Abstract
The aim of this study was to investigate the prevalence, correlation, and differences of C-shaped root canals (CSRCs) morphology in permanent mandibular premolars and molars in Eastern Chinese individuals using cone-beam computed tomography (CBCT). A total of 8000 mandibular first premolars (MFPs), mandibular second premolars (MSPs), mandibular first molars (MFMs), and mandibular second molars (MSMs) CBCT images from 1000 patients (692 females and 308 males) were collected. The prevalence, correlation, bilateral/unilateral presence, the morphology of CSRCs, level of canal bifurcation, gender differences, and location of radicular grooves (RGs) were evaluated. The prevalence of CSRCs in MFPs, MSPs, MFMs and MSMs were 10.25%, 0.25%, 0.55% and 47.05%, respectively. The prevalence of CSRCs in MFPs of males was higher than that in females, while the prevalence of CSRCs in MSMs of females was higher than that in males (P < 0.05). The bilateral symmetry presence of CSRCs in MSMs was significant but not in MFPs, MSPs, and MFMs. RGs were predominantly found on the mesiolingual (ML) surface of premolars and the lingual surface of molars. There was a high prevalence of CSRCs in MFPs and MSMs in the Eastern Chinese population, but there was no correlation. The prevalence of CSRCs in MFPs and MSMs differ significantly by gender (P < 0.05).
Similar content being viewed by others
Introduction
Successful root canal treatment requires adequate debridement, shaping, and complement obturation of all root canals in three dimensions (3D), so a thorough knowledge of the anatomy and morphology of the root canals is necessary1. There are numerous types of research on root canal morphology, which mainly focus on: root canal morphology in different teeth from different regions and populations2,3,4, and case reports of unique root canal morphology5,6,7. There are currently recognized variances in root canal morphology based on tooth position, race, and gender2,4,8,9,10,11.
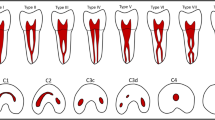
The discovery of C-shaped roots dates back a century and the specific terminology: C-shaped root canals (CSRCs) was first proposed by Cooke and Cox in 1979 when depicting this anatomy in mandibular second molars12. Then CSRCs were also identified in mandibular premolars1 and maxillary molars13. The inability of Hertwig's epithelial root sheath to fuse on the lingual or buccal root surface and the cementum deposition over time may be the leading causes of CSRCs14. A fin or web connecting the individual root canals is the primary anatomical feature of CSRCs15, and thorough debridement of these anatomical structures is a big challenge16,17. In1991, Melton et al. were the first to put forward principles of the CSRCs in molars18, and a modified classification based on Melton’s principle was proposed by Fan et al. in 2004, which classified CSRCs into five categories, described the differences between them, and made up for the shortcomings of the initial categorization15. The 3D morphology of the CSRCs system was divided into three types: (a) Merging type, (b) symmetrical type, and (c) asymmetrical type19.
Many approaches were employed to examine human teeth' internal and exterior structure, such as radiography techniques20, cleaning techniques21, micro-CT in vitro22, and cone-beam computed tomography (CBCT) in vivo1. Micro CT produces better image details compared with CBCT23. It used extracted teeth as samples for in vitro research, but it is not easy to collect many extracted teeth to match the experiment's requirements, which makes it difficult to understand the relationship of CSRCs with other factors such as sex, location (left or right side), and bilaterality1. Furthermore, the reasons why teeth are extracted including complex internal morphologies more difficult to treat or periodontal problems that might be related to the presence of radicular grooves (RGs) caused a misunderstanding of the true prevalence of CSRCs1,24. Over the last three decades, the use of CBCT in endodontics has gradually increased and confirmed the values of CBCT on diagnosis, treatment planning, and decision-making25,26,27. CBCT provides a non-invasive 3D confirmatory diagnosis to complement conventional radiography25. For endodontists, CBCT is critical in the event of a treatment-related mishap, such as perforation of pulp bottom, root canal perforation, or instrument separation28.
The CSRCs in mandibular second molars (MSMs) have been extensively studied in the past. The prevalence of CSRCs in MSMs is much higher in the Asian population than in other races16,29,30. Although there are many reports on the prevalence of CSRCs in the Chinese population, large-sample research on the prevalence of CSRCs in mandibular premolars is scarce1,29. Furthermore, the prevalence of CSRCs in mandibular first premolars (MFPs) was high in the Chinese population22,31,32, while there has been no published research on the relationship between MFPs and MSMs in the Chinese population. There was just one study investigating the relationship between the prevalence of complicated root canals in the mandibular posterior teeth in the Chinese population32, which revealed that the prevalence of CSRCs in MFPs will increase when the distolingual root is found in permanent mandibular first molars (MFMs) in the Chinese-Taiwanese population.
The purpose of this study is to investigate the prevalence, correlation, and differences of CSRCs morphology in permanent mandibular premolars and molars in Eastern Chinese individuals utilizing CBCT.
Methods and materials
Image acquisition
CBCT images with MFPs, mandibular second premolars (MSPs), MFMs, and MSMs with completely developed roots were collected. The presence of unclear images, posts or crowns, periapical lesions, and endodontic treatments were excluded. A total of 8000 mandibular premolars and molars CBCT images from 1000 patients (692 females and 308 males) were collected (Table 1). These 1000 patients are all of Han nationality.
