Abstract
Up to now, there is only limited information available on a possible relationship between clinical characteristics and the mineralization of metacarpal bones and finger joint space distance (JSD) in patients with psoriatic arthritis (PsA). Computerized digital imaging techniques like digital X-ray radiogrammetry (DXR) and computer-aided joint space analysis (CAJSA) have significantly improved the structural analysis of hand radiographs and facilitate the recognition of radiographic damage. The objective of this study was to evaluate clinical features which potentially influence periarticular mineralization of the metacarpal bones and finger JSD in PsA-patients. 201 patients with PsA underwent computerized measurements of the metacarpal bone mineral density (BMD) with DXR and JSD of all finger joints by CAJSA. DXR-BMD and JSD were compared with clinical features such as age and sex, disease duration, C-reactive protein (CRP) as well as treatment with prednisone and disease-modifying antirheumatic drugs (DMARDs). A longer disease duration and an elevated CRP value were associated with a significant reduction of DXR-BMD, whereas JSD-parameters were not affected by both parameters. DXR-BMD was significantly reduced in the prednisone group (–0.0383 g/cm²), but prednisone showed no impact on finger JSD. Patients under the treatment with bDMARDs presented significant lower DXR-BMD (–0.380 g/cm²), JSDMCP (–0.0179 cm), and JSDPIP (–0.0121 cm) values. Metacarpal BMD was influenced by inflammatory activity, prednisone use, and DMARDs. In contrast, finger JSD showed only a change compared to baseline therapy. Therefore, metacarpal BMD as well as finger JSD represent radiographic destruction under different aspects.
Similar content being viewed by others
Introduction
Psoriatic arthritis (PsA) is a multisystemic and chronic inflammatory musculoskeletal disease associated with cutaneous psoriasis, affecting most commonly the axial skeleton as well as peripheral joints of hands and feet1,2.
Conventional radiology has been the gold standard assessing the damage and radiographic progression in PsA2,3. As shown by Siannis et al., in the majority of patients radiological damage is detected before clinical damage is observed4.
Computer-aided image analysis is increasingly utilized within radiology, connecting elements of artificial intelligence and computer vision with radiological image processing. Computer-based structural analysis of hand radiographs include digital X-ray radiogrammetry (DXR) and computer-aided joint space analysis (CAJSA). These diagnostic techniques allow the quantification of bone mineral density (BMD) and finger joint space distance (JSD) in rheumatoid arthritis (RA) and PsA5,6,7. Therefore, DXR- and CAJSA-parameters serve as surrogate markers for radiological and structural damage as well as for radiological progression in RA5,8.
Some recent published studies revealed a demineralization of the metacarpal bones in PsA and BMD as an additional hallmark of radiographic damage in PsA6,9,10. In addition, joint space narrowing of finger joints represents a characteristic radiologic feature of the PsA-associated joint destruction process2.
So far, there is little information available regarding the relationship between clinical attributes and the mineralization of the metacarpal bones and finger JSD in patients with PsA. Therefore, the aim of our retrospective study was to evaluate clinical parameters which potentially influence periarticular mineralization of metacarpal bones as well as finger JSD in these patients.
Methods
The study enrolled 201 PsA-patients. The following parameters were captured as clinical features: Disease duration, swollen joint count (SJC), tender joint count (TJC) inflammatory activity measured by C-reactive protein (CRP) and Disease Activity Score 28 (DAS28) as well as therapy with prednisone, non-steroidal anti-inflammatory drugs (NSAIDs), coxibs and disease-modifying antirheumatic drugs (DMARDs). Data of SJC, TJC and DAS28 were available for 58 patients. All subjects underwent radiographic examinations of the hands (anteroposterior view).
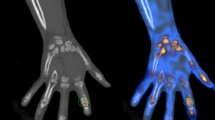
Computer-based structural analysis (Fig. 1)
Computer-based structural analysis of the hands included DXR for the quantification of metacarpal bone mineralization and CAJSA for the quantification of finger JSD.
Digital X-ray radiogrammetry
DXR (Pronosco X-Posure System™, Version 2.0; Sectra; Sweden) was applied to determine BMD (g/cm2)11. All plain radiographs were subsequently scanned (Scanner UMAX Power Look 1100, resolution 300 dots per inch) into the DXR system, turning them into digital images.
