Abstract
Wage earning in low- and middle-income countries (LMICs) is predominantly through physical labour. Consequently, limb-related disabilities caused by abnormal fracture unions (AFUs) preclude gainful employment and perpetuate the cycle of poverty. Many AFUs result from traditional bone-setting (TBS), a pervasive treatment for long bone fractures in LMICs. The objective of this study was to accentuate the expediency of solid locked intramedullary nail in the early restoration of victims of TBS-induced abnormal fracture unions (AFUs) to their pre-injury functioning, including work. One hundred AFUs in 98 patients treated with a solid locked intramedullary nail in our center over a period of 7 years were prospectively studied. We found the mean age to be 47.97 years. Males constituted 63.9% of the patients’ population. Atrophic non-union accounted for 54.1% of the AFUs. The mean fracture-surgery interval was 21.30 months. By the 12th post-operative week, more than 75% of the fractures had achieved knee flexion/shoulder abduction beyond 90°, were able to squat and smile (or do shoulder abduction-external rotation), and were able to bear weight fully. The study demonstrated the expediency of solid locked nail in salvaging TBS-induced abnormal fracture unions in a way that permitted early return to pre-injury daily activities and work, thereby reducing fracture-associated poverty.
Similar content being viewed by others
Introduction
Socioeconomic functioning in low- and middle-income countries (LMICs) often requires a good ambulatory capacity and satisfactory use of the upper limbs since wage earning is predominantly through physical labour. Hence, limb-related disabilities render an individual incapable of gainful employment and perpetuate the cycle of poverty1. Therefore, poverty-mitigating fracture care in LMICs must allow early use of the limbs to foster prompt return to pre-injury daily activities and work. This is particularly desirable in victims of abnormal fracture unions (AFUs) whose disability has often resulted in psychological distress, social and economic costs in terms of loss of work days and eventual higher cost of effective treatment2,3,4. A faster functional recovery and return to work which can lessen the economic impact of an injury requires early weight bearing (WB)5. In high income countries, various newer strategies that ensure quicker restoration of function are now available to treat AFUs but these are currently non-existent in most LMICs6,7,8. Thus, most surgeons in LMICs have continued to treat AFUs with methods which are less compatible with early WB. These include external fixation, and internal fixation using plates or unlocked intramedullary (IM) nails9,10,11,12.
Long bone fractures have been turned into an epidemic by rapid urbanizations, increased use of motorized vehicles and incessant violent incidents in many LMICs. Regrettably, traditional bone-setting (TBS) has continued to flourish in LMICs as the first line (or the only) care for these injuries. This is due to superstitious beliefs, ignorance, cultural norms, poor orthodox health system and high cost of modern fracture care facilities2,9,13,14. Traditional bonesetters are found in most communities of developing countries13,14,16. These are unorthodox practitioners without any training in a formal, medical education setting, having inherited their purported skills from older generations in the family15,16. While a few previous authors identified some usefulness of TBS13,17, most other studies have established havocs done to the injured by bonesetters18,19. Limb gangrene, tetanus, chronic bone infection or eventual fatality are the most devastating disasters of TBS18,19. However, also associated with the practice is disability caused by AFUs, including delayed union, mal-union and non-union10,20.
Controversies exist about the standard definition but the term ‘non-union’ has recently been applied to a fracture which shows no progressive signs of healing after three months of treatment3,6,21,22. Atrophic non-union means a fracture site is devoid of healing potential with accompanying dearth of callus, usually as a result of biological factors. The fracture has only minimal amounts of callus in oligotrophic non-unions due to inadequate immobilisation while hypertrophic non-union is characterized by exuberant callus formation but in a disorganized manner, due to inadequate mechanical stability3. Mal-union describes a fracture that healed non-anatomically with resultant length, alignment or angular deformities and, often functional impairment10. Delayed union applies to a fracture which in spite of progressing towards union, has not healed in the expected amount of time for a comparable fracture22.
In this study, we present the data on patients who had their TBS-induced AFUs fixed with the Surgical Implant Generation Network’s (SIGN) locked IM nail in our centre. The aim is to accentuate the expediency of solid locked IM nail in early restoration of victims of TBS AFUs in LMICs to their pre-injury functioning, including work.
