Abstract
Polypharmacy and its rising global prevalence is a growing public health burden. Using a large representative nationwide Korean cohort (N = 761,145), we conducted a retrospective cross-sectional study aiming to identify subpopulations of patients with polypharmacy and characterize their unique patterns through cluster analysis. Patients aged ≥ 30 years who were prescribed at least one medication between 2014 and 2018 were included in our study. Six clusters were identified: cluster 1 mostly included patients who were hospitalized for a long time (4.3 ± 5.3 days); cluster 2 consisted of patients with disabilities (100.0%) and had the highest mean number of prescription drugs (7.7 ± 2.8 medications); cluster 3 was a group of low-income patients (99.9%); cluster 4 was a group of high-income patients (80.2%) who frequently (46.4 ± 25.9 days) visited hospitals/clinics (7.3 ± 2.7 places); cluster 5 was mostly elderly (74.9 ± 9.8 years) females (80.3%); and cluster 6 comprised mostly middle-aged (56.4 ± 1.5 years) males (88.6%) (all P < 0.001). Patients in clusters 1–5 had more prescribed medications and outpatient visit days than those in cluster 6 (all P < 0.001). Given limited health care resources, individuals with any of the identified phenotypes may be preferential candidates for participation in intervention programs for optimal medication use.
Similar content being viewed by others
Introduction
Polypharmacy is a growing major public health burden with rising global prevalence; the proportion of the older population continues to increase and they usually have a number of chronic health conditions1. Although there is no clear consensus on the definition of polypharmacy, the term is commonly defined as the routine use of five or more concurrent medications2,3,4. It has been estimated that the global prevalence of polypharmacy among residents in long-term care facilities accounts for 38–91%5. In Korea, approximately half of the elderly population, aged ≥ 65 years, receive multi-drug prescriptions and considering the current aging trend, that number is expected to further increase in the future6,7.
Patients with polypharmacy have a higher risk of harmful effects, such as medication errors, adverse drug reactions, falls, dizziness, and increases in hospitalization and mortality8,9,10. It has been reported that inappropriate management of polypharmacy has a significant impact on avoidable expenditure on health care resources and costs, leading to a large economic burden11,12. Accordingly, the World Health Organization has asked countries and the concerned authorities to prioritize medication safety in polypharmacy, take early action, and reduce avoidable medication-related harm13.
Although some countries are developing evidence-based strategies and introducing them for the optimal use of multiple medications, structured management programs or their supporting policies are still limited in many countries, including Korea14,15,16,17,18. It is emphasized that a comprehensive consideration in the clinical context, rather than a simple approach with the number of medications used, is essential to develop rational policies to improve polypharmacy use behavior2,3,19. To the best of our knowledge, most studies on polypharmacy conducted in Korea have only targeted certain vulnerable patient groups, such as the elderly and severely ill, and only simple status, including the prevalence of polypharmacy and its mortality, have been reported6,7,20. In-depth research to determine several distinct phenotypes of patients with polypharmacy could be helpful in developing effective management strategies by diversifying their countermeasures accordingly.
Therefore, using a large nationwide cohort of Korean adults, this study aimed to identify subpopulations of patients with polypharmacy and characterize their unique patterns through cluster analysis.
Results
A total of 761,145 patients were included in the training set for cluster analysis. Their mean age was 67.05 ± 12.57 years, and those aged 70–79 years accounted for majority (29.78%). Of all patients, 88,674 (11.65%) were medical aid beneficiaries. The mean number of outpatient visits was 30.61 ± 27.11 days, and 226,283 patients (29.73%) were hospitalized. Among medical institutions by type, the medical clinic was visited by most patients (89.84%). Patients visited a mean of 4.72 ± 2.87 medical institutions per year and prescribed 7.03 ± 2.42 medications. The most common diseases among patients were chronic gastritis/gastroesophageal reflux disease (639,017 patients, 83.95%), hypertension (584,156 patients, 76.75%), and dyslipidemia (503,941 patients, 66.21%) (Table 1).
