Abstract
Chronic low back pain, defined as low back pain lasting more than 3 months, is a globally prevalent health problem with significantly high medical and economic burden on individuals and the society. This study aimed to estimate the prevalence of chronic low back pain and examine its association with health outcomes including physical function, mental health, and quality of life among adult population in Singapore. Cross-sectional secondary data analysis was performed using baseline data of the 1941 adults (mean age: 52.6 years, range: 21–97 years) from a representative population health survey conducted in the Central region of Singapore. Those with self-reported chronic low back pain in past six months were identified. The Late-Life Function and Disability Instrument, Patient Health Questionnaire-9, and EQ-5D-5L were used to measure physical function and limitation, mental health, and health-related quality of life, respectively. Generalized Linear Regressions were used to examine the association of chronic low back pain with physical function, limitation, depressive symptoms, and health-related quality of life. There were 8.1% (n = 180) participants reporting having chronic low back pain in past six months, among whom 80.5% sought treatments at either primary care, specialist outpatient, or Traditional Chinese Medicine clinics. Individuals with chronic low back pain reported poorer physical function, more limitations in performing major life tasks and social activities, more depressive symptoms, and lower health-related quality of life (all p < 0.01), even after adjusting for socio-demographics, lifestyle factors, and number of morbidities. The prevalence of chronic low back pain was 8.1% among the study population. Chronic low back pain was associated with poorer physical function, more limitations and depressive symptoms, and lower health-related quality of life. The findings highlight the significant impact of chronic low back pain on physical function and limitation, mental health, and health-related quality of life in a general population. Increased awareness on prevention, early and proper management of low back pain, and rehabilitation policies are required to better tackle the burden of low back pain at the population level.
Similar content being viewed by others
Introduction
Low back pain (LBP) is a common musculoskeletal problem with high prevalence among middle-aged and older adults1,2. It was estimated that 49–90% of people in developed countries will develop LBP at some point in their life3. As the main contributor to the overall burden of musculoskeletal conditions, LBP remains the leading global cause of years of life with disability (YLDs) in 2019 worldwide4,5. In Singapore, musculoskeletal disorder is the leading cause of YLDs and LBP accounted for 9.5% of total YLDs: 10.3% among those aged 15–49 years, 10.1% among those aged 50–69 years old and 7.7% among those aged 70 years and above in 20196. LBP has become a great public health issue resulting in considerable medical and economic burden (including direct and indirect costs) to individuals, families, and the society7.
There have been many studies on the epidemiology of LBP in the past several decades. However, the accurate assessment of the prevalence remains challenging as there is little scientific evidence on LBP diagnosis3. Due to the heterogeneity of study population, design and methodology, the prevalence derived from different studies may not be directly comparable8. However, studies worldwide have consistently documented that LBP has significant impacts on individuals’ physical and psychosocial health. It not only limits one’s physical functioning and daily activities9,10, but also has the potential to cause higher levels of subclinical distress and depression11,12. A local study on LBP patients attending the Musculoskeletal Physiotherapy Clinic in a government-structured hospital also found that LBP results in significant disability and time lost off work13. When LBP persists for 12 weeks or longer, it becomes chronic low back pain (cLBP)14. CLBP may have more profound impacts on one’s performance of social responsibilities in family, work and social life, which may significantly affect the health-related quality of life (HRQoL)15,16.
In view of the significant burden of LBP (as estimated by YLDs), it is important to estimate the prevalence of cLBP, examine the potential risk factors, and evaluate its association with health outcomes among community-dwelling adults in Singapore. To date, there is scarcity of research on cLBP among general population in Singapore. To address this gap, we conducted this cross-sectional secondary data analysis by using population-based health survey data collected in the Central region of Singapore to (1) estimate the prevalence of cLBP in the community-dwelling adult population and healthcare seeking rates; (2) examine the association between cLBP and socio-demographic, lifestyle, and health factors, and (3) examine the association between cLBP and physical function and limitation, depressive symptoms, and HRQoL. We hypothesized that cLBP would have a negative impact on physical function and limitation, depressive symptoms, and HRQoL.
