Abstract
The electrocardiogram (ECG) and cardiovascular magnetic resonance imaging (CMR) provide powerful prognostic information. The aim was to determine their relative prognostic value. Patients (n = 783) undergoing CMR and 12-lead ECG with a QRS duration < 120 ms were included. Prognosis scores for one-year event-free survival from hospitalization for heart failure or death were derived using continuous ECG or CMR measures, and multivariable logistic regression, and compared. Patients (median [interquartile range] age 55 [43–64] years, 44% female) had 155 events during 5.7 [4.4–6.6] years. The ECG prognosis score included (1) frontal plane QRS-T angle, and (2) heart rate corrected QT duration (QTc) (log-rank 55). The CMR prognosis score included (1) global longitudinal strain, and (2) extracellular volume fraction (log-rank 85). The combination of positive scores for both ECG and CMR yielded the highest prognostic value (log-rank 105). Multivariable analysis showed an association with outcomes for both the ECG prognosis score (log-rank 8.4, hazard ratio [95% confidence interval] 1.29 [1.09–1.54]) and the CMR prognosis score (log-rank 47, hazard ratio 1.90 [1.58–2.28]). An ECG prognosis score predicted outcomes independently of CMR. Combining the results of ECG and CMR using both prognosis scores improved the overall prognostic performance.
Similar content being viewed by others
Introduction
Prognostic information can be gleaned from both the electrocardiogram (ECG)1 and cardiovascular magnetic resonance imaging (CMR) measures of left ventricular (LV) mass2, cardiac function3, and myocardial tissue characterization4. However, the ECG and CMR provide potentially complementary information, and how these measures perform in relation to each other has not been studied head-to-head.
The ECG reflects the electrical activity of the heart, and the information present in the ECG may complement measures of cardiac structure and function. To study the prognostic performance, prognosis scores can be created from parameters that best predict outcome. We aimed to create separate prognosis scores for the ECG and CMR, respectively, and compare them with regards to ability to predict the combined end-point of hospitalization for heart failure or death. Furthermore, rather than generating scores based on attributing points to criteria fulfilling set thresholds (point-based scores), we sought to harness the statistical strength of continuous variables to create continuous scores ranging from 0 to 100% likelihood of an event. We also sought to compare our results to a recently published point-based ECG risk score5. The hypothesis of the study was that an ECG score could provide incremental prognostic information beyond CMR measures with known powerful prognostic performance.
Methods
Study patients
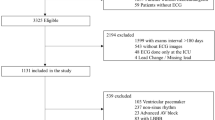
In this cross-sectional study, patients were identified from a prospectively acquired database of 1828 enrolled patients referred for a clinical CMR scan at University of Pittsburgh Medical Center (Pittsburgh, PA, USA) between 2008 and 2017, and followed until April 2018. The study was approved by the University of Pittsburgh Medical Center Institutional Review Board, and all participants provided written informed consent. All methods were carried out in accordance with relevant guidelines and regulations. Inclusion criteria were completion of a gadolinium-based contrast agent-enhanced CMR, and a digital ECG with sinus rhythm and a QRS duration < 120 ms acquired within 30 days of CMR.
Exclusion criteria were ECG confounders including complete right and left bundle branch blocks (RBBB, LBBB), atrial fibrillation or flutter, paced rhythm or other severe arrhythmia such as premature atrial or ventricular ectopy in bigeminy or trigeminy. A QRS duration < 120 ms was used to exclude RBBB and LBBB as these electrical conduction patterns cannot be compared to conduction in the absence of bundle branch block. Furthermore, complete bundle branch blocks are known to adversely affect prognosis6. ECG variables were otherwise not excluded based on their distribution. Further exclusion criteria included CMR findings of amyloidosis, hypertrophic cardiomyopathy, Takotsubo cardiomyopathy, congenital heart disease, siderosis, Fabry’s disease and poor CMR image quality. Hospitalization for first heart failure event after CMR was identified by medical record review using pre-defined criteria evaluated by a board-certified cardiologist, and mortality status was ascertained by medical record review and Social Security Death Index queries as previously described9.
