Abstract
Patients with severe uncontrolled asthma still experience acute asthma symptoms and exacerbations, particularly those with non-eosinophilic inflammation who take the maximum amount of standard drug therapy. Tezepelumab, a human monoclonal antibody, can improve lung function and enhance control of asthma symptoms in those patients, regardless of the disease’s baseline characteristics. This study aims to investigate the safety and efficacy of using tezepelumab in controlling severe symptoms of uncontrolled asthma. We performed a comprehensive literature search in several databases, including PubMed, Scopus, Web of Science, Cochrane Library, and clinicaltrial.gov, using a well-established search strategy to include all relevant publications. According to our inclusion criteria, we searched for randomized controlled trials comparing tezepelumab versus placebo in patients with severe, uncontrolled asthma. We analyzed the data using The Revman 5.4 program software. The search identified 589 potential articles. After excluding studies inconsistent with selection criteria, four studies were included and analyzed qualitatively and quantitatively. The pooled effect demonstrated the better performance of tezepelumab over the placebo regarding the decrease in annualized asthma exacerbation rate (MD = − 0.74, (95% CI [− 1.04, − 0.44], p < 0.00001)), asthma control questionnaire-6 (ACQ-6) Score MD = − 0.32, (95% CI [− 0.43, − 0.21], p < 0.00001)), blood eosinophil count (MD = − 139.38 cells/mcL, (95% CI [− 150.37, − 128.39], p < 0.00001)), feNO (MD = − 10 ppb, (95% CI [− 15.81, − 4.18], p = 0.0008)) and serum total IgE (MD = − 123.51 UI/ml, (95% CI [− 206.52, − 40.50], p = 0.004)). All tezepelumab groups had higher pre-bronchodilator forced expiratory volume in 1 s than the placebo group (MD = 0.16, (95% CI [0.10, 0.21], p < 0.00001)). Higher efficacy and safety profile was detected for tezepelumab to control the exacerbations of severe uncontrolled adult asthmatics.
Similar content being viewed by others
Introduction
According to the Global Initiative of Asthma (GINA), asthma is a condition that affects the lower parts of the airway, represented by recurrent respiratory manifestations including wheezing, breathlessness, tightness of the chest, and coughing as well as fluctuating airflow restriction1. In adults, the prevalence rate of asthma is estimated to be 4.5%, which translates to nearly 300 million persons with asthma globally. In developed countries, this prevalence reaches 21.5%2.
In most cases, airway restriction and asthmatic clinical manifestations change with the time of day manner. The manifestations frequently get worse at bedtime or in the early hours of the morning. Flares can be produced by both particular stimuli like allergens and general stimuli like exercising, laughing, irritating exposures, cold air, and respiratory tract infections1.
Symptoms and exacerbations occur in severe and uncontrolled cases of chronic asthma despite receiving the maximum amount of standard drug therapy. These cases have type 2 (T2), non-T2, or combined mechanisms-induced chronic airway inflammation3. Because of the chronic nature of this inflammatory disease, patients may experience restructuring all air passages, including epithelial apoptotic cell death, proliferation and differentiation of smooth muscle cells, and stimulation of fibroblastic cells contributing to matrix formation. These changes are collectively known as “airway remodeling” and, therefore, can contribute to chronic airway obstruction4,5.
Inhaled corticosteroids (ICSs) help decrease airway inflammation, which leads to better clinical asthma results6. Biological therapy can be used to enhance the response of the patients to moderate- to high-dose ICSs. The biological therapies that are now approved address particular T2 inflammatory mediators, adding therapeutic value for those with particular asthma characteristics (e.g. eosinophilic or allergic)7,8,9. Yet, certain people with chronic asthma, especially those with non-allergic or non-eosinophilic types, are ineligible for current biologic therapies10,11.