The system performs a continuous self-testing validation to maintain the quality of digital X-ray imaging, stopping the process when imaging becomes inferior (i.e. incorrect determination of bone contours and false identification of bone structures). The computer algorithms automatically defined regions of interest around the narrowest bone parts of the metacarpals II, III and IV and subsequently determined the outer and inner cortical edges of the cortical metacarpal bone parts and bone mineral density of the metacarpal bones (DXR-BMD) was verified.
Computer-aided joint space analysis
CAJSA (Radiogrammetry Kit, Version 1.3.6; Sectra; Sweden) measured all JSDMCP (metacarpophalangeal joints, thumb to small finger), JSDPIP (proximal interphalangeal joints, index finger to small finger), and JSDDIP (distal interphalangeal joints, index finger to small finger). The measurement procedure was performed as follows: positioning of the region of interest to mark the particular joint to be measured. This is the only operator-dependent procedure in the entire measurement process. The CAJSA software is based on an automatic edge filtering within the region of interest identifying the specified joints. A 1.5 cm long edge across each bone was further determined and the distance between the two edges estimated as a function of the horizontal position. This was followed by calculation of the mean average and standard deviation of the distance over an extended interval of 0.8 cm by the CAJSA software. The distance between the bones was defined to be the edge interval for which the standard deviation is minimal. Additional, the Z-score as an age- and sex-independent parameter for the quantification of finger JSD was quantified12.
Statistical analysis
Statistical computations were performed, using the programming language Python (version 3.6.9) and the additional packages NumPy (version 1.16.2), pandas (version 0.25.0), and Statsmodels (version 0.11.1). Data visualisation was carried out using the packages Matplotlib (version 3.3.0) and Seaborn (version 0.9.0).
The results of the DXR- and CAJSA-measurements were expressed as mean and standard deviation.
To adjust for age and sex-related changes in finger JSD that are disease-independent, Z-scores of all finger JSD were calculated according to Pfeil et al. 200912 as followed:
To adjust for age- and sex-related changes in BMD as well as disease-associated finger JSD, linear regressions models (statsmodels.formula.api.ols) were adjusted for DXR-BMD and all finger JSDs as well as their Z-scores as dependent variables (y_i), using age and sex as independent variables (Eq. 1).
The respective residuals of these models were used as dependent variables (y_resid_i) in linear regression models for SJC, TJC, CPR, DAS28, disease duration, prednisone and DMARDs treatment as independent variables (x_j). Furthermore, all Z-scores were adjusted for disease-associated age and sex-related effects accordingly (Eq. 2).
To stabilize variance and compensate skewness, the continuous variables CRP and disease duration were log10 transformed prior to linear regression. Since disease duration included zeros, an off set of one year was added to disease duration before log10 transformation.
Anova Type II (statsmodels.stats.anova.anova_lm) was used for all linear regression models. P-values were reported to describe the influence of the respective independent variable on the respective dependent variable. P-values < 0.05 were considered as significant results.
Ethics approval
All examinations were performed in accordance with the rules and regulations of the local human research and Ethics Committee. The study protocol was approved by the Ethics Committee of the Friedrich-Schiller-University Jena, Germany (registration number 2018-1212). A consent was obtained from all subjects and/or their legal guardian(s). As a special note, the authors emphasize that all radiographs used for DXR- and CAJSA-calculations were performed as part of routine clinical care; no additional radiographs were obtained only for study purposes.
Results
Baseline characteristics (Table 1).
The study enrolled 201 PsA-patients (79 men and 122 women). The mean age was 53.8 ± 13.6 years. The mean disease duration was 6.8 ± 9.8 years and CRP was 10.1 ± 19.6 mg/l. 33 patients were administered prednisone (mean dosage: 7.5 ± 8.2 mg). In addition, 116 subjects were treated with NSAIDs or coxibs, 58 patients received conventional synthetic DMARDs (csDMARDs), and 27 participants biological DMARDs (bDMARDs).
