Abstract
Correction modelling using reported BMI values has been employed in adolescent and adult populations to improve the accuracy of self-reporting. This study aimed to evaluate the feasibility of establishing correction modelling for mother-reported child height and weight at 2 years using data from an Australian trial in 2019. Correction modelling for BMI was conducted using mother-reported and objectively measured height and weight of 2-year-olds. Mother-reported height, weight and BMI values of 2-year-old children were adjusted based on objectively measured anthropometric data using linear regression models. ‘Direct’ and ‘indirect’ corrections were applied to the correction of BMI values. We defined the direct collection as using corrected BMI values that were predicted directly by the model and indirect correction as using corrected weight and height values to calculate corrected BMI values. Corrected BMI values via the indirect correction showed higher sensitivity or similar specificity in predicting overweight status, compared to the direct correction, and also showed higher agreement with measured values compared to the mother-reported measures. Corrected self-reported measures via an indirect correction had a better accuracy and agreement with the objectively measured data in the BMI values and classification of overweight, compared to the mother-reported values.
Similar content being viewed by others
Introduction
Childhood obesity affects growth and development and has become a worldwide health issue. The World Health Organization (WHO) proposed a goal of zero increase in childhood overweight by 20251. In Australia, about one quarter of both children aged 2–4 years and also children and adolescents aged 2–17 years were affected by overweight or obesity in 2017–20182,3. Echoing the WHO global target, Australia has developed the National Obesity Strategy 2022–2032 with the aim to reduce overweight and obesity in children and adolescents by at least 5% by 20303. It is important to ensure the estimation of overweight and obesity in populations is accurate to effectively assess and monitor trends and evaluate the impact of health promotion efforts.
Body mass index (BMI; weight (kg)/height (m)2) is used widely to determine overweight and obesity among children4,5. BMI calculated by parental- or self-reported height and weight from surveys is commonly used in epidemiological studies as its feasible, efficient, and economical. However, there is a risk of both random and systematic errors embedded in the use of reported measures. For example, participants tend to overestimate their height and underestimate their weight due to social desirability, resulting in an underestimation of their actual BMI6,7,8,9. BMI correction, therefore, has been applied to obtain a closer approximation to the measured BMI based on the self-reported height and weight in large population studies, including in adolescents and adults7,10,11,12,13,14. However, to date few studies have used corrected BMI values in 2-year-old children. Several studies have investigated the accuracy of measured and mother-reported height and weight in children10,15,16 and have raised concerns about the accuracy of mother-reported anthropometry. There have been recommendations to adjust mother-reported anthropometry based on correction equations10.
We therefore aimed (1) to evaluate the feasibility of establishing correction modelling for mother-reported child height and weight using data from a randomised controlled trial in 2-year-old children, (2) to investigate the bias of mother-reported child anthropometric data compared with data measured objectively by researchers, and (3) to examine whether the corrected anthropometric data improved the accuracy of the mother-reported data and agreement with the objectively measured data.
Methods
Study context
The Communicating Healthy Beginnings Advice by Telephone Randomised Controlled Trial (CHAT) randomised controlled trial (RCT) was a three-armed RCT conducted in metropolitan Sydney, New South Wales (NSW), Australia 2017–2019. The CHAT RCT aimed to evaluate the efficacy of using telephone support or SMS, plus mailed intervention materials in promoting healthy infant feeding practices and obesity-protective behaviours in the early years of life. As part of the main outcomes, children’s height and weight were measured by research assistants (RAs) through home visiting, and also independently reported by their mother via computer assisted telephone interviewing (CATI) at 2 years of their age. The study protocol, eligibility criteria, recruitment process and outcomes are reported in detail elsewhere17,18,19. The CHAT RCT was registered with the Australian Clinical Trial Registry (ACTRN12616001470482p, 21/10/2016).
Study participants
At 2 years of age, 797 (69%) completed the telephone survey20, of whom 484 were excluded from this analysis due to lack of mother-reported child weight or height, 53 due to the lack of anthropometric measurement and 26 due to anthropometric measurement being completed beyond 30 days of telephone survey. In total 234 participants were included in this study (Fig. 1). Participants’ demographic characteristics were compared by whether or not provision of self-reported and objectively measured anthropometric measurement at 2 years of age, showing a similar distribution in participants’ demographics between groups. However, a higher percentage of first-time mothers or mothers born overseas was observed in the group providing both self-reported and objectively measured anthropometrics (P < 0.05) (Supplement Table 1).
