Abstract
Nigeria like most developing nations still faced with a higher rate of short birth interval (SBI), and its associated consequences, such as adverse maternal and child health outcomes. This study aimed to determine the distribution and factors associated with SBI in rural and urban Nigeria. The data for this study were extracted from the 2018 Nigeria Demographic and Health Survey (2018 NDHS). Statistical analyses were descriptive analysis and binary logistic model. The proportions of SBI in rural and urban Nigeria were 20.7% and 20.3% respectively. Women’s age, geopolitical region, education level, and the number of children ever born were significantly associated with SBI in rural and urban Nigeria. Maternal Wealth index and antenatal care visits were only significant in rural while working status was only significant in urban Nigeria after controlling for other factors. Higher odds of SBI for middle class women than poor women (AOR = 1.19, 95% CI = 1.06–1.35), and increase in ANC visits reduces the odds of having SBI: 4–7 visits (AOR = 0.87, 95% CI = 0.77–0.98) and > 7visits (AOR = 0.83, 95% CI = 0.69–0.99). There were slight disparities in the prevalence of short birth intervals in rural and urban areas. Wealth index and ANC visits were only significant in rural Nigeria. Public health awareness campaigns should be strengthened to drive the importance of birth spacing techniques such as the utilization of modern contraceptives and breastfeeding in all the geo-political regions and across all age strata. Women particularly those residing in the rural areas should be encouraged to advance their education to at least a secondary level and enlightened on the importance of ANC.
Similar content being viewed by others
Introduction
Birth spacing, also known as an inter-birth interval (IBI), or inter-pregnancy interval refers to how soon after a prior pregnancy a woman becomes pregnant or gives birth again. Optimal birth spacing (defined as an inter-birth interval length of 24–59 months) is incontrovertibly linked to better health outcomes for both mothers and babies1,2,3. The World Health Organization (WHO) currently recommends an interval between the last live birth and the next pregnancy of at least 24 months4, and any birth less than this is considered a short birth interval (SBI). Short birth intervals lead to adverse maternal, perinatal, neonatal, and child health outcomes5,6. Short birth interval is associated with under-five mortality and low birth weight7,8. Globally, it is estimated that 25% of births still occur less than 24 months, and most of these births were observed in Central Asia (33%) and Sub-Saharan Africa (20%)9.
In Nigeria according to the 2018 Nigeria Demographic and Health Survey stood at 25% with a median birth interval of 30.9 months10. This suggests that Nigeria, like other developing nations, still is faced with a high rate of short birth intervals. Other African countries with similar rates include Rwanda: 20%, Uganda: 25.3%, Cameroon: 21.3% and Ethiopia: 24.9%, and these high rates were attributed to a lack of access to family planning options11. A study in Abuja, the capital city of Nigeria reported that 50% of women had birth to pregnancy intervals of fewer than 24 months, while 14 (3.5%) had birth to pregnancy intervals of greater than 60 months1. A similar study in Enugu, Nigeria also reported that the median inter-birth interval was 21.5 months2.
Few factors have been associated with birth intervals. Some of these are direct factors such as frequency of sexual activity, use of contraceptives, postpartum in fecundability, abortion, and sterility while indirect factors include socioeconomic and cultural factors12,13. Interbirth interval is also influenced by sociodemographic, economic, and birth history6. Fayehun et al. reported that the type of contraceptives used, living in rural or urban settings, wealth index, husbands’ occupation, and sex of preceding children determined birth intervals14. Having more female children and the last birth been a female significantly reduced birth intervals in the quest for a male child14. The use of contraceptives for birth spacing was also seen to be affected by male child preference where the last child is a female, a woman would like to use a short-acting contraceptive in order not to wait too long to get a male child6.