Influence of age and sex on DXR-BMD, JSD, and Z-score (Fig. 2)
Adjustment of bone mineral density (BMD), measured by digital X-ray radiogrammetry (DXR), finger JSD, and Z-score [metacarpophalangeal joint (MCP), proximal interphalangeal joint (PIP)1, distal interphalangeal joint (DIP)] as quantified by computer-aided joint space analysis (CAJSA) regarding age and sex [A: P = 5.5e−03 (P < 0.05), P = 6.3e−10* (P < 0.001); B: P = 1.6e−01 (P = n. s.), P = 2.5e−06* (P < 0.001); C: P = 6.0e−02 (P = n. s.), 7.4e−05* (P < 0.001); D: P = 8.4e−02 (P = n. s.), 3.8e−08* (P < 0.001); E: 3.7e−07* (P < 0.001), P = 2.7e−02 (P < 0.05), P = 1.9e−01 (P = n. s.)].
The linear regression revealed a significant negative influence of age (regression coefficient β = − 2.26e−03; P < 0.001) and sex (β = −2.72e−02; P < 0.01) on DXR-BMD. Regarding the interaction of age and JSD, a significant β of −7.37e−04 (MCP), −4.43e−04 (PIP), and −7.32e−04 (DIP) was shown.
Influence of DMARDs- and prednisone treatment, disease duration and disease activity on DXR-BMD, JSD, and Z-score
DXR-BMD (Tables 2, 3, 4, 5 and 6, Fig. 3):
Linear regression model for DMARDs, prednisone, DAS28, SJC, TJC, disease duration, and CRP as independent variables of bone mineral density (DXR-BMD) after the correction of age and sex [A: P = 4.4e−03 (P < 0.05); B: P = 2.6e−02 (P < 0.05); C: P = 5.7e−01 (P = n. s.); D: P = 8.6e−01 (P = n. s.); E: P = 8.8e−01 (P = n. s.); F: P = 2.0e−02 (P < 0.05); G: P = 4.2e−02 (P < 0.05)].
Regarding disease duration, there was a significant reduction of the DXR-BMD (difference: −0.0036 g/cm2) between a disease duration less than two years and more than 10 years.
DAS28 revealed a non-significant difference (−0.0082 g/cm2) for active PsA. A similar result was quantified for TJC (difference: −0.0127 g/cm2) and SJC (difference: −0.0183 g/cm2). Concerning CRP levels, a significant change was evaluated for DXR-BMD.
An equivalent result was observed for treatment with prednisone on DXR-BMD (difference: −0.0383 g/cm2). Patients treated with bDMARDs presented a significant lower DXR-BMD (difference: −0.0380 g/cm2), compared to patients treated with NSAIDs/coxibs.
JSD (Tables 2, 3, 4, 5 and 6, Fig. 4)
Linear regression model for DMARDs, prednisone, DAS28, SJC, TJC, disease duration, and CRP as independent variables on JSD [metacarpophalangeal joint (MCP), proximal interphalangeal joint (PIP), distal interphalangeal joint (DIP)] after the correction of age and sex [A: P = 2.2e−05 (P < 0.001); B: P = 8.0e−01 (P = n. s.); C: P = 1.5e−01 (P = n. s.); D: P = 6.6e−01 (P = n. s.); E: P = 4.7e−02 (P < 0.05); F: P = 2.0e−03 (P < 0.05); G: P = 7.7e−01 (P = n. s.); I: P = 1.0e−02 (p < 0.05); J: P = 5.3e−01 (P = n.s.); K: P = 7.2e−01 (P = n.s.); L: P = 8.3e−01 (P = n.s.); M: P = 7.2e−01 (P = n.s.); N: P = 6.8e−01 (P = n.s.); O: P = 4.6e−01 (P = n.s.); P: P = 7.0e–02 (P = n.s.); Q: P = 8.2e−01 (P = n.s.); R: P = 5.1e−01 (P = n.s.); S: P = 7.1e−01 (P = n.s.); T: P = 1.5e−01 (P = n.s.); U: P = 2.4e−01 (P = n.s.); V: P = 3.0e−01 (P = n.s.)].
Disease duration, SJC, TJC, DAS28 and CRP showed no significant association to all JSD-parameters in the regression analysis. This also applies to prednisone, showing no significant impact on finger JSD. Furthermore, linear regression analysis revealed a significant influence of DMARDs on JSDMCP (difference: −0.0179 cm) and JSDPIP (difference: −0.0121 cm). DMARDs revealed no significant linear regression analysis to JSDDIP.