Subgroups
From the database, 783 patients had an ECG within 30 days of CMR with a sinus rhythm and QRS duration < 120 ms and were included to create the ECG score. Among these, 730 patients had readily available CMR data including global longitudinal strain (GLS) and extracellular volume fraction (ECV), and were used to create the CMR score, and for prognosis calculations. For the ECG and CMR prognosis scores, respectively, patients were grouped as either having experienced an event of hospitalization for heart failure or death within one year of CMR, or no event.
CMR acquisition and analysis
CMR imaging methodology and typical acquisition parameters have previously been described10. In brief, CMR images were acquired using a 1.5 Tesla scanner, and LV mass, volumes, and ejection fraction were measured from short-axis stacks of end-systolic and end-diastolic cine images. ECV was calculated in basal and mid-ventricular myocardial short-axis slices in areas without focal late gadolinium enhancement (LGE), as described previously11. GLS analysis was performed using semi-automated tissue feature tracking software in end-diastole. For an extended description of CMR methodology, see the supplemental material.
The following CMR parameters were imputed into the CMR prognosis score analysis: GLS, LVEF, ECV, left ventricular end-diastolic volume indexed to body surface area (LVEDVI), left ventricular mass indexed to body surface area (LVMI), infarct size by LGE, and non-ischemic scar size by LGE.
ECG acquisition and analysis
Resting 12-lead ECG data for each subject was collected from the local ECG storage system (MUSE® Cardiology Information System, Version 8.0 SP2, GE Healthcare, IL, USA) and exported into anonymized xml files with coded identification. The xml files were analyzed digitally using previously described semi-automated software developed in-house8,12. The following ECG measures were included into the ECG prognosis score analysis: conventional ECG parameters including scalar durations, axes, and amplitudes; vectorcardiographic measures derived using Kors’ transform13 including spatial durations, axes, and amplitudes; and QRS-wave and T-wave complexity measures quantified using singular value decomposition8. The combination of the aforementioned ECG methods is referred to as Advanced-ECG (A-ECG). The conventional ECG risk score by Aro et al.5 (Aro ECG risk score), was also investigated, and defined as fulfillment of at least four of the following: heart rate > 75 bpm, QRS duration > 110 ms, QTc time > 450 ms in men and > 460 ms in women, Tpeak–Tend duration > 89 ms, frontal plane QRS-T angle > 90°, delayed QRS transition zone, electrocardiographic left ventricular hypertrophy (LVH), or a delayed intrinsicoid deflection.
Statistical analysis
Statistical analysis was performed in R (R Foundation for Statistical Computing, version 3.4.3, Vienna, Austria). Prognosis scores for one-year event-free survival were derived using multivariable stepwise forward logistic regression for variable selection. The event time of one year was chosen for investigation as it is at a time point when both a statistically and clinically meaningful number of events would have been observed. The area under the receiver operating curve (AUC) was bootstrapped 2000 times to obtain the 95% confidence intervals (CI). In order to avoid overfitting the score, one incremental parameter was considered appropriate for every ten events14. The ECG or CMR parameters, respectively, that yielded the highest AUC were chosen for the respective prognosis scores. The Youden index15 or, when not applicable, the point closest the top left in the AUC16, was used to determine the score cut-off that optimizes sensitivity and specificity for a given score. DeLong’s test was used to compare the AUC of ECG prognosis score to the Aro ECG risk score. The prognosis scores ranged from 0 to 100% and showed the likelihood of having an event as mathematically calculated from the logistic regression by:
The constants in the logistic regression equations for both the ECG and CMR scores were adjusted so that the optimal cut-offs for event risk were defined as a score ≥ 50% when all measures within the given score were handled as continuous rather than categorical. The prognosis scores were compared to each other with regards to survival free from hospitalization for heart failure or death using univariable and multivariable Cox regression, and Kaplan–Meier analysis. The chi-square (χ2) value was calculated to compare the effect of the estimates. Hazard ratios were reported with an increment of one standard deviation (SD) of the respective measures. Linear correlations were evaluated using Pearson’s correlation coefficient and expressed as its square (R2). Multivariable linear regression was performed without adjustments to investigate how CMR measures related to the ECG prognosis score. As antiarrhythmic medication can affect the ECG, and in particular prolong the QT, the ECG prognosis score was further tested in a sub-cohort of patients without antiarrhythmic medication. The Kolmogorov–Smirnov test was used to test if data were normally distributed, and differences between subgroups’ baseline data were tested using the Mann–Whitney U test or chi-square test, as appropriate. Data were described using median and interquartile range, or percentage, respectively. Furthermore, prediction models using logistic regression with a Ridge, Lasso, or Elastic Net penalty, respectively, as well as Cox regression with a Lasso penalty were also evaluated. A p-value < 0.05 was considered statistically significant.