While adequate birth spacing is considered as a very significant factor for the health of women and their children11, inadequate birth spacing was rated as the highest risk faced by African women during pregnancy compared to other pregnancy-related outcomes15. Some studies in Nigeria and elsewhere have also shown a significant association between preceding birth intervals and under-five mortality16,17,18,19,20. However, studies on the determinants of the short birth interval using nationally representative data such as Nigeria Demographic and Health Survey (NDHS) are sparse in Nigeria. Existing studies were Hospital-based2,21,22,23, and each of them was only limited to the city or town in which the Hospital is located. This study bridged the gap by estimating the determinants of short birth intervals at the national level using NDHS data.
Given the above, it is important to gain a deeper understanding of the disparities existing among women living in rural and urban Nigerians in terms of interbirth interval. This study, therefore, aimed to determine the distribution and factors associated with short birth intervals in rural and urban Nigeria.
Methods
Data source
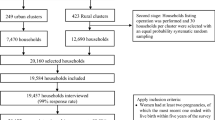
The data for this study were extracted from the 2018 Nigeria Demographic and Health Survey (NDHS) conducted by the National Population Commission (NPC) and ICF international. Being a national survey, it elicits information from women and men of reproductive age across the 36 states and the Federal Capital Territory (FCT) Abuja, nominated through a stratified two-stage cluster sampling technique. The NDHS, like other Demographic and Health Surveys (DHS) is conducted every five years in the consenting low- and middle-income countries.
Data
The data involved 41,821 women residing in rural and urban Nigeria, extracted from women data of 2018 NDHS.
Study variables
The outcome variable in this study was preceding birth interval which was recoded as < 24 months and ≥ 24 months. This is based on the definition of the World Health Organization4. The explanatory variables were sociodemographic and health care-seeking characteristics.
The explanatory variables and their categories were:
Mother’s age: < 20/20–29/30–39/ ≥ 40 years.
Child’s sex: Male/female.
Mother’s Religion: Christianity/Islam/Others.
Current Region of residence: North-central/North-east/ North-west/South-east/South-south/South-west.
Current place of residence: Urban/rural.
Mother’s educational level: None/primary/secondary/higher.
Marital status: Never married/married.
Employment status: Unemployed/employed.
Wealth index: Poor/middle/rich.
Number of children ever born: 0–2/ 3–4/ > 4.
Antenatal care visits: None/1–3/4–7/ > 7 visits.
Data analysis and statistical technique
We analyzed the data using univariate, bivariate and multivariate techniques. At the univariate level, proportion was used to describe the characteristics of the respondents; at the bivariate technique level, chi-square was utilized to assess the association between the characteristics and the birth interval; while binary logistic regression was fitted at the multivariate level to determine the influence of these factors on birth interval to explain the disparities in the birth interval between rural and urban women.
The outcome variable, the birth interval, was categorized and coded as (≥ 24 months = 0 and < 24 months = 1) and used in the logistic regression. Firstly, we described the characteristics. Secondly, we assessed the association between the explanatory variables and the birth interval; and lastly, only the significant variables were included in the multiple binary logistic regression model. Three logistic regression models were fitted for the study: the entire country, rural Nigeria, and urban Nigeria. To account for the complex nature of the DHS data, we adjusted for sampling weight, clustering, and stratification. The measure of associations was the odds ratio, and its statistical significance was assessed at 95% confidence interval excluding unit and P-value < 0.05. Analysis was arried out using Stata version 15.0 (StataCorp, College Station, TX)s.
The logistic regression model is expressed as:
where p is the probability of an event to occur (having a short birth interval) and 1-p is the probability of the event not occurring (not having a short birth interval), \(\frac{p}{1 - p}\) is the “odds” of occurrence of the event against its non-occurrence. \(\beta_{i}\) and \(X_{i}\) are the regression coefficient of the explanatory variables and the explanatory variables (sociodemographic factors) respectively; and \(\beta_{0}\) is the constant for the logistic regression model.
