day did not include patients who expired during hospitalization.
Statistical analysis
Continuous variables were analyzed with the Mann–Whitney U test, and categorical variables were analyzed with chi-square test, or Fisher’s exact test. Kaplan–Meier analysis and log-rank tests were applied for comparison of survival between the CRAB and CSO AB groups. Statistical analyses were performed with SPSS software version 18.0 (SPSS Inc., Chicago, IL). A P value ≤ 0.5 was considered statistically significant.
Ethics approval and consent to participate
The present study was approved by the Institutional Review Board (IRB) of the five participating hospitals, including IRB of Taipei Veterans General Hospital (2018-03-001CC), IRB of Tri-Service General Hospital (1-107-05-054), IRB of Kaohsiung Medical University Hospital (KMUHIRB-E(I)-20180141), IRB of China Medical University Hospital (CMUH107-REC3-052) and IRB of Taichung Veterans General Hospital (IRB CE18100A). The need of informed consent was waived by the Institutional Review Boards for the respective essence of this study, and the ethical principles and issues were in accordance with the Declaration of Helsinki.
Results
Prevalence of CSO AB and comparison of demographic characteristics
There were 955 patients with CR-GNB associated pneumonia enrolled initially in this study (Fig. 1). 380 patients were excluded according to the exclusion criteria including diagnosis of CAP/HCAP (64 cases), without ICU admission (156 cases), lung cancer with obstructive pneumonitis (8 cases) and non-CRAB pathogens (152 cases). Finally, 575 patients who were admitted to the ICU with CRAB-associated nosocomial pneumonia remained for following analysis. Among them, 79 cases were classified with CSO AB as the causative pathogen of pneumonia. Thus, the prevalence of CSO AB in CRAB-associated pneumonia in ICU patients is calculated to be 13.74% (79/575).
In Table 1, we compared the demographic characteristics of patients with CRAB and CSO AB pneumonias. Patients with CSO AB pneumonia were significantly more likely to receive intravenous (49.4% vs 29.0%, p = 0.001) or inhaled (50.6% vs 36.3%, p = 0.021) colistin therapy than patients with CRAB pneumonia. However, there was no significant difference between the groups regarding age, sex, body mass index, smoking, alcohol consumption, pneumonia types, ICU type, or comorbidities.
Disease severities at initial presentation
In Table 2, we compared the disease severities, including APACHE II score, SOFA score, septic shock, mechanical ventilation, P/F ratio, dialysis and laboratory studies, and there was no significant difference between CRAB and CSO AB-associated pneumonia. Among these, APACHE II score was recorded at ICU admission; other variables were recorded on the pneumonia index date.
Treatment outcomes
In Table 3, we compared the treatment outcomes between both groups. The in-hospital mortality was similar between CRAB and CSO pneumonia (46.4% vs 45.6%, p = 0.991). With regard to mortality at day 7, 14 and 28, it was similar between both groups. The CSO AB group had a significantly higher ratio of favorable clinical outcomes at day 7 than the CRAB group (65.8% vs 52.4%, p = 0.036), but this difference was not observed at day 14 and 28. The length of ICU stay was significantly longer in the CSO AB group than the CRAB group (27 days vs 19 days, p = 0.043), while the length of hospital stay was similar between groups. Furthermore, there was no significant difference regarding ventilator weaning at day 28, new need for dialysis, or microbiological eradication at day 7, 14, and 28, and the length of stay before and after pneumonia index day. In Fig. 2, the Kaplan–Meier analysis of 28-day survival between both groups shows non-significant difference (log rank test = 0.709).
Discussion
In 2007, Rios etc. observed that prior antimicrobial therapy and VAP are risk factors for acquiring CSO AB-associated VAP12. However, limited studies discussing the prevalence, presentation, disease severity, or outcome of CSO AB pneumonia were published after Rios’s report. This multicenter retrospective cohort study observed 13.74% of CRAB pneumonia were colistin-susceptible-only and patients with CSO AB and CRAB pneumonia had similar demographic characteristics and disease severities at initial presentation. Although patients with CSO AB pneumonia had significantly better clinical outcomes at day 7 and longer length of ICU stay than those with CRAB pneumonia, other treatment outcomes were similar, including clinical outcomes at day 14 and 28, mortality, microbiological eradication, ventilator weaning, and new need for dialysis.