Methods
Study design and participants
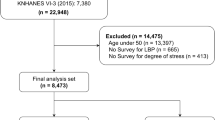
Cross-sectional secondary data analysis was performed using baseline data of the longitudinal Population Health Index (PHI) study, a population health survey conducted in the Central region of Singapore among representative community-dwelling adults. The participant recruitment for the PHI study was initiated in November 2015 and ended in January 2017, followed by two subsequent annual follow-ups. Singapore citizens and permanent residents who were aged 21 years and above and staying in any of the nine planning areas (PAs, including Novena, Geylang, Kallang, Rocher, Toa Payoh, Bishan, Serangoon, Ang Mo Kio, and Hougang) of the Central region of Singapore were eligible for the study. The estimated population in the Central region was 821,650 residents17.
The study design, sampling procedure, participant recruitment, and follow-up processes of the PHI survey were detailed elsewhere17,18 and the contents of the survey questionnaire were listed in another study19. In brief, a total of 5350 residential dwelling units from the nine PAs were proportionally selected from the National Database on Dwellings in Singapore maintained by the Department of Statistics. An invitation letter was sent to the selected dwelling units to notify and invite them to participate in the survey. During the house visits to the selected dwelling units by trained interviewers, Kish tables were used to identify one eligible household member from each dwelling unit to participate in the study. A total of 1942 individuals (response rate: 53.3%, based on 3645 eligible residents) were recruited and participated in the baseline survey.
All participants who responded to the question on cLBP at baseline (N = 1941) was sampled for this secondary data analysis. To ensure the sufficiency of this sample size for the study, we calculated the minimum number of necessary sample for prevalence studies using Scalex SP Version 1.0.120. The calculation result suggested that for the expected prevalence of 13.16%4, the required sample size was 1098 for the margin of error of ± 2% in estimating the prevalence with 95% confidence and considering the potential non-response rate of 50%. Hence, the actual sample size used in this study was sufficient.
Measures
Chronic low back pain status
Presence of cLBP was determined based on responses to the following question included in the PHI survey: “In the past 6 months, have you ever sought medical consultation/treatment for chronic low back pain (lasting for more than three months)?”. There were five options. An individual without cLBP would choose the option “No pain, not applicable” and those with cLBP but never sought medical consultation/treatment would select “With pain but never sought treatment”. Individuals with cLBP and sought medical consultation/treatment in past six months were asked to indicate where they received the consultation/treatment from: “Polyclinic/General Practitioner (GP)”, “Specialist Outpatient clinic (SOC)”, or “Traditional Chinese Medicine (TCM) Clinic”. Two or more options could be selected for the care setting. Based on their response to the question, the individuals were then categorized into either group: “without cLBP” or “with cLBP”.
Physical function and limitation
Overall physical function refers to the “ability to perform discrete actions or activities as part of daily routines without the help of others”21. The overall physical function was measured using the 32-item Function Domain of the Late-Life Function and Disability Instrument (Late-Life FDI) which include items measuring upper extremity functioning (7 items), basic lower extremity functioning (14 items), and advanced lower extremity functioning (11 items)21. The questions were phased “How much difficulty do you have (doing a particular activity) without the help of someone else and without the use of assistive devices?” with five response options of “5 = None”, “1 = A little”, “3 = Some”, “4 = Quite a lot”, and “5 = Cannot do”.
Individuals’ physical limitation in performing major life tasks and social activities in the community was assessed by the 16-item Limitation domain of the Late-Life FDI. The limitation questions were phrased “To what extent do you feel limited in (doing a particular task)?” and each question had five response options: “5 = Not at all”, “4 = A little”, “3 = Somewhat”, “2 = A lot”, and “1 = Completely”.
The raw scores of the Function and Limitation domains were calculated by summing up the respective item scores. They were then transformed to scaled scores ranging from 0 to 100 with 0 indicating worse function or more limitation and 100 indicating better overall function or less limitation21. The Late-Life FDI demonstrated high level of reliability with Cronbach’s alphas for Overall Function and Limitation of 0.97 and 0.94, respectively in the present study.