All methods were carried out in accordance with relevant guidelines and regulations. In addition, all experimental protocols and ethical approval were obtained from the National Health Research. Ethics Committee of Nigeria (NHREC) (ref. no. NHREC/01/01/2017). Written informed consent was obtained from all subjects and/or their legal guardian(s).
Results
The distributions of the characteristics and their association with birth interval are shown in Table 1. The results show that all factors are significantly associated with short birth intervals across Nigeria (P < 0.05), except the sex of the child (P = 0.749), and so was excluded in further analysis. The proportion of < 24 months and ≥ 24 months birth intervals were respectively 20.6% vs 79.4% for Nigeria, 20.3% vs 79.7% for urban Nigeria and 20.7% vs 79.3% for rural Nigeria, as shown in Fig. 1.
Table 2 shows the results of the analysis of association between birth interval and the women characteristics using logistic regression. The result indicates the impact of sociodemographic and health care related factors contributing to short birth interval in rural and urban Nigeria. The result indicated higher odds of short birth interval in rural areas (AOR = 1.16, 95% CI = 0.96–1.16) compared to urban areas, though not statistically significant. Analysis showed a significant decrease in odds of short birth interval with increased maternal age in Nigeria (20–29 years: AOR = 0.40, 95% CI = 0.34–0.47; 30–39 years: AOR = 0.22, 95% CI = 0.19–0.27; ≥ 40 years: AOR = 0.15, 95% CI = 0.11–0.19); and rural Nigeria (20–29 years: AOR = 0.39, 95% CI = 0.33–0.47; 30–39 years: AOR = 0.24, 95% CI = 0.19–0.30; ≥ 40 years: AOR = 0.15, 95% CI = 0.11–0.21) and urban areas (20–29 years: AOR = 0.37, 95% CI = 0.27–0.51; 30–39 years: AOR = 0.17, 95% CI = 0.11–0.23; ≥ 40 years: AOR = 0.10, 95% CI = 0.07–0.17).
There was significantly higher odds of having a short birth interval among rural women living in only the South-east (AOR = 2.09, 95% CI = 1.66–2.63) and South-south (AOR = 1.42, 95% CI = 1.15–1.76). While among women residing in the urban areas, living in the North-east (AOR = 1.41, 95% CI = 1.09–1.78), South-east (AOR = 1.75, 95% CI = 1.36–2.26) and South-south (AOR = 1.56, 95% CI = 1.16–2.08) were significantly more likely to have short birth interval compared with those living in the North-central; whereas living in south-west urban Nigeria was significantly less likely to have short birth interval compared with those living in the North-central (AOR = 0.75, 95% CI = 0.58–0.95).
Whereas women who had no formal education were 61% and 58% significantly higher odds of having short birth interval than women with higher education in urban Nigeria (AOR = 1.61, 95% CI = 1.19–2.19) and rural Nigeria (AOR = 1.58, 95% CI = 1.17–2.08) respectively. Furthermore, employed women residing in the rural areas had lower odds of having short birth interval than unemployed women (AOR = 0.95, 95% CI = 0.87–1.03), though not statistically significant. Whereas, in urban areas employed women had significantly lower odds of having short birth interval than unemployed women (AOR = 0.74, 95% CI = 0.67–0.84). Regarding the household wealth index, middle wealth index women living in rural areas were 1.19 times more likely to have short birth intervals compared to poor women (AOR = 1.19, 95% CI = 1.06–1.35). But in the urban areas, middle wealth index women had a lower odds of having short birth intervals than the poor women, though not statistically significant (AOR = 0.94, 95% CI = 0.74–1.18).