All images were obtained from a CBCT database from the Department of Oral & Maxillofacial Imaging, the Affiliated Stomatological Hospital of Nanjing Medical University. Images were gathered from the patients who required CBCT imaging as part of their dental evaluation for orthodontics, implants, trauma, temporomandibular joint diseases, and other reasons between January and October 2021. The Ethical Committee Department of the Affiliated Stomatological Hospital of Nanjing Medical University approval (PJ2021-116-001) was obtained, and as recommended by the Research and Ethics Committee, formal consent is not required.
The CBCT images were obtained using a CBCT scanner (NewTom 5G, QR s.r.l., Italy) at 110 kV and 4–14 mA with an exposure time of 3–5 s and FOV (Field of view) of 16 × 18 cm or 15 × 12 cm. The voxel size of the images and axial thickness was 0.30 mm. According to the manufacturer's recommended protocol, an experienced radiologist performed the acquisition process.
Image evaluation
Two endodontists independently evaluated the images twice using NNT 10.0.0 software (QR s.r.l., Verona, Italy). A radiologist with experience in endodontics was invited to perform a third evaluation and reach a final consensus when existing disagreements. Their measurements were calibrated before the experiment by reading 20 CBCT images of CSRCs in premolars and molars chosen to ensure the accuracy of the results. Cohen's kappa statistical analysis was used to assess the intra- examiner and inter-examiner reliability.
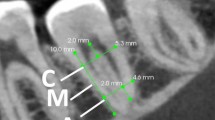
The cross-sectional configurations were analyzed to determine the frequency of CSRCs at different axial levels in premolars and molars: “A,” the coronal-third point (1/3 the distance between the orifice and the anatomical apex), “B,” the middle of the roots (mid-point from orifice to apex distance-wise); “C,” the apical-third point (junction between the middle and apical thirds of the root distance-wise); “D,” 2 mm from the anatomical apex. The mandibular molars were defined as CSRCs when exhibiting all the characteristics: fused roots, a longitudinal groove on the root’s lingual or buccal surface, and at least one cross-section of the canal belonging to the C1, C2, or C3 configuration according to Fan’s classification15:
-
C1: the shape was a continuous “C” with no separation or division.
-
C2: the canal shape resembled a semicolon resulting from a discontinuation in the “C” outline.
-
C3: two separate round, oval, or flat canals.
-
C4: only one round or oval canal in that cross-section.
-
C5: no canal lumen could be observed.
All mandibular premolars were defined as CSRCs when exhibiting all the characteristics: fused roots, a radicular groove on the root’s surface, and at least one cross-section of the canal belonging to the C1 or C2 configuration33.
Age, gender, tooth position (left or right side), morphology of CSRCs, Vertucci root canal classification of premolars presenting CSRCs34 (Fig. 1), and location of RGs were recorded.
Classification of root canal configuration. Type I; a single canal extends from the pulp chamber to the apex. Type II; two separate canals leave the pulp chamber and join short of the apex to form one canal. Type III; one canal leaves the pulp chamber, divides into two within the root, and then merges to exit as one canal. Type IV; two separate and distinct canals extend from the pulp chamber to the apex. Type V; one canal leaves the pulp chamber and divides short of the apex into two separate and distinct canals with separate apical foramina. Type VI; two separate canals leave the pulp chamber, merge in the body of the root, and re-divide short of the apex to exit as two distinct canals. Type VII; one canal leaves the pulp chamber, divides and then rejoins within the body of the root, and finally re-divides into two distinct canals short of the apex. Type VIII; three separate and distinct canals extend from the pulp chamber to the apex.
Statistical analysis
The prevalence of CSRCs was expressed with a 95% confidence interval (CI). The Chi-square test and Fisher’s exact test were used to analyze the correlation between the prevalence of CSRCs and RGs in different tooth positions, age groups, and sex difference by SPSS 25.0 software (SPSS Inc, Chicago, IL, USA). Differences were statistically significant when P was < 0.05.
Results
CBCT evaluations revealed no intra-observer variance for either of the observers (P > 0.05). Intra-examiner and inter-examiner agreements had kappa values of 0.875 to 0.902, respectively.
Mandibular first premolars
The prevalence of CSRCs in the MFPs was 10.25% (205/2000; 95% CI 8.9–11.6%), of which were 16.23% (100/616; 95%CI 13.3–19.2%) in males and 7.59% (105/1384; 95%CI 6.2–9.0%) in females. The prevalence of RGs in the MFPs was 21.10% (422/2000; 95%CI 19.3–22.9%), of which were 26.95% (166/616; 95%CI 23.4–30.5%) in males and 18.50% (256/1384; 95%CI 16.4–20.5%) in females. The prevalence of CSRCs and RGs in males was higher than in females (P < 0.05). There was no statistical difference in the prevalence of CSRCs and RGs in different tooth positions (Table 2).
RGs were mainly located on the mesiolingual (ML) surface of the root, and there was no significant difference in the prevalence of CSRCs in different types of RGs (P > 0.05). Root canal bifurcations were primarily located in the middle third, and the prevalence of CSRCs was significantly lower in the non-bifurcation group than that in the other group (P < 0.05) (Table 3). The canal shape in CSRCs could vary along the length of the root. C4 (77.07%, 158/205) prevailed on the axial of A. C3 (52.20%, 107/205) dominated the axial of B. C2 (54.63%, 112/205) played the most crucial role on the axis of C, followed by C3 (25.37%, 52/205). C3 (60.00%, 123/205) dominated the axial of D. Detailed morphology of different axials in CSRCs was presented in (Table 4).