A. baumannii is an concerning pathogen that has a staggering tendency for acquiring antimicrobial resistance to various categories of antibiotics by multiple mechanisms6,17,18. For CRAB in particular, Acinetobacter baumannii acquires carbapenem resistance by synthesis of carbapenemases, alterations in penicillin-binding proteins, loss of outer membrane porins, and overexpression of efflux pumps, among other mechanisms19,20. The A. baumannii resistance to carbapenems has been reported to be increasing during the last decade; more than 50 percent of Acinetobacter baumannii specimens isolated were carbapenem-resistant in most of the country21,22,23; the frequency of CRAB even reached 80–100 percent in south and southeast Asia24. The study regarding the epidemiology of CSO AB pneumonia, a subgroup of CRAB pneumonia, is scarce. Jacob etc. reported Acinetobacter baumannii accounted for 61% of CSO related infections, followed by Klebsiella pneumonia (24.4%), Pseudomonas aeruginosa (12.2%), and Escherichia coli (2.4%) in critically ill patients who were intubated and mechanically ventilated25. Our study further investigated the ratio of colistin-susceptible-only A. baumannii in CRAB pneumonia and observed that 13.74% (79/575) of CRAB were only susceptible to colistin. If clinicians could know the portion or percentage of colistin, tigecycline, or sulbactam-susceptible-only A. baumannii in CRAB infections in their hospitals or countries, appropriate empiric antimicrobial agents could be prescribed early when CRAB infections were suspected, a scenario that can possibly make the difference between mortality and survival in a critical care setting. Furthermore, pandrug-resistance (PDR) A. baumannii is another issue worthy to be concerned. PDR A. baumannii has been increasingly reported worldwide26, which could be, at least in part, associated with the high prevalence (33%) of colistin heteroresistance27 and the emergence of colistin resistance during treatment for A. baumannii infection28. The treatment options for PDR A. baumannii are limited and undetermined, that were primarily relied on the synergistic combination of antimicrobial agents29,30,31. High mortality (in hospital mortality rate: 79%) urges studies in future to investigate the effectively therapeutic regimen for PDR A. baumannii infection32.
Early prediction of CSO AB infection may help achieve better clinical outcomes by allowing early prescription of colistin. The delay of four days or more for colistin initiation lead to increase mortality in patients with VAP caused by CSO AB33. A prior episode of VAP and previous antimicrobial therapy more than 10 days have been reported as independent risk factors for acquiring CSO AB pneumonia12. However, these are also the risk factors for pneumonia caused by other multidrug-resistant pathogens, including CRAB34,35,36; other predictive factors, specific for developing CSO AB pneumonia, need to be identified and reported for clinical use. After comparing many variables representing demographic characteristics (Table 1) and disease severity (Table 2) between CRAB and CSO AB pneumonias, we detected no significant differences at initial presentation. It is worthy to investigate other predictive factors for developing CSO AB pneumonia by large randomized controlled studies in the future.
The in-hospital mortality of CRAB pneumonia in the present study was 46.4% (230/496), which is consistent with Zheng’s report (45.6%)36. We further explored the mortality of CSO AB pneumonia at days 7, 14, and 28, as well as in-hospital mortality, which were similar to that of CRAB pneumonia. A case–control study conducted by Samrah reported the 30-day mortality rate was 46.4% in patients with CSO AB associated VAP33, which was higher than the 28-day mortality rate (34.2) and close to the in-hospital mortality (45.6) of the present study. This disparity could be attributed to different characteristics of enrolled patients, for approximately one fourth were HAP patients in our study, while all patients were VAP in Samrah’s study.
We also observed that patients with CSO AB pneumonia had significantly better clinical outcomes at day 7 compared to patients with CRAB pneumonia. We hypothesize that significantly higher prescription of intravenous or inhaled colistin in the CSO AB group could attribute to this result, based on the evidence that colistin-based therapy may be associated with lower treatment failure rates37. However, the effect of better clinical outcomes at day 7 could not affect the longer ICU stay in patients with CSO AB pneumonia (Table 3), while longer stay in ICU of CSO infection was also reported in Jacob’s study25. We supposed patients with CSO infection may need longer period of intensive care compared to patients with non-CSO infection, but the precise causality needs to be further investigated. Furthermore, although more patients in CSO AB group received intravenous colistin therapy, there was no difference in new need for dialysis between both groups, which may be related to lower treatment failure at day 7 in the CSO AB group (less sepsis-induced kidney injury) or the occurrence of acute kidney injury but without the necessity for hemodialysis.