Mental health
The 9-item Patient Health Questionnaire (PHQ-9), a self-administered version of the Primary Care Evaluation of Mental Disorders diagnostic instrument for common mental disorders, was used to assess mental health22. A 4-point scale (0 = not at all, 1 = several days, 2 = more than half the days, 3 = nearly every day) was used to assess each PHQ-9 item. The score of each item was summed up to derive the total depressive symptoms score which ranges from 0 to 27, with a higher score indicating more or severer depressive symptoms22. As a well validated and widely used brief diagnostic and severity measure of depression, the PHQ-9 also demonstrated good internal consistency reliability (Cronbach's alpha = 0.77) in this study.
Health-related quality of life
HRQoL was measured using the EQ-5D-5L descriptive system of five domains (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) with five levels (level 1 = no problems, level 2 = slight problems, level 3 = moderate problems, level 4 = severe problems and level 5 = extreme problems)23. A single index value (EQ-5D index score) was derived from the EQ-5D-5L descriptive system, with 0 indicating death and 1 (the highest score) indicating complete health. An EQ-5D index score less than 0 indicated health state worse than death. As there was no available EQ-5D-5L value set for Singapore, the Japan value set24 was used to calculate the EQ-5D index score to represent a person’s HRQoL. The EQ visual analogue scale (VAS) records a person’s self-rated health on a vertical scale ranging from 0 (the worst health you can imagine) to 100 (the best health you can imagine). The EQ-5D-5L demonstrated acceptable internal consistency reliability in the present study with a Cronbach’s alpha of 0.77.
Other data collected
The socio-demographic factors used in the analysis included age in years, sex, marital status (single, married, and divorced/widowed), living arrangement (living alone vs living with others), and financial status assessed by self-reported money insufficiency for basic daily living (perceived money sufficiency vs insufficiency). Occupation was collected using the ten major groups described in the Singapore Standard Occupational Classification 201525 and re-categorized into three groups: PMETs (Professionals, Managers, Executives and Technicians, including Major Group 1–3, X), CSSWs (Clerical, Sales and Service Workers, including Major Group 4–5), and PTOCLs (Production and Transport Operators, Cleaners and Labourers, including Major Group 6–9). An additional group named “Others” was added to the occupational groups to represent individuals who were unemployed and inactive. In addition, lifestyle factors including smoking status (never smoked, former smoker, and current smoker) and alcohol misuse (yes and no, assessed by the Alcohol Use Disorders Identification Test Consumption screening tool26) were also included. Furthermore, the number of diagnosed chronic morbidities (0, 1, and 2 or more) was derived based on self-reported diagnosis of the 17 chronic diseases including dyslipidemia, high blood pressure, diabetes, chronic kidney disease, heart attack/ischemic heart disease, heart failure, stroke/transient ischemic attack, asthma, chronic bronchitis/emphysema/chronic obstructive pulmonary disease, cancer, osteoarthritis/gout/rheumatoid arthritis, osteoporosis, depression, anxiety disorder, schizophrenia, dementia/Alzheimer’s, and Parkinson’s disease27.
Data analysis
Characteristics of the study participants were described using mean and standard deviation (SD) for continuous variables, and frequency and weighted percentage for categorical variables. The weighted prevalence of cLBP for all participants and by individual socio-demographics, lifestyle and health categories were calculated. The weighted rates of seeking care at different care settings for all participants were reported. The differences in socio-demographics, lifestyle, and health characteristics between participants with and without cLBP were examined using chi-square tests for categorical variables and t-test for continuous variables. A logistic regression anaysis was performed to determine the factors associated with cLBP (dependent variable). Odds ratios (OR) and 95% confidence intervals (95% CI) were reported.