Results
Baseline characteristics of the study population are presented in Table 1. A total of 783 patients with a CMR scan and an ECG with a QRS duration < 120 ms and without rhythm confounders were included in the study. All 783 patients were used to create the ECG score, and 730 patients were used to create the CMR score and for the survival analyses. The study patients experienced 155 events during 5.7 [4.4–6.6] years follow-up: 113 deaths (14.4%), 68 (8.7%) hospitalizations for heart failure, and 26 (3.3%) with both. In comparison to patients with no event, patients with an event were older, and had more CMR comorbidities and cardiovascular medications.
ECG prognosis score
The final ECG prognosis score for 1-year event included 1) the frontal plane QRS-T angle (degrees), and 2) the heart rate corrected (Bazett) QT duration (ms), and was calculated as:
The ECG prognosis score had an AUC (95% CI) of 0.78 (0.71–0.84), see Fig. 1, a sensitivity of 78% (67–89%) and a specificity of 71% (62–80%). The Frontal QRS-T angle and QTc were negligibly correlated (R2 = 0.06, p < 0.001). In multivariable linear regression analysis, the ECG prognosis score related to GLS, ECV, LVMI and infarct size (global R2 = 0.28, p < 0.001). An additional ECG score was also created with four ECG parameters, which was the maximum number that did not violate the rule of 10 events per variable. However, the more complex four-parameter ECG score did not add a clinically meaningful magnitude of incremental prognostic power, as shown in the supplemental material.
The prediction models using Cox regression, or logistic regression with a Ridge, Lasso, or Elastic Net penalty, respectively, did either not outperform multivariable stepwise forward logistic regression, or did not provide any clinically meaningful magnitude of improved diagnostic performance (results not shown).
CMR prognosis score
The final CMR prognosis score for 1-year event included 1) GLS (%), and 2) ECV (%), and was calculated as:
The CMR prognosis score had an AUC of 0.77 (0.69–0.84), see Fig. 1, a sensitivity of 79% (50–95%) and a specificity of 65% (46–92%). GLS and ECV were negligibly correlated (R2 = 0.05, p < 0.001).
Aro ECG risk score
Fifty-two patients (7%) out of the total study population, and 19 patients (12%) with an event had four or more abnormal parameters in the Aro ECG risk score. The Aro ECG risk score yielded an AUC of 0.65 (0.57–0.72), see Fig. 1, a sensitivity of 12% and a specificity of 93%. Univariable Cox showed an association with outcomes (χ2 14, HR 1.33 [1.14–1.55], p < 0.001). In the current study, the Aro ECG risk score had a lower AUC than the ECG prognosis score, p < 0.001.
ECG and CMR prognosis scores and outcomes
Table 2 summarizes the results for the Cox regression based on the 730 patients with readily available CMR data. Univariable Cox analysis showed that the CMR prognosis score had a higher univariable association with outcomes (χ2 93, HR 2.17 [1.85–2.54], p < 0.001) than the ECG prognosis score (χ2 58, HR 1.79 [1.54–2.08], p < 0.001). Multivariable Cox regression showed an association with outcomes for both the CMR prognosis score (χ2 47, p < 0.001) and the ECG prognosis score (χ2 8.4, p = 0.004), respectively. Kaplan Meier analysis showed that the combination of ≥ 50% for both the ECG (log-rank 55, p < 0.001) and the CMR prognosis score (log-rank 85, p < 0.001) yielded the highest prognostic value (log-rank 105, p < 0.001). For the event of hospitalization for heart failure only, or death only, respectively, the ECG prognosis score had a log-rank of 43, and log-rank of 31, respectively, p < 0.001 for both.