This is a multicenter study that minimized selection bias by taking different clinical settings and practices into consideration. However, some limitations exist. First, we calculated the prevalence of CSO AB pneumonia (13.74%) by the ratio of CSO to CRAB instead of A. baumannii, and that is analyzed according to the local pathogen data of Taiwan. Thus, the finding should be carefully extrapolated or applied for the concern of different microbial spectrum in different countries. Second, we did not collect prior antimicrobial therapy and previous VAP episode for baseline variable analysis, because these were reported as independent risks for developing CSO AB pneumonia in prior study12. Third, there were no detailed medical records regarding the APACHE II score at the pneumonia index date (only the date at ICU admission), so we could not compare the difference of APACHE II score at the time closest to pneumonia development. However, we analyzed the SOFA score at the pneumonia index date, which is also a good surrogate for disease severity. Fourth, we evaluated renal function impairment in both groups by new need for dialysis instead of acute kidney injury, which may underestimate the incidence of nephrotoxicity due to intravenous colistin, which was prescribed more frequently in the CSO AB group. Fifth, this study only recruited patients with nosocomial pneumonia caused by Acinetobacter baumannii, so the findings cannot be extrapolated to other pathogens. Sixth, polymicrobial infection and co-infection at other site are important issues to differentiate colonization versus true pathogen, and monomicrobial versus polymicrobial infection. However, we did not collect the associated variables for these differentiation. Seventh, the method for antimicrobial susceptibility to colistin was the BD Phoenix™ system or the VITEK® 2 system, instead of broth microdilution, a currently recommended method for colistin susceptibility. Eighth, we did not further apply multivariate analysis for the absence of survival differences in univariate analysis. Ninth, we did not further delineate the different antimicrobial therapeutic regimens in this study. However, we tried to simplify and keep the most essence/representation of regimen by illustrating as Table 1 (Antibiotics prescribed). Finally, due to an observational and retrospective study design, the bias regarding preference of clinicians for prescription of antimicrobial agents existed, such as colistin underused in the CRAB group.
Conclusions
We provided more information regarding CSO AB pneumonia by observing that CSO AB accounted for 13.74% of all CRAB pneumonias, and the clinical presentation, disease severities and treatment outcomes were similar between CSO AB and CRAB pneumonia. Our findings will provide useful information for physicians when facing CSO AB pneumonia in clinical practice.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- A. baumannii :
-
Acinetobacter baumannii
- APACHE:
-
Acute physiology and chronic health evaluation
- CRAB:
-
Carbapenem-resistant Acinetobacter baumannii
- CR-GNB:
-
Carbapenem-resistant Gram-negative bacterial
- CSO AB:
-
Colistin susceptible-only Acinetobacter baumannii
- CVVHD:
-
Continuous venovenous hemodialysis
- HD:
-
Hemodialysis
- ICU:
-
Intensive care unit
- VAP:
-
Ventilator-associated pneumonia
- WHO:
-
World Health Organization
References
Howard, A., O’Donoghue, M., Feeney, A. & Sleator, R. D. Acinetobacter baumannii: An emerging opportunistic pathogen. Virulence 3, 243–250 (2012).
Huang, Y. et al. Acinetobacter baumannii ventilator-associated pneumonia: clinical efficacy of combined antimicrobial therapy and in vitro drug sensitivity test results. Front. Pharmacol. 10, 92 (2019).
Bianco, A. et al. Control of carbapenem-resistant Acinetobacter baumannii outbreak in an intensive care unit of a teaching hospital in Southern Italy. BMC Infect. Dis. 16, 747 (2016).
Wisplinghoff, H. et al. Nosocomial bloodstream infections due to Acinetobacter baumannii, Acinetobacter pittii and Acinetobacter nosocomialis in the United States. J. Infect. 64, 282–290 (2012).
Vivo, A. et al. Epidemiology and outcomes associated with carbapenem-resistant Acinetobacter baumannii and carbapenem-resistant Pseudomonas aeruginosa: A retrospective cohort study. BMC Infect. Dis. 22, 491 (2022).
Ayoub Moubareck, C. & Hammoudi, H. D. Insights into Acinetobacter baumannii: A review of microbiological, virulence, and resistance traits in a threatening nosocomial pathogen. Antibiotics (Basel, Switzerland) 9, 1 (2020).