Thymic stromal lymphopoietin (TSLP), a cytokine released from epithelial cells, is believed to trigger a number of cell groups and inflammatory pathways implicated in the pathophysiology of asthma. The pathogenesis of both T2 and non-T2 mediated asthma is affected by TSLP, which plays a part in the initiation and maintenance of the airway inflammation12,13. The epithelium is the source of TSLP, which is released after its exposure to inhaled epithelial pathogens, including allergens, viruses, and bacteria. By upregulating T2 cytokines, TSLP regulates particular elements of neutrophilic inflammation and activates numerous T2 pro-inflammatory cells. These cells include group 2 innate lymphoid, dendritic, and mast cells13. TSLP has also been demonstrated to contribute to airway remodeling. This remodeling is done by fibroblasts and airway smooth muscle proliferation as TSLP increases collagen production14.
Tezepelumab, a human monoclonal antibody, attaches to TSLP and blocks binding to its heterodimeric receptors15,16. Despite basal values of T2 inflammatory biomarkers, tezepelumab decreased flare-ups dramatically in adults with severe uncontrolled asthma in phase 3 “NAVIGATOR” (NCT03347279) and phase 2b “PATHWAY” (NCT02054130) investigations15. To combine the existing data and assess the efficiency and safety of tezepelumab as a treatment for severe uncontrolled asthma in adults, we conducted this systematic review and meta-analysis.
Methods
We conducted this study and presented our findings in accordance with the preferred reporting guidelines for systematic reviews and meta-analyses (PRISMA) 202017 and Cochrane Handbook of Systematic Reviews of Intervention18. In addition, we used PROSPERO to register the protocol for this meta-analysis (CRD: CRD42021290047).
Literature search
We searched Cochrane Central Register of Controlled Trials (CENTRAL), PubMed, Web of Science, clinicaltrial.gov, and Scopus for articles from inception to September 25, 2022, with terms related to asthma and tezepelumab. Supplementary file 1 shows the search strategy we used in detail.
Eligibility criteria and studies selection
Two independent authors Ramadan Abdelmoez Farahat and Bassant Hassan Shawki, examined the articles to check if they fit our inclusion criteria. We considered randomized controlled studies (RCT) that looked at the clinical efficacy and safety of tezepelumab. In adults with severe, uncontrolled asthma who were either males or females aged ≥ 18. GINA 2012 guidelines define severe uncontrolled asthma despite being treated with long-acting beta-agonists coupled with a medium dose of fluticasone (250–500 g/day via a dry-powder inhaler or equivalent) or high dosage of fluticasone (> 500 g/day via dry-powder inhaler or equivalent) of inhaled glucocorticoids19.
Except for RCTs, we excluded all other study designs. Also, we did not include research whose extracted data were unreliable for analysis. Another third author arbitrated any discrepancies between the two authors.
Quality assessment
The Cochrane risk-of-bias tool for randomized trials (RoB 2) was applied to evaluate the quality of included Randomized clinical trials20. The Rob2 tool consists of six domains: (1) the randomization process, (2) missing outcome data, (3) deviations from the intended interventions, (4) selection of the reported result, (5) measure of the outcome and (6) other bias. The response options of the authors were classified as yes, probably yes, probably no, no, and no information. Two authors separately rated the quality, and all the debates were dealt with and resolved.
Data extraction and study outcomes
Two authors, Ahmed K. Awad and Eman Reda Gad, worked independently to extract data from a pre-defined excel spreadsheet, including the following data: a brief of the clinical trials’ essential characteristics, descriptions of the patients included in the clinical trials, and tezepelumab outcomes related to safety and efficacy. A discussion between the authors solved discrepancies.
Outcome definition
Treatment efficacy was assessed by annualized asthma exacerbation rate (AERR), change from baseline in pre-dose/pre-bronchodilator (pre-BD) forced expiratory volume in 1 s (FEV1), weekly mean daily. In addition to asthma symptom diary score, ACQ-6 Score, standardized asthma quality of life questionnaire for 12 years and older (AQLQ(S) + 12) total score, European quality of life-5 dimensions 5 level version (EQ-5D-5L) health state evaluation at Week 52, blood eosinophil count, FeNO, and serum total IgE.
Treatment-emergent adverse events (TEAEs) and Treatment-emergent serious adverse events (TESAEs) assessed the occurrence of the adverse events.