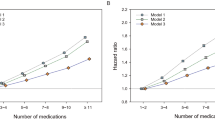
The results of determining the optimal number of clusters, using the elbow method, are presented in Fig. 1. The scree plots provided the optimal number of clusters, which was determined to be six. Of the six clusters of patients with polypharmacy, cluster 4 had the largest distribution. In cluster 5, the proportion of females was 80.3%, and the average age was the highest, at 74.9 years. In cluster 6, 88.6% were male, and the average age was 56.4 years. In cluster 3, 44.5% were medical aid beneficiaries, and the remaining 55.4% were National Health Insurance subscribers with relatively low incomes. On the other hand, there was no medical aid beneficiary in cluster 4 and 80.2% had a relatively high income level. All patients in cluster 2 had disabilities (all P < 0.001) (Table 2). The characteristics of health care utilization by cluster are shown in Fig. 2. Cluster 2 had the highest number of prescribed medications (7.7 ± 2.8 medications). In cluster 1, all patients experienced hospitalization, and 27.7% of the patients were hospitalized for > 6 days, which was the highest among the clusters. The proportion of outpatient visits exceeding 31 days per year was 77.5% in cluster 4, which was significantly higher than that of the other clusters. As for the number of visiting medical institutions, 80.8% of cluster 4 visited six or more institutions per year (all P < 0.001) (Fig. 2). The results of the multiple linear regression analysis are presented in Supplementary Table S1. Compared with patients in cluster 6, those in clusters 1–5 reported more prescribed medications (β = 0.70, standard error = 0.01; 1.10, 0.01; 0.65, 0.01; 0.76, 0.01; and 0.09, 0.01, respectively) and more outpatient visit days (β = 5.28, standard error = 0.11; 23.67, 0.10; 24.23, 0.12; 30.69, 0.10; and 0.96, 0.11, respectively) (all P < 0.001) (Supplementary Table S1). Regarding diagnosed diseases, cluster 1 had a higher cancer prevalence than other clusters (16.3%) and a higher number of severe diseases. The prevalence of hypertension was 82.2% in cluster 5, that of dyslipidemia was 71.2% in cluster 6, and that of diabetes was 54.4%, which was higher than that of other clusters (all P < 0.001) (Fig. 3). The most frequently prescribed medications in every cluster were the same in the order of aspirin, atorvastatin, and metformin (data not shown).
Scree plots for the K-means cluster analysis of study patients with polypharmacy. The elbow method was performed to determine the optimal number of clusters by estimating the (A) R-squared value and (B) CCC according to the number of clusters. The analysis used variables including sex, age, type of medical coverage, income level, disability, number of outpatient visits or hospitalization days per year, and number of visited medical institutes per year. These plots indicate that K = 6 is the optimal number of clusters in this study. CCC cubic clustering criterion.
Comparison of health care utilization in six clusters of study patients with polypharmacy. Categorical variables were evaluated by chi-square test and continuous variables by t-test to compare the characteristics of each cluster. The following attributes are described by cluster: (A) the number of prescribed medications per year; (B) hospitalization experience; (C) the number of outpatients visit days per year; (D) the number of medical institutes visited by patients per year; and (E) medical institution type visited by patients (all P < 0.001).
Comparison of diagnosed diseases in six clusters of study patients with polypharmacy. To compare the diagnosed diseases of patients in each cluster, they were evaluated by chi-square test and described by cluster (all P < 0.001). GERD gastroesophageal reflux disease, COPD chronic obstructive pulmonary disease.
Variables with O/E ratios of ≥ 2 or exclusivity of ≥ 25% were observed in each cluster (Supplementary Table S2). The highest O/E ratio and exclusivity were hospitalization for ≥ 6 days in cluster 1 (8.02% and 98.03%, respectively) (all P < 0.001). The validity of this clustering was confirmed by randomly selecting the patients as a test set.
Discussion
To our knowledge, this is the first study to determine subpopulations of patients with polypharmacy and characterize their patterns in a large nationwide cohort. We identified six distinct phenotypes of patients with polypharmacy in the Korean adult population.
In patients with polypharmacy, cluster 1 mostly included patients with severe disease who were hospitalized for a long time or frequently. Cluster 2 was patients with disabilities who had many inpatient and outpatient visits and the highest average number of prescription drugs among all clusters. Cluster 3 was low-income patients, including medical aid beneficiaries, who frequently visited several clinics, while cluster 4 was high-income patients who visited multiple clinics most frequently. Cluster 5 was mostly elderly females, whereas cluster 6 was mostly middle-aged males. Most patients in these last two clusters had multiple mild chronic diseases, but the frequency of visits to medical institutions was relatively lower than in other clusters.