Figure 2 shows survival according to the ECG and CMR prognosis scores, respectively, and for patients with one normal but one increased score, or with both scores increased, using score probability greater than 50% as the cut-off. Figure 3 shows survival for the Aro ECG risk score (log-rank 15, p = 0.005), and the ECG (log-rank 64, p < 0.001) and CMR (log-rank 103, p < 0.001) prognosis scores, respectively, using score cut-offs at 25%, 50% and 75%.
Antiarrhythmic medication and outcomes
A total of 49 patients had antiarrhythmic medication, mainly amiodarone and sotalol. When evaluating the ECG score in a sub-cohort without patients on antiarrhythmic medication (n = 734), the ECG score performance was effectively unchanged with an AUC of 0.80 (0.74–0.86). Antiarrhythmic medication correlated with outcomes in univariable Cox regression, HR 1.80 (1.02–3.20), p = 0.04, but not in multivariable Cox regression analysis together with the ECG prognosis score, HR 0.50 (0.29–1.7), p = 0.09.
Discussion
The major finding of this study was that, in patients with a QRS duration < 120 ms, a new ECG prognosis score provided prognostic information beyond CMR measures with known powerful prognostic utility. Importantly, the combination of the ECG prognosis score and the CMR prognosis score provided the best risk stratification, and should preferentially be used in concert.
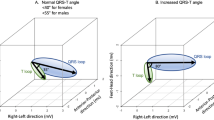
ECG measures and outcomes
The frontal plane QRS-T angle is the angle between the QRS axis and the T axis in the frontal plane. In a healthy heart, the angle between the QRS and T axis is small, whereas it increases as a result of myocardial pathology17, reflecting an abnormal dispersion between the depolarization and repolarization of the left ventricle18. Increased QRS-T angles are typically found in LVH, myocardial pacing, bundle branch blocks, and ischemia, and are a predictor of adverse events in patients with non-ischemic cardiomyopathy19. The QT duration spans the beginning of the depolarization until the end of the repolarization. A prolonged heart rate corrected QT time, QTc20, is associated with an increased risk of ventricular fibrillation and sudden death21.
The ECG holds more proven prognostic information than is usually considered, e.g. in the vectorcardiographic spatial QRS-T angle22,23, and more complex measures of the QRS-wave and T-wave24. However, the two-parameter ECG prognosis score from the current study did not include any such measure. It may be that such measures are associated with events over durations of time markedly shorter or longer than one year, since they are known to be associated with other specific cardiac diagnoses such as LVH, coronary artery disease, and LV systolic dysfunction8.
The Aro ECG risk score was constructed to predict sudden cardiac death, which may be why it had limited power in predicting the outcomes evaluated in the current study. Nevertheless, in the study by Aro, et al., 16% of all cases compared to 12% of the cases in the current study had four or more abnormal parameters. Furthermore, 3% of Aro et al.’s controls compared to 7% of the patients without events in the current study had a risk score of four or more abnormal parameters5. The control participants in Aro et al.'s study were individuals with no history of ventricular arrhythmias or cardiac arrest, whereas patients with no events in the current study where referred for a clinical CMR and are thus more likely to have cardiovascular disease. Besides, they may have had events prior to the cardiac scan (not investigated).
CMR measures and outcomes
Cardiovascular disease can lead to an increase in the myocardial extracellular space, consisting mainly of diffuse myocardial fibrosis, leading to systolic and diastolic dysfunction, and an increased risk of arrhythmia and mortality25. The prognostic utility of GLS has been shown to be superior to that of LVEF26,27. GLS can detect changes in myocardial contractility that may precede an abnormal LVEF28. This might help explain why LVEF did not have a multivariable association with the CMR prognosis score in the presence of GLS, even though there was a difference in LVEF between patients with versus without a one-year event. Previous studies have reported LVMI as an outcome predictor2. However, no difference in LVMI was found in our study between patients with versus without one-year events. Regarding ECV, myocardial diseases such as amyloidosis, hypertrophic cardiomyopathy, and Takotsubo cardiomyopathy were excluded due to their distinct impact on this measure29. However, other pathologies such as sarcoidosis and myocarditis were not excluded because they commonly result in focal myocardial inflammation or scarring analogous to ischemic scar or scars of other non-ischemic origins while having no impact on remote ECV29.
