Abstract
Weekend effect has been considered to be associated with poorer quality of care and patient’s survival. For acute myocardial infarction (AMI) patients, the question of whether patients admitted during off-hours have worse outcomes as compared with patients admitted during on-hours is still inconclusive. We conducted this study to explore the weekend effect in AMI patients, using a nationwide insurance database in Taiwan. Using Taiwan National Health Insurance (NHI) claims database, we designed a retrospective cohort study, and extracted 184,769 incident cases of AMI through the NHI claims database between January 2006 and December 2014. We divided the patients into weekend admission group and weekday admission group. Patients were stratified as ST elevation/non-ST elevation AMI and receiving/not receiving percutaneous coronary intervention (PCI). We used a logistic regression model to examine the relative risk of in-hospital mortality and 1-year mortality which were obtained from the Taiwan National Death Registry between study groups. We found no difference between weekend group and weekday group for risk of in-hospital mortality (15.8% vs 16.2%, standardized difference 0.0118) and risk of 1-year mortality (30.2% vs 30.9%, standardized difference 0.0164). There was no statistically significant difference among all the comparisons through the multivariate logistic regression analysis adjusting for all the covariates and stratifying by the subtypes of AMI and whether or not executing PCI during hospitalization. As for AMI patients in Taiwan, admission on weekends or weekdays did not have a significant impact on either in-hospital mortality or 1-year cumulative mortality.
Similar content being viewed by others
Introduction
Acute myocardial infarction (AMI) is an important cause of death and ischemic heart disease has consistently ranked among the top ten causes of death in Taiwan1. Currently, there are standard practice guidelines for AMI2,3,4. Previous studies have shown that the delayed implementation of specific interventions for patients with AMI can result in worse outcomes5,6. Generally, there are fewer employees in the hospital on weekends than on weekdays. Decreased staffing and increased hospital workload are associated with increases in medical adverse events and imply adverse outcomes for ICU patients7,8. Many studies have claimed a weekend effect on patient survival rates, i.e. outcomes for patients admitted at the weekends were worse than patients admitted at the weekdays9,10. However, for AMI, the question of whether patients admitted during off-hours have worse outcomes as compared with patients admitted during on-hours is still inconclusive11. We conducted this retrospective study to explore the weekend effect in patients suffering from AMI, using a nationwide insurance database in Taiwan. This is a subgroup analysis of the previous main research12.
Methods
Data sources
National Health Insurance (NHI) is mandatory to all citizens in Taiwan. The Taiwan NHI claims database comprises administrative claims data routinely gathered from the NHI operating system. We obtained this research dataset for claims occurring between 2005/1/1 and 2015/12/31 from the NHI claims database. Diagnostic codes were based on the International Classification of Diseases, 9th revision, Clinical modification (ICD-9-CM). We linked our research dataset to the Taiwan National Death Registry and got exact dates of death. In this study, all the personal identifiers were encrypted and all data were analyzed anonymously.
Study design
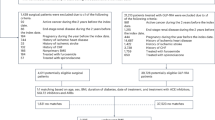
This study was a retrospective cohort analysis, of which all patients were adults (≥ 20 years old) having a discharge diagnosis of AMI (ICD-9-CM codes: 410.x) between 2006/1/1 and 2014/12/31. The diagnosis of AMI was further classified as ST elevation myocardial infarction (STEMI) (ICD-9-CM codes: 410.0–410.6 and 410.8), and non-ST elevation myocardial infarction (NSTEMI) (ICD-9-CM codes: 410.7 and 410.9). The index date was defined as the admission date of the index hospitalization for AMI. Weekend admission was defined for patients being admitted to hospital on Saturday, Sunday and national festival days. All other times were defined as weekday admission. Any patient having the same diagnosis within 1 year prior to index date, age younger than 20 years old or admission to psychiatric hospitals would be excluded. For the patient’s referrals between hospitals, only one admission was considered. The outcome measures were in-hospital mortality and 1-year mortality. All patients were followed until death or 365 days after discharge from the index hospitalization whichever came first.
Background characteristics
Based on Elixhauser’s Comorbidities13, underlying comorbidities were defined as appearance of the same diagnostic codes more than twice in outpatient visits or more than once in hospitalizations within 1 year prior to index date. Any medications administered were extracted from the NHI claims database within the 1-year period prior to index date14. Only comorbidities and medications with a prevalence of more than 1.0% were retained in the analysis.
We also identified characteristics about the first hospital visited by each patient and age/gender of the attending physician who carried out the percutaneous coronary intervention (PCI) procedures.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. The study protocol was reviewed and exempted from approval by the Institution Review Board of the National Taiwan University Hospital Hsin-Chu Branch. The need of informed consent was waived also by the Institution Review Board of the National Taiwan University Hospital Hsin-Chu Branch.