There have been several studies on the characteristics of patients with polypharmacy or related factors. However, no clustering studies have been conducted on polypharmacy based on multi-faceted patient factors. Clustering has usually been performed in a single disease to identify its subtypes of patients regarding their prognosis and to provide tailored approaches to those subtypes21,22,23. Cluster analysis on multimorbidity patients was performed, but only clustering of frequently morbid diseases or prescription drugs was performed24. Our study identified some characteristic phenotypes in patients with polypharmacy, including sociodemographic factors, clinical status, and medical utilization behavior, through K-means cluster analysis.
It has been well elucidated that older age, living in care homes, cancer survivors, and multimorbidity are significantly associated with higher prevalence of polypharmacy3,25. In their study in Japan, Ishizaki et al. reported that patients with more hospitalizations and visits to medical institutions were at a higher risk of polypharmacy26. In our study, most patients with polypharmacy were elderly people with multimorbidity and a group comprising inpatients with severe diseases, such as cancer, was also included. However, in one cluster, the majority were middle-aged males and the patients in some clusters were those with mild chronic diseases who had relatively few visits to medical institutions and did not receive sufficient health care. A study conducted in the United States reported a significant relationship between polypharmacy in Medicaid beneficiaries and higher medical use and expenditures27. This is in line with one cluster found in our study. In Korea, the medical aid program, a public assistance system similar to Medicaid in the United States, has been operated by government authorities for low-income people. Health care services are provided to the entire population in Korea based on a national fee-for-service and mainly two types of health security systems are in operation28. The National Health Insurance program, which is a compulsory social insurance, allows the insured’s contributions and the government subsidy to share health care costs28. Some low-income households are guaranteed to receive appropriate medical services without financial difficulties as medical aid beneficiaries29. The patients in cluster 3 consisted of low-income people with relatively frequent visits to several clinics in the community; many medical aid beneficiaries were included. However, the patients in cluster 4 were high-income older people who used multiple clinics most frequently (Table 2, Fig. 2). In both clusters, the patients often had psychiatric and musculoskeletal disorders and asthma or chronic obstructive pulmonary disease (Fig. 3).
Interestingly, we found that the types of patients with polypharmacy included these opposing groups: inpatients with severe disease or disability, outpatients with mild chronic disease, medical aid beneficiaries and patients with high-income level, and patients who overuse health care and those who do not even receive essential medical care. These findings support that a multi-faceted approach to manage polypharmacy would be more effective in ensuring the optimization of medication prescriptions in patients with various characteristics, rather than a single strategy. Although the policies and systems for polypharmacy management in Korea are still in the introductory stage and mainly focused on general drug safety management, several programs that have demonstrated significant clinical effects in optimizing medication use in patients with polypharmacy have been implemented in other countries30,31,32. These programs commonly provide systematic and structured medication reviews to patients, usually the elderly with multimorbidity. They presented guidelines for patient-centered clinical polypharmacy management with a comprehensive evaluation and approach, rather than simply reducing the number of medications prescribed30,31,32. According to the results of this study, it would be more efficient to diversify intervention strategies by target groups for patient-centered management. For example, hospital-based programs that provide polypharmacy management in hospital-level medical institutions may be appropriate for patients with severe chronic diseases or disabilities. The multidisciplinary team approach of medication management would be effective in the case of a hospital-based model. A clinic-based model in the community would be appropriate for low-income or high-income elderly patients with relatively more frequent visits to multiple clinics. It may be effective to designate regularly visited clinics and activate the primary health care system to control the number of indiscriminate visits to medical institutions. It has been noted that psychotropic drugs including benzodiazepines and antidepressants are one of the most commonly over-prescribed medications worldwide33,34. Previous study has also shown that excessive use of Nonsteroidal anti-inflammatory drugs or overtreatment in patients with musculoskeletal diseases such as arthritis and osteoporosis are common in clinical practice35,36. Based on our findings, it is necessary to manage over-prescription of psychiatric and nonsteroidal anti-inflammatory drugs since patients with polypharmacy often have psychiatric and musculoskeletal disorders. It is also necessary to reorganize the health system to prevent doctor shopping and duplicate prescriptions targeting them as patients often have psychiatric diseases, low-income medical aid beneficiaries included. Elderly females and middle-aged males with mild multimorbidity did not have a relatively high number of visits to medical institutions or prescription medications. Clinic-based programs may be appropriate for patients with mild multimorbidity. It would be effective to provide adequate chronic disease management in primary health care settings. It is necessary to develop and apply standardized management guidelines for multimorbidity, rather than only a single disease.