Data synthesis and assessment of heterogeneity
For statistical analyses, we used Revman software Version 5.4.1. For dichotomous data, pooled risk ratio (RR) was used, while for continuous data, the mean difference was used with 95% confidence intervals (CI). We used the random-effect model for the analysis. We considered p-value < 0.05 as a significant point. For heterogeneity, I-square and p-value were used. If the p-value was < 0.05 or I-square was > 60%, the analysis was considered heterogeneous. A leave-one-out test or subgrouping analysis was adopted to solve the heterogeneity21.
Results
Literature search results
We obtained 1196 studies from clinical trial.gov, PubMed, Web of Science, and Cochrane library, Scopus. 194 of them were duplicates. After removing the duplicates and the title and abstract screening, 963 articles were excluded as they did not follow our inclusion criteria, while 39 full-text articles were evaluated for eligibility. Finally, the meta-analysis included four RCTs (Fig. 1).
Preferred reporting items for systematic reviews and meta-analyses (PRISMA). From reference17. For more information, visit: http://www.prisma-statement.org/.
Summary of the included studies
1600 patients made up the whole sample size of the meta-analysis. 798 patients received tezepelumab, and 802 patients received a placebo. Patients were allowed to use the concomitant medication in the four studies. In contrast, patients were allowed to utilize short-acting beta two agonists (SABA) as rescue medicine, and all participants in the study groups continued to receive inhaled glucocorticoids along with rescue medications that may or may not include oral glucocorticoids without alteration.
A comprehensive overview of the included trials is provided in Table 1.
Tables 2, 3 provide the baseline characteristics of the patients.
Quality assessment
ROB 2 tool evaluated the bias risk of the included trials from low to high risk. Figures 2, 3 illustrate the bias risk summary.
Randomization process bias: We evaluated all the included trials as low risk for the randomization process.
Intended interventions bias: In terms of deviations from the intended interventions, the majority of the included trials showed a low risk of bias except for Diver S. et al. 2021, which were judged as high risk. This is because the statistical analysis that was done to calculate the impact of assignments was as treated analysis, and there was a loss during the follow-up exceeding 5% of the population.
Missing outcome data bias: Due to the use of the intention to treat analysis, most included trials had a low risk of bias in the missing outcome data, except Diver S et al. 2021. which had a high risk of bias because the authors used an as-treated analysis with 8% withdrawal in the intervention group, and they did not mention the reasons for exclusion in the intervention group.
Measurement outcome bias: Because all outcome assessors were blinded and used appropriate outcome measurement methods, we judged the bias risk in the measurement of the outcome as low in the majority of the included trials. Hence, due to the lack of information about blinding the outcome assessor, we judged Wechsler 2022 as having some concerns.
Selection of the reported results bias: We judged the risk of bias owing to the selection of the reported results of Wechsler 2022 as raised some concerns, but the other trials were rated low risk because all outcomes established in the results were in the protocols.
Other Bias: There is no other bias.
Publication bias
We couldn’t use Egger’s test for funnel plot asymmetry in this study to detect publication bias as we have only four studies, and for less than ten pooled studies, publication bias assessment is unreliable22.
Data-analysis
Annualized asthma exacerbation rate (AAERR)
Our analysis of annualized asthma exacerbation rate (AERR) includes three studies with a total of 739 patients in the tezepelumab arms and 745 patients in placebo arms, revealed a significant decrease in AERR favoring tezepelumab with MD -0.74 (95% CI [− 1.04, − 0.44], p < 0.00001). High heterogeneity was observed (p = 0.001, I2 = 85%) but we could not perform leave one out test as we have only three studies in the analysis. (Fig. 4).
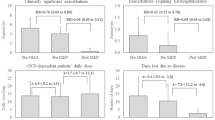
Change from the baseline in Pre-dose/pre-bronchodilator (pre-BD) forced expiratory volume in 1 s (FEV1)
Analysis of pre-BD FEV1 includes three studies with a total of 714 patients in the tezepelumab arms and 726 patients in placebo arms, revealed a significant increase in FEV-1 favoring tezepelumab with MD 0.16 (95% CI [0.10, 0.21], p < 0.00001). Low heterogeneity was found (p = 0.29, I2 = 20%) (Fig. 5).