Health outcomes including physical function and limitation, depressive symptoms, and HRQoL were described using mean ± SD, median, and the first (Q1) and third quartiles (Q3). They were compared between participants with and without cLBP using chi-square tests for categorical outcome variables and Mann Whitney U tests for continuous outcome variables. As health outcome variables were generally skewed towards larger values, a series of Generalized Linear Models (GLM) with Gamma family distribution and log link function were performed to determine the association between cLBP (independent variable) and each health outcome (dependent variable), adjusting for socio-demographics (including age in years, sex, marital status, living arrangement, occupational groups, and financial status), lifestyle factors (including smoking status and alcohol misuse), and number of diagnosed chronic morbidities. Beta coefficients (B) and 95% CIs were reported. Any participant with missing data were omitted from the regression models. The number of records with missing data for the outcome variables were: Overall Function (n = 1, 0.05%), PHQ-9 depressive symptom score (n = 11, 0.57%), EQ5D anxiety and EQ5D Index (n = 4, 0.21%), and EQ VAS (n = 7, 0.36%). Variables in each model were tested for multicollinearity and those with a variance inflation factor (VIF) value of 5 or higher28 would be removed from the respective model.
All the analyses were conducted using Stata/SE 16.1 for Windows (StataCorp, College Station, TX) and a p value of 0.05 was set as the level of significance for all tests.
Ethics approval and consent to participate
The PHI study was approved by the ethics review committee of the National Healthcare Group Domain Specific Review Board (Reference Number: 2015/00269). The study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all individual participants after they were being informed about the study objectives and the safeguards put in place so that confidentiality of the collected data is maintained.
Results
Characteristics of participants
The characteristics of all the 1941 participants were described in Table 1. The mean age of the participants was 52.5 years old with a standard deviation of 16.9 years. Majority of the participants were Chinese (78.3%), 56.2% were females, and 36.9% were unemployed or inactive.
Prevalence of chronic low back pain and rates of care seeking
There were 180 participants (weighted percentage: 8.1%) reported having cLBP in past 6 months. Among the 180 participants reported having cLBP, 143 (80.5%) sought consultations or treatments at polyclinics/GPs (46.2%), SOCs (43.5%) or TCM clinics (40.1%) in past 6 months, and 20.7% sought consultations or treatments at two or more of these three care settings.
Socio-demographics associated with chronic low back pain
Compared to those who did not report cLBP (n = 1761), individuals reporting cLBP (n = 180) were significantly older (mean ± SD: 57.2 ± 17.5 vs 52.1 ± 16.7) with higher proportion of individuals aged 75 years and above (20.0% vs 9.0%), and more likely to be divorced/widowed (22.4% vs 10.2%) or living alone (8.2% vs 5.1%), more likely to report having no formal education (24.4% vs 13.3%), money insufficiency (31.4% vs 12.8%) or having two or more chronic conditions (54.7% vs 33.3%) (Table 1). After adjusting for the rest of the categorical socio-demographic factors showed in Table 1, individuals who were females (OR 1.55, 95% CI 1.04, 2.32), perceiving money insufficiency for basic daily living (OR 2.71, 95% CI 1.84, 3.99), and having existing comorbidity (OR 3.36, 95% CI 2.09, 5.41) had higher risk of cLBP (Table 2).
Association between chronic low back pain and health outcomes
The comparison of physical function and limitation, mental health (depressive symptoms), and HRQoL between individuals with and without cLBP in past six months showed that those with cLBP had significantly lower overall function, more limitation, and more depressive symptoms. Individuals experienced cLBP had significantly higher proportions of individuals having problem in morbidity, self care, activity, or having pain or anxiety compared to those who did not have cLBP (Table 3). Individuals with cLBP also had lower HRQoL (lower EQ-5D index score and EQ5D VAS). Although those sought consultation/treatment for cLBP had relatively lower mean scores in overall function, limitation, and HRQoL, and higher depressive symptom score compared to those did not seek consultation/treatment, these differences were not significant (all p > 0.05).
The GLM regression analysis results in Table 4 showed that cLBP remained significantly associated with lower overall physical function (B = − 0.08, 95% CI − 0.10, − 0.05), more physical limitation (B = − 0.04, 95% CI − 0.07, − 0.01), more or severer depressive symptoms (B = 0.63, 95% CI 0.32, 0.94), and worse HRQoL (EQ-5D Index: B = − 0.07, 95% CI − 0.09, − 0.05, EQ VAS: B = − 0.10, 95% CI − 0.13, − 0.07), even after adjusting for covariates (age was excluded from the models due to collinearity). The full generalized linear regression results including all adjusted variables are presented in Supplementary Table S1.