Meletis, G. Carbapenem resistance: Overview of the problem and future perspectives. Ther. Adv. Infect. Dis. 3, 15–21 (2016).
Tacconelli, E. et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect. Dis. 18, 318–327 (2018).
Wunderink, R. G. et al. Cefiderocol versus high-dose, extended-infusion meropenem for the treatment of Gram-negative nosocomial pneumonia (APEKS-NP): A randomised, double-blind, phase 3, non-inferiority trial. Lancet Infect. Dis. 21, 213–225 (2021).
Van Hise, N. et al. A real-world assessment of clinical outcomes and safety of eravacycline: A novel fluorocycline. Infect. Dis. Ther. 9, 1017–1028 (2020).
Piperaki, E. T., Tzouvelekis, L. S., Miriagou, V. & Daikos, G. L. Carbapenem-resistant Acinetobacter baumannii: in pursuit of an effective treatment. Clin. Microbiol. Infect. 25, 951–957 (2019).
Rios, F. G. et al. Ventilator-associated pneumonia due to colistin susceptible-only microorganisms. Eur. Respir. J. 30, 307–313 (2007).
Feng, J. Y. et al. Efficacy of adjunctive nebulized colistin in critically ill patients with nosocomial carbapenem-resistant Gram-negative bacterial pneumonia: A multi-centre observational study. Clin. Microbiol. Infect. 27, 1465–1473 (2021).
Wang, S. H. et al. The necessity of a loading dose when prescribing intravenous colistin in critically ill patients with CRGNB-associated pneumonia: A multi-center observational study. Crit. Care (London, England) 26, 91 (2022).
Chen, C. Y. et al. Clinical outcome of nosocomial pneumonia caused by Carbapenem-resistant gram-negative bacteria in critically ill patients: A multicenter retrospective observational study. Sci. Rep. 12, 7501 (2022).
Levy, M. M. et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit. Care Med. 31, 1250–1256 (2003).
Lee, C. R. et al. Biology of Acinetobacter baumannii: Pathogenesis, antibiotic resistance mechanisms, and prospective treatment options. Front. Cell. Infect. Microbiol. 7, 55 (2017).
Kyriakidis, I., Vasileiou, E., Pana, Z. D. & Tragiannidis, A. Acinetobacter baumannii antibiotic resistance mechanisms. Pathogens (Basel, Switzerland) 10, 1 (2021).
Nguyen, M. & Joshi, S. G. Carbapenem resistance in Acinetobacter baumannii, and their importance in hospital-acquired infections: A scientific review. J. Appl. Microbiol. 131, 2715–2738 (2021).
Poirel, L. & Nordmann, P. Carbapenem resistance in Acinetobacter baumannii: mechanisms and epidemiology. Clin. Microbiol. Infect. 12, 826–836 (2006).
Lob, S. H., Hoban, D. J., Sahm, D. F. & Badal, R. E. Regional differences and trends in antimicrobial susceptibility of Acinetobacter baumannii. Int. J. Antimicrob. Agents 47, 317–323 (2016).
Asif, M., Alvi, I. A. & Rehman, S. U. Insight into Acinetobacter baumannii: Pathogenesis, global resistance, mechanisms of resistance, treatment options, and alternative modalities. Infect. Drug Resist. 11, 1249–1260 (2018).
Zilberberg, M. D., Kollef, M. H. & Shorr, A. F. Secular trends in Acinetobacter baumannii resistance in respiratory and blood stream specimens in the United States, 2003 to 2012: A survey study. J. Hosp. Med. 11, 21–26 (2016).
Hsu, L. Y. et al. Carbapenem-resistant Acinetobacter baumannii and Enterobacteriaceae in South and Southeast Asia. Clin. Microbiol. Rev. 30, 1–22 (2017).
Jacob, I., Rangappa, P., Thimmegowda, L. C. & Rao, K. A study of multidrug-resistant, colistin-only-sensitive infections in intubated and mechanically ventilated patients over 2 years. J. Glob. Infect. Dis. 12, 5–10 (2020).
Karakonstantis, S., Kritsotakis, E. I. & Gikas, A. Pandrug-resistant Gram-negative bacteria: A systematic review of current epidemiology, prognosis and treatment options. J. Antimicrob. Chemother. 75, 271–282 (2020).