Methods
Study site
The study was carried out at Bowen University Teaching Hospital, Ogbomoso, a semi-urban city located in South-Western Nigeria. The city is inhabited by artisans, civil servants, subsistence farmers and small business owners. The hospital serves other nearby villages/towns composed of similar populations.
Study design
Over a period of 7 years (July 2014 to June 2021), we used the SIGN locked IM nail to treat a total of 100 fractures of the humerus, femur and tibia in 98 patients. All the fractures were TBS-induced AFUs. Using a descriptive study design, data were collected prospectively on all the fractures. The data included patient and fracture characteristics, as well as treatment outcome. The data were analysed with SPSS version 23 (IBM Corp, New York, USA) and presented as descriptive statistics in tables and figures.
The standard occupational classification system designed by the Office of Population Census and Surveys, London (OPCS 1991)23 and modified for Nigeria24 was used to classify the patients into occupational classes 1 to 3 as follows:
-
Class 1—Skilled workers e.g. professionals and managerial officers and retirees of this cadre.
-
Class 2—Unskilled workers e.g. artisans and traders.
-
Class 3—Dependants. e.g. retirees of class 2, those not on pensions, house wives of class 2 cadre, students.
Fracture location and morphology were defined according to AO/OTA guideline25. Abnormal unions were grouped into atrophic non-union (≥ 3 months, scanty or no callus on plain radiograph, motion at fracture site)3,6,22, hypertrophic non-union (≥ 3 months, excessive callus on plain radiograph, motion at fracture site)3,6,22, mal-union (healed but mal-aligned or shortened)10, and delayed union (< 3 months, no clinical or radiographic evidence of ongoing healing)22. The time length between the occurrence of fracture and performance of surgery (fracture-surgery interval) was grouped into: ≤ 3 months, > 3 but ≤ 6 months, > 6 but ≤ 9 months, > 9 but ≤ 18 months, and > 18 months. The time length between skin incision and closure (duration of surgery) was categorized into: within 1 h, within 2 h, within 3 h, within 4 h, and > 4 h (Table 2).
Operative and post-operative care
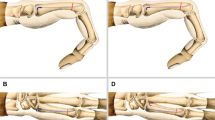
Following satisfactory routine pre-operative work-up, each patient underwent a one-stage surgical fixation of his/her fractures with the SIGN nail. After anaesthesia was given, ankylosed limb joints were manipulated to improve the range of motion. All of the fractures had open reduction. The fibrous tissues were excised in non- and delayed unions while mal-unions were osteotomized. The bone canals were opened up with bone curette and manual reamers.
Reduction was achieved manually either by gradually distracting the fragments with a periosteal elevator placed between them or by hooking the fragments together in flexion while gradually extending the fracture site. Rotational malalignment was avoided by stabilizing the reduced fracture using a Lowman Clamp while aligning the linea aspera of the femur, or anterior border of the tibia. For the humerus, limb was placed in anatomical position beside the patient’s body. Subsequently, the locked nail was inserted as described by the manufacturer26. Autologous bone grafting was done for non-unions. The graft was harvested from the proximal tibia. All the patients had a five-day course of intravenous ceftriaxone. Pre- and post-operative radiographs were taken.
As permitted by their fracture pattern, bone integrity, and general condition, the patients were ambulated from the first post-operative day, and encouraged to move their joints. They were discharged from the hospital in the first or second post-operative week. Follow-up was continued at the out-patient clinic with plain radiographs and a test of ability to ‘squat and smile’ (femur and tibia) or do shoulder abduction-external rotation (humerus). The follow-ups were done at least twice—at six weeks and 12 weeks—but also at six and 12 months if painless ambulation or fracture healing was not achieved at the 12th week follow-up. The time taken to achieve full WB and knee flexion/shoulder abduction beyond 90° was noted. Occurrence of nerve palsy, presence of infection or need for a repeat surgery were also noted.
Ethical consideration
All patients gave informed consent to be included in the study. All methods were carried out in accordance with relevant guidelines and regulations, and the study protocols were approved by Bowen University Teaching Hospital Research Ethics Committee.