Change from baseline in asthma control questionnaire-6 (ACQ-6) score
Analysis of ACQ-6 score includes three studies with a total of 638 patients in the tezepelumab arms and 652 patients in placebo arms, revealed a significant decrease in ACQ-6 score favoring tezepelumab with MD − 0.32 (95% CI [− 0.43, − 0.21], p < 0.00001). Heterogeneity evidence was found (p = 0.93, I2 = 0%) (Fig. 6).
Change from baseline in standardized asthma quality of life questionnaire for 12 years and older (AQLQ + 12) total score
Analysis of AQLQ + 12 total score includes three studies with a total of 634 patients in the tezepelumab arms and 643 patients in placebo arms, revealed a significant increase in AQLQ + 12 score favoring tezepelumab with MD 0.32 (95% CI [0.20, 0.44], p < 0.00001). Heterogeneity evidence was found (p = 0.68, I2 = 0%) (Fig. 7).
Change from the baseline in blood eosinophil count
Analysis of blood eosinophil count includes three studies with a total of 575 patients in tezepelumab arms and 574 patients in placebo arms, which revealed a significant decrease in blood eosinophil count favoring tezepelumab with MD -139.38 cells/mcL (95% CI [− 150.37, − 128.39], p < 0.00001). Heterogeneity evidence was found (p = 0.40, I2 = 0%) (Fig. 8).
Change from the baseline in FeNO
Analysis of FeNO levels includes four studies with a total of 646 patients in the tezepelumab arms and 643 patients in placebo arms, which revealed a significant decrease in FeNO levels favoring tezepelumab with MD − 10 ppb (95% CI [− 15.81, − 4.18], p = 0.0008). High heterogeneity was observed (p < 0.00001, I2 = 97%), which was solved by sensitivity analysis excluding Corren et al. 2021 (p = 0.59, I2 = 0%) (Fig. 9).
Change from the baseline in serum total IgE
Analysis of serum total IgE includes three studies with a total of 601 patients in the tezepelumab arms and 593 patients in placebo arms, revealed a significant decrease in serum total IgE favoring tezepelumab with MD -123.51 UI/ml (95% CI [− 206.52, − 40.50], p = 0.004). Low heterogeneity was found (p = 0.38, I2 = 0%) (Fig. 10).
Adverse effects
Tezepelumab significantly lowers the risk of any serious adverse effects than placebo, with RR 0.71 (95% CI [0.54, 0.93], p = 0.01), as opposed to the analysis of any adverse effects showing no significant risk reduction between tezepelumab and placebo with RR 0.92 (95% CI [0.62, 1.38], p = 0.70). (Figs. 11, 12).
Discussion
This study revealed significant improvements in asthma management, lung functional status, well-being, and quality of life with tezepelumab treatment compared to placebo. Tezepelumab significantly decreased the occurrence of asthma exacerbations in adults with chronic uncontrolled asthma, including those with reduced blood eosinophil levels, compared to placebo. In addition, tezepelumab showed significant improvements in ACQ-6, AQLQ(S) + 12 scores, and FEV1, decreasing hospitalization or emergency room visits. However, the tezepelumab and placebo groups did not differ significantly regarding the frequency and kinds of adverse incidents.
Tezepelumab concurrently decreased blood eosinophil count, FENO, and serum total IgE levels, indicating that the drug inhibits numerous inflammatory pathways. Tezepelumab influence on these biomarker levels could be linked to the lower levels of interleukin-5 and interleukin-1323. The observed decrease in serum total IgE levels could be related to lower levels of interleukin-4 and interleukin-13, which would result in a gradual reduction in B-cell shifting from IgM to IgE isotype production. These findings support the theory that TSLP inhibition has a more considerable physiological impact than just targeting individual T2 cytokines24.
In response to stimulation (including irritants, infections, harmful airborne particles, and traumatic agents), the function of TSLP as an early mediator between cells of immunity and epithelial cells of the airways indicates that tezepelumab may normalize local inflammation through allergic and non-allergic mechanisms, regardless of blood eosinophil count. It is anticipated that TSLP inhibition will reduce the T2 cytokine produced by T-memory cells, mast cells, and innate lymphocyte type 2 cells across the spectrum of inflammation. The roles of TSLP in triggering responsiveness via dendritic cells and interactions between mast cells and smooth muscle cells of the air passages are pathways that could be important to inflammation in low-eosinophil populations13,25,26.