Statistical analysis
Continuous variables are presented as means and categorical variables are presented as frequencies. With a sufficiently large sample, a statistical test will almost always demonstrate a significant difference15. We used the standardized difference to assess balance of covariates between weekend and weekday groups whereby an absolute standardized difference of greater than 0.10 represented meaningful imbalance16. Patients were stratified as STEMI/NSTEMI and receiving/not receiving PCI during the index hospitalization. We applied the logistic regression model to estimate the relative risks (odds ratios [ORs]) of various clinical outcomes to compare weekend group with weekday group by adjustment of background characteristics (all the variables listed in Table 1 and Supplementary Table 1 were included as regressors). We used SAS software, version 9.4 (SAS Institute, Inc., Cary, North Carolina) for data analysis.
Conference presentation
A part of this manuscript (pooled results without stratification by subtypes of acute myocardial infarction and percutaneous coronary intervention or not) had been presented at the European Society of Cardiology (ESC) Congress 2019 held in Paris, France on Sep. 3, 2019.
Results
Patient characteristics
There were 184,769 patients identified in the NHI dataset between 2006/1/1 and 2014/12/31. The study population comprised 130,908 admissions on weekdays and 53,861 admissions on weekends. Besides, 42,954 patients were admitted for a STEMI, and 141,815 patients were admitted for a NSTEMI. Table 1 summarizes the patient characteristics across both weekday and weekend groups. There was no significant difference in background characteristics between the weekday and weekend groups. Less than 50% of patients had undergone PCI during hospitalization in both of the groups. The subtypes of myocardial infarction and whether or not executing PCI were not statistically different in both groups (Table 1, Supplementary Table 1).
Clinical outcomes
The crude in-hospital and 1-year mortality rates of weekday admission were comparable to those of weekend admission. For in-hospital mortality, the weekday group was 16.2% and the weekend group was 15.8% (standardized difference 0.0118). For 1-year mortality, the weekday group was 30.9% and the weekend group was 30.2% (standardized difference 0.0164) (Table 1).
Table 2 shows in-hospital and 1-year mortality stratified by subtypes of myocardial infarction and whether or not executing PCI across both the weekday and weekend groups. The in-hospital and 1-year mortality of both groups were not statistically different within all strata with a standardized difference less than 0.1.
Table 3 shows the results of the multivariate logistic regression analysis stratified by the subtypes of myocardial infarction and whether or not executing PCI after adjusting for all the covariates. Among the STEMI subgroup, there was no difference between the weekend group and weekday group with respect to risk of in-hospital mortality (with PCI: adjusted OR 1.033, 95% confidence interval [CI] 0.929–1.150, p = 0.54; without PCI: adjusted OR 0.934, 95% CI 0.855–1.020, p = 0.13) and risk of 1-year mortality (with PCI: adjusted OR 1.037, 95% CI 0.954–1.128, p = 0.39; without PCI: adjusted OR 0.962, 95% CI 0.891–1.039, p = 0.32). Among the NSTEMI subgroup, there was no difference in risk of in-hospital mortality (with PCI: adjusted OR 0.978, 95% CI 0.912–1.050, p = 0.55; without PCI: adjusted OR 0.979, 95% CI 0.944–1.015, p = 0.26) and risk of 1-year mortality (with PCI: adjusted OR 1.007, 95% CI 0.956–1.061, p = 0.79; without PCI: adjusted OR 0.971, 95% CI 0.940–1.004, p = 0.08) between weekend group and weekday group.
Discussion
In this retrospective cohort analysis, we found no difference in in-hospital and 1-year mortality between the weekday and weekend admissions for AMI in Taiwan. The results remained unchanged after controlling for background characteristics and stratifying the study population into STEMI/NSTEMI and receiving/not receiving PCI.
The weekend effect had been described for higher perinatal mortality of babies born at weekends in 1970s17. For major medical emergencies, Bell and Redelmeier reported that there was higher mortality rate among patients admitted on a weekend than patients admitted on a weekday for ruptured abdominal aortic aneurysm, acute epiglottitis and pulmonary embolism but no difference was found for AMI, intracerebral hemorrhage and acute hip fracture18. Using the American Acute Coronary Treatment and Intervention Outcomes Network-Get With The Guidelines (ACTION-GWTG) database for analysis, Dasari et al. reported that coronary reperfusion was delayed by an average of 16 min, and the mortality rate was 13% higher in patients presenting off-hours compared with patients presenting on-hours19. However, several subsequent studies have reported no significant association between mortality rate and the admission time, in contrast to the study using ACTION-GWTG database11,20,21,22. In Taiwan, the workforce is fewer on weekends than on weekdays indeed. However, cardiologists in Taiwan had dedicated themselves to shortening of door-to-balloon times for patients with STEMI by introducing variable effort and audit programs for many years. Elimination of difference in door-to-balloon times between patients presented on off-hours and on-hours had been achieved23. Based on the previous findings, we further disclosed that there was no significant difference in clinic outcomes between AMI patients who were admitted on weekdays and holidays in Taiwan.