Results
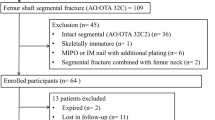
Over the study period, a total of 100 TBS-induced AFUs were treated in 98 patients. These included the 20 humerus, 64 femur and 16 tibia fractures. Of this, 96 fractures were seen for follow-up and were included in the analysis of treatment outcome (Table 4, Figs. 1 and 2), giving a follow-up rate of 96%. The four (4) femur fracture cases that were lost to follow-up were excluded. Three (15%) of the humerus fractures had iatrogenic radial nerve palsy which had recovered by the 12th week follow-up.
Table 1 shows the mean and range were 48.16 and 10–99 years respectively. Males constituted almost two-thirds (63.3%) of the patients’ population. Less than one-quarter (23.5%) were educated to tertiary level and only 17.3% belonged to occupational class 1. Motorcycle accidents was responsible for the highest proportion (40.8%) of the fractures.
Table 2 reveals that most of humerus fractures were simple diaphyseal fractures with the simple transverse (12-A3) having the largest percentage (40.0%). The femur fractures were more of diaphyseal simple transverse (23.4%), intact wedge (20.3%) or simple oblique (17.2%). The tibia fractures were mostly diaphyseal simple transverse (37.5%) and simple oblique (32.2%) fractures.
In Table 3, it is observed that there were more fractures on the right limb (55.0%) than the left (45.0%). Diaphyseal fractures constituted the highest proportion (90.0%). More than one-half (55.0%) of all the fractures were atrophic non-unions. The mean fracture-surgery interval was 21.04 months and surgery was completed within three hours in most of the cases.
In Table 4, it is observed that by the 12th post-operative week, 75% or more of the fractures had achieved knee flexion/shoulder abduction beyond 90°, were able to squat and smile (or do shoulder abduction-external rotation), had evidence of ongoing radiographic healing and were able to bear weight fully.
Figure 1 shows four cases got infected, including 3 deep and 1 superficial infection of the surgical site, giving an overall infection rate of 4.1%.
Figure 2 shows five (5.2%) patients had their implants removed: three because of deep infection, one because the implant was protruding into a joint, and one in a growing child.
Figures 3, 4 and 5 are clinical photographs of some patients who returned to work shortly after their fractures were treated, before radiological union occurred.
A 41-year old public servant with neglected atrophic non-union of a mid-shaft femur fracture fixed 92.8 months post-injury. She had walked with a limp and a stick before she had the fractured fixed, and was glad to return to work without the limp and the stick immediately after the 6th week follow-up visit, even without radiological union.
Discussion
In many LMICs, people seek fracture care from bonesetters irrespective of the cause, location, or type of fractures, and the patronage cuts across socio-demographic boundaries9,14. Our findings (Tables 1, 2 and 3) are in consonance with this previously documented assertions. There were more closed, simple/wedge (AO/OTA type A and B) and diaphyseal fractures than open, multi-fragmentary (type C) and end-segment fractures. This is similar to the pattern reported by earlier studies in our environment27,28. Nevertheless, it is also possible that the number of open fractures that eventually presented to us as AFUs was reduced by pre-hospital fatal complications such as septicaemia and tetanus18,19 or that many patients with open fractures sought orthodox care of the wound16.
Non-union was the most common form of AFUs in our series, and this has been reported by other studies on complications of TBS10,20. High energy injuries, the cause of majority of the fractures in our series, are known to predispose to non-unions owing to the accompanying soft tissue disruption3. The excessive movement at the fracture site produced by bonesetters’ practice of daily massage could also be responsible3,9. With a mean fracture-surgery interval of 21.04 months and a range of 1.12–219.03 months, the fractures in our study were much older than those of similar previous studies9,10,29. Since SIGN Fracture Care International started donating implants to our centre, patronage for fracture care has considerably increased, including old fractures which had hitherto been neglected. Many people in our area are often reluctant to seek surgical care in hospitals of neighbouring states due to distance, poverty and unfamiliarity with the hospitals.