Z-score (Tables 2, 3, 4, 5 and 6, Fig. 5)
Linear regression model for DMARDs, prednisone, DAS28, SJC, TJC, disease duration, and CRP as independent variables on the Z-score [metacarpophalangeal joint (MCP), proximal interphalangeal joint (PIP), distal interphalangeal joint (DIP)] after the correction of age and sex [A: P = 4.9e–05 (P < 0.001); B: P = 6.3e−01 (P = n. s.); C: P = 1.2e−01 (P = n.s.); D: P = 5.9e−01 (P = n.s.); E: P = 2.9e−01 (P < 0.05); F: P = 2.2e−03 (P < 0.05); G: P = 5.1e−01 (P = n.s.); I: P = 1.0e−02 (P < 0.05); J: P = 3.6e−01 (p = n. s.); K: P = 5.7e−01 (P = n.s.); L: P = 8.5e−01 (P = n.s.); M: P = 6.4e−01 (P = n.s.); N: P = 7.4e−01 (P = n.s.); O: P = 3.0e−01 (P = n.s.); P: P = 6.1e−02 (P = n.s.); Q: P = 7.2e−01 (P = n.s.); R: P = 4.5e−01 (P = n.s.); S: P = 7.7e−01 (P = n.s.); T: P = 1.7e−01 (P = n.s.); U: P = 3.7e−01 (P = n.s.); V: P = 7.5e−01 (P = n.s.)].
No association was found between the Z-score and the treatment with disease duration, SJC, TJC, DAS28, CRP and prednisone.
In accordance with JSD, the Z-score of MCP- and PIP-joints was influenced by bDMARDs with a reduction of the Z-scoreMCP (difference: −0.5028) and Z-scorePIP (difference: −0.5725), whereas the Z-scoreDIP was not significantly reduced.
Discussion
In contrast to the significant improvement in the understanding of the pathogenesis and treatment of PsA in the last ten years, there is only little known regarding the impact of clinical features on structural and radiological damage. To close this gap, the aim of our retrospective study was to quantify clinical parameters which influence periarticular mineralization of the metacarpal bones and finger JSD in PsA-patients.
In our study, a decrease in DXR-BMD was found for both disease duration and elevated CRP. In addition, prednisone use was associated with a decreased DXR-BMD. However, these parameters did not have an impact on JSD and Z-score. Furthermore, we demonstrated a decrease in DXR-BMD and JSDMCP as well as JSDPIP under therapy with bDMARDs.
Computer-aided techniques including DXR and CAJSA serve as innovative tools in the quantification of radiological damage5,6,13. The computer-based structural analysis of hand radiographs offers significant advantages in the quantification of radiographic damage in inflammatory arthritis (e. g. RA and PsA) in comparison with conventional scoring of hand radiographs6,13,14,15. Mainly, the computer-based measurement of DXR-BMD (coefficient of variation: 0.13–1.50%) and CAJSA-JSD (coefficient of variation: 0.38–0.66%) provide a high reproducibility, compared to standard scoring methods for the detection of radiographic damage (e. g. reproducibility of the van der Heijde modification of the Sharp Score: 1.8–3.8%)16,17,18. Therefore, detailed changes of bone structure and JSD are noticeable, especially with regard to the detection of treatment effects, and represent markers for structural damage13,14,15.
The present study evaluated the influence of clinical features such as disease duration, inflammatory activity, prednisone use, and other different treatment strategies on structural parameters of the hands as measured by DXR-BMD and finger JSD in PsA-patients.
In our study, PsA-patients with a disease duration of more than ten years showed a significantly reduced DXR-BMD, JSDMCP and Z-ScoreMCP. This is in accordance with previous data, which revealed an increase of erosive bone changes in PsA, depending on disease duration as measured with high-resolution peripheral quantitative computed-tomography (HR-pQCT)19. In this context, the results of our study revealed a significant influence of age on DXR-BMD and finger JSD in PsA patients which has also been shown in healthy subjects20,21,22. Simon et al. reported a lower volumetric articular BMD of the MCP-joints, measured by HR-pQCT in PsA-patients, compared with healthy subjects23. In addition, patients with RA showed a significantly reduced DXR-BMD (− 20.7%) and JSD of MCP-joints (− 18.9%) versus a healthy control group12,24. Sex had an additional impact on DXR-BMD, whereas JSD was not influenced. As demonstrated before, the DXR-BMD in healthy women is significantly lower (−12.8%) versus healthy men20.