Prognosis scores
Clinical cardiovascular risk scores are often based on multivariable algorithms of parameters readily available in clinics, such as age, blood pressure, and presence of diabetes30. We used stepwise logistic regression to construct scores that estimate risk probabilities based on incorporation of continuous rather than dichotomous variables.
The benefits of doing this include reduced training and utilization times, and facilitation of data understanding31. Developing a score based on Cox regression using a continuous outcome variable did not improve the performance of the score, and thus the logistic regression score was used in the interest of having a parsimonious score. Both measures incorporated into our ECG score are also components of the Aro ECG risk score. However, in spite of the greater complexity of the Aro ECG risk score, with incorporation of multiple additional dichotomous measures, its AUC was 0.65 in this study, compared to 0.78 for the simpler ECG prognosis score.
ECG vs imaging for prognosis
The ECG has previously been compared to other imaging modalities with regards to prognosis, and found to have an incremental or independent prognostic power in, for instance, the setting of myocardial infarction with non-obstructed coronary arteries32, and LVH33. As the ECG and imaging provide different and complementary information, it is beneficial to assess both when possible.
Study limitations
This study had several limitations. The retrospective design introduces the risk of selection bias, even though the data were acquired prospectively. This was a single-center study that may not reflect the general population. Moreover, patients with notable ECG pathologies such as bundle branch blocks, and atrial fibrillation were also excluded given the already-known adverse prognoses associated with such conditions6,7, plus our desire to better preserve score generalizability in future groups of patients wherein the prevalence of such more severe ECG conditions might randomly differ. Thus, our scores are not currently applicable to such patients. On the other hand, patients with incomplete bundle branch block have an increased risk of progressing towards (complete) bundle brunch blocks34, but were not excluded. Right ventricular CMR data were readily available in only 184 patients and thus not investigated. Furthermore, the risk scores were derived and validated in the same cohort, as opposed to separate training and validation sub-cohorts which could impact the statistical robustness, and results can vary if sub-cohort are split differently35. To account for this, the results were confirmed using the resampling technique bootstrapping to obtain the variance in confidence intervals. Such an approach has been shown to be both robust and preferable in situations where the sample size may be limited35. Nevertheless, all parameters incorporated into the scores have had proven prognostic utility in previous studies.
We also investigated the composite outcome of hospitalization for heart failure and all-cause mortality, which may not necessarily be due to cardiac pathology. However, all hospitalization events were adjudicated according to strict criteria.
Clinical perspectives
The ECG and the parameters in the newly proposed ECG prognosis score might be readily numerically presented by most ECG vendors, making the ECG prognosis score a clinically accessible tool. Patients with a high score may benefit from more intensive risk management and surveillance, and future prospective studies are justified to evaluate such an approach. The ECG is less expensive and more available than CMR. However, the ECG and CMR convey independent and complementary prognostic information and should preferentially be combined when possible.
Conclusions
A new ECG prognosis score predicted outcomes independently of, and beyond, comprehensive CMR measures with known prognostic power. Combining the results of ECG and CMR using both prognosis scores improved overall prognostic utility.
Data availability
The datasets used and/or analyzed in current study are available from the corresponding author on reasonable request.
Abbreviations
- A-ECG:
-
Advanced electrocardiography
- CMR:
-
Cardiovascular magnetic resonance
- ECV:
-
Extracellular volume fraction
- GLS:
-
Global longitudinal strain
- LGE:
-
Late gadolinium enhancement
- LV:
-
Left ventricle
References
Aro, A. L. & Huikuri, H. V. Electrocardiographic predictors of sudden cardiac death from a large Finnish general population cohort. J. Electrocardiol. 46(5), 434–438 (2013).