In assessing treatment outcome, we placed greater emphasis on the patients’ functional recovery rather than radiological union. Despite the extensive amount of research on finding reliable ways of determining fracture healing, no ‘gold standard’ methods of assessing fracture union currently exist21. Hence, clinicians are to draw on multiple assessment modalities that measure or correlate with bone healing21. The modalities they draw on, however, is dependent on the ones available and feasible in their practice location/culture. Hence, for our study, the indices employed in the outcome assessment included patients’ abilities to: (i) achieve full WB (ii) squat and smile (S&S) (or do shoulder abduction and external rotation [SAER] for humerus fractures) and, (iii) flex the knee (KF > 90°) or abduct the shoulder (SA > 90°) beyond 90°.
Test for painless WB has remained one of the mainstays of determining fracture union in the clinical setting notwithstanding many advances in fracture union assessment30. However, in addition to physician-based clinical and radiological methods, evaluations of fracture healing should also incorporate a patient-centered approach which includes patients’ goals and expectations from the healing process as it relates to their physical and mental functioning21,31. Fascinatingly, we observed that the SIGN nail being a solid locked rod, allows early WB and return to pre-injury daily activities even when the fracture has not radiographically healed. Thus some of our patients with simple diaphyseal fractures started unaided ambulation before discharge from the hospital, and by the 12th week follow-up visit, three-quarters or more had achieved FWB, S&S/SAER and KF > 90°/SA > 90°, and had returned to work.
Conversely, Ogunlade et al.who treated similar fractures with plate and screws in an analogous population initially mobilised their patients on non-WB crutches for 6–8 weeks, partial WB when callus was radiographically visible and full WB only when the fracture was “judged to have healed enough”, the whole process taking 3–4 months9. Another comparable study by Madu et al. 11 reported a better outcome with locked IM nailing than plating of femoral non-unions. Locked IM nailing is known to tolerate early WB and joint motion1,11. Hence, immediate WB as tolerated has been recommended for tibial and femoral shaft fractures treated with locked IM nail whereas initial 6–8 weeks of touch-down WB followed by progressive WB is recommended for plate and screws osteosynthesis of similar fractures5.
In our environment, most patients seek fracture care to regain the use of their limbs to an extent that allows them return to their pre-injury activities and work. Once this is achieved, they consider their fractures to have healed, and would often self-stop further follow-up irrespective of radiological findings1,32. The fact that the S&S test is based on squatting makes it locally relevant—for social, cultural, religious or occupational reasons. Since it can assess the mobility and stability of joints, especially hip and knee, the quality of squatting is said to be a proxy reflection of the functional outcome after fixation of lower limb fracture, particularly in LMICs where other assessment modalities are either expensive or unavailable31,33.
We encountered a lower incidence of complications than reported by previous authors who used implants other than locked IM nail: Three humerus fracture cases (15%) had radial nerve palsy which had recovered by the 12th week follow-up, but Madu et al.11 and Olasinde et al.12 reported 23.5% and 27.3% respectively in patients treated with plate and screws. One tibia fracture had superficial surgical site infection which healed with debridement and antibiotic treatment while three (3.1%) fractures had deep infection for which the implants were removed after the fractures had healed. The infection resolved subsequently.
Conclusion
Our study has shown the diversity of patients and fracture characteristics that were treated by TBS. It also revealed the forms of consequent AFUs and the valuableness of the SIGN’s solid locked IM nail in salvaging the fractures in a way that permitted early WB. Besides public health education, easy proximate access to efficient orthopaedic implants is a potential preventive public health mechanism to reduce the patronage of bonesetters and consequent complications of TBS. This is because such implants allow for a shorter hospital stay and early return to patients’ pre-injury economic activities and are therefore poverty-mitigating.
Nevertheless, the small number of fractures treated and the descriptive nature of our data analysis are limitations to foregoing conclusion. Further studies involving larger number of AFUs are needed to establish the statistical significance of the findings in this study.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Phillips, J., Zirkle, L. G. & Gosselin, R. A. Achieving locked intramedullary fixation of long bone fractures: Technology for the developing world. Int. Orthop. 36, 2007–2013 (2012).