The NHI program has been available in Taiwan since 1995, and insures > 99% of 23.4 million residents in Taiwan24. The single-payer NHI program in Taiwan provides all insured people comprehensive health care regardless of different social, economic, and health status. Lee et al. found a significant reduction in death rate after the implementation of NHI in Taiwan25. Our study showed the prevalence of PCI for patients with AMI was 46%, which was comparable to those in other countries26. The findings of our study revealed no difference in short-term and long-term mortality between weekend and weekday admission groups among patients with AMI and this could be attributed to increases in accessibility and the availability of critical care services in Taiwan under the NHI program27.
According to previous studies, the mortality rate of STEMI after PCI was about 7%28. In our study, the in-hospital mortality rate of STEMI patients in Taiwan after PCI was also about 7% which was comparable to previous data. In the COMPLETE trial, at a median follow-up of 3 years, death from cardiovascular causes or new myocardial infarction occurred in 7.8% of patients in the complete revascularization group while the rate was 10.5% in patients only receiving intervention for culprit lesion29. In our study, 1-year mortality among patient with STEMI receiving PCI was about 13% which seemed higher than that reported in the COMPLETE trial. However, the cause of higher long-term mortality in our study was beyond the scope of this paper. It is warranted to conduct a further investigation to explore the possible causes of higher long-term mortality for AMI patients in Taiwan. And we should be more committed to improving the long-term survival rate of STEMI to achieve better long-term outcomes.
Study limitations
Our study has some limitations. First, we couldn’t extract the exact admission hours from the Taiwan NHI claims database but could only define the weekend admission as admission on Saturday, Sunday and national festival days. Second, our findings only disclosed the current health care status in Taiwan. These findings couldn’t be applied to other healthcare systems in other countries. Third, door-to-balloon time was not available in our NHI claim database. We had no way of knowing whether there was a significance difference in door-to-balloon times between weekend group and weekday group.
Conclusion
As for AMI patients in Taiwan, admission on weekends or weekdays did not have a significant impact on either in-hospital mortality or 1-year cumulative mortality. The Taiwan NHI system has provided timely accessibility and reliable quality of care for all insured residents suffering from AMI without any difference between admission on weekdays and weekends.
Data availability
The authors do not own the data underlying this study. The data that support the findings of this study are available from the Health and Welfare Data Science Center (HWDC), Ministry of Health and Welfare, Executive Yuan, Taiwan. The contact information is as follows: Address: No. 488, Sec. 6, Zhongxiao E. Rd., Nangang Dist. Taipei City 11558, Taiwan; Tel: + 886-2-8590-6805; Mr. Young, e-mail address: stsung@mohw.gov.tw. The HWDC must review and approve all applications for use of the database. The process of data analysis has to be conducted in specific offices provided by the HWDC. Only the results of analysis are released after review by the HWDC. The database owned by the HWDC is subject to related regulations of the HWDC including payment, and so is not publicly available.
References
Hsiao, A. J., Chen, L. H. & Lu, T. H. Ten leading causes of death in Taiwan: A comparison of two grouping lists. J. Formos Med. Assoc. 114, 679–680 (2015).
Ibanez, B. et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 39, 119–177 (2017).
O’Gara, P. T. et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 61, e78–e140 (2013).
Amsterdam, E. A. et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 130, e344–e426 (2014).
Magid, D. J. et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA 294, 803–812 (2005).
Sorita, A. et al. Off-hour presentation and outcomes in patients with acute myocardial infarction: Systematic review and meta-analysis. BMJ 348, f7393 (2014).
Weissman, J. S. et al. Hospital workload and adverse events. Med. Care 45, 448–455 (2007).
Penoyer, D. A. Nurse staffing and patient outcomes in critical care: A concise review. Crit. Care Med. 38, 1521–1528 (2010).
Honeyford, K., Cecil, E., Lo, M., Bottle, A. & Aylin, P. The weekend effect: Does hospital mortality differ by day of the week? A systematic review and meta-analysis. BMC Health Serv. Res. 18, 870 (2018).
Pauls, L. A. et al. The weekend effect in hospitalized patients: A meta-analysis. J. Hosp. Med. 12, 760–766 (2017).