Armstrong, A. C. et al. LV mass assessed by echocardiography and CMR, cardiovascular outcomes, and medical practice. JACC Cardiovasc. Imaging. 5(8), 837–848 (2012).
Kalam, K., Otahal, P. & Marwick, T. H. Prognostic implications of global LV dysfunction: A systematic review and meta-analysis of global longitudinal strain and ejection fraction. Heart 100(21), 1673–1680 (2014).
Schelbert, E. B. et al. Temporal relation between myocardial fibrosis and heart failure with preserved ejection fraction: Association with baseline disease severity and subsequent outcome. JAMA Cardiol. 2(9), 995–1006 (2017).
Aro, A. L. et al. Electrical risk score beyond the left ventricular ejection fraction: Prediction of sudden cardiac death in the Oregon Sudden Unexpected Death Study and the Atherosclerosis Risk in Communities Study. Eur. Heart J. 38(40), 3017–3025 (2017).
Zegard, A. et al. Prognosis of incidental left bundle branch block. Europace 22(6), 956–963 (2020).
Benjamin, E. J. et al. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation 98(10), 946–952 (1998).
Schlegel, T. T. et al. Accuracy of advanced versus strictly conventional 12-lead ECG for detection and screening of coronary artery disease, left ventricular hypertrophy and left ventricular systolic dysfunction. BMC Cardiovasc. Disord. 10, 28 (2010).
Schelbert, E. B. et al. Myocardial fibrosis quantified by extracellular volume is associated with subsequent hospitalization for heart failure, death, or both across the spectrum of ejection fraction and heart failure stage. J. Am. Heart Assoc. 4, 12 (2015).
Piehler, K. M. et al. Free-breathing, motion-corrected late gadolinium enhancement is robust and extends risk stratification to vulnerable patients. Circ. Cardiovasc. Imaging 6(3), 423–432 (2013).
Arheden, H. et al. Measurement of the distribution volume of gadopentetate dimeglumine at echo-planar MR imaging to quantify myocardial infarction: Comparison with 99mTc-DTPA autoradiography in rats. Radiology 211(3), 698–708 (1999).
Lindow, T., Palencia-Lamela, I., Schlegel, T. T. & Ugander, M. Heart age estimated using explainable advanced electrocardiography. Sci. Rep. 12(1), 9840 (2022).
Kors, J. A., van Herpen, G., Sittig, A. C. & van Bemmel, J. H. Reconstruction of the Frank vectorcardiogram from standard electrocardiographic leads: Diagnostic comparison of different methods. Eur. Heart J. 11(12), 1083–1092 (1990).
Peduzzi, P., Concato, J., Feinstein, A. R. & Holford, T. R. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J. Clin. Epidemiol. 48(12), 1503–1510 (1995).
Youden, W. Index for rating diagnostic tests. Cancer 3(1), 32–35 (1950).
Robin, X. et al. pROC: An open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. 12, 77 (2011).
Oehler, A., Feldman, T., Henrikson, C. A. & Tereshchenko, L. G. QRS-T angle: A review. Ann. Noninvasive Electrocardiol. 19(6), 534–542 (2014).
Voulgari, C., Pagoni, S., Tesfaye, S. & Tentolouris, N. The spatial QRS-T angle: Implications in clinical practice. Curr. Cardiol. Rev. 9(3), 197–210 (2013).
Pavri, B. B. et al. Prognostic value and temporal behavior of the planar QRS-T angle in patients with nonischemic cardiomyopathy. Circulation 117(25), 3181–3186 (2008).
Bazett, H. C. An analysis of the time-relations of electrocardiograms. Heart 7, 353 (1920).
Montanez, A., Ruskin, J. N., Hebert, P. R., Lamas, G. A. & Hennekens, C. H. Prolonged QTc interval and risks of total and cardiovascular mortality and sudden death in the general population: A review and qualitative overview of the prospective cohort studies. Arch. Intern Med. 164(9), 943–948 (2004).
Gleeson, S. et al. ECG-derived spatial QRS-T angle is associated with ICD implantation, mortality and heart failure admissions in patients with LV systolic dysfunction. PLoS ONE 12(3), e0171069 (2017).