Agarwal-Harding, K. J., von Keudell, A., Zirkle, L. G., Meara, J. G. & Dyer, G. S. M. Understanding and addressing the global need for orthopaedic trauma care. J. Bone Jt. Surg. Am. 98-A, 1844–1853 (2016).
Stewart, S. K. Fracture non-union: A review of clinical challenges and future research needs. Malays. Orthop. J. 13, 1–10 (2019).
Singaram, S. & Naidoo, M. The physical, psychological and social impact of long bone fractures on adults: A review. Afr. J. Prim. Health Care Fam. Med. 11, a1908 (2019).
Erik, N. K., Michael, J. B., Kylee, N., Robert, H. & Michael, Q. P. Early weight bearing after lower extremity fractures in adults. J. Am. Acad. Orthop. Surg. 21, 727–738 (2013).
Wu, N. et al. Economic burden of illness among us patients experiencing fracture non-union. Orthop. Res. Rev. 5, 21–33 (2013).
Berner, A. et al. Treatment of long bone defects and non-unions: From research to clinical practice. Cell Tissue Res. https://doi.org/10.1007/s00441-011-1184-8 (2011).
Gellman, R. E. Fracture care challenges in the austere and humanitarian environments. Curr. Trauma Rep. 2, 100–105 (2016).
Ogunlade, S. O., Omololu, A. B., Alonge, T. O., Diete, S. T. & Obawonyi, J. E. Predisposing factors and outcome of treatment of non-union of long-bone fractures in Ibadan, Nigeria. Niger. Postgrad. Med. J. 18, 56–60 (2011).
Ikpeme, I. A., Mkpanam, N. E., Abang, I. E., Ngim, N. E. & Udosen, A. M. Long bone non-unions and malunions: Risk factors and treatment outcomes in Calabar, Southern Nigeria. Open J. Orthop. 3, 253–257 (2013).
Madu, K. A., Nnyagu, H. & Ede, O. Non-union treatment outcomes in South-East Nigeria. Niger. J. Orthop. Trauma 17, 77–80 (2018).
Olasinde, A. A., Oluwadiya, K. S., Adetan, O. & Ogunlusi, J. D. Results of surgical treatment of nonunion of humeral shaft fracture with dynamic compression plate and cancellous bone grafting. Acta Ortop. Bras. 20, 223–225 (2012).
Nwachukwu, B. U., Okwesili, I. C., Harris, M. B. & Katz, J. N. Traditional bonesetters and contemporary orthopaedic fracture care in a developing nation: historical aspects, contemporary status and future directions. Open Orthop. J. 5, 20–26 (2011).
Abang, I. E. et al. Reasons for patronage of traditional bone setters. Niger. J. Surg. 22, 102–106 (2016).
Agarwal, A. & Agarwal, R. The practice and tradition of bonesetting. Educ. Health 23, 225 (2010).
Ariës, M. J. H., Joosten, H., Wegdam, H. H. J. & Der Geest, S. V. Fracture treatment by bonesetters in central Ghana: Patients explain their choices and experiences. Trop. Med. Int. Health 12, 564–574 (2007).
Onuminya, J. E. The role of the traditional bonesetter in primary fracture care in Nigeria. S. Afr. Med. J. 94, 652–658 (2004).
Nwadiaro, H. C. Bone setters’ gangrene. Niger. J. Med. 16, 8–10 (2007).
Adesina, S. A. et al. Family structure and bonesetter’s gangrene in children: A case series. Int. J. Trop. Dis. Health 14, 1–8 (2016).
Odatuwa-Omagbemi, D. O., Adiki, T. O., Elachi, C. I. & Bafor, A. Complications of traditional bone setters (TBS) treatment of musculoskeletal injuries: Experience in a private setting in Warri, South-South Nigeria. Pan. Afr. Med. J. 30, 189 (2018).
Morshed, S. Current options for determining fracture union. Adv. Med. https://doi.org/10.1155/2014/708574 (2014).
Pugh, K. J. & Rozbruch, S. R. Non-unions and mal-unions. in Orthopaedic Knowledge Update (ed. Baumgaertner, M. R. & Tornetta, P. III) 115–130 (American Academy of Orthopaedic Surgeons, 2005).
