Abstract
Polycystic ovary syndrome (PCOS) coexisting mood disorders along with a combination of aesthetic manifestations may have a detrimental effect on women's sexual function. Hence, different phenotypes of PCOS have different clinical and biochemical signs and symptoms. The aim of this study was to compare women's sexual function (SF) in different phenotypes of PCOS. This cross-sectional study was conducted on 364 women who met the Rotterdam diagnostic criteria to compare different PCOS phenotypes (A = 95, B = 79, C = 95, and D = 95) and 100 non PCOS women in control group. All participants were invited to fill out the female sexual function index (FSFI). Significant differences were observed between the different phenotypes and control group in terms of the total score, sexual desire, arousal, lubrication, and satisfaction (P < 0.001); however, no significant differences were found between different phenotypes in terms of pain (P > 0.05) and orgasm (P > 0.05) but difference was significant between different phenotypes and control group. In addition, phenotype B had the lowest mean score of total FSFI (P < 0.05). The results indicated that women's SF is significantly different in different PCOS phenotypes. It is concluded that in order to solve the SF problems of women with PCOS, different treatment and care measures should be considered according to the relevant phenotype.
Similar content being viewed by others
Introduction
Polycystic Ovary Syndrome (PCOS) is a heterogeneous disorder that influences 6–10% of reproductive-aged women1. It is associated with a combination of distressing manifestations such as subfertility, irregular menstruation, acne, obesity, alopecia, and hirsutism, which may affect feminine identity, self-esteem, and body image destructively2,3. These aesthetic factors together with sex hormone imbalances (hyperinsulinemia, hyperandrogenism, and increased luteinizing hormone level) can trigger anxiety, depression, and worsened Quality of Life (QoL) in women4,5,6. In addition, these mood disorders and their medications can pose detrimental effects on Sexual Function (SF)7,8.
Four different phenotype categories have been identified for PCOS based on the National Institute of Health (NIH) consensus panel: phenotype A including Hyperandrogenism clinical or biochemical (HA), Ovulatory Dysfunction (OD), and Polycystic Ovary (PCO), Phenotypes B and C: HA + OD, and HA + PCO, respectively, and phenotype D including OD and PCO.
Furthermore, the clinical manifestations as well as metabolic and hormonal profiles are different in these phenotypes9. So, SF can be influenced differently in different phenotypes of PCOS.
Although clinical signs of PCOS can be deleterious for SF, the association of PCOS with SF remains inconsistent. In addition, there are limited studies specifically evaluating SF regarding different PCOS phenotypes. Therefore, the present study was conducted to compare SF of different phenotypes of PCOS and non PCOS women in Iran.
Materials and methods
This cross-sectional study was conducted on a group of PCOS women and a healthy control group who were referred to the gynecological clinics of hospitals in Tehran province (Iran) between May 2018 and February 2019 through the convenience sampling method. The Ethics Committee of Tarbiat Modares University of Medical Sciences approved the study protocol (IR.MODARES.REC. 1397.211).
Firstly, the sample size was calculated using the appropriate formula and considering the 95% confidence interval. Consequently, 364 women with PCOS diagnosis according to the Rotterdam criteria (95 women with phenotype A, 79 women with phenotype B, 95 women with phenotype c, and 95 women with phenotype D and 100 healthy women in control group) were recruited after obtaining written consent. Eligibility criteria required for selecting the subjects were as follows: married women of reproductive age (18–45 years) who lived with a husband and were sexually active (had sexual intercourse in the past four weeks). In addition, PCOS was diagnosed based on the Rotterdam criteria and willing to participate in this study. The possible confounding factors were avoided by the exclusion criteria: pregnancy, breastfeeding, suffering from endocrine and chronic diseases (like diabetes, cardiovascular diseases, kidney disease, benign and malignant tumors, etc.), taking any hormonal and herbal medicines in the last month due to their possible impact on SF and androgen levels. The participants were asked to fill out the questionnaires, which included a series of questions about demographic characteristics and sexual dysfunction.