Data collection
Anthropometric measurement
Anthropometric measurements were objectively measured by four RAs at the participants’ residence when the child was 2 years of age.
Measured height and weight
At the 2-year follow-up, an RA took height and weight measurements. Two measurements of height were made using the Seca 213 portable stadiometer and recorded it to the nearest 0.1 cm; a third measure was taken if the first two measurements differed by 0.5 cm or more and the mean of these two or three values was recorded. Weight was measured using Seca 803 digital scales on children wearing light clothes and no shoes. The measures were recorded to the nearest 0.1 kg and the mean of two measurements recorded.
Reported height and weight
During the same period, mother-reported height and weight were also collected within 30 days through a telephone survey. The survey was administered via telephone using CATI.
BMI, BMI z-score and obesity/overweight
Children’s BMI was calculated as [weight (kg)/height (m)2] and BMI z-score for sex and age was calculated using WHO Anthro21. Overweight/obesity for children at two years of age was classified based on the International Obesity Taskforce recommended age-standardised BMI cut points. A child with a BMI equals or above 18.41 for male or 18.02 for female was considered as overweight, and with a BMI equals or above 20.09 for male or 19.81 for female was considered as obesity4.
Demographics data
Sociodemographic data collected at baseline included maternal age, employment status, education level, marital status, language spoken at home, and country of birth of mothers. The questionnaires were based on the previous Healthy Beginnings Trial22,23,24.
Statistical analysis
Descriptive analyses were undertaken to summarise the distributions of characteristics of the study participants. Considering the potential impact of the time gap between the mother-reported and the objectively measured anthropometric data on child’s height, weight and BMI outcomes, we grouped the data by the time gap, i.e., telephone-surveyed and RA-measured data within seven days or within 30 days. The distributions of participants’ characteristics were therefore described and compared by the time gap. Students t-test and Chi square test were used to test the differences between groups as appropriate. The significant level is set as two-sided P < 0.05, same below.
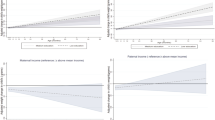
The distributions of reported and measured height, weight, calculated BMI, BMI z-score, obesity and overweight/obesity were then described for the overall sample. To identify biases in reporting, we tested for differences between reported and measured values of these outcomes using a paired t-test or McNemar’s test as appropriate. An agreement analysis was also conducted between the reported and measured data. Scatter plots were generated to show the distributions of measured height, weight and BMI calculated by measured values against reported values.
A linear regression model with measured height, weight, BMI or BMI z-score as the dependent variable and reported values of the same variable as the key independent variable was used for correction. Univariate analysis was employed to determine the selection of participants’ characteristics entering into the models, in combination with the Akaike Information Criterion. The fit of models was assessed using the adjusted-R2 statistic. A random normal noise term was added to the models to show the variability to the corrected values. As stated above, to evaluate the potential impact of the time gap between the reported and measured anthropometrics on the correction, two models were considered for each outcome: Model 1 for reported and measured data within 7 days (n = 111), and Model 2 for reported and measured data within 30 days (n = 234). Direct or indirect correction was applied to the correction of BMI values. Direct correction used the corrected BMI predicted by the model. Indirect correction used the corrected weight and height values to calculate corrected BMI.
We also assessed classification error using sensitivity and specificity for the binary indicators of obesity and overweight/obesity for the reported and corrected data within 7 and 30 days (Model 1–2). Sensitivity (true positive) indicates a model’s ability to correctly classify an individual with overweight or obesity while specificity (true negative) indicates its ability to correctly classify an individual with non-obesity or non-overweight/non-obesity.
Lastly, to assess the improvement of corrected estimates, we compared the agreement between corrected estimates and objectively measured data to the agreement between mother reported data and objectively measured data. Agreement analyses were undertaken and intra-class correlation coefficients (ICCs) and kappa statistics were reported to understand the extent of agreement between corrected and measured height, weight and BMI. ICC values between 0.5 and 0.75 and between 0.75 and 0.9 indicate moderate and good reliability, respectively25. Kappa statistics between 0.41–0.60, between 0.61–0.80 and between 0.81–1.00 suggest moderate, substantial and perfect agreement, respectively26. Histograms of differences between measured and self-reported height, weight and BMI values, between corrected and self-reported values, and between measured and corrected values were also generated. Data were analysed using Stata, version 13 (StataCorp LLC).