Women in rural Nigeria who have had three to four deliveries and above were less likely to have a short birth interval (AOR = 0.21, 95% CI = 0.03–0.37) and (AOR = 0.67, 95% CI = 0.42–0.96) respectively than those with two deliveries or less. In urban Nigerian only women who had more than 4 children were significantly less likely to have a short birth interval than women who had two children or fewer (AOR = 0.24, 95% CI = 0.22–0.29). But those who had 3–4 children had lower odds of having short birth intervals compared with women who had two children or less, though not statistically significant. Women who attended antenatal care at least four times during pregnancy had lower odds of having short birth intervals in only rural Nigeria than those who did not attend: Four to seven ANC visits (AOR = 0.87, 95% CI = 0.77–0.98) and more than seven ANC visits (AOR = 0.83, 95% CI = 0.69–0.99).
Discussion
This study was designed to assess short birth interval and its determinant with a focus on rural–urban variation in Nigeria. We defined a short birth interval as having another birth before 24 months of having a preceding birth. The overall prevalence of short birth intervals in Nigeria was 20.6%. While rural and urban areas of Nigeria were 20.7% and 20.3% respectively. This result is higher than the SBI reported in Rwanda, but lower compared to findings in some other African countries5,11 as well as in Brazil12. The observed differences could be attributed to the prevalent socio-geographical and cultural differences in the studied areas. These results indeed call for urgent action considering the adverse consequences of a short birth interval to mothers and children. Though all the variables were significantly associated with short birth intervals at the bivariate level, the multivariate analysis showed that maternal age at childbirth, geopolitical region, number of children ever born, and ANC visits were all statistically associated with short birth intervals. Although we found the sex of the child not be significant in the current study, the quest for male children or children in the Africa context, Nigeria inclusive, could affect birth interval among women.
While the educational level was significant in urban areas, the household wealth index was significantly associated with short birth intervals in rural areas at a multivariate level. Though, both variables were significant in Nigeria.
This study showed that the odds of having a short birth interval decrease as the mother’s age at birth of the child increases. In the other words, the odds of having the next child within 24 months is reduced as women get older, and this result agreed with previous studies3,24. Fecundity could be a possible explanation for this, as younger women are highly fecund than older women and the likelihood of younger women using contraceptives is less compared to older women because they have a high desire to bear children24. More so, younger women are likely to be less privileged and as such may not afford more birth spacing techniques compared to older women as shown in a study conducted in Finland25.
The study revealed that women residing in rural Nigeria were more likely to have short birth intervals compared with those residents in urban areas. This again substantiates the essence of this study, as it is believed that contributing factors to short birth interval is dependent on the place of residence, and as such could not be the same. This is consistent with reports of similar studies which indicate a relatively higher occurrence of short birth intervals in rural areas compared to urban areas14,26,27. This could be attributed to the relatively lower information on birth intervals and the nonavailability of modern contraceptives in rural areas compared to urban areas. Women who have information about short birth intervals through any media channel are expected to have a better understanding of the negative impact of short birth intervals on maternal and children’s health. As a result, women who have no exposure to any media are more likely to experience short birth intervals than those who have media exposure28,29.
Whereas all the zones in the country except North-west were associated with high odds of having a short birth interval at the national level and rural areas, only south-east and south-south were significantly associated with high odds of having short birth interval among urban residents. This could be because of the under-utilization of contraceptives in all the regions in rural and urban Nigeria by both men and women30.
The study also revealed that women that attended the WHO minimum of four antenatal care visits were less likely to have a short birth interval than those that attended less than the minimum visits in rural Nigeria. This is because ANC attendees have access to health education that explains the consequences of short birth intervals and information and materials that will enable them to prolong pregnancy to their desired time. Having more than two children was less likely to have a short birth interval than having less for women residing in both rural and urban areas of Nigeria. This is true because these women that had more children may have achieved their desired family size and may feel less pressure or be in less of a hurry to get pregnant again3.
This study has observed that Maternal education is protective of short birth intervals as an increase in educational attainment leads to a decrease in the likelihood of experiencing short birth intervals. This implies that educated women were more likely to have spaced births than non-educated women. This finding is consistent with other studies in Ethiopia and Pakistan31,32,33. The explanation might be attributed to the fact that better-educated women are more likely to use contraception to delay their inter-birth intervals and may also be exposed to more health education. Furthermore, there is a likelihood that literate women may be engaged in careers that are not well-suited to childbearing32,34.