Discussion
Chronic low back pain is a major public health issue with considerably high medical, social, and economic impacts. This study estimated the prevalence of cLBP and rates of care in different settings, identified the potential factors associated with cLBP and examined the association of cLBP with health outcomes in representative community-dwelling adults in the Central region of Singapore. The results showed that the prevalence of cLBP was 8.1% in the study population, of whom 80.5% sought consultation/treatment at polyclinics/GPs, SOCs, or TCM clinics. The study identified significant association of cLBP with physical function and limitation, mental health, and HRQoL in the context of a community setting in Singapore.
The prevalence of cLBP in the study population was 8.1%, which is slightly higher than 7.5% – the estimated global age-standardized point prevalence of LBP (ranging from 3.92% in East Asia to 13.47% in Latin America) in 20174. Existing evidence on the prevalence of LBP in different populations varies widely. The point-prevalence of LBP based on general population surveys in four high-income western countries (Britain, Belgium, Germany, and Sweden) ranged from 14% (Britain) to 35% (Sweden)29. One literature review reported that the one-year prevalence of LBP among adults was estimated to range from 15 to 20%8. A population-based study conducted in Taiwan reported that 25.7% reported LBP within the past three months30. It is also worth highlighting that these studies reported the prevalence of LBP without differentiating acute or chronic condition. In our study, we only identified cLBP (lasting for more than three months) in past six months. Hence, the prevalence of LBP in our study population (8.1%) was lower than the age-standardized point prevalence of LBP estimated for high-income Asia Pacific countries (13.16%)4, however, it was much higher than the prevalence reported in North Carolina population (3.9%) more than 20 years ago31. The heterogeneity in study population, definition or inclusion criteria for LBP, data source, measure used (point or lifetime prevalence, pooled, or age-standardized prevalence), and duration of observation across studies32 might explain the wide variation in LBP or cLBP prevalence across countries.
Among individuals who reported having cLBP in past 6 months, 80.5% sought consultation/treatment at different care settings with comparable rates ranging from 40.1% at TCM clinics to 46.2% at polyclinics/GPs. Unfortunately, care seeking in any emergency department of hospitals was not surveyed. The physician visit rate for LBP in past year was 61.2% in Spain33 while the pooled health-care utilisation rates for LBP from any health-care provider as reported in a systematic review was 67% in USA, 48% in Europe, and 47% in UK32. The higher care seeking rate observed in our study could be potentially explained by the higher distress caused by cLBP compared to acute LBP.
Consistent with the global trend that females had higher prevalence of cLBP than males4, the prevalence of cLBP in female adults in our population was 8.9%, which was slightly but not significantly higher than that in males (7.1%, p = 0.093). However, after adjusting for other socio-demographics, lifestyle factors and number of chronic morbidities, females had higher odds of cLBP. This study found cLBP was prevalent in the elderly aged 75 years and above and increasing age was associated with a higher odd of cLBP in univariate analysis, however, the association was no longer significant after adjusting for other covariates. Smoking34, lower education, and occupation30 were found to be risk factors for the development of LBP. Prior studies found that LBP is highly prevalent among agricultural/forestry/fishery workers35 and less well educated individuals36,37. Our study found individuals who were PTOCLs (blue-collar workers) and having no formal education had higher prevalence of cLBP, however, they were no longer associated with cLBP after controlling for the covariates. Consistent with other studies38,39, our study further confirmed that lower subjective economic situation (measured by self-reported money insufficiency for basic daily living in this study) and having multiple chronic morbidities were significantly associated with cLBP, even after adjusting for other covariates.
Prior studies have documented that LBP was associated with both physical function and mental wellbeing11,40,41,42. Although this study did not capture current existing or acute LBP which lasted for less than 3 months, we still observed significant association between cLBP and physical function, limitation, and depressive symptoms even after controlling for socio-demographics, lifestyle factors, and number of morbidities. The findings further showed that cLBP corresponded to reporting problems in all domains of HRQoL as measured by EQ-5D-5L. Consistent with the findings from a French study43, the association between cLBP and poorer HRQoL remained after controlling for socio-demographics, lifestyle and number of morbidities. Our findings underscore the significant impacts of cLBP on health outcomes and highlight the necessity of raising public awareness on LBP prevention and proper treatment. Although one local study found the association of occupational groups with physical and mental health44, it was not observed in our study.