Phenotypical features
Anthropometric measurements including weight, height, hip circumference (HC), and waist circumference (WC) were measured by the same person for all participants. Body mass index (BMI) was calculated based on dividing weight in kilograms by the square of height in meters for assessing obesity10. Additionally, WC was measured at the narrowest point between the lower rib and iliac crest in the standing position and HC was calculated at the widest part of the buttocks, dividing WC by the HC was considered the Waist to Hip Ratio (WHR)11.
Clinical and para-clinical features
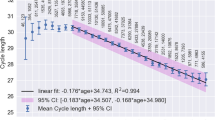
Clinical features such as hirsutism, menstrual cycle status, and acne were assessed by a clinician. Menstrual cycle lengths shorter than 24 days and longer than 34 days were considered abnormal. The modified Ferriman–Gallwey (mFG) was used to identify hirsutism. It consists of observing the quantity and distribution of terminal hair in nine body areas, including the upper lip, chin, chest, upper and lower abdomen, back, sacroiliac region, thighs, and arms. These areas were given a score ranging from 0 to 4 according to quantity and density, with higher scores indicating a greater amount of body hair12. The reliability and validity of this questionnaire have been confirmed in Iran13.
The degree of severity of acne was examined based on the Conference on Acne Classification, which is divided into mild, moderate, and severe. The mild form consists of small comedowns’ number of papules and nodules, with no cysts and scars. Although there is a very large number of papules and posture in the medium form of acne, nodules, cysts, and scars are seen rarely. In the severe form, the number of papules and pustules is very large and the number of nodules, cysts, and scars is also high14.
Polycystic ovary morphology (PCOM) was detected based on the Rotterdam PCOS criteria: An ovarian volume > 10 mL or containing 12 or more follicles (2–9 mm) in size was distinguished as a positive PCOM.
All blood samples which contained LH, FSH, Testosterone, SHBG, TSH, progesterone and prolactin were measured on day-3 of the menstrual cycle by the same laboratory tests (ELISA method). Also, the Free Androgen Index (FAI) value was calculated by dividing the total testosterone (nmol/lit)/SHBG multiplied × 100.
Questionnaire
A socio-demographic questionnaire (including age, marital status, employment status, educational level, BMI, history of chronic disease, menstrual and reproductive history such as duration and length of the menstrual cycle, regularity of cycle, number of children, and abortion) was completed.
Sexual function
To assess SF, all participants were asked to fill out the Female Sexual Function Index (FSFI), which includes 19 questions to measure women's SF in six areas: desire, arousal, moisture, orgasm, satisfaction, and pain. The evaluation was done through the Likert scale. The total score was obtained by summing the six domain scores. A higher score is associated with a lower degree of sexual dysfunction and the total score of 26.55 is the optimal cut score for differentiating women with and without sexual dysfunction15. The reliability and validity of this questionnaire have been confirmed in Iran16.
Statistical method
Statistical analysis was performed by using the SPSS software (Version 16, SPSS Inc, Chicago, IL, USA). The normality of data was assessed using Kolmogorov–Smirnov's test and presented as mean + SD for normal and quantitative data. A one-way ANOVA was used with Bonferroni Post Hoc test to compare normal variables between the groups, and Kruskal–Wallis test was used to compare non-normal variables between different groups. Also, to compare qualitative variables between the different groups, Chi-square test, Fisher's exact test, Fisher's generalized test were used. P values lower than 0.05 were considered statistically significant.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board, and the Ethics Committee of Tarbiat Modares University of Medical Sciences approved the study protocol. All procedures were in accordance with the ethical standards of the Regional Research Committee, as well as the Declaration of Helsinki 1964 and its later amendments. After explaining the study's purposes, informed written consent and verbal assent was obtained from all participants. They were informed that their participation was voluntary, confidential, and anonymous and that they had the right to withdraw from the research at any time.
Results
Among the 492 participants interviewed for this study, 28 women didn’t meet the inclusion criteria (7%) (Fig. 1). Table 1 illustrates some of the basic features of PCOS diagnosis in each group.
Table 2 compares the demographic characteristics of different phenotypes of PCOS and control group. As can be seen, there are no significant differences in the women’s age, BMI, WC, HC, WHR, education level, occupation status, number of children, number of abortions and fertility status between group.