Karakonstantis, S. & Saridakis, I. Colistin heteroresistance in Acinetobacter spp.: systematic review and meta-analysis of the prevalence and discussion of the mechanisms and potential therapeutic implications. Int. J. Antimicrob. Agents 56, 106065 (2020).
Karakonstantis, S. A systematic review of implications, mechanisms, and stability of in vivo emergent resistance to colistin and tigecycline in Acinetobacter baumannii. J. Chemother. (Florence, Italy) 33, 1–11 (2021).
Karakonstantis, S., Ioannou, P. & Kofteridis, D. D. In search for a synergistic combination against pandrug-resistant A. baumannii; methodological considerations. Infection 50, 569–581 (2022).
Karakonstantis, S., Ioannou, P., Samonis, G. & Kofteridis, D. P. Systematic review of antimicrobial combination options for pandrug-resistant Acinetobacter baumannii. Antibiotics (Basel, Switzerland) 10, 1 (2021).
Karakonstantis, S., Kritsotakis, E. & Gikas, A. Treatment options for K. pneumoniae, P. aeruginosa and A. baumannii co-resistant to carbapenems, aminoglycosides, polymyxins and tigecycline: An approach based on the mechanisms of resistance to carbapenems. Infection 48, 835–851 (2020).
Karakonstantis, S., Gikas, A., Astrinaki, E. & Kritsotakis, E. I. Excess mortality due to pandrug-resistant Acinetobacter baumannii infections in hospitalized patients. J. Hosp. Infect. 106, 447–453 (2020).
Samrah, S. et al. Impact of colistin-initiation delay on mortality of ventilator-associated pneumonia caused by A. baumannii. J. Infect. Dev. Countries 10, 1129–1134 (2016).
Watkins, R. R. & Van Duin, D. Current trends in the treatment of pneumonia due to multidrug-resistant Gram-negative bacteria. F1000Research 8, 1 (2019).
Xia, J. et al. A retrospective analysis of carbapenem-resistant Acinetobacter baumannii-mediated nosocomial pneumonia and the in vitro therapeutic benefit of cefoperazone/sulbactam. Int. J. Infect. Dis. 23, 90–93 (2014).
Zheng, Y. L. et al. Risk factors and mortality of patients with nosocomial carbapenem-resistant Acinetobacter baumannii pneumonia. Am. J. Infect. Control 41, e59-63 (2013).
Liang, C. A. et al. Antibiotic strategies and clinical outcomes in critically ill patients with pneumonia caused by carbapenem-resistant Acinetobacter baumannii. Clin. Microbiol. Infect. 24, 908 (2018).
Acknowledgements
We thank professor Yu-Ching Chou’s team from the School of Public Health, National Defense Medical Center, Taipei, Taiwan, for statistical and methodological advice.
Funding
This study, in part, was financially supported by the grants from Tri-Service General Hospital, Taipei, Taiwan (Grant Numbers: TSGH-D-110050, TSGH-C108-217, and TSGH-E-111231), and Medical Affairs Bureau Ministry of National Defense, Taiwan (Grant Numbers: MND-MAB-C-11116-111057).
Author information
Authors and Affiliations
Contributions
Conceptualization: J.Y.F., S.H.W., C.K.P., C.C.S., Y.C.L., M.C.C., K.Y.Y. Data curation: C.K.P., J.Y.F., C.M.C., C.Y.C., Z.R.Z. Formal analysis: S.H.W., C.K.P., Y.C.C. Methodology: S.H.W., C.K.P., J.Y.F., C.C.S., Y.C.L., M.C.C., K.Y.Y., Y.C.C. Project administration: C.K.P., C.C.S., Y.C.L., M.C.C., K.Y.Y. Supervision: C.K.P., C.C.S., Y.C.L., M.C.C., K.Y.Y. Validation: C.K.P., C.C.S., Y.C.L., M.C.C., K.Y.Y. Writing—original draft: S.H.W., C.K.P. Writing—review and editing: S.H.W., C.K.P., J.Y.F., C.C.S., C.M.C., Y.C.L., C.Y.C., M.C.C., Z.R.Z., K.Y.Y.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
This retrospective study waived the consent from participants approved by the Institutional Review Boards.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, SH., Yang, KY., Sheu, CC. et al. The prevalence, presentation and outcome of colistin susceptible-only Acinetobacter Baumannii-associated pneumonia in intensive care unit: a multicenter observational study. Sci Rep 13, 140 (2023). https://doi.org/10.1038/s41598-022-26009-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-26009-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.