Given the limited health care resources, it would be efficient for individuals with any of the phenotypes identified in our study to preferentially be included as candidates for participation in intervention programs for optimal medication use.
This study has several limitations that must be carefully considered when interpreting the results. The data used in this study were collected by the National Health Insurance Service (NHIS) for the purposes of claim and reimbursement of medical service costs, not for research purposes37. These collected data did not include records of purchases of non-reimbursable prescriptions and over-the-counter medications that are not covered by the National Health Insurance. However, it is expected to reflect real-world clinical practice through the large sample size, which is nationally representative37. Based on our medication coding method, the number of all medication ingredients that were administered may be greater than the estimated number. The K-means clustering method is not robust to some outliers. Outliers are data that are very far from the cluster centroid and other data points38. Thus, further in-depth studies on the detailed factors related to polypharmacy are needed in the future. Finally, our results were obtained in the Korean health care delivery system. Therefore, they are not generalizable worldwide and consideration of local circumstances is required.
Despite these limitations, this study systematically identified novel patterns and types of patients with polypharmacy and provides a basis for developing effective management programs for tailored improvement of their medication use behavior. Furthermore, our findings could be helpful in developing effective multi-faceted strategies or their supporting policies for the optimal use of multiple medications in patients with various characteristics in the current Korean healthcare system.
In conclusion, this study elucidates distinct subpopulations in terms of sociodemographics, clinical features, and health care utilization in patients with polypharmacy. These findings could contribute to reducing the burden of inappropriate polypharmacy and facilitate appropriate medication use by developing tailored strategies for patients with different tendencies and characteristics.
Methods
Study design and data source
This was a retrospective cross-sectional study, performed using a non-hierarchical clustering method. We used data from the National Health Information Database (NHID), a nationwide database of the entire Korean population. The NHID is a public database with a large volume of health insurance information, including sociodemographics, insurance eligibility, treatment details, medical institution status, and health care utilization among the entire Korean population37. Almost all citizens in Korea are obliged to join the National Health Insurance program as part of the social security system39. The NHIS constructs the NHID by collecting medical information of all citizens based on the health care delivery system of the fee-for-service model and provides it as de-identified data to support various research activities37 (Fig. 4).
This study was conducted in accordance with the Declaration of Helsinki. Written informed consent was waived by the institutional review board of Chung-ang University Hospital because of the characteristics of NHIS data. Before we used the data from the NHID, this study was approved by the Institutional Review Board (IRB) of Chung-ang University Hospital (IRB no.: 2003-010-19308).
Coding of medications
When coding medications in this study, we only used the data on oral medications prescribed to outpatients or inpatients. To clarify the number of prescribed medications, we excluded injections and topical drugs. Medications prescribed for < 180 days per year were also excluded to not include cases of temporary polypharmacy status during the analysis. Each medication was coded based on its main ingredients.
Definition of polypharmacy
Polypharmacy was defined as a case in which five or more medications with different main ingredients were used simultaneously, among prescribed medications. However, over-the-counter medications or medications not covered by health insurance were not included in this definition.
Study Population
Patients aged ≥ 30 years who were prescribed at least one medication from January 1, 2014, to December 31, 2018, were initially retrieved from the entire Korean population enrolled in the NHID. Due to the limited data processing capacity of the server for analysis, 30% of the population (7,106,640 patients) were obtained using a simple random sampling method. We excluded 2,288,749 patients who were prescribed any medication for < 180 days per year to not include cases of temporary polypharmacy status during the analysis. We also excluded patients whose data on prescribed medications were missing or outliers. Of the remaining 4,809,580 patients, those who had five or more medications prescribed simultaneously were included in this study (1,103,336 patients).
A total of 761,145 patients were finally included for cluster modeling as a training set (70% with random sampling), after excluding patients in the test set (remaining 30%) for validation (Fig. 4).