Inflammatory activity is strongly associated with radiographic damage in PsA25. Regarding inflammatory activity as measured by CRP levels, PsA-patients with increased CRP values showed a reduced DXR-BMD. The linear regression models yielded a significant impact of CRP on DXR-BMD. Furthermore, Wu et al. reported a significant bone loss of the second and third metacarpal bone head, quantified by HR-pQCT in association with elevated CRP values in PsA-patients26. These results highlight the strong interaction of inflammatory activity and demineralization of metacarpal bones in inflammatory arthritis which was also published for RA27,28. Additionally, CRP served as an independent predictor of radiographic progression in PsA29. At the time of initial diagnosis, elevated CRP levels were associated with new erosions as a marker for radiographic progression30.
We demonstrated, that treatment with prednisone was associated with a significant reduction of DXR-BMD ( -0.0383 g/cm²). A negative correlation between the change of DXR-BMD over 24 months and the use of corticosteroids (r = −0.27; P < 0.005) was also observed by Hoff et al.10. These results indicate that corticosteroids can lead to a demineralization of metacarpal bones. The JSD-parameters in our study revealed no significant changes in association with prednisone treatment. Bond et al. showed an increase of radiological damage, assessed with the Steinbrocker staging system under corticosteroids31, where the Steinbrocker method represented a composite score including the quantification of periarticular demineralisations, erosions, joint space narrowing and ankyloses.
Recently published studies showed periarticular metacarpal demineralization6,9,10,19 as well as metacarpal bone loss dependent on radiographic damage quantified by Psoriatic Arthritis modified van der Heijde Sharp Score or Psoriatic Arthritis Ratingen Score in patients with PsA6. Additionally, finger joint space narrowing represented a common radiographic hallmark for structural damage in PsA. In summary, both parameters reflected PsA-associated radiographic damage. In the present study, treatment with bDMARDs resulted in a significant lower DXR-BMD (−0.0380 g/cm2), JSDMCP (−0.0179 cm), JSDPIP (−0.0121 cm), Z-scoreMCP (−0.5028) and Z-scorePIP (−0.5725) compared to csDMARDs and NSAIDs. Concerning DXR-BMD and CAJSA-JSD as radiographic markers of damage and disease severity5,8, bDMARDs-treated patients in our study showed more structural damage, which is explainable with the advanced course of the disease.
As a result, patients with an accentuated radiographic damage should be treated earlier with bDMARDs to avoid radiographic structural damage. In this case, the use of csDMARDs should be critically questioned, whereas bDMARDs revealed also higher response rates and reduced radiographic progression in PsA32. Radiographic damage and progression correlated with the Health Assessment Questionnaire (HAQ) as outcome marker for disability33.
Our study is potentially limited by the cross-sectional design which showed an association of the clinical characteristics of PsA-patients in the mineralisation of the metacarpal bones and the finger joint space width. Further investigations are needed to verify these results in a longitudinal prospective study design. However, the present study offered the first insights of the influence of clinical features on DXR-BMD and JSD as surrogate markers of radiographic damage in PsA patients.
Conclusion
In conclusion, metacarpal BMD measured by DXR and finger JSD quantified by CAJSA are established markers in the quantification of radiographic damage in PsA-patients. Metacarpal BMD was more influenced by clinical factors like disease duration, inflammatory activity, prednisone, and DMARDs compared to finger JSD which was significantly reduced by DMARDs. In this context, DXR-BMD and JSD represent radiographic damage under different aspects.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- bDMARDs:
-
Biological disease-modifying anti-rheumatic drugs
- CAJSA:
-
Computer-aided joint space analysis
- CRP:
-
C-reactive protein
- csDMARDs:
-
Conventional synthetic disease-modifying antirheumatic drugs
- DIP:
-
Distal interphalangeal joint
- DAS28:
-
Disease Activity Score 28
- DXR:
-
Digital X-ray radiogrammetry
- DXR-BMD:
-
Bone mineral density (g/cm2) estimated by DXR
- HR-pQCT:
-
High-resolution peripheral quantitative computed-tomography
- JSD:
-
Joint space distance
- MCP:
-
Metacarpophalangeal joint
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- n.s.:
-
Not significant
- PIP:
-
Proximal interphalangeal joint
- PsA:
-
Psoriatic arthritis
- SD:
-
Standard deviation
- SJC:
-
Swollen joint count
- TJC:
-
Tender joint count
References
Ocampo, D. V. & Gladman, D. Psoriatic arthritis. F1000Research 2019, 8 (2019).