The Office for National Statistics. Standard Occupational Classification, the National Statistics Socio-Economic Classification Vol. 3 (Palgrave Macmillan, 2010).
Akinboboye, B. O., Shaba, O. P., Akeredolu, P. A. & Oderinu, O. H. Sociodemographic determinants of usage of complete dentures in a Nigerian teaching hospital: A pilot study. Eur. J. Prosthodont. 1, 37–41 (2013).
Meinberg, E. G., Agel, J., Roberts, C. S., Karam, M. D. & Kellam, J. F. Fracture and dislocation classification compendium—2018. J. Orthop. Trauma 32, S1-170 (2018).
SIGN Fracture Care International. Technique Manual of SIGN IM Nail & Interlocking Screw System Insertion & Extraction Guide. Revision # TM-2016.04.11 (SIGN Fracture Care International, 2016).
Adesina, S. A. et al. Radiation-free interlocking intramedullary nailing of three-hundred and seventy long bone fractures in Ogbomoso, Nigeria. Sci. Rep. 11, 10070 (2021).
Adesina, S. A. et al. Closed reduction and locked intramedullary nailing of diaphyseal long bone fractures without intra-operative imaging and fracture table. Int. Orthop. 46, 51–59 (2022).
Shah, S. B. et al. Outcome of treatment of nonunion tibial shaft fracture by intramedullary interlocking nail augmented with autogenous cancellous bone graft. Nepal Med. Coll. J. 16, 58–62 (2014).
Bhandari, M., Fong, K., Sprague, S., Williams, D. & Petrisor, B. Variability in the definition and perceived causes of delayed unions and nonunions: A cross-sectional, multinational survey of orthopaedic surgeons. J. Bone Jt. Surg. Am. 94, e1091–e1096 (2012).
Maharjan, R., Pokharel, B., Kalawar, R. P. S., Rijal, R. & Baral, D. Squat and smile assessment in predicting healing of lower limb fractures fixed with a SIGN nail. J. Clin. Orthop. Trauma 19, 32–41 (2021).
Shearer, D., Cunningham, B. & Zirkle, L. G. Population characteristics and clinical outcomes from the SIGN online surgical database. Tech. Orthop. 24, 273 (2009).
Wu, H. et al. Development of squat-and-smile test as proxy for femoral shaft fracture-healing in patients in Dar es Salaam, Tanzania. J. Bone Jt. Surg. Am. 101, 353–359 (2019).
Acknowledgements
The authors are deeply grateful to SIGN Fracture Care International and its founder and president, Dr L. G. Zirkle for the free donation of SIGN implants and training without which this study would not have been possible.
Author information
Authors and Affiliations
Contributions
Authors S.A.A., S.U.E., I.O.A. and A.I.A. were responsible for the conception and design of the study. Authors S.A.A. and A.I.A. acquired the data. Authors I.O.A. and A.O.D. carried out the analysis and interpretation of data. Authors S.A.A., I.O.A. and O.T.A. drafted the article. Authors S.U.E. and J.I.O. revised the manuscript critically for important intellectual content. All authors gave approval for the final version of the manuscript to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Adesina, S.A., Eyesan, S.U., Amole, I.O. et al. Solid locked intramedullary nailing for expeditious return of bone-setting-induced abnormal fracture union victims to work in South-western Nigeria. Sci Rep 12, 21432 (2022). https://doi.org/10.1038/s41598-022-25862-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-25862-3
This article is cited by
-
Retrograde intramedullary nailing with supplemental plate and lag screws allows early weight bearing following distal end-segment femur fractures (AO/OTA 33) in a low-resource setting
European Journal of Orthopaedic Surgery & Traumatology (2024)
-
Follow-up non-attendance after long-bone fractures in a low-resource setting: a prospective study of predictors and interventions to increase attendance rates
BMC Health Services Research (2023)
-
Locked intramedullary nailing of diaphyseal femur fractures without intraoperative fluoroscopy, fracture table and power reaming: retrograde affords greater procedural efficiency than antegrade approach
International Orthopaedics (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.