Variables in clustering
Data on sociodemographic characteristics (sex, age, type of medical coverage, income level, and disability), health care utilization (number of outpatient/hospitalization days per year and medical institutions visited), and clinical information (prescribed medications and diagnosed diseases) were collected during the study period.
The study patients were classified into two types according to their medical coverage in Korea. Most of the Korean population is obligated to join the National Health Insurance, so their medical expenses are shared with the government28. Some other populations are included in the government medical aid program and are guaranteed to receive appropriate medical services without financial difficulties29. These medical aid beneficiaries include low-income populations who cannot afford to pay for health care expenses. In this study, except medical aid beneficiaries, the remaining National Health Insurance subscribers were divided into quartiles from the lowest (quartile 1) to the highest income (quartile 4). The number of patients prescribed medication, medical institutions visited, and number of outpatient/hospitalization days were counted on an annual basis. Medical institutions visited by patients were classified by type according to the number of beds and difficulty of treatment, based on the Korean Medical Law. A medical clinic is a medical institution that provides medical treatment to outpatients for common diseases that are frequently encountered in daily life and provides comprehensive health care services through initial contact with patients and can accommodate up to 29 beds40. A hospital was defined as a medical institution with > 30 and < 100 beds, mainly providing medical care to inpatients40. A general hospital mainly provides medical care to inpatients, with > 100 beds, > 7 departments, and an exclusive specialist for each department40. A tertiary hospital is a general hospital that specializes in high-difficulty treatment for severe diseases and is designated after deliberation by health authorities40. The tertiary hospital has > 20 medical departments and specialists dedicated to each department. A long-term care hospital is defined as a hospital with ≥ 30 beds for patients requiring long-term hospitalization. This hospital is mainly for patients who are geriatric, chronically ill, and recovering after surgical operations or injuries40. When a diagnosed disease is coded for each patient from the NHID, the prevalence is not estimated based on the number of related prescriptions received each year, and the information on the five main diseases registered to each patient from any medical institution is retrieved and classified according to the International Classification of Diseases version 1037. The inpatient/outpatient prescription medication history was also collected.
Statistical analysis
For all analysis results, categorical variables are expressed as frequencies and percentages and continuous variables as mean ± standard deviation.
We conducted a descriptive analysis of the study population. K-means cluster analysis was performed to define the clusters of study patients with polypharmacy, and the SAS FASTCLUS procedure was applied using the following variables: sex, age, type of medical coverage, income level, disability, number of outpatient visits or hospitalization days per year, and number of visited medical institutes per year. These variables showed significant differences between polypharmacy (1,103,336 patients) and non-polypharmacy patients (3,706,244 patients) in the initially obtained study population (4,809,580 patients) (data not shown). The R-squared value and cubic clustering criterion (CCC), according to the number of clusters, were estimated to determine the optimal number of clusters, using the elbow method. To compare the characteristics of each cluster obtained, categorical variables were evaluated using the chi-square test and continuous variables by t-test. Multiple linear regression analysis was conducted to compare health care utilization in the six clusters after adjusting for age, sex, and income level. We estimated the observed to expected ratios (O/E ratios) for each variable value in each cluster by dividing the value of each variable in each cluster by the corresponding value in the entire study population. If the O/E ratio was ≥ 2, the variable was considered to clearly show the distinct characteristics of the cluster41. To evaluate the discrimination and stability of clusters in the study population, we calculated the exclusivity as the proportion of patients included in each cluster among all patients corresponding to each variable. After clustering, validation analysis was performed using the study sample that was reserved for the test set.
Statistical significance was set at P values of < 0.05, and all statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Data availability
Data are accessible from NHIS database, but the access to data used in this study is only available for the researchers who have applied for and have been granted. Further information is available in online homepage of National Health Insurance Sharing Service (https://nhiss.nhis.or.kr).
References
Payne, R. A. & Avery, A. J. Polypharmacy: One of the greatest prescribing challenges in general practice. Br. J. Gen. Pract. 61, 83–84 (2011).
Masnoon, N., Shakib, S., Kalisch-Ellett, L. & Caughey, G. E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 17, 230 (2017).
Molokhia, M. & Majeed, A. Current and future perspectives on the management of polypharmacy. BMC Fam. Pract. 18, 70 (2017).