Sorita, A. et al. Off-hour admission and outcomes for patients with acute myocardial infarction undergoing percutaneous coronary interventions. Am. Heart J. 169, 62–68 (2015).
Lai, C. L., Kuo, R. N., Wang, T. C. & Chan, K. A. Mortality of major cardiovascular emergencies among patients admitted to hospitals on weekends as compared with weekdays in Taiwan. BMC Health Serv. Res. 21, 528 (2021).
Quan, H. et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 43, 1130–1139 (2005).
Kuo, R. N. et al. Predicting healthcare utilization using a pharmacy-based metric with the WHO’s anatomic therapeutic chemical algorithm. Med. Care 49, 1031–1039 (2011).
Sullivan, G. M. & Feinn, R. Using effect size-or why the P value is not enough. J. Grad. Med. Educ. 4, 279–282 (2012).
Austin, P. C. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun. Stat. Simul. Comput. 38, 1228–1234 (2009).
MacFarlane, A. Variations in number of births and perinatal mortality by day of week in England and Wales. Br. Med. J. 2, 1670–1673 (1978).
Bell, C. M. & Redelmeier, D. A. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N. Engl. J. Med. 345, 663–668 (2001).
Dasari, T. W. et al. Impact of time of presentation on process performance and outcomes in ST-segment-elevation myocardial infarction: A report from the American Heart Association: Mission Lifeline program. Circ. Cardiovasc. Qual. Outcomes 7, 656–663 (2014).
Kim, S. S. et al. Impact of patients’ arrival time on the care and in-hospital mortality in patients with non-ST-elevation myocardial infarction. Am. J. Cardiol. 113, 262–269 (2014).
Geng, J. et al. Outcomes of off- and on-hours admission in ST-segment elevation myocardial infarction patients undergoing primary percutaneous coronary intervention: A retrospective observational cohort study. Medicine (Baltimore) 95, e4093 (2016).
Martin, G. P. et al. Effect of weekend admission on process of care and clinical outcomes for the management of acute coronary syndromes: A retrospective analysis of three UK centres. BMJ Open 7, e016866 (2017).
Lai, C. L. et al. Impact of an audit program and other factors on door-to-balloon times in acute ST-elevation myocardial infarction patients destined for primary coronary intervention. Acad. Emerg. Med. 16, 333–342 (2009).
Cheng, T.-M. Reflections on the 20th anniversary of Taiwan’s single-payer national health insurance system. Health Aff. 34, 502–510 (2015).
Lee, Y.-C. et al. The impact of universal National Health Insurance on population health: The experience of Taiwan. BMC Health Serv. Res. 10, 225 (2010).
Ui, S., Chino, M. & Isshiki, T. Rates of primary percutaneous coronary intervention worldwide. Circ. J. 69, 95–100 (2005).
Lai, C. C., Ho, C. H., Chang, C. L. & Cheng, K. C. Availability of critical care services in Taiwan under National Health Insurance. Br. J. Anaesth. 119, 335–337 (2017).
Keeley, E. C., Boura, J. A. & Grines, C. L. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: A quantitative review of 23 randomised trials. Lancet 361, 13–20 (2003).
Mehta, S. R. et al. Complete revascularization with multivessel PCI for myocardial infarction. N. Engl. J. Med. 381, 1411–1421 (2019).
Acknowledgements
All the data used in this study were released and approved by the Health and Welfare Data Science Center (HWDC), Ministry of Health and Welfare, Executive Yuan, Taiwan.
Funding
This work was supported by grants from the Ministry of Science and Technology, Taiwan (MOST 106-2410-H-002-218- and MOST 107-2410-H-002-237-).
Author information
Authors and Affiliations
Contributions
S.-F.L.: study design, interpretation of data, and drafting of the manuscript. C.-L.L.: study design, obtaining funding, interpretation of data, and revision of the manuscript. R.N.-C.K.: study design, interpretation of data, and revision of the manuscript. T.-C.W.: study design, data analysis, and interpretation of data. T.-T.L.: study design, and interpretation of data. K.A.C.: study design, obtaining funding, and revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, SF., Lai, CL., Kuo, R.NC. et al. Mortality among acute myocardial infarction patients admitted to hospitals on weekends as compared with weekdays in Taiwan. Sci Rep 13, 2320 (2023). https://doi.org/10.1038/s41598-022-25415-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-25415-8
This article is cited by
-
Association between holiday and weekend admissions and mortality outcomes among patients with acute myocardial infarction receiving percutaneous coronary intervention in Taiwan
Scientific Reports (2024)
-
The dose–response effect of time between emergency admission and inpatient care on mortality
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.