According to Vertucci classification, Type V (72.68%, 149/205) was the primary morphology of MFPs presenting CSRCs, followed by type III (15.61%, 32/205), type I (10.24%, 21/205), and type VII (0.49%, 1/205). The bilateral symmetry presence of CSRCs was not significant in MFPs (Fig. 2a; Table 5). The prevalence of CSRCs in the contralateral tooth increased when presented on one side. The Chi-square test revealed inter-group disparities in the prevalence of CSRCs across age groups (Table 6).
Mandibular second premolars
The prevalence of CSRCs in the MSPs was 0.25% (5/2000; 95%CI 0–0.5%), of which were 0.49% (3/616; 95%CI 0.1–1%) in males and 0.14% (2/1384; 95%CI 0.1–0.3%) in females. The prevalence of RGs in the MSPs was 0.40% (8/2000; 95%CI 0.1–0.7%), of which were 0.65% (4/616; 95%CI 0–1.3%) in males and 0.29% (4/1384; 95%CI 0–0.6%) in females (Table 2). There was no statistical difference between males and females in the prevalence of CSRCs and RGs in MSPs (P > 0.05). There was no statistical difference in the prevalence of CSRCs and RGs in different positions (P > 0.05).
RGs were mainly located on the lingual surface of the root, and there was no significant difference in the prevalence of CSRCs in different types of RGs (P > 0.05). Root canal bifurcations were primarily located in the middle third, and there was no difference in the prevalence of CSRCs in different canal bifurcations (Table 3). Detailed morphology of different axials in CSRCs was presented in (Table 4). According to Vertucci’s criteria, type I (40%, 2/5) and type III (40%, 2/5) were the primary morphologies in MSPs presenting CSRCs, followed by type V (20%, 1/5). Regarding the symmetry presence of CSRCs and RGs in MSPs, no one presented this condition in any teeth (Table 5). The Chi-square test revealed no difference in the prevalence of CSRCs across age groups (Table 6).
Several examples of root canal system configurations and different CSRCs and RGs in mandibular premolars were shown in Figs. 3 and 4.
Mandibular first molars
The prevalence of CSRCs in the MFMs was 0.55% (11/2000; 95%CI 0.2–0.9%), of which were 0.32% (2/616; 95%CI 0.1–0.8%) in males and 0.65% (9/1384; 95%CI 0.2–1.1%) in females (Table 2). There was no difference in the prevalence of CSRCs in gender and dental position (P > 0.05).
RGs were mainly located on the root’s lingual surface (54.55%, 6/11), followed by buccolingual (45.45%, 5/11). A detailed analysis of different axials in CSRCs was presented in (Table 4). Regarding the symmetry presence (Table 5), CSRCs in MFMs occurred bilaterally in 0.20% (2/1000) of patients (Fig. 2b), unilaterally in 0.70% (7/1000), or on neither side in 99.10% (991/1000). The bilateral symmetry presence of CSRCs was not significant in MFMs (P > 0.05). The Chi-square test revealed no difference in prevalence across age groups (P > 0.05) (Table 6).
Mandibular second molars
Of 2000 MSMs evaluated, 941(47.05%;95%CI 44.9–49.2%) were classified as CSRCs, with 732 in females (52.89%; 95%CI 50.3–55.5%) and 209 in males (33.92%; 95%CI 30.2–37.7%) (Table 2). The Chi-square test showed a higher chance of CSRCs occurring in females than males (P < 0.05). There was no difference in the prevalence of CSRCs in dental positions (P > 0.05).
Most of the grooves were located on the lingual surface (64.72%, 609/941) of the root, followed by the buccolingual (35.07%, 330/941) and the buccal (0.21%, 2/941). C1 (55.04%, 518/941) and C2 (35.92%, 338/941) prevailed on the axial of A. C2 (53.24%, 501/941) dominated the axial of B. C2 (42.72%, 402/941) and C1 (28.06%, 264/941) played the most critical roles on the axis of C, followed by C3 (18.92%, 178/941).C4 (50.90%, 479/941) dominated the axial of D (Table 4).
Regarding symmetry (Table 5), CSRCs in MSMs occurred bilaterally in 38.9% (389/1000) of patients, unilaterally in 16.3% (163/1000), or on neither side in 44.80% (448/1000). In patients presenting CSRCs, 70.47% (389/552) had a bilateral condition (Fig. 2a), and 29.52% (163/552) had a unilateral condition. The bilateral symmetry presence of CSRCs in MSMs was significant. The Chi-square test revealed no inter-group disparities in the prevalence of CSRCs across age groups (P > 0.05) (Table 6).
Different CSRCs and RGs in mandibular molars were presented in (Fig. 5).
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethical Committee Department of the Affiliated Stomatological Hospital of Nanjing Medical University (PJ2021-116-001). Through this approval, the research team had the required administrative permissions to access the data used in this research. For this type of retrospective study, and as recommended by the Research and Ethics Committee, formal consent is not required.