Table 3 presents the summary statistics for the comparison of FSFI characteristics between different groups. As shown, there is a significant difference between the PCOS categories and control group in the mean total score of FSFI, sexual desire, arousal, lubrication, satisfaction, and orgasm (P < 0.05). However, no significant differences were found between these groups in terms of pain (P > 0.05). In addition, there are significant differences between the scores of phenotype B and other categories in all SF sub-groups except orgasm (P < 0.05).
Discussion
In this study, for the first time, SF was compared between different confirmed PCOS phenotypic categories in a representative sample of Iranian women. According to the obtained results, there were significant differences in terms of all FSFI domains except orgasm and pain between different phenotypes of PCOS. It was also found that sexual symptoms’ scores in phenotype B were significantly lower as compared with the other phenotypes. This finding is consistent with Bahadori et al.’s study, they also reported that phenotype B had the lowest mean score in the FSFI and SF-12 questionnaires. Furthermore, a significant difference was observed between the women with PCOS and the control group in terms of arousal, lubrication, pain, and mean total score of FSFI17.
The SF of PCOS women is affected by the interaction of many factors. Firstly, although there is a positive association between androgen levels and enhanced quality of SF, the HA manifestations can adversely affect the patients’ mental health18. Hirsutism, acne, and overweight often manifest when SF and raising a family is very important. These alternations in appearance and aesthetic standards allow PCOS women to report a feeling of unattractiveness and less feminine19, leading to psychosocial implications and decreased sexual self-worth20.Tian et al. reported that women with more severe clinical symptoms of hyperandrogenism had a lower sexual function score21. Secondly, emotional and social discomforts concomitant with long-term health risks can cause impaired SF and psychological well-being19. In addition, PCOS women are at an increased risk for mood disorders, such those 14 to 67% of patients who have been reported to suffer from depressive symptoms22. As a matter of fact, increased incidence of depression could result from frequent rate of infertility23; additionally, complaining of reduced libido has been reported by infertile women and those experiencing recurrent abortion24. In the study by Naumova et al.25 with the aim of comparison of psychological issues and sexual function in women with different infertility Causes, they reported that the prevalence of depression and anxiety was significantly higher in infertile women with PCOS than other infertile group. Hyperandrogenism and overweight was associated with higher incidence of depression and anxiety and the severity of anxiety symptom was associated with the status and response to infertility treatments. Finally, the results of their study showed that women's sexual performance in the areas of orgasm and satisfaction was impaired. Stapinska-Syniec et al.26 outlined, however, that infertility does not have isolated impact on depression in PCOS women.
Many studies have revealed that although having the same frequency of sexual intercourses and fantasies as controls, PCOS women are less satisfied and sexually attractive27. Stovall et al.28 reported that women with PCOS are comparable with the controls in SF scores except orgasm domain. Since HA is considered as a hallmark of PCOS, they evaluated the association of serum testosterone levels and SF. Overall, it is argued that minimum levels of testosterone are associated with the lowest scores of SF; surprisingly, higher testosterone levels are associated with higher desire/frequency rather than desire/interest scores28. Mantzou et al. demonstrated that the adverse effect of PCOS on women's sexual performance is largely dependent on the hormonal changes that caused by it and independent of BMI and ovulation disorders are considered as an important factor in determining the prognosis of PCOS on the sexual performance of affected women29.
In the present study, there is significant difference between control group and groups with different phenotypes of PCOS in terms of desire, arousal, lubrication, orgasm, pain and satisfaction that can confirm the hypothesis of the detrimental effects of PCOS on Sf. In addition, women with phenotype B PCOS had more impaired SF than the other phenotypes. These results can be explained by hormonal differences. In a recent study by the Lizneva et al.30, phenotypes A and B were considered as classic categories possessing more menstrual dysfunction, higher androgen and insulin levels, increased rate of insulin resistance, and being at higher risk of metabolic syndrome and obesity comparing to non-HA phenotypes. In addition, the highest antimüllerian hormone levels were found in the classic PCOS categories.