Ethical approval and consent to participate
This study was part of the trial granted ethics approval by the Ethics Review Committee of Sydney Local Health District (Protocol No. X16–0360 & LNR/16/RPAH/495 and Protocol No X18–0387 & HREC/18/RPAH/545). Written informed consent was obtained from all study participants.
Results
Participants’ characteristics
The mean age of the children (47% female) at survey was 23.9 ± 0.36 months. The majority of mothers were married or had a de factor partner (96%), had a university education level (71%), were born overseas (69%), employed (67%), were first-time mothers (63%) and had a household income over $80,000 (58%). Just over half of mothers spoke English at home (51%). Two-fifths of mothers (42%) were aged 30 to 34 years, followed by 29% aged 35–39 years (Table 1).
The mean time gap between surveyed and measured anthropometrics was 10.3 ± 6.986 days, with 47% of participants having anthropometrics measured within 7 days of the telephone survey (n = 111). Similar participants’ characteristics were observed in the group with the time gap within 7 days, a lower percentage of participants with a university education (64%) was observed in the group with a time gap within 7 days (Table 1).
Reporting biases between reported and measured anthropometrics
On average, the reported height and weight was 0.4 cm higher and 0.1 kg lower than measured height and weight, respectively. The reported BMI and BMI z-score were both 0.2 units lower than measured BMI and BMI z-score, but the difference was not statistically significant (P > 0.05) (Table 2). The differences in the anthropometrics between the reported and measured anthropometrics were further analysed by different time gaps, showing the variation of differences rose as the time gap increases (Supplement Table 2). The discrepancies in measured and reported data by participants’ characteristics were described in the supplement Tables 3 and 4.
The proportion of those with obesity derived from self-report was 7% higher than that derived from the measured value, but the difference was not statistically significant (P > 0.05). However, the proportion of those with combined overweight/obesity from the survey was the same as the measured value (Table 2).
The agreement analysis showed a good agreement (ICC = 0.81) between the reported and measured weight, a moderate agreement between the reported and measured height (ICC = 0.42), but a poor agreement between reported and measured BMI (ICC = 0.28). The Kappa coefficient of 0.26 was also low in the classification of overweight or obesity status based on reported data. The scatter plots of measured height, weight and BMI values against reported values are provided in the Supplement Figs. 1–6.
Quality of BMI correction models
The adjusted R2 statistics were higher for models with weight as a dependent variable (66–74%) compared to models of height (27–28%), BMI z-score (16–19%) and BMI (11–17%). Not surprisingly, across all outcomes (height, weight, BMI z-score and BMI), the correction models derived from reported and measured anthropometrics within 7 days (Model 1) had a consistently highest adjusted R2 compared to the models derived from data with a time gap within 30 days (Model 2) (Table 3). Considering the adjusted R2 values were all below 75%, a random normal noise with mean 0 and standard deviation equals to the square root of the mean square error from the model was added to each prediction model to show the variability to the corrected value.
The correction equations for height, weight, BMI and BMI z-score are listed below.
Model 1 (time gap between the reported and measured within 7 days):
Model 2 (time gap between the reported and measured within 30 days):
Accuracy of reported and corrected obesity and overweight estimates
When comparing sensitivity across reported, indirect and direct correction models using data from different time gaps (within 7 days or 30 days, respectively), indirect correction models derived from corrected anthropometrics within 7 days (Model 1) and within 30 days (Model 2) had a sensitivity of 58% and 53% for overweight/obesity respectively, and substantially higher than that of uncorrected mother’s report (around 41%). Direct correction values from Model 1 and 2 had a very low sensitivity for overweight/obesity (2–4%). The sensitivity indicator for obesity was not calculated when no child was classified as obesity, either based on the objective or corrected values. Therefore, this indicator was not available for a comparison across the models (Table 4).
When comparing specificity across the models under ‘reported’, ‘indirect’ or ‘direct’ approaches, the specificity for overweight/obesity was highest in direct correction values (around 98%), followed by the indirect values (around 86%) and uncorrected reports (about 85%). Overall, the specificity of overweight/obesity was similar based on the indirect correction models across different time gaps (Table 4). Similar to the sensitivity indicator, the specificity indicator for obesity was not available for a comparison across the models (Table 4).