To our knowledge, this is the first study estimating the prevalence of cLBP and care seeking rates and examining the association of cLBP with various health outcomes in community-dwelling adult population in Singapore. The sampling procedures ensured the study sample to be representative of the community-dwelling adults in the Central region of Singapore. This allows the findings to be generalised to this population. While the findings provide better understanding of cLBP in our population, several limitations should be acknowledged. Firstly, our study is restricted to cLBP whereas many other studies included both chronic and acute LBP. Hence, the actual prevalence of LBP in Singapore might be even higher; and the prevalence reported in our study and those reported in many other studies cannot be directly compared. Secondly, the cLBP status and settings of care seeking were based on self-reported data without using medical/professional assessment or hospital/clinic records as additional verification, hence, data used in this study might be subject to recall errors. Thirdly, although we did not observe significant differences in health outcomes between individuals who sought consultation/treatment and those did not, as the severity of cLBP was not collected, we could not infer whether the non-significant difference was due to the small sample size of participants with cLBP or the difference in severity of cLBP. Fourthly, as the study participants were only sampled from the community-dwelling adults in the Central region of Singapore, individuals who were hospitalised or institutionalised were not surveyed, therefore, the study findings could not be generalised to the entire adult population in Singapore. Hence, our findings should be interpreted with caution.
Conclusions
The prevalence of chronic low back pain was 8.1% among the study population and 80.5% individuals with cLBP sought consultation/treatment in either primary care, SOC or TCM clinics. CLBP was associated with poorer physical function, more limitations and depressive symptoms, and lower health-related quality of life. The findings highlight the significant impact of cLBP on physical and mental health as well as health-related quality of life in a general adult population. Increased awareness on prevention, early and proper management of LBP, and rehabilitation policies are required to better tackle the burden of LBP at the population level.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to the laws, rules and regulations stated in the “Advisory Guidelines for the Healthcare Sector”, but are available from the corresponding author on reasonable request.
Abbreviations
- cLBP:
-
Chronic low back pain
- CSSWs:
-
Clerical, sales and service workers
- DALYs:
-
Disability-adjusted life years
- EQ VAS:
-
EQ visual analogue scale
- GLM:
-
Generalized linear models
- GP:
-
General practitioner
- HRQoL:
-
Health-related quality of life
- LBP:
-
Low back pain
- Late-Life FDI:
-
Late-life function and disability instrument
- OR:
-
Odds ratio
- PA:
-
Planning areas
- PMETs:
-
Professionals, managers, executives, and technicians
- PHQ-9:
-
9-Item patient health questionnaire
- PHI:
-
Population health index
- PTOCLs:
-
Production and transport operators, cleaners & labourers
- Q1:
-
The first quartile (25th percentile)
- Q3:
-
The third quartile (75th percentile)
- SD:
-
Standard deviation
- SOC:
-
Specialist outpatient clinic
- TCM:
-
Traditional Chinese medicine
- VAS:
-
Visual analogue scale
- YLDs:
-
Years of life with disability
References
Taguchi, T. Low back pain in young and middle-aged people. J. Jpn. Med. Assoc. 46, 7 (2003).
de Souza, I. M. B. et al. Prevalence of low back pain in the elderly population: A systematic review. Clinics 74, 789 (2019).
Scott, N. A., Moga, C. & Harstall, C. Managing low back pain in the primary care setting: The know-do gap. Pain Res. Manag. 15, 392–400 (2010).
Wu, A. et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the Global Burden of Disease Study 2017. Ann. Transl. Med. 8, 299 (2020).
Chen, S. et al. Global, regional and national burden of low back pain 1990–2019: A systematic analysis of the Global Burden of Disease study 2019. J. Orthop. Transl. https://doi.org/10.1016/j.jot.2021.07.005 (2021).