Discussion
The prevalence of CSRCs in mandibular posterior teeth varies between countries and teeth, 1%21 to 28.94%35 in MFPs, 0%36 to 7.14%35 in MSPs, 0%37,38,39,40,41 to 24.01%42 in MFMs, and 1.9%43 to 48.7%41 in MSMs. Surprisingly, there was also a large variation in the prevalence of CSRCs in the same tooth position within the same country, such as Brazil42,44,45, Thailand46,47, and China22,31,32,48,49,50. Both China and Brazil are multi-ethnic countries, which may be one reason for the different prevalence rates, in addition to differences in sample size, methods, and definition of CSRCs. Disagreement over the definition of CSRCs exists mainly among premolars, one study adopted C1 as standard36, some studies considered C1 and C2 as standard1,33,46,51, and others included C3 or C431,35,47,49,52,53.
The optimal sample size means that there are enough patients included in the study to find a statistically significant or clinically worthwhile effect if there is one. More patients than necessary are not recommended to save research time and money54. A study examining the prevalence of CSRCs in MSMs from different regions of the world used a sample size of 400 teeth per region, which was chosen because the final proportion of a pilot study stabilized at 400, and did not change significantly as the measure increased16. When using CBCT images to study the prevalence of anatomical structures, fewer than half of the studies selected the correct sample size, and the JBI assessment methodology was recommended to determine sample size55.
In this study, the prevalence of CSRCs in MFPs of males was higher than that in females (P < 0.05). This study was the first to find gender differences in the prevalence of CSRCs in Chinese MFPs. This finding was consistent with other studies1,46 but contradicted other studies30,35,47. Two studies46,47 investigating the Thai population reached different conclusions on whether there is a gender difference in the occurrence of CSRCs in premolars. The main reason for this difference may be the definition of CSRCs, except sample size. CSRCs in MSMs were more common in women, consistent with other recent studies worldwide16,42,45,56,57,58,59. There are also reports that there is no gender difference in the prevalence of CSRCs60,61,62. The main reason may be racial differences and sample size. No significant differences were found in gender concerning the presence of CSRCs in MSPs and MFMs in this research. Only one study42 has reported a significantly higher prevalence of CSRCs in women than men in first molars. The main reason for this difference may be racial differences.
We did not find an effect of the left or right side on the prevalence of CSRCs in MFPs, MSPs, MFMs, and MSMs, which was consistent with the conclusions of other studies1,57,58,59,61,62. We found no studies reporting significant differences between different tooth positions. In this study, the bilateral symmetry presence of CSRCs was not significant in MFPs, MSPs, and MFMs, while patients with bilateral presence of the CSRCs in MSMs were more common. This result was consistent with some studies1,16,42,47,51,52,57,58,62 but contradicted other studies32,47,53,56,61. We did not find patients with bilateral CSRCs in MSPs. So far, only one study claimed that C-shaped root canal symmetry was significant in MFMs42. In the other two studies56,61, only one patient presented CSRCs in MFMs, leading to an underestimation of whether symmetry occurred. The main reason for these differences may be the low prevalence of CSRCs, different methods adopted, sample size, the definition of CSRCs, and ethnic differences.
RGs in MFPs and MSPs were mainly located on the ML surface of the root. This finding was consistent with earlier studies1,22,30,35,46,51,52,53,63. Most of the RGs in MFMs and MSMs were located on the lingual surface of the root. This finding was consistent with some studies30,57,61,62. Root canal bifurcations in MFPs and MSPs were mainly located in the middle of the root, consistent with other studies46,47,51.
In this research, type V was the main configuration in MFPs presenting CSRCs, which was consistent with other studies1,32,33,47,51. Type III (40%, 2/5) and type I (40%, 2/5) were the primary morphologies of MSPs presenting CSRCs. Since the prevalence of CSRCs in MSPs was very low, this result is not very informative.
The most common root canal configuration in MFPs presenting CSRCs was C3. This result was consistent with Wu et al.32 and Fan et al.22 but contradicted Martins et al.1. The main reason for this difference was the diverse axials selected, apart from race and sample size disparities. C1 was mainly found in the middle of the root, and this result was consistent with Fan et al.22 and Martins et al.1. C4 was mainly located in the coronal third, and C5 was found primarily in the apical third, like the findings in other studies1,22. In this research, C1 was the primary canal morphology at the coronal third in MSMs showing CSRCs, consistent with Kim et al.58 and Vaz de Azevedo et al.42. C1, C2, and C3 prevailed in the middle third. C2 and C4 were the main configurations in the apical third. This finding was also consistent with Alfawaz et al.56 but contradicted Kim et al.58. Ethnic differences may be a prominent cause. Morphological analysis of large samples of MSPs and MFMs is still lacking.
The Chi-square test revealed inter-group disparities in the prevalence of CSRCs in MFPs across age groups. So far, few reports about the prevalence of CSRCs in MFPs showed significant differences between age groups. Only one study reported that the higher prevalence of CSRCs in molars was found among the 45–54 years group with 11.1%, while the lowest rate was found in the 65–74 years group with a prevalence of 5.3%59. There are two reasons to explain the disparities. Firstly, there was a significant difference in the proportion of gender among age groups. Secondly, the prevalence of CSRCs in males of first premolars is significantly higher than that in females.
In this study, the correlations between the prevalence of the CSRCs in mandibular premolars and molars were investigated. The results showed that the prevalence of CSRCs in MFPs was significantly higher than that of MSPs (P < 0.05), and the prevalence of CSRCs in MSMs was considerably higher than that of MFMs (P < 0.05). There was no relationship between CSRCs in MFPs and MSMs, consistent with MH Mashyakhy’s research30, suggesting to clinicians that the occurrence of CSRCs in MSMs does not imply an increased chance of CSRCs occurring in the ipsilateral MFPs. In this study, no patient had a C‑shaped system in MFPs, MSPs, MFMs, and MSMs simultaneously.