Agreement analysis between reported, corrected and measured outcomes
In Model 1, indirect corrected and reported means of height, weight and BMI, and overweight/obesity prevalence estimates were closer to those obtained from objective measurements. The estimate of obesity prevalence (5%) was higher than the objective value (0%). Similar to those between the reported and objective values, the ICCs between the indirect corrected and objective values ranged from 0.4 (for height) to 0.9 (for weight). However, a higher ICC for BMI (0.6) and a higher Kappa coefficient of 0.43 in the classification of overweight or obesity status were reported between the indirect corrected and objective values, compared to those between the uncorrected report or direct corrected values and objective measures (Table 5). Similar findings were observed in Model 2, where the time gap between the reported and measured data within 30 days, a higher ICC for BMI (0.6) and a higher Kappa coefficient of 0.37 in the classification of overweight or obesity status were reported between the indirect corrected and objective values, compared to those between the uncorrected report or direct corrected values and objective measures (Table 5).
Histograms of differences between measured and self-reported height, weight and BMI values, between corrected and self-reported values, and between measured and corrected values were shown in Supplement Figs. 7–28, separated by different time gaps. The Figures show a decreased difference when the time gap between the reported and measured data was within 7 days, and between the measured and corrected values when compared to the differences between the measured and self-reported values (Supplement Figs. 7–28).
Discussion
Principal findings of the study
Findings from our study have shown a poor agreement in BMI and classification of overweight between the mother-reported and objectively measured data. We therefore aimed to explore the feasibility of establishing correction modelling for mother-reported child height and weight at 2 years of age. The correction modelling has shown an improvement in the accuracy and agreement in BMI values and the classification of overweight compared to the mother-reported data. Further, we have found the correction modelling in height, weight, BMI z-score and BMI reported a better fit if the time gap between the occurrence of survey and objective measurement was within seven days (Model 1), compared to that within 30 days (Model 2). Also, corrected BMI values via an indirect correction (i.e., use of the corrected weight and height values to calculate corrected BMI) showed a higher sensitivity and similar specificity, and a better agreement with measured values compared to the corrected BMI values derived from a direct correction (i.e., use of corrected BMI predicted by the model in both Models 1 and 2).
Meaning of the study
Although correction modelling of BMI has been evaluated in the population of adolescents and adults7,10,11,12,13,14, we are not aware of a similar study that has been reported in children at 2 years of age. Our analyses have shown a poor agreement between mother-reported and objectively-measured data, consistent with previous studies in children10,15,16, suggesting the necessity of correction modelling based on mother-reported data in children. The corrected BMI values from the correction modelling have shown a better accuracy and agreement with the measured data, compared to the mother-reported data. Our findings suggest corrected anthropometric data (i.e., BMI) from mothers reported value can be considered as an option to allow health professionals to monitor children growth and development.
What the study adds
Our findings suggest corrected BMI value had a better accuracy and agreement with the objectively measured BMI value compared to reported data, especially when the survey and measurement occurred within a short timeframe that is within seven days. These findings might be attributed to the child’s growth, or be impacted by the chance of increasing the magnitude of errors as the sample size of participants increases, as shown in the supplement data, where the variation of difference between reported and measured anthropometrics increased as more data were included. Further study is warranted in terms of the impact of timeframe to collect reported and measured data on correction modelling.
Our findings also showed BMI values corrected via an indirect correction (i.e., calculated by corrected height and weight) had a better performance than the direct correction (i.e., corrected BMI values predicted by the model) in terms of accuracy in predicting overweight/obese status and agreement with the objectively measured BMI value. The better performance of indirect correction model was consistent with a previous study in adolescents11, which suggested undertaking BMI correction using the corrected height and weight values to calculate corrected BMI, rather than taking the direct corrected BMI values predicted by the BMI correction model. This could be explained by the better fit of models (higher R2) in the height and weight correction models than the direct BMI correction model.
Across the correction models, weight correction models consistently showed a better fit when compared to the correction models in the height, BMI z-score and BMI. The variation of difference in weight between measured and reported data was lower than the height. Feedback from the RAs also reflected the difficulty in measuring the height over weight among children in this study. Therefore, a guideline in measurement of children’s height and weight should be developed to support parents in collecting more acute anthropometric data.
Unanswered questions and future research
Apart from the correction modelling of weight, the correction models of height and BMI had a lower fit than a previous correction modelling study in adolescents11. Further study to explore the feasibility of correction modelling in a large sample of children is warranted.
Although misreporting was found to be related to gender, ethnicity and other socioeconomic status in other studies10,15,16, we did not find many discrepancies in this study. The role of socioeconomic-status bias in the BMI correction modelling study in children needs to be further investigated.