According to a previous systematic review, omalizumab, tezepelumab, and dupilumab may modulate airway hyperresponsiveness by direct action on smooth muscle cells in the airway, in addition to indirect effects on parasympathetic activity and eosinophilic inflammation27. Another worldwide study on adolescents and adults showed that tezepelumab reduced the annual occurrence of asthma symptoms significantly in adults and adolescents with severe uncontrolled asthma, even in individuals who have blood eosinophil counts as low as 300 cells per microliter at baseline28. Furthermore, another trial, “The PATHWAY” (NCT03347279), showed more reduction in the asthma symptoms yearly incidence than “The NAVIGATOR” trial (NCT02054130).
Tezepelumab, as compared to placebo, decreased exacerbations in patients who have or who do not have perennial allergy in a 52-week trial. Furthermore, lung function was enhanced, and blood eosinophil counts and FENO levels decreased regardless of allergy status. In this study, no significant differences were found in the majority of asthma severity assessments between individuals who have and who do not have allergies at baseline. However, there were some differences in the biological indicators of the inflammatory process: patients who have allergic reactions had greater serum total IgE and high FENO at baseline, without discernible change in plasma eosinophil count. Rhinitis and atopic dermatitis were also more prevalent in allergy patients than in non-allergy patients and younger ones29.
Patients who took tezepelumab instead of a placebo had a more significant percentage of responders as evaluated by the AQLQ(S) + 12 and ACQ-630. The percentage of placebo patients whose ACQ-6 and AQLQ(S) + 12 scores increased by clinically significant levels was between 61–78% and 70%, respectively. This finding is consistent with evidence from studies investigating other biologic therapies in asthma31,32,33,34. The high number of placebo group responders in these studies might be attributed to greater adherence to standard-of-care medicines while participating in these clinical trials. Furthermore, several trials have demonstrated that a patient’s impression of the benefits of clinical trial participation may result in a positive response to placebo therapy35,36.
Tezepelumab did not decrease submucosal neutrophil cells or lymphocyte cells of the airways, which is reassuring from a safety standpoint. Eosinophil-depleting medications do not cause clinically significant immunosuppressive response, as evidenced by the fact that there was no increased incidence of infectious events in the tezepelumab compared to placebo groups in the previous trial37. Also, Corren et al. found that tezepelumab was safe, the number of patients was modest, and treatment was administered every 2 or 4 weeks for a total duration of 1 year15.
Strengths and limitations
Tezepelumab efficacy and safety in patients with severe uncontrolled asthma were summarized in this systematic review and meta-analysis. The study includes four RCTs, yielding a high level of evidence. The studies included ranged in quality from poor to excellent. The study limitations were due to the inherent research: RCTs have often been conducted in small, carefully selected groups of asthmatic patients. Furthermore, the majority of the identified heterogeneity was not resolved. Moreover, due to the small number of papers included, publication bias could not be examined. In addition, we could not get data of Wechsler 2022 from its full text, so we got its data from the protocol.
Conclusion
Tezepelumab provided considerable ability to control the exacerbations of severe uncontrolled adult asthmatics. However, minimal is known regarding the actual clinical impact of monoclonal antibodies like tezepelumab in the treatment of asthma. Further research involving large, ethnically varied samples of individuals with uncontrolled asthma is critical to address this clinical challenge for long-term illness care.
Data availability
All data generated or analyzed during this study are included in this published article or in the data repositories listed in references.
Abbreviations
- TSLP:
-
Thymic stromal lymphopoietin
- AAERs:
-
Annualized asthma exacerbation rates
- GINA:
-
The global initiative of asthma
- ICSs:
-
Inhaled corticosteroids
- PRISMA:
-
The preferred reporting items for systematic reviews and meta‐analyses
- CENTRAL:
-
Cochrane central register of controlled trials
- RCT:
-
Randomized controlled trials
- pre-BD:
-
Pre-dose/pre-bronchodilator
- FEV1:
-
Forced expiratory volume in 1 s
- ACQ-6 score:
-
Asthma control questionnaire-6 score
- AQLQ(S) + 12 total score:
-
Standardized asthma quality of life questionnaire for 12 years and older total score
- EQ-5D-5L:
-
European quality of life-5 dimensions 5 level version
- TEAEs:
-
Treatment-emergent adverse events
- TESAEs:
-
Treatment-emergent serious adverse events
- SABA:
-
Short-acting beta two agonists
- MD:
-
Mean difference
References
Global Initiative for A. Pocket Guide for Asthma Management and Prevention: (For Adults and Children Older than 5 Years) (Global Initiative for Asthma, 2018).