One limitation of our work was that it was a retrospective study. We cannot control for characteristics such as FOV and voxel size. A voxel size of 0.250 mm or 0.200 mm was effective in recognizing C-shaped morphologies in earlier research1,16,30,36,41,42,45,47,56,59, and 0.3 mm voxel has only been used in few studies43,64. CBCT must be justified, like any other radiographic examination, and the potential benefits must balance the risk of ionizing radiation exposure25. Each examination should be tailored to the specific patient and their diagnostic requirements26. The principle of ALARA (as low as reasonably achievable) must be followed. Most CBCT images investigated in this study came from CBCT images taken for temporomandibular joint disease diagnosis and standard pre-orthodontic examinations. The 0.3 mm voxel can meet the needs of orthodontic and temporomandibular joint surgeons.
This study was the first to investigate the relationship and differences between CSRCs in different mandibular tooth positions in the Eastern Chinese population and find gender differences in the prevalence of CSRCs in Chinese MFPs. Large-sample research on the prevalence of CSRCs in mandibular premolars is scarce, this research provided the prevalence of CSRCs in MFPs in the Eastern Chinese population with large sample size. Interestingly, we found no significant difference in the prevalence of CSRCs in different types of RGs, and the prevalence of CSRCs was significantly lower in the non-bifurcation group. There have been no relevant studies reported so far. According to previous assumptions, cementum deposition may lead to C-shaped roots14. Compare the CBCT images of the same patient in young and old age stages to confirm the validity of this hypothesis, which will be an exciting direction for future research, and whether there is family inheritance in the occurrence of CSRCs deserves to investigate. CSRCs in the maxillary second molar were not unusual65. Whether there is a connection between the upper and lower jaws for the occurrence of C-shaped root canals in the dentition may be a direction for future research.
Conclusions
There was a high prevalence of CSRCs in MFPs and MSMs in the Eastern Chinese population, but there was no correlation. The prevalence of CSRCs in MFPs and MSMs differ significantly by gender (P < 0.05). The bilateral symmetry presence of CSRCs in MSMs was significant but not in MFPs, MSPs, and MFMs. Root canal bifurcations of premolars presenting CSRCs were primarily located in the middle third. The prevalence of CSRCs in the contralateral tooth increased when presented on one side. Clinicians should pay attention to this phenomenon. In the process of root canal treatment of teeth with CSRCs, CBCT should be taken if necessary, and the treatment should be carried out with the aid of a microscope.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CSRCs:
-
C-shaped root canals
- RGs:
-
Radicular grooves
- CBCT:
-
Cone beam computed tomography
- MFPs:
-
Mandibular first premolars
- MSPs:
-
Mandibular second premolars
- MFMs:
-
Mandibular first molars
- MSMs:
-
Mandibular second molars
- 3D:
-
Three dimension
- SPSS:
-
Statistical Package for the Social Sciences
- FOV:
-
Field of view
- CI:
-
Confidence interval
- ML:
-
Mesiolingual
References
Martins, J. N. R., Francisco, H. & Ordinola-Zapata, R. Prevalence of C-shaped configurations in the mandibular first and second premolars: A cone-beam computed tomographic in vivo study. J. Endod. 43, 890–895. https://doi.org/10.1016/j.joen.2017.01.008 (2017).
Martins, J. N. R., Gu, Y., Marques, D., Francisco, H. & Carames, J. Differences on the root and root canal morphologies between Asian and white ethnic groups analyzed by cone-beam computed tomography. J. Endod. 44, 1096–1104. https://doi.org/10.1016/j.joen.2018.04.001 (2018).
Wolf, T. G. et al. 3-Dimensional analysis and literature review of the root canal morphology and physiological foramen geometry of 125 mandibular incisors by means of micro-computed tomography in a German population. J. Endod. 46, 184–191. https://doi.org/10.1016/j.joen.2019.11.006 (2020).
Martins, J. N. R. et al. Worldwide prevalence of a lingual canal in mandibular premolars: A multicenter cross-sectional study with meta-analysis. J. Endod. 47, 1253–1264. https://doi.org/10.1016/j.joen.2021.04.021 (2021).
Agrawal, P. K., Wankhade, J. & Warhadpande, M. A rare case of type III dens invaginatus in a mandibular second premolar and its nonsurgical endodontic management by using cone-beam computed tomography: A case report. J. Endod. 42, 669–672. https://doi.org/10.1016/j.joen.2016.01.001 (2016).
Ring, J. & Ring, K. C. Rare root canal configuration of mandibular second premolar using cone-beam computed tomographic scanning. J. Endod. 43, 1897–1900. https://doi.org/10.1016/j.joen.2017.04.023 (2017).
Zhang, M., Xie, J., Wang, Y. H. & Feng, Y. Mandibular first premolar with five root canals: A case report. BMC Oral Health 20, 253. https://doi.org/10.1186/s12903-020-01241-0 (2020).
Wolf, T. G., Anderegg, A. L., Wierichs, R. J. & Campus, G. Root canal morphology of the mandibular second premolar: A systematic review and meta-analysis. BMC Oral Health 21, 309. https://doi.org/10.1186/s12903-021-01668-z (2021).