Scott, I. A. et al. Reducing inappropriate polypharmacy: The process of deprescribing. JAMA Intern. Med. 175, 827–834 (2015).
Jokanovic, N., Tan, E. C., Dooley, M. J., Kirkpatrick, C. M. & Bell, J. S. Prevalence and factors associated with polypharmacy in long-term care facilities: A systematic review. J. Am. Med. Dir. Assoc. 16, 535.e1-535.e12 (2015).
Fau, P. H. et al. Prescribed drugs and polypharmacy in healthcare service users in South Korea: An analysis based on National Health Insurance claims data. Int. J. Clin. Pharmacol. Ther. 54, 369–377 (2016).
Kim, H. A., Shin, J. Y., Kim, M. H. & Park, B. J. Prevalence and predictors of polypharmacy among Korean elderly. PLoS ONE 9, e98043 (2014).
Maher, R. L., Hanlon, J. & Hajjar, E. R. Clinical consequences of polypharmacy in elderly. Expert Opin. Drug Saf. 13, 57–65 (2014).
Viktil, K. K., Blix, H. S., Moger, T. A. & Reikvam, A. Polypharmacy as commonly defined is an indicator of limited value in the assessment of drug-related problems. Br. J. Clin. Pharmacol. 63, 187–195 (2007).
Gurwitz, J. H. et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA 289, 1107–1116 (2003).
Picco, L. et al. Economic burden of multimorbidity among older adults: Impact on healthcare and societal costs. BMC Health Serv. Res. 16, 173 (2016).
Cahir, C. et al. Potentially inappropriate prescribing and cost outcomes for older people: A national population study. Br. J. Clin. Pharmacol. 69, 543–552 (2010).
WHO. WHO Global Patient Safety Challenge: Medication Without Harm (World Health Organization, Geneva, 2017).
McIntosh, J. et al. A case study of polypharmacy management in nine European countries: Implications for change management and implementation. PLoS ONE 13, e0195232 (2018).
Kua, C. H., Mak, V. S. L. & Huey, L. S. W. Health outcomes of deprescribing interventions among older residents in nursing homes: A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 20, 362-372.e11 (2019).
Bloomfield, H. E. et al. Deprescribing for community-dwelling older adults: A systematic review and meta-analysis. J. Gen. Intern. Med. 35, 3323–3332 (2020).
Page, A. T., Clifford, R. M., Potter, K., Schwartz, D. & Etherton-Beer, C. D. The feasibility and effect of deprescribing in older adults on mortality and health: A systematic review and meta-analysis. Br. J. Clin. Pharmacol. 82, 583–623 (2016).
Rollason, V. & Vogt, N. Reduction of polypharmacy in the elderly: A systematic review of the role of the pharmacist. Drugs Aging 20, 817–832 (2003).
Cadogan, C. A., Ryan, C. & Hughes, C. M. Appropriate polypharmacy and medicine safety: When many is not too many. Drug Saf. 39, 109–116 (2016).
Jang, T. A study on the Drug Prescription Status, Underlying Disease, and Prognosis of Polypharmacy Users Using Data from the National Health Insurance (National Health Insurance Service Ilsan Hospital, Goyang, 2019).
Seymour, C. W. et al. Derivation, validation, and potential treatment implications of novel clinical phenotypes for sepsis. JAMA 321, 2003–2017 (2019).
Fuente-Tomas, L. et al. Classification of patients with bipolar disorder using k-means clustering. PLoS ONE 14, e0210314 (2019).
Ahlqvist, E. et al. Novel subgroups of adult-onset diabetes and their association with outcomes: A data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol. 6, 361–369 (2018).
Violán, C. et al. Multimorbidity patterns with K-means nonhierarchical cluster analysis. BMC Fam. Pract. 19, 108 (2018).
Keats, M. R. et al. Burden of multimorbidity and polypharmacy among cancer survivors: A population-based nested case-control study. Support Care Cancer 29, 713–723 (2021).
Ishizaki, T. et al. Drug prescription patterns and factors associated with polypharmacy in >1 million older adults in Tokyo. Geriatr. Gerontol. Int. 20, 304–311 (2020).
Feng, X. et al. Prevalence and geographic variations of polypharmacy among West Virginia Medicaid beneficiaries. Ann. Pharmacother. 51, 981–989 (2017).