To, T. et al. Global asthma prevalence in adults: Findings from the cross-sectional world health survey. BMC Public Health 12, 1–8 (2012).
Fahy, J. V. Type 2 inflammation in asthma—Present in most, absent in many. Nat. Rev. Immunol. 15, 57–65 (2015).
Brightling, C. E., Gupta, S., Gonem, S. & Siddiqui, S. Lung damage and airway remodelling in severe asthma. Clin. Exp. Allergy 42, 638–649 (2012).
Hough, K. P. et al. Airway remodeling in asthma. Front. Med. 7, 191 (2020).
Walls, A. F., Roche, W. R., Howarth, P. H. & Holgate, S. T. Effect of an inhaled corticosteroid on airway inflammation and symptoms in asthma1-3. Am. Rev. Respir. Dis. 145, 669–714 (1992).
Busse, W. W. et al. BORA study investigators long-term safety and efficacy of benralizumab in patients with severe, uncontrolled asthma: 1-year results from the BORA phase 3 extension trial. Lancet Respir. Med. 7, 46–59 (2019).
Busse, W. W. et al. Quest LA. Phase 3 randomized, double-blind, placebo-controlled, parallel-group study to evaluate dupilumab efficacy/safety in patients with uncontrolled, moderate-to-severe asthma. Adv. Ther. 35, 737–48 (2018).
Normansell, R., Walker, S., Milan, S. J., Walters, E. H. & Nair, P. Omalizumab for asthma in adults and children. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD003559.pub4 (2014).
Carr, T. F., Zeki, A. A. & Kraft, M. Eosinophilic and noneosinophilic asthma. Am. J. Respir. Crit. Care Med. 197, 22–37 (2018).
Hinks, T. S. C., Levine, S. J. & Brusselle, G. G. Treatment options in type-2 low asthma. Eur. Respir. J. 57, 2000528 (2021).
Corren, J. & Ziegler, S. F. TSLP: From allergy to cancer. Nat. Immunol. 20, 1603–1609 (2019).
Gauvreau, G. M., Sehmi, R., Ambrose, C. S. & Griffiths, J. M. Thymic stromal lymphopoietin: Its role and potential as a therapeutic target in asthma. Expert Opin. Ther. Targets 24, 777–792 (2020).
Wu, J. et al. Thymic stromal lymphopoietin promotes asthmatic airway remodelling in human lung fibroblast cells through STAT3 signalling pathway. Cell Biochem. Funct. 31, 496–503 (2013).
Corren, J. et al. Tezepelumab in adults with uncontrolled asthma. N. Engl. J. Med. 377, 936–946 (2017).
Gauvreau, G. M. et al. Effects of an anti-TSLP antibody on allergen-induced asthmatic responses. N. Engl. J. Med. 370, 2102–2110 (2014).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 10, 1–11 (2021).
Higgins, J. P. T., Green, S. & Cochrane, C. Cochrane Handbook for Systematic Reviews of Interventions (Wiley-Blackwell, 2008).
Global strategy for asthma management and prevention updated. http://ginasthma.org. Accessed 21 May 2022. (2012).
Sterne, J. A. C. et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 366, l4898 (2019).
Higgins, J. P. T. Measuring inconsistency in meta-analyses. BMJ 327, 557–560 (2003).
Egger, M., Smith, G. D., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634 (1997).
Pham, T. H., Ren, P., Parnes, J. R. & Griffiths, J. M. Tezepelumab reduces multiple key inflammatory biomarkers in patients with severe, uncontrolled asthma in the phase 2b PATHWAY study. In B21. Severe Asthma: Clinical and Mechanistic Studies (eds Pham, T. H. et al.) A2677 (American Thoracic Society, 2019).