Kottoor, J., Albuquerque, D., Velmurugan, N. & Kuruvilla, J. Root anatomy and root canal configuration of human permanent mandibular premolars: A systematic review. Anat. Res. Int. 2013, 254250. https://doi.org/10.1155/2013/254250 (2013).
Ahmed, H. M. & Hashem, A. A. Accessory roots and root canals in human anterior teeth: A review and clinical considerations. Int. Endod. J. 49, 724–736. https://doi.org/10.1111/iej.12508 (2016).
Wolf, T. G. et al. 3-Dimensional analysis and systematic review of root canal morphology and physiological foramen geometry of 109 mandibular first premolars by micro-computed tomography in a mixed Swiss-German population. J. Endod. 46, 801–809. https://doi.org/10.1016/j.joen.2020.03.002 (2020).
Kato, A. et al. Aetiology, incidence and morphology of the C-shaped root canal system and its impact on clinical endodontics. Int. Endod. J. 47, 1012–1033. https://doi.org/10.1111/iej.12256 (2014).
Martins, J. N., Mata, A., Marques, D., Anderson, C. & Carames, J. Prevalence and characteristics of the maxillary C-shaped molar. J. Endod. 42, 383–389. https://doi.org/10.1016/j.joen.2015.12.013 (2016).
Manning, S. A. Root canal anatomy of mandibular second molars. Part II. C-shaped canals. Int. Endod. J. 23, 40–45. https://doi.org/10.1111/j.1365-2591.1990.tb00801.x (1990).
Fan, B., Cheung, G. S., Fan, M., Gutmann, J. L. & Bian, Z. C-shaped canal system in mandibular second molars: Part I-Anatomical features. J. Endod. 30, 899–903. https://doi.org/10.1097/01.don.0000136207.12204.e4 (2004).
von Zuben, M. et al. Worldwide prevalence of mandibular second molar C-shaped morphologies evaluated by cone-beam computed tomography. J. Endod. 43, 1442–1447. https://doi.org/10.1016/j.joen.2017.04.016 (2017).
Pereira, B. et al. Association between endodontically treated maxillary and mandibular molars with fused roots and periapical lesions: A cone-beam computed tomography cross-sectional study. J. Endod. 46, 771–777.e771. https://doi.org/10.1016/j.joen.2020.03.003 (2020).
Melton, D. C., Krell, K. V. & Fuller, M. W. Anatomical and histological features of C-shaped canals in mandibular second molars. J. Endod. 17, 384–388. https://doi.org/10.1016/s0099-2399(06)81990-4 (1991).
Gao, Y., Fan, B., Cheung, G. S., Gutmann, J. L. & Fan, M. C-shaped canal system in mandibular second molars part IV: 3-D morphological analysis and transverse measurement. J. Endod. 32, 1062–1065. https://doi.org/10.1016/j.joen.2006.05.014 (2006).
Lambrianidis, T., Lyroudia, K., Pandelidou, O. & Nicolaou, A. Evaluation of periapical radiographs in the recognition of C-shaped mandibular second molars. Int. Endod. J. 34, 458–462. https://doi.org/10.1046/j.1365-2591.2001.00417.x (2001).
Velmurugan, N. & Sandhya, R. Root canal morphology of mandibular first premolars in an Indian population: A laboratory study. Int. Endod. J. 42, 54–58. https://doi.org/10.1111/j.1365-2591.2008.01494.x (2009).
Fan, B., Yang, J., Gutmann, J. L. & Fan, M. Root canal systems in mandibular first premolars with C-shaped root configurations. Part I: Microcomputed tomography mapping of the radicular groove and associated root canal cross-sections. J. Endod. 34, 1337–1341. https://doi.org/10.1016/j.joen.2008.08.006 (2008).
Zhang, D. et al. The root canal morphology in mandibular first premolars: A comparative evaluation of cone-beam computed tomography and micro-computed tomography. Clin. Oral Investig. 21, 1007–1012. https://doi.org/10.1007/s00784-016-1852-x (2017).
Garrido, I., Abella, F., Ordinola-Zapata, R., Duran-Sindreu, F. & Roig, M. Combined endodontic therapy and intentional replantation for the treatment of palatogingival groove. J. Endod. 42, 324–328. https://doi.org/10.1016/j.joen.2015.10.009 (2016).
Patel, S. et al. Cone beam computed tomography in endodontics—A review. Int. Endod. J. 48, 3–15. https://doi.org/10.1111/iej.12270 (2015).
Patel, S. et al. Cone beam computed tomography in endodontics—A review of the literature. Int. Endod. J. 52, 1138–1152. https://doi.org/10.1111/iej.13115 (2019).
Luz, L. B. et al. The impact of cone-beam computed tomography on diagnostic thinking, treatment option, and confidence in dental trauma cases: A before and after study. J. Endod. 48, 320–328. https://doi.org/10.1016/j.joen.2021.12.011 (2022).
AAE and AAOMR Joint Position Statement. Use of cone beam computed tomography in endodontics 2015 update. J. Endod. 41, 1393–1396. https://doi.org/10.1016/j.joen.2015.07.013 (2015).
Martins, J. N. R. et al. Prevalence of C-shaped canal morphology using cone beam computed tomography—a systematic review with meta-analysis. Int. Endod. J. 52, 1556–1572. https://doi.org/10.1111/iej.13169 (2019).