Borleffs, C. J. et al. Predicting ventricular arrhythmias in patients with ischemic heart disease: Clinical application of the ECG-derived QRS-T angle. Circ. Arrhythm Electrophysiol. 2(5), 548–554 (2009).
Okin, P. M. et al. Repolarization abnormality for prediction of all-cause and cardiovascular mortality in American Indians: the Strong Heart Study. J. Cardiovasc. Electrophysiol. 16(9), 945–951 (2005).
Broberg, C. S., Chugh, S. S., Conklin, C., Sahn, D. J. & Jerosch-Herold, M. Quantification of diffuse myocardial fibrosis and its association with myocardial dysfunction in congenital heart disease. Circ. Cardiovasc. Imaging 3(6), 727–734 (2010).
Stanton, T., Leano, R. & Marwick, T. H. Prediction of all-cause mortality from global longitudinal speckle strain: Comparison with ejection fraction and wall motion scoring. Circ. Cardiovasc. Imaging 2(5), 356–364 (2009).
Fröjdh, F. et al. Extracellular volume and global longitudinal strain both associate with outcomes but correlate minimally. JACC Cardiovasc. Imaging 13(11), 2343–2354 (2020).
Ng, A. C. T. et al. Left ventricular global longitudinal strain is predictive of all-cause mortality independent of aortic stenosis severity and ejection fraction. Eur. Heart J. Cardiovasc. Imaging 19(8), 859–867 (2018).
Patel, A. R. & Kramer, C. M. Role of cardiac magnetic resonance in the diagnosis and prognosis of nonischemic cardiomyopathy. JACC Cardiovasc. Imaging 10(10), 1180–1193 (2017).
D’Agostino, R. B. et al. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation 117(6), 743–753 (2008).
Guyon, I. & Elisseeff, A. An introduction to variable and feature selection. J. Mach. Learn. Res. 3, 1157–1182 (2003).
Dastidar, A. G. et al. Prognostic role of cardiac MRI and conventional risk factors in myocardial infarction with nonobstructed coronary arteries. JACC Cardiovasc. Imaging 2019, 5 (2019).
Bacharova, L. et al. Determinants of discrepancies in detection and comparison of the prognostic significance of left ventricular hypertrophy by electrocardiogram and cardiac magnetic resonance imaging. Am. J. Cardiol. 115(4), 515–522 (2015).
Senesael, E. et al. Progression of incomplete toward complete left bundle branch block: A clinical and electrocardiographic analysis. Ann. Noninvasive Electrocardiol. 25(4), e12732 (2020).
Harrell, F.E. Regression Modeling Strategies. ULR https://hbiostat.org/doc/rms.pdf 178–184 (2022).
Acknowledgements
The authors acknowledge Daniel Loewenstein, MD, and Zak Loring, MD, for valuable discussions regarding the statistical analysis.
Funding
Open access funding provided by Karolinska Institute. The study was supported in part by grants from the Swedish Heart and Lung Foundation, the Swedish Research Council, Stockholm County Council, and Karolinska Institutet.
Author information
Authors and Affiliations
Contributions
M.M., T.T., E.S., and M.U. designed the study and drafted the manuscript. M.M., F.F., L.N., E.S., and M.U. participated in study design and CMR data acquisition and analysis. M.M., B.W., T.S., L.B., and M.U. participated in ECG data analysis. M.M., T.T., and M.U. performed the statistical analysis. All authors revised the manuscript critically for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
Dr. Schlegel is a principal of Nicollier-Schlegel SARL, a company that performs ECG research consultancy using the software used in the present study. Dr. Ugander is principal investigator on a research and development agreement regarding cardiovascular magnetic resonance between Siemens and Karolinska University Hospital. The remaining authors have nothing to disclose that is relevant to the contents of this paper.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maanja, M., Schlegel, T.T., Fröjdh, F. et al. An electrocardiography score predicts heart failure hospitalization or death beyond that of cardiovascular magnetic resonance imaging. Sci Rep 12, 18364 (2022). https://doi.org/10.1038/s41598-022-22501-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-22501-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.