Strengths and limitations
To our knowledge, this is the first study to investigate the feasibility of correction modelling of BMI based on mother-reported height and weight in children of 2 years age. However, our study has several limitations. First, the sample size was relatively smaller than in other correction modelling studies7,11,12. The differences between the mother-reported and objectively measured data were not significant partially due to the lack of statistical power resulting from the small sample size. It is important to replicate our results for less common outcomes such as obesity status with larger sample sizes. Second, due to the small sample size, we were not able to assess the model’s predictive capacity on a separate dataset that was not used to develop this model. Finally, the majority of mothers included in the correction modelling study were from a culturally and linguistically diverse background, with a university education level and were first-time mother, all these may contribute to a less reporting bias of child’s height and weight, therefore limit the generalisability of our findings.
Conclusion
In this study we found a poor agreement between reported and measured data. Corrected anthropometric data via an indirect correction has a better accuracy and agreement with the objectively measured data in terms of BMI values and classification of overweight, compared to the mother-reported values. The correction modelling had a better fit if the time gap between measured and reported data within seven days. Our findings suggest corrected anthropometric data (e.g., BMI) from mothers-reports can be considered as an option to allow health professionals to monitor children growth and development.
Data availability
The datasets used and/or analysed during the current study will be available from the corresponding author upon reasonable request and ethics approval after the completion of the study in June 2023.
References
World Health Organization. Global Nutrition Targets 2025: Childhood overweight policy brief (WHO/NMH/NHD/14.6). World Health Organization. Updated December 30, 2014. https://www.who.int/publications/i/item/WHO-NMH-NHD-14.6. Accessed 6 May 2022
Australian Bureau of statistics. National Health Survey: First results, 2017–2018. Australian Bureau of statistics. Updated December 12, 2018. https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-first-results/latest-release#key-statistics. Accessed 7 Apr 2022.
Commonwealth of Australia. National Obesity Strategy 2022–2032. Health Ministers Meeting. Updated March 18, 2022. https://www.health.gov.au/resources/publications/national-obesity-strategy-2022-2032. Accessed 7 Apr 2022.
Cole, T. J., Bellizzi, M. C., Flegal, K. M. & Dietz, W. H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 320(7244), 1240. https://doi.org/10.1136/bmj.320.7244.1240 (2000).
Cole, T. J., Flegal, K. M., Nicholls, D. & Jackson, A. A. Body mass index cut offs to define thinness in children and adolescents: International survey. BMJ 335(7612), 194. https://doi.org/10.1136/bmj.39238.399444.55 (2007).
Shields, M., Connor Gorber, S., Janssen, I. & Tremblay, M. S. Bias in self-reported estimates of obesity in Canadian health surveys: An update on correction equations for adults. Health Rep. 22(3), 35–45 (2011).
Drieskens, S., Demarest, S., Bel, S., De Ridder, K. & Tafforeau, J. Correction of self-reported BMI based on objective measurements: A Belgian experience. Archives of Public Health. 76(1), 10. https://doi.org/10.1186/s13690-018-0255-7 (2018).
Hayes, A. J., Kortt, M. A., Clarke, P. M. & Brandrup, J. D. Estimating equations to correct self-reported height and weight: implications for prevalence of overweight and obesity in Australia. Aust N Z J Public Health. 32(6), 542–545. https://doi.org/10.1111/j.1753-6405.2008.00306.x (2008).
Hayes, A. J., Clarke, P. M. & Lung, T. W. C. Change in bias in self-reported body mass index in Australia between 1995 and 2008 and the evaluation of correction equations. Popul. Health Metrics 9(1), 53. https://doi.org/10.1186/1478-7954-9-53 (2011).
Chai, L. K., Collins, C. E., May, C., Holder, C. & Burrows, T. L. Accuracy of parent-reported child height and weight and calculated body mass index compared with objectively measured anthropometrics: Secondary analysis of a randomized controlled trial. J Med Internet Res. 21(9), e12532. https://doi.org/10.2196/12532 (2019).
Ghosh-Dastidar, M., Haas, A. C., Nicosia, N. & Datar, A. Accuracy of BMI correction using multiple reports in children. BMC Obesity. 3(1), 37. https://doi.org/10.1186/s40608-016-0117-1 (2016).
Stommel, M. & Schoenborn, C. A. Accuracy and usefulness of BMI measures based on self-reported weight and height: Findings from the NHANES & NHIS 2001–2006. BMC Public Health 9(1), 421. https://doi.org/10.1186/1471-2458-9-421 (2009).