Mashyakhy, M. H. et al. C-shaped canal configuration in mandibular premolars and molars: Prevalence, correlation, and differences: An in vivo study using cone-beam computed tomography. Niger. J. Clin. Pract. 23, 232–239. https://doi.org/10.4103/njcp.njcp_335_19 (2020).
Lu, T. Y., Yang, S. F. & Pai, S. F. Complicated root canal morphology of mandibular first premolar in a Chinese population using the cross section method. J. Endod. 32, 932–936. https://doi.org/10.1016/j.joen.2006.04.008 (2006).
Wu, Y. C. et al. Relationship of the incidence of c-shaped root canal configurations of mandibular first premolars with distolingual roots in mandibular first molars in a Taiwanese population: A cone-beam computed tomographic study. J. Endod. 44, 1492–1499.e1491. https://doi.org/10.1016/j.joen.2018.05.016 (2018).
Fan, B., Ye, W., Xie, E., Wu, H. & Gutmann, J. L. Three-dimensional morphological analysis of C-shaped canals in mandibular first premolars in a Chinese population. Int. Endod. J. 45, 1035–1041. https://doi.org/10.1111/j.1365-2591.2012.02070.x (2012).
Vertucci, F. J. Root canal anatomy of the human permanent teeth. Oral Surg. Oral Med. Oral Pathol. https://doi.org/10.1016/0030-4220(84)90085-9 (1984).
Brea, G., Gomez, F. & Gomez-Sosa, J. F. Cone-beam computed tomography evaluation of C-shaped root and canal morphology of mandibular premolars. BMC Oral Health 21, 236. https://doi.org/10.1186/s12903-021-01596-y (2021).
Pedemonte, E. et al. Root and canal morphology of mandibular premolars using cone-beam computed tomography in a Chilean and Belgian subpopulation: A cross-sectional study. Oral Radiol. 34, 143–150. https://doi.org/10.1007/s11282-017-0297-5 (2018).
Peiris, R., Takahashi, M., Sasaki, K. & Kanazawa, E. Root and canal morphology of permanent mandibular molars in a Sri Lankan population. Odontology 95, 16–23. https://doi.org/10.1007/s10266-007-0074-8 (2007).
Ahmed, H. A., Abu-bakr, N. H., Yahia, N. A. & Ibrahim, Y. E. Root and canal morphology of permanent mandibular molars in a Sudanese population. Int. Endod. J. 40, 766–771. https://doi.org/10.1111/j.1365-2591.2007.01283.x (2007).
Al-Qudah, A. A. & Awawdeh, L. A. Root and canal morphology of mandibular first and second molar teeth in a Jordanian population. Int. Endod. J. 42, 775–784. https://doi.org/10.1111/j.1365-2591.2009.01578.x (2009).
Zhang, R. et al. Use of cone-beam computed tomography to evaluate root and canal morphology of mandibular molars in Chinese individuals. Int. Endod. J. 44, 990–999. https://doi.org/10.1111/j.1365-2591.2011.01904.x (2011).
Pan, J. Y. Y. et al. Root canal morphology of permanent teeth in a Malaysian subpopulation using cone-beam computed tomography. BMC Oral Health 19, 14. https://doi.org/10.1186/s12903-019-0710-z (2019).
Vaz de Azevedo, K. R. et al. C-shaped canals in first and second mandibular molars from Brazilian individuals: A prevalence study using cone-beam computed tomography. PLoS ONE 14, e0211948. https://doi.org/10.1371/journal.pone.0211948 (2019).
Celikten, B. et al. Cone beam CT evaluation of mandibular molar root canal morphology in a Turkish Cypriot population. Clin. Oral Investig. 20, 2221–2226. https://doi.org/10.1007/s00784-016-1742-2 (2016).
Silva, E. J., Nejaim, Y., Silva, A. V., Haiter-Neto, F. & Cohenca, N. Evaluation of root canal configuration of mandibular molars in a Brazilian population by using cone-beam computed tomography: an in vivo study. J. Endod. 39, 849–852. https://doi.org/10.1016/j.joen.2013.04.030 (2013).
Nejaim, Y. et al. C-shaped canals in mandibular molars of a Brazilian subpopulation: Prevalence and root canal configuration using cone-beam computed tomography. Clin. Oral Investig. 24, 3299–3305. https://doi.org/10.1007/s00784-020-03207-6 (2020).
Arayasantiparb, R. & Banomyong, D. Prevalence and morphology of multiple roots, root canals and C-shaped canals in mandibular premolars from cone-beam computed tomography images in a Thai population. J. Dent. Sci. 16, 201–207. https://doi.org/10.1016/j.jds.2020.06.010 (2021).
Thanaruengrong, P., Kulvitit, S., Navachinda, M. & Charoenlarp, P. Prevalence of complex root canal morphology in the mandibular first and second premolars in Thai population: CBCT analysis. BMC Oral Health 21, 449. https://doi.org/10.1186/s12903-021-01822-7 (2021).
Yang, H. et al. A cone-beam computed tomography study of the root canal morphology of mandibular first premolars and the location of root canal orifices and apical foramina in a Chinese subpopulation. J. Endod. 39, 435–438. https://doi.org/10.1016/j.joen.2012.11.003 (2013).
Gu, Y., Zhang, Y. & Liao, Z. Root and canal morphology of mandibular first premolars with radicular grooves. Arch. Oral Biol. 58, 1609–1617. https://doi.org/10.1016/j.archoralbio.2013.07.014 (2013).