SF is reportedly more impaired in phenotype B rather than in other groups, possibly due to HA. Although HA has a prominent role in PCOS diagnosis31, the association between levels of androgen and SF remains inconsistent. Previous studies have shown that serum testosterone levels are associated positively with SF6,32; however, Ercan et al.33 demonstrated an inverse relationship. In addition, two large studies showed that there is not any association between SF and the levels of androgen (total and free testosterone and free androgen index34,35. Morotti et al.36found that lean PCOS patients have been considered the same as non-PCOS women in terms of sexual behavior, meaning that moderate hirsutism and HA do not have an important impact on their self-esteem and body image. Contrary to these results, another study in non-PCOS women supports the positive effect of high level of testosterone on the psychological experiences of orgasm in PCOS women37. In addition, these results are in agreement with the findings of Dilbaz et al. who analyzed the health-related QOL scores between infertile women and different PCOS phenotypes. The levels of hirsutism, primary infertility and phenotype HA-AO were correlated with QOL scores38.
Furthermore, irregular menstrual cycle, which characterizes PCOS, can manifest in classic phenotypes more than others30 Although considered as a distress factor that can impair psychological health, menstrual irregulation does not have confirmed effects on SF39.
According to the fact that infertility is considered as one of the main confounders of sexual function that has been omitted in this study to assess the effects of PCOS on SF. Although the main strength of this study includes evident phenotypic classification, it has some limitations such as lack of non-PCOS group to compare the results, and relatively small sample size in each group. Furthermore, the lack of psychological evaluation before recruiting the participants is considered one of the limitations of this study and the result would have been more reliable if we could assess their psychological health.
Conclusion
The results of this study indicated significant differences in terms of SF and its domains in different phenotypes of PCOS. To treat sexual dysfunction in women with PCOS, different treatment and care measures should be considered according to the relevant phenotype. Accordingly, further studies are needed to identify and overcome this difficulty in different populations.
Data availability
The data sets used and analyzed for the current study are available upon reasonable request of the corresponding author Dr. Shahideh Jahanian (shahideh.jahanian@modares.ac.ir).
Abbreviations
- PCOS:
-
Polycystic ovary syndrome
- PCO:
-
Polycystic ovaries
- NIH:
-
National institute of health
- DHEAS:
-
Dehydroepiandrosterone sulfate
- OD:
-
Ovulatory dysfunction
- FAI:
-
Free androgen index
- LH:
-
Luteinizing hormone
- FSFI:
-
Female sexual function index
- FSH:
-
Follicle stimulating hormone
- WC:
-
Waist circumference
- BMI:
-
Body mass index
- WHR:
-
Waist to hip ratio
- HA:
-
Hyperandrogenism
- TT:
-
Total testosterone
- HC:
-
Hip circumference
- MW:
-
Mann–Whitney
- QoL:
-
Quality of life
- FSD:
-
Female sexual dysfunction
- mFG:
-
Modified Ferriman–Gallwey
References
Rodriguez Paris, V. & Bertoldo, M. J. The mechanism of androgen actions in PCOS etiology. Med. Sci. (Basel) 7(9), 89 (2019).
Escobar-Morreale, H. F. Polycystic ovary syndrome: Definition, aetiology, diagnosis and treatment. Nat. Rev. Endocrinol. 14(5), 270–284 (2018).
Noroozzadeh, M., Ramezani Tehrani, F., Bahri Khomami, M. & Azizi, F. A Comparison of sexual function in women with polycystic ovary syndrome (PCOS) whose mothers had PCOS during their pregnancy period with those without PCOS. Arch. Sex Behav. 46(7), 2033–2042 (2017).
Cronin, L. et al. Development of a health-related quality-of-life questionnaire (PCOSQ) for women with polycystic ovary syndrome (PCOS). J. Clin. Endocrinol. Metab. 83(6), 1976–1987 (1998).
Barry, J. A., Kuczmierczyk, A. R. & Hardiman, P. J. Anxiety and depression in polycystic ovary syndrome: A systematic review and meta-analysis. Hum. Reprod. 26(9), 2442–2451 (2011).