Institute for Health Metrics and Evaluation. GBD Compare-Singapore. IHME Viz Hub. 2021. http://vizhub.healthdata.org/gbd-compare. Accessed 26 Oct 2021.
Alonso-García, M. & Sarría-Santamera, A. The economic and social burden of low back pain in Spain: A national assessment of the economic and social impact of low back pain in Spain. Spine 45, E1026 (2020).
Rubin, D. I. Epidemiology and risk factors for spine pain. Neurol. Clin. 25, 353–371 (2007).
Lee, H. et al. How does pain lead to disability? A systematic review and meta-analysis of mediation studies in people with back and neck pain. Pain 156, 988–997 (2015).
Martin, B. I. et al. Expenditures and health status among adults with back and neck problems. JAMA 299, 656–664 (2008).
Robertson, D., Kumbhare, D., Nolet, P., Srbely, J. & Newton, G. Associations between low back pain and depression and somatization in a Canadian emerging adult population. J. Can. Chiropr. Assoc. 61, 96–105 (2017).
Siddiqui, D., Khan, S., Saher, T. & Siddiqui, H. A. Association of chronic low back pain with depression and anxiety. J. Physiother. Res. 4, 1–10 (2020).
Goh, M. R., Po, I. Y. Y. & Olafsdottir, K. Low back pain in changi general hospital: An observational study. Proc. Sing. Healthc. 19, 175–182 (2010).
National Institute of Health. Low Back Pain Fact Sheet. Fact Sheet (National Institute of Neurological Disorders and Stroke, 2020).
Járomi, M. et al. Assessment of health-related quality of life and patient’s knowledge in chronic non-specific low back pain. BMC Public Health 21, 1479 (2021).
Montazeri, A. & Mousavi, S. J. Quality of life and low back pain. In Handbook of Disease Burdens and Quality of Life Measures (eds Preedy, V. R. & Watson, R. R.) 3979–3994 (Springer, 2010).
Yap, C. W., Ge, L., Ong, R., Li, R. & Heng, B. H. Development of a scalable and extendable multi-dimensional health index to measure the health of individuals. PLoS ONE 15, e0240302 (2020).
Ge, L., Yap, C. W., Ong, R. & Heng, B. H. Social isolation, loneliness and their relationships with depressive symptoms: A population-based study. PLoS ONE 12, e0182145 (2017).
Ge, L., Yap, C. W. & Heng, B. H. Prevalence of frailty and its association with depressive symptoms among older adults in Singapore. Aging Ment. Health. 1, 1–6 (2018).
Naing, L., Nordin, R. B., Abdul Rahman, H. & Naing, Y. T. Sample size calculation for prevalence studies using Scalex and ScalaR calculators. BMC Med. Res. Methodol. 22, 209 (2022).
Haley, S. M. et al. Late life function and disability instrument. II. Development and evaluation of the function component. J. Gerontol. A. 57, 217–222 (2002).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613 (2001).
Cheung, Y. B., Luo, N., Ng, R. & Lee, C. F. Mapping the functional assessment of cancer therapy-breast (FACT-B) to the 5-level EuroQoL Group’s 5-dimension questionnaire (EQ-5D-5L) utility index in a multi-ethnic Asian population. Health Qual. Life Outcomes. 12, 180 (2014).
Shiroiwa, T. et al. Comparison of value set based on DCE and/or TTO data: Scoring for EQ-5D-5L health states in Japan. Value Health. 19, 648–654 (2016).
Singapore Department of Statistics. Singapore Standard Occupational Classification (SSOC). (2015).
Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D. & Bradley, K. A. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP): Alcohol Use Disorders Identification Test. Arch. Intern. Med. 158, 1789–1795 (1998).
Ge, L., Yap, C. W. & Heng, B. H. Sex differences in associations between multimorbidity and physical function domains among community-dwelling adults in Singapore. PLoS ONE 13, e0197443 (2018).
Hair, J. F., Ringle, C. M. & Sarstedt, M. PLS-SEM: Indeed a silver bullet. J. Mark. Theor. Pract. 19, 139–152 (2011).