Shin, W. Y., Kim, C., Lee, S. Y., Lee, W. & Kim, J. H. Role of primary care and challenges for public–private cooperation during the coronavirus disease 2019 pandemic: An expert Delphi study in South Korea. Yonsei Med. J. 62, 660–669 (2021).
Bahk, J., Kang, H. Y. & Khang, Y. H. Trends in life expectancy among medical aid beneficiaries and National Health Insurance beneficiaries in Korea between 2004 and 2017. BMC Public Health 19, 1137 (2019).
Adam, L. et al. Rationale and design of OPtimising thERapy to prevent Avoidable hospital admissions in Multimorbid older people (OPERAM): A cluster randomised controlled trial. BMJ Open 9, e026769 (2019).
Muth, C. et al. Effectiveness of a complex intervention on prioritising multimedication in multimorbidity (primum) in primary care: Results of a pragmatic cluster randomised controlled trial. BMJ Open 8, e017740 (2018).
Mizokami, F. et al. Clinical medication review type III of polypharmacy reduced unplanned hospitalizations in older adults: A meta-analysis of randomized clinical trials. Geriatr. Gerontol. Int. 19, 1275–1281 (2019).
Airagnes, G., Pelissolo, A., Lavallée, M., Flament, M. & Limosin, F. Benzodiazepine misuse in the elderly: Risk factors, consequences, and management. Curr. Psychiatry Rep. 18, 89 (2016).
Haller, E., Watzke, B., Blozik, E., Rosemann, T. & Reich, O. Antidepressant prescription practice and related factors in Switzerland: A cross-sectional analysis of health claims data. BMC Psychiatry 19, 196 (2019).
Khawaja, M. N., Alhassan, E., Bilal, J., Jatwani, S. & Mehta, B. Medical overuse of therapies and diagnostics in rheumatology. Clin. Rheumatol. 40, 2087–2094 (2021).
Hungin, A. P. & Kean, W. F. Nonsteroidal anti-inflammatory drugs: Overused or underused in osteoarthritis?. Am. J. Med. 110, 8S-11S (2001).
Ahn, E. Introducing big data analysis using data from National Health Insurance Service. Korean J. Anesthesiol. 73, 205–211 (2020).
Gesicho, M. B., Were, M. C. & Babic, A. Evaluating performance of health care facilities at meeting HIV-indicator reporting requirements in Kenya: An application of K-means clustering algorithm. BMC Med. Inform. Decis. Mak. 21, 6 (2021).
Cheol-Seong, S. et al. Data resource profile: The National Health Information database of the National Health Insurance Service in South Korea. Int. J. Epidemiol. 46, 799–800 (2017).
Medical Service ACT. (Medical institutions). https://www.law.go.kr/LSW/lsInfoP.do?lsiSeq=215393&chrClsCd=010203&urlMode=engLsInfoR&viewCls=engLsInfoR#0000:article3.
Schäfer, I. et al. Reducing complexity: A visualization of multimorbidity by combining disease clusters and triads. BMC Public Health 14, 1285 (2014).
Acknowledgements
The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Health Insurance Service.
Funding
This study was supported and funded by the National Health Insurance Service (ref no. 2020-2-0006). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization: S.Y.L., W.L., J.L., and J.K.; Data curation: W.S., T.G., D.R.K., and S.K.; Formal analysis: W.S., T.G., and D.R.K.; Funding acquisition: J.K.; Investigation: All authors.; Methodology: T.G., D.R.K., W.L., J.L., and J.K.; Project administration: J.K.; Resources: W.S., T.G., D.R.K., and J.K.; Supervision: S.Y.L., W.L., and J.K.; Validation: S.Y.L. and W.L.; Visualization: W.S., T.G., S.K., J.L., and J.K.; Writing—original draft: W.S., T.G., and J.K.; Writing—review and editing: All authors.; Approval of final manuscript: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shin, Wy., Go, TH., Kang, D.R. et al. Patterns of patients with polypharmacy in adult population from Korea. Sci Rep 12, 18073 (2022). https://doi.org/10.1038/s41598-022-23032-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-23032-z
This article is cited by
-
Differences in healthcare service utilization in patients with polypharmacy according to their risk level by adjusted morbidity groups: a population-based cross-sectional study
Journal of Pharmaceutical Policy and Practice (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.