Yu, X. et al. Cone-beam computed tomography study of root and canal morphology of mandibular premolars in a western Chinese population. BMC Med. Imaging 12, 18. https://doi.org/10.1186/1471-2342-12-18 (2012).
Kaya Buyukbayram, I., Subay, R. K., Colakoglu, G., Elcin, M. A. & OrduluSubay, M. Investigation using cone beam computed tomography analysis, of radicular grooves and canal configurations of mandibular premolars in a Turkish subpopulation. Arch. Oral Biol. 107, 104517. https://doi.org/10.1016/j.archoralbio.2019.104517 (2019).
ChaintiouPiorno, R., ConsoliLizzi, E. P., Gualtieri, A. F. & Rodriguez, P. A. C-Shaped canal system in mandibular premolars evaluated by cone-beam computed tomography in a population of the Autonomous City of Buenos Aires, Argentina. Arch. Oral Biol. 123, 105040. https://doi.org/10.1016/j.archoralbio.2021.105040 (2021).
Chen, Y. C., Tsai, C. L., Chen, Y. C., Chen, G. & Yang, S. F. A cone-beam computed tomography study of C-shaped root canal systems in mandibular second premolars in a Taiwan Chinese subpopulation. J. Formos Med. Assoc. 117, 1086–1092. https://doi.org/10.1016/j.jfma.2017.12.001 (2018).
Verhagen, A. & Yu, L. M. Editorial: What about sample size?. Musculoskelet. Sci. Pract. 54, 102405. https://doi.org/10.1016/j.msksp.2021.102405 (2021).
Martins, J. N. R. et al. Preferred reporting items for epidemiologic cross-sectional studies on root and root canal anatomy using cone-beam computed tomographic technology: A systematized assessment. J. Endod. 46, 915–935. https://doi.org/10.1016/j.joen.2020.03.020 (2020).
Alfawaz, H. et al. Prevalence of C-shaped canal system in mandibular first and second molars in a Saudi population assessed via cone beam computed tomography: A retrospective study. Clin. Oral Investig. 23, 107–112. https://doi.org/10.1007/s00784-018-2415-0 (2019).
Khawaja, S. et al. The C-shaped root canal systems in mandibular second molars in an Emirati population. Sci. Rep. 11, 23863. https://doi.org/10.1038/s41598-021-03329-1 (2021).
Kim, S. Y., Kim, B. S. & Kim, Y. Mandibular second molar root canal morphology and variants in a Korean subpopulation. Int. Endod. J. 49, 136–144. https://doi.org/10.1111/iej.12437 (2016).
Martins, J. N. R., Mata, A., Marques, D. & Carames, J. Prevalence of C-shaped mandibular molars in the Portuguese population evaluated by cone-beam computed tomography. Eur. J. Dent. 10, 529–535. https://doi.org/10.4103/1305-7456.195175 (2016).
Pawar, A. M. et al. Root canal morphology and variations in mandibular second molar teeth of an Indian population: An in vivo cone-beam computed tomography analysis. Clin. Oral Investig. 21, 2801–2809. https://doi.org/10.1007/s00784-017-2082-6 (2017).
Shemesh, A. et al. C-shaped canals-prevalence and root canal configuration by cone beam computed tomography evaluation in first and second mandibular molars-a cross-sectional study. Clin. Oral Investig. 21, 2039–2044. https://doi.org/10.1007/s00784-016-1993-y (2017).
Zheng, Q. et al. C-shaped root canal system in mandibular second molars in a Chinese population evaluated by cone-beam computed tomography. Int. Endod. J. 44, 857–862. https://doi.org/10.1111/j.1365-2591.2011.01896.x (2011).
Chen, J. et al. A micro-computed tomography study of the relationship between radicular grooves and root canal morphology in mandibular first premolars. Clin. Oral Investig. 19, 329–334. https://doi.org/10.1007/s00784-014-1242-1 (2015).
Lee, J. B. & Seo, M. S. Mandibular incisors with two canals are associated with the presence of the distolingual root in mandibular first molars: A cone-beam computed tomographic study. BMC Oral Health 22, 145. https://doi.org/10.1186/s12903-022-02184-4 (2022).
Abdalrahman, K., Talabani, R., Kazzaz, S. & Babarasul, D. Assessment of C-shaped canal morphology in mandibular and maxillary second molars in an Iraqi subpopulation using cone-beam computed tomography. Scanning 2022, 4886993. https://doi.org/10.1155/2022/4886993 (2022).
Acknowledgements
The authors are grateful to the study participants.
Funding
The work was supported by the scientific research project of health care for cadres of Jiangsu Province (BJ21034) and A Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD, 2018-87).
Author information
Authors and Affiliations
Contributions
C.C., conceptualization, data curation, formal analysis, writing—original draft. T.Z., methodology, data curation review and editing. H.W., investigation, validation, visualization, investigation, validation, visualization. X.Z., D.L., J.W. investigation, validation, visualization. L.Y., supervision, review and editing, project administration. D.W., supervision, project administration.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, C., Zhu, T., Wu, H. et al. Prevalence and correlation of C-shaped root canals of mandibular premolars and molars in Eastern Chinese individuals. Sci Rep 12, 19779 (2022). https://doi.org/10.1038/s41598-022-24381-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-24381-5
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.