Gorber, S. C., Tremblay, M., Moher, D. & Gorber, B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: A systematic review. Obes. Rev. 8(4), 307–326. https://doi.org/10.1111/j.1467-789X.2007.00347.x (2007).
Merrill, R. M. & Richardson, J. S. Validity of self-reported height, weight, and body mass index: findings from the National Health and Nutrition Examination Survey, 2001–2006. Prev. Chronic Dis. 6(4), A121–A121 (2009).
O’Connor, D. P. & Gugenheim, J. J. Comparison of measured and parents’ reported height and weight in children and adolescents. Obesity (Silver Spring) 19(5), 1040–1046. https://doi.org/10.1038/oby.2010.278 (2011).
Dubois, L. & Girad, M. Accuracy of maternal reports of pre-schoolers’ weights and heights as estimates of BMI values. Int J Epidemiol. 36(1), 132–138. https://doi.org/10.1093/ije/dyl281 (2007).
Wen, L. M. et al. A 3-Arm randomised controlled trial of Communicating Healthy Beginnings Advice by Telephone (CHAT) to mothers with infants to prevent childhood obesity. BMC Public Health 17(1), 79–79. https://doi.org/10.1186/s12889-016-4005-x (2017).
Ekambareshwar, M. et al. Facilitators and challenges in recruiting pregnant women to an infant obesity prevention programme delivered via telephone calls or text messages. Trials 19(1), 494. https://doi.org/10.1186/s13063-018-2871-5 (2018).
Wen, L. M. et al. Effects of telephone and short message service support on infant feeding practices, “tummy time”, and screen time at 6 and 12 months of child age: A 3-group randomized clinical trial. JAMA Pediatr. 174(7), 657–664. https://doi.org/10.1001/jamapediatrics.2020.0215 (2020).
Wen, L. M. et al. Effects of telephone support or short message service on body mass index, eating and screen time behaviours of children age 2 years: A 3-arm randomized controlled trial. Pediatr. Obes. 17(5), e12875. https://doi.org/10.1111/ijpo.12875 (2022).
WHO Anthro for Personal Computers: Software for Assessing Growth and Development of the world's Children. Version 3.2.2. WHO; 2011. http://www.who.int/childgrowth/software/en/
Wen, L. M. et al. Effectiveness of home based early intervention on children’s BMI at age 2: randomised controlled trial. BMJ 344, e3732. https://doi.org/10.1136/bmj.e3732 (2012).
Wen, L. M. et al. Early intervention of multiple home visits to prevent childhood obesity in a disadvantaged population: a home-based randomised controlled trial (Healthy Beginnings Trial). BMC Public Health 7(1), 76. https://doi.org/10.1186/1471-2458-7-76 (2007).
Wen, L. M., Baur, L. A., Simpson, J. M., Rissel, C. & Flood, V. M. Effectiveness of an early intervention on infant feeding practices and “tummy time”: A randomized controlled trial. Arch. Pediatr. Adolesc. Med. 165(8), 701–707. https://doi.org/10.1001/archpediatrics.2011.115 (2011).
Bobak, C. A., Barr, P. J. & O’Malley, A. J. Estimation of an inter-rater intra-class correlation coefficient that overcomes common assumption violations in the assessment of health measurement scales. BMC Med. Res. Methodol. 18(1), 93. https://doi.org/10.1186/s12874-018-0550-6 (2018).
McHugh, M. L. Interrater reliability: The kappa statistic. Biochem Med (Zagreb). 22(3), 276–282 (2012).
Acknowledgements
We sincerely thank all the participating families in this study. We thank the members of the Steering Committee, Management Committee and working group for their advice and support. We wish to thank the project partners from the Sydney, South Eastern Sydney, South Western Sydney and Southern NSW Local Health Districts, in NSW, Australia.
Funding
This study was part of an intervention trial funded by the NSW Health Translational Research Grant Scheme 2016 (ID number: TRGS 200) and the Australian National Health and Medical Research Council Partnership Project APP1169823. We declare that the funder (NSW Health and NHMRC) played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
L.M.W. conceived the study idea and design and contributed to data interpretation and writing initial drafts. Y.C. conducted data analysis and prepared the first draft. HX and LB contributed to data collection and the literature search. All authors provided critical comments to the drafts and approved the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cheng, Y., Xu, H., Rissel, C. et al. Estimation and feasibility of correction modelling for mother-reported child height and weight at 2 years using data from the Australian CHAT trial. Sci Rep 12, 21353 (2022). https://doi.org/10.1038/s41598-022-25388-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-25388-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.