Veras, A. B., Bruno, R. V., de Avila, M. A. & Nardi, A. E. Sexual dysfunction in patients with polycystic ovary syndrome: Clinical and hormonal correlations. Compr. Psychiatry 52(5), 486–489 (2011).
Janssen, O. E., Hahn, S., Tan, S., Benson, S. & Elsenbruch, S. Mood and sexual function in polycystic ovary syndrome. Semin. Reprod. Med. 26(1), 45–52 (2008).
Kennedy, S. H., Dickens, S. E., Eisfeld, B. S. & Bagby, R. M. Sexual dysfunction before antidepressant therapy in major depression. J. Affect Disord. 56(2–3), 201–208 (1999).
Sachdeva, G., Gainder, S., Suri, V., Sachdeva, N. & Chopra, S. Comparison of the different PCOS phenotypes based on clinical metabolic, and hormonal profile, and their response to clomiphene. Indian J. Endocrinol. Metab. 23(3), 326–331 (2019).
uddin Ismail, B., Ali, S. F. A., Ayaz, A. A., editors. Microcontroller based automated body mass index (BMI) calculator with LCD display. In 2nd International Conference on Electrical, Electronics and Civil Engineering (ICEECE'2012) Singapore April 2012.
Tolstrup, J. et al. The relation between drinking pattern and body mass index and waist and hip circumference. Int. J. Obes. 29(5), 490–497 (2005).
Hatch, R., Rosenfield, R. L., Kim, M. H. & Tredway, D. Hirsutism: Implications, etiology, and management. Am. J. Obstet. Gynecol. 140(7), 815–830 (1981).
Tehrani, F. R., Minooee, S. & Azizi, F. Validation of a simplified method to assess hirsutism in the Iranian population. Eur. J. Obstet. Gynecol. Reprod. Biol. 174, 91–95 (2014).
Strauss, J. S. et al. Guidelines of care for acne vulgaris management. J. Am. Acad. Dermatol. 56(4), 651–663 (2007).
Wiegel, M., Meston, C. & Rosen, R. The female sexual function index (FSFI): Cross-validation and development of clinical cutoff scores. J. Sex Marital Ther. 31(1), 1–20 (2005).
Fakhri, A., Pakpour, A. H., Burri, A., Morshedi, H. & Zeidi, I. M. The female sexual function index: Translation and validation of an Iranian version. J. Sex. Med. 9(2), 514–523 (2012).
Bahadori, F., Jahanian Sadatmahalleh, S., Montazeri, A. & Nasiri, M. Sexuality and psychological well-being in different polycystic ovary syndrome phenotypes compared with healthy controls: A cross-sectional study. BMC Womens Health 22(1), 390 (2022).
Ferraresi, S. R., da Silva Lara, L. A., Reis, R. M. & de Sá Rosa, A. C. J. Changes in sexual function among women with polycystic ovary syndrome: A pilot study. J. Sex. Med. 10(2), 467–473 (2013).
Farkas, J., Rigó, A. & Demetrovics, Z. Psychological aspects of the polycystic ovary syndrome. Gynecol. Endocrinol. 30(2), 95–99 (2014).
Janssen, O. E., Hahn, S., Tan, S., Benson, S. & Elsenbruch, S. Mood and sexual function in polycystic ovary syndrome. Semin. Reprod. Med. 26, 045–052 (2008).
Tian, X. et al. Sexual function in chinese women with polycystic ovary syndrome and correlation with clinical and biochemical characteristics. Reprod. Sci. 28(11), 3181–3192 (2021).
Kerchner, A., Lester, W., Stuart, S. P. & Dokras, A. Risk of depression and other mental health disorders in women with polycystic ovary syndrome: A longitudinal study. Fertil. Steril. 91(1), 207–212 (2009).
Deeks, A. A., Gibson-Helm, M. E. & Teede, H. J. Anxiety and depression in polycystic ovary syndrome: A comprehensive investigation. Fertil. Steril. 93(7), 2421–2423 (2010).