Wassenberg, S. Radiographic scoring methods in psoriatic arthritis. Clin. Exp. Rheumatol. 33(5 Suppl 93), S55–S59 (2015).
van der Heijde, D., Sharp, J., Wassenberg, S., & Gladman, D.D. Psoriatic arthritis imaging: A review of scoring methods. Ann. Rheum. Dis. 64(Suppl 2), ii61–4 (2005).
Siannis, F., Farewell, V. T., Cook, R. J., Schentag, C. T. & Gladman, D. D. Clinical and radiological damage in psoriatic arthritis. Ann. Rheum. Dis. 65(4), 478–481 (2006).
Pfeil, A. et al. Joint damage in rheumatoid arthritis: Assessment of a new scoring method. Arthritis Res. Ther. 15(1), R27 (2013).
Pfeil, A. et al. Psoriatic arthritis is associated with bone loss of the metacarpals. Arthritis Res. Ther. 18(1), 248 (2016).
Pfeil, A. et al. Visualisation of structural damage as a surrogate marker of radiographic progression in patients with rheumatoid arthritis. Ann. Rheum. Dis. 73(4), e24 (2014).
Pfeil, A. et al. Value of digital X-ray radiogrammetry in the assessment of inflammatory bone loss in rheumatoid arthritis. Arthritis Care Res. (Hoboken). 63(5), 666–674 (2011).
Kocijan, R. et al. Quantitative and qualitative changes of bone in psoriasis and psoriatic arthritis patients. J. Bone Miner. Res. 30(10), 1775–1783 (2015).
Hoff, M., Kavanaugh, A. & Haugeberg, G. Hand bone loss in patients with psoriatic arthritis: Posthoc analysis of IMPACT II data comparing infliximab and placebo. J. Rheumatol. 40(8), 1344–1348 (2013).
Rosholm, A., Hyldstrup, L., Backsgaard, L., Grunkin, M. & Thodberg, H. H. Estimation of bone mineral density by digital X-ray radiogrammetry: Theoretical background and clinical testing. Osteoporos. Int. 12(11), 961–969 (2001).
Pfeil, A. et al. Implementation of Z-scores as an age- and sex-independent parameter for estimating joint space widths in rheumatoid arthritis. J. Rheumatol. 36(4), 717–723 (2009).
Pfeil, A. et al. Is there a role for digital X-ray radiogrammetry as surrogate marker for radiological progression and imaging of structural integrity in rheumatoid arthritis?. BMC Musculoskelet. Disord. 16, 155 (2015).
Pfeil, A. et al. Inhibition of periarticular bone loss is associated with clinical remission and ACR70-Response in rheumatoid arthritis. Rheumatol. Int. 39(4), 637–645 (2019).
Pfeil, A. et al. Radiographic remission in rheumatoid arthritis quantified by computer-aided joint space analysis (CASJA): A post hoc analysis of the RAPID 1 trial. Arthritis Res. Ther. 22(1), 229 (2020).
Pfeil, A. et al. Reproducibility and influence of hand rotation on computer-aided joint space analysis. Jt. Bone Spine 79(4), 384–388 (2012).
Bottcher, J. et al. Influence of image-capturing parameters on digital X-ray radiogrammetry. J. Clin. Densitom. 8(1), 87–94 (2005).
Rau, R. & Wassenberg, S. Imaging techniques in rheumatology: Scoring methods in rheumatoid arthritis. Z. Rheumatol. 62(6), 555–565 (2003).
Simon, D. et al. Simultaneous quantification of bone erosions and enthesiophytes in the joints of patients with psoriasis or psoriatic arthritis—Effects of age and disease duration. Arthritis Res. Ther. 20(1), 203 (2018).
Bottcher, J. et al. Normative data for digital X-ray radiogrammetry from a female and male German cohort. J. Clin. Densitom. 9(3), 341–350 (2006).
Pfeil, A. et al. Normative reference values of joint space width estimated by computer-aided joint space analysis (CAJSA): The distal interphalangeal joint. J. Digit. Imaging. 21(Suppl 1), 104–112 (2008).