Volinn, E. The epidemiology of low back pain in the rest of the world: A review of surveys in low- and middle-income countries. Spine 22, 1747–1754 (1997).
Chou, Y.-C., Shih, C.-C., Lin, J.-G., Chen, T.-L. & Liao, C.-C. Low back pain associated with sociodemographic factors, lifestyle and osteoporosis: A population-based study. J Rehabil. Med. 45, 76–80 (2013).
Carey, T. S. et al. Care-seeking among individuals with chronic low back pain. Spine 20, 312–317 (1995).
Beyera, G. K., O’Brien, J. & Campbell, S. Health-care utilisation for low back pain: A systematic review and meta-analysis of population-based observational studies. Rheumatol. Int. 39, 1663–1679 (2019).
Carmona, L., Ballina, J., Gabriel, R. & Laffon, A. The burden of musculoskeletal diseases in the general population of Spain: Results from a national survey. Ann. Rheum. Dis. 60, 1040–1045 (2001).
Deyo, R. A. & Bass, J. E. Lifestyle and low-back pain: The influence of smoking and obesity. Spine 14, 501–506 (1989).
Tomioka, K., Shima, M. & Saeki, K. Occupational status and self-reported low back pain by gender: A nation-wide cross-sectional study among the general population in Japan. Environ. Health Prev. Med. 26, 111 (2021).
Dionne, C. et al. Formal education and back pain: A review. J. Epidemiol. Community Health. 55, 455–468 (2001).
Kwon, M. A. et al. A correlation between low back pain and associated factors: A study involving 772 patients who had undergone general physical examination. J. Korean Med. Sci. 21, 1086–1091 (2006).
Ikeda, T. et al. Socioeconomic inequalities in low back pain among older people: The JAGES cross-sectional study. Int. J. Equity Health. 18, 15 (2019).
Williams, J. S. et al. Risk factors and disability associated with low back pain in older adults in low- and middle-income countries: Results from the WHO Study on Global AGEing and Adult Health (SAGE). PLoS ONE 10, e0127880 (2015).
Nassar, N., Assaf, N., Farrag, D., Ibrahim, D. & Al-Sheekh, A. Depression in patients with chronic low back pain. Egypt Rheumatol. Rehabil. 46, 48–54 (2019).
Rudy, T. E., Weiner, D. K., Lieber, S. J., Slaboda, J. & Boston, R. J. The impact of chronic low back pain on older adults: A comparative study of patients and controls. Pain 131, 293–301 (2007).
Weiner, D. K. et al. How does low back pain impact physical function in independent, well-functioning older adults? Evidence from the Health ABC cohort and implications for the future. Pain Med. 4, 311–320 (2003).
Husky, M. M., Ferdous Farin, F., Compagnone, P., Fermanian, C. & Kovess-Masfety, V. Chronic back pain and its association with quality of life in a large French population survey. Health Qual. Life Outcomes. 16, 195 (2018).
Sambasivam, R. et al. Occupational groups and its physical and mental health correlates: Results from the Singapore Mental Health Study 2016. Int. Arch. Occup. Environ. Health. 95, 753–764 (2022).
Funding
This work was supported by National Healthcare Group Pte Ltd in the form of salaries for all authors. The funder had no role in/influence on study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
L.G. conceived and designed the study, analysed and interpreted the data, drafted the first version of the article and revised it. M.J.P. conceived the study, interpreted the data, and revised the article. C.W.Y. interpreted the data and revised the article. B.H.H. obtained the internal funding support, interpreted the data, and revised the article. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ge, L., Pereira, M.J., Yap, C.W. et al. Chronic low back pain and its impact on physical function, mental health, and health-related quality of life: a cross-sectional study in Singapore. Sci Rep 12, 20040 (2022). https://doi.org/10.1038/s41598-022-24703-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-24703-7
This article is cited by
-
Cross-cultural adaptation and psychometric properties of the Thai version of the patient-reported outcomes measurement information system short form– depression 8a in individuals with chronic low back pain
Journal of Patient-Reported Outcomes (2024)
-
Investigation of factors influencing low physical activity levels in community-dwelling older adults with chronic pain: a cross-sectional study
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.