Janeway, C. A. Jr., Travers, P., Walport, M. & Shlomchik, M. J. The production of IgE. In Immunobiology: The Immune System in Health and Disease 5th edn (eds Janeway, C. A., Jr. et al.) (Garland Science, 2001).
Allakhverdi, Z., Comeau, M. R., Jessup, H. K. & Delespesse, G. Thymic stromal lymphopoietin as a mediator of crosstalk between bronchial smooth muscles and mast cells. J. Allergy Clin. Immunol. 123, 958–960 (2009).
Tanaka, J. et al. Human TSLP and TLR3 ligands promote differentiation of Th17 cells with a central memory phenotype under Th2-polarizing conditions. Clin. Exp. Allergy 39, 89–100 (2009).
Calzetta, L. et al. The impact of monoclonal antibodies on airway smooth muscle contractility in asthma: A systematic review. Biomedicines 9, 1281 (2021).
Menzies-Gow, A. et al. Tezepelumab in adults and adolescents with severe, uncontrolled asthma. N. Engl. J. Med. 384, 1800–1809 (2021).
Corren, J. et al. Efficacy of tezepelumab in patients with severe, uncontrolled asthma and perennial allergy. J. Allergy Clin. Immunol. 9, 4334–42 (2021).
Corren, J. et al. Tezepelumab improves patient-reported outcomes in patients with severe, uncontrolled asthma in PATHWAY. Ann. Allergy Asthma Immunol. 126, 187–193 (2021).
Castro, M. et al. Benralizumab, an anti-interleukin 5 receptor α monoclonal antibody, versus placebo for uncontrolled eosinophilic asthma: A phase 2b randomised dose-ranging study. Lancet Respir. Med. 2, 879–890 (2014).
Castro, M., Zangrilli, J. & Wechsler, M. E. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: Results from two multicentre, parallel, double-blind, randomised, placebo-controlled, phase 3 trials (vol 3, pg 355, 2015). Lancet Respir. Med. 4, E50 (2016).
Corren, J. et al. Dupilumab improves symptoms, quality of life and productivity in uncontrolled persistent asthma. Ann. Allergy Asthma Immunol. 122, 41–49 (2019).
Piper, E. et al. A phase II placebo-controlled study of tralokinumab in moderate-to-severe asthma. Eur. Respir. J. 41, 330–338 (2013).
Castro, M. et al. Asthma intervention research 2 (AIR2) trial. Am. J. Respir. Crit. Care Med. 181, 116–124 (2010).
Wechsler, M. E. et al. Active albuterol or placebo, sham acupuncture, or no intervention in asthma. N. Engl. J. Med. 365, 119–126 (2011).
Diver, S. et al. Effect of tezepelumab on airway inflammatory cells, remodelling and hyperresponsiveness in patients with moderate-to-severe uncontrolled asthma (CASCADE): A double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Respir. Med. 9, 1299–1312 (2021).
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). All author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
M.S.A. led the team, carried out the search strategy and data collection steps, resolved any conflicts during the screening phase, and resolved any conflicts during the quality evaluation phase, and drafted the tables. A.K.A. took part in the quality assessment, data extraction, and meta-analysis. E.R.G. took part in the full-text screening, quality assessment, and data extraction. A.A.E. wrote the introduction and discussion sections and edited the manuscript. M.M.A. contributed to the full-text screening and writing the result section. R.A.F. was involved in the title and abstract screening and wrote the introduction section. B.H.S. took part in the title and abstract screening and writing the methods section. M.A.-E. supervised the authors in all steps and performed peer-review. All authors reviewed the final manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shaban Abdelgalil, M., Ahmed Elrashedy, A., Awad, A.K. et al. Safety and efficacy of tezepelumab vs. placebo in adult patients with severe uncontrolled asthma: a systematic review and meta-analysis. Sci Rep 12, 20905 (2022). https://doi.org/10.1038/s41598-022-24763-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-24763-9
This article is cited by
-
Effects of Tezepelumab on Quality of Life of Patients with Moderate-to-Severe, Uncontrolled Asthma: Systematic Review and Meta-Analysis
Current Allergy and Asthma Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.