Pfeil, A. et al. Computer-aided joint space analysis of the metacarpal-phalangeal and proximal-interphalangeal finger joint: Normative age-related and gender-specific data. Skelet. Radiol. 36(9), 853–864 (2007).
Simon, D. et al. A comparative analysis of articular bone in large cohort of patients with chronic inflammatory diseases of the joints, the gut and the skin. Bone 116, 87–93 (2018).
Pfeil, A. et al. Digital X-ray radiogrammetry and its sensitivity and specificity for the identification of rheumatoid arthritis-related cortical hand bone loss. J. Bone Miner. Metab. 35(2), 192–198 (2017).
Aletaha, D., Alasti, F. & Smolen, J. S. Disease activity states of the DAPSA, a psoriatic arthritis specific instrument, are valid against functional status and structural progression. Ann. Rheum. Dis. 76(2), 418–421 (2017).
Wu, D. et al. Comparison of bone structure and microstructure in the metacarpal heads between patients with psoriatic arthritis and healthy controls: An HR-pQCT study. Osteoporos. Int. 31(5), 941–950 (2020).
Pye, S. R. et al. Disease activity and severity in early inflammatory arthritis predict hand cortical bone loss. Rheumatology (Oxford) 49(10), 1943–1948 (2010).
Bøyesen, P. et al. Antibodies to cyclic citrullinated protein and erythrocyte sedimentation rate predict hand bone loss in patients with rheumatoid arthritis of short duration: A longitudinal study. Arthritis Res. Ther. 11(4), R103 (2009).
Gladman, D. D. et al. Risk factors for radiographic progression in psoriatic arthritis: Subanalysis of the randomized controlled trial ADEPT. Arthritis Res. Ther. 12(3), R113 (2010).
Haroon, M., Gallaghar, P., Ahmad, M. & FitzGerald, O. Elevated CRP even at the first visit to a rheumatologist is associated with long-term poor outcomes in patients with psoriatic arthritis. Clin. Rheumatol. 39(10), 2951–2961 (2020).
Bond, S. J., Farewell, V. T., Schentag, C. T. & Gladman, D. D. Predictors for radiological damage in psoriatic arthritis: Results from a single centre. Ann. Rheum. Dis. 66(3), 370–376 (2007).
Mease, P. J. et al. Etanercept and methotrexate as monotherapy or in combination for psoriatic arthritis: Primary results from a randomized, controlled phase III trial. Arthritis Rheumatol. 71(7), 1112–1124 (2019).
Feced Olmos, C. M. et al. Relationship between structural damage with loss of strength and functional disability in psoriatic arthritis patients. Clin. Biomech. (Bristol, Avon). 68, 169–174 (2019).
Acknowledgements
The authors would like to thank Ms. Monika Arens (managing director, Arewus GmbH) and Mr. Jacob Algulin (managing director, Sectra, Sweden) for the use of the digital X-ray radiogrammetry and the computer-aided joint space analysis. Many thanks to Dr. Katrina Recker for the editing of the manuscript. Also many thanks to Ms. Dr. rer. nat. Kirsten Hessel (Novartis Pharma GmbH, Nürnberg, Germany) for the support in performing the investigator-initiated study in Jena, Germany and for the helpful critical discussion of the data.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study is a part of the Investigator Initiated study “The quantification of radiographic destruction and progression of psoriatic arthritis using computer based structure analysis” which is supported by Novartis Pharma GmbH, Roonstraße 25, 990429 Nürnberg, Germany.
Author information
Authors and Affiliations
Contributions
A.P. and J.B. designed the study, analysed the radiographs, performed the statistical analysis, wrote the manuscript and revised the manuscript. M.H. performed the DXR- and CAJSA-analysis as well as the study design. T.W. and D.D. performed the statistical analysis. D.R. and M.F. interpreted the data and helped to draft the manuscript. P.O. edited the manuscript. G.W. interpreted the data and edited the manuscript. A.M. participated on the study design, and wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pfeil, A., Heinz, M., Hoffmann, T. et al. The relationship between structural analysis of the hand and clinical characteristics in psoriatic arthritis. Sci Rep 12, 18913 (2022). https://doi.org/10.1038/s41598-022-23555-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-23555-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.