Podfigurna-Stopa, A. et al. Mood disorders and quality of life in polycystic ovary syndrome. Gynecol. Endocrinol. 31(6), 431–434 (2015).
Naumova, I., Castelo-Branco, C. & Casals, G. Psychological issues and sexual function in women with different infertility Causes: Focus on polycystic ovary syndrome. Reprod. Sci. 28(10), 2830–2838 (2021).
Stapinska-Syniec, A., Grabowska, K., Szpotanska-Sikorska, M. & Pietrzak, B. Depression, sexual satisfaction, and other psychological issues in women with polycystic ovary syndrome. Gynecol. Endocrinol. 34(7), 597–600 (2018).
Hahn, S. et al. Clinical and psychological correlates of quality-of-life in polycystic ovary syndrome. Eur. J. Endocrinol. 153(6), 853–860 (2005).
Stovall, D. W., Scriver, J. L., Clayton, A. H., Williams, C. D. & Pastore, L. M. Sexual function in women with polycystic ovary syndrome. J. Sex. Med. 9(1), 224–230 (2012).
Mantzou, D. et al. Impaired sexual function in young women with PCOS: The detrimental effect of anovulation. J. Sex. Med. 18(11), 1872–1879 (2021).
Lizneva, D. et al. Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertil. Steril. 106(1), 6–15 (2016).
Norman, R. J., Dewailly, D., Legro, R. S. & Hickey, T. E. Polycystic ovary syndrome. The Lancet. 370(9588), 685–697 (2007).
Månsson, M. et al. Sexuality and psychological wellbeing in women with polycystic ovary syndrome compared with healthy controls. Eur.J. Obstet. Gynecol. Reprod. Biol. 155(2), 161–165 (2011).
Ercan, C. et al. Sexual dysfunction assessment and hormonal correlations in patients with polycystic ovary syndrome. Int. J. Impot. Res. 25(4), 127–132 (2013).
Hodgins, M. B., Spike, R. C., Mackie, R. M. & MacLean, A. B. An immunohistochemical study of androgen, oestrogen and progesterone receptors in the vulva and vagina. BJOG Int. J. Obstet. Gynaecol. 105(2), 216–222 (1998).
Li, Q., Sullivan, N. R., McAllister, C. E., Van de Kar, L. D. & Muma, N. A. Estradiol accelerates the effects of fluoxetine on serotonin 1A receptor signaling. Psychoneuroendocrinology 38(7), 1145–1157 (2013).
Morotti, E. et al. Body imaging and sexual behavior in lean women with polycystic ovary syndrome. J. Sex. Med. 10(11), 2752–2760 (2013).
van Anders, S. M. & Dunn, E. J. Are gonadal steroids linked with orgasm perceptions and sexual assertiveness in women and men?. Horm. Behav. 56(2), 206–213 (2009).
Dilbaz, B., Çınar, M., Özkaya, E., Tonyalı, N. V. & Dilbaz, S. Health related quality of life among different PCOS phenotypes of infertile women. J. Turk. Ger. Gynecol. Assoc. 13(4), 247 (2012).
Hashemi, S., Tehrani, F. R., Farahmand, M. & Khomami, M. B. Association of PCOS and its clinical signs with sexual function among Iranian women affected by PCOS. J. Sex. Med. 11(10), 2508–2514 (2014).
Acknowledgements
This study was carried out with the kind collaboration of the participants. It is a part of a research work done in Tarbiat Modares University, Tehran, Iran. There were no conflicts of interest.
Author information
Authors and Affiliations
Contributions
S.J.S. and M.Y. contributed to the conception and design of the study; S.J.S., M.Y., K.A. and N.M. did the literature search; S.J.S., N.M., and M.Y. performed the statistical analysis; and K.A. and N.M. wrote the first draft of the manuscript. All authors contributed to the manuscript revision and read and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yarjanli, M., Jahanian Sadatmahalleh, S., Mirzaei, N. et al. Female sexual function in different phenotypes of polycystic ovarian syndrome: a comparative cross-sectional study. Sci Rep 12, 19317 (2022). https://doi.org/10.1038/s41598-022-24026-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-24026-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.