The household wealth index was also identified as a significant determinant of short birth interval in rural Nigeria. This study revealed that the odds of experiencing short birth intervals were less common in households in the rich and middle wealth index than in the poor wealth index. This is consistent with studies carried out in Ethiopia, Saudi Arabia31,35. The possible explanation for this could be that privileged women may have more access to health care education and information and could afford health care services that apply logically enhanced short interbirth interval31. Furthermore, there was a disparity in the association between working status and short birth in rural and urban Nigeria. Whereas in urban areas, working-class women had significantly lower odds of having short birth interval, it was not significant in rural areas. The insignificance of working status in rural areas could be that in rural Nigeria it is difficult to distinguish between working and non-working women because all women are involved in one activity to other. The significant association between employment status to short birth interval found in this study was consistent with other studies done abroad36,37. The reason has been that working-class women can afford modern contraceptives that could be used to delay pregnancy to enable them to put in some months in their job after maternity leave. Married women have higher odds of experiencing short birth intervals than never-married women. The reason may be that married women are less likely to use contraceptives than never-married women38.
The major strength of this study was the fact that it utilized nationally representative data collected through standardized questionnaires and valid sampling procedures. While the limitation was on the ground that the design was cross-sectional which involves some missing information on reproductive indicators. Our findings should be interpreted with caution as we could not establish causation.
Conclusion
This study has demonstrated disparities in short birth interval in rural and urban Nigeria, by estimating prevalence and identifying factors influencing short birth intervals in these areas. There were slight disparities in the prevalence of short birth intervals in rural and urban areas. This is evident in the contributing factors as almost all the same factors such as maternal age at childbirth, geopolitical regions, educational attainment, and the number of children ever born were significantly associated with short birth intervals in both areas. It only differed in wealth index and the ANC visits for rural areas. Thus, policymakers and the relevant stakeholders should intensify existing strategies geared toward maintaining optimal birth spacing to ensure the well-being of mothers and children in rural and urban areas of Nigeria. Public health awareness campaigns should be strengthened to drive the importance of birth spacing techniques such as the utilization of modern contraceptives and breastfeeding in all the geo-political regions and across age strata. Finally, women, particularly in rural areas should be encouraged to advance their education to at least a secondary level and enlightened on the importance of ANC.
Data availability
The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.
References
Agida, T. E., Akaba, G. O., Ekele, B. A. & Isah, D. Practice of healthy timing and spacing of pregnancy (HSTP), experience from a low resource setting. Trop. J. Obstet. Gynaecol. 33(1), 57–63 (2016).
Dim, C. C., Ugwu, E. O. & Iloghalu, E. I. Duration and determinants of inter-birth interval among women in Enugu, south-eastern Nigeria. J. Obstet. Gynaecol. (Lahore) 33(2), 175–179. https://doi.org/10.3109/01443615.2012.747494 (2013).
De Jonge, H. C. et al. Determinants and consequences of short birth interval in rural Bangladesh: a cross-sectional study. BMC Pregnancy Childbirth 14(1), 427. https://doi.org/10.1186/s12884-014-0427-6 (2014).
Report of a WHO Technical Consultation on birth spacing. Geneva: WorldHealth Organization; 2005. Available at www.who.int/maternal_child_adolescent/.../birth_spacing05/en/. Accessed on August 2021.
Ajayi, A. I. & Somefun, O. D. Patterns and determinants of short and long birth intervals among women in selected sub-Saharan African countries. Medicine (Baltimore) 99(19), e20118 (2020).
Pimentel, J. et al. Factors associated with short birth interval in low- and middle-income countries: A systematic review. BMC Pregnancy Childbirth 20(1), 156. https://doi.org/10.1186/s12884-020-2852-z (2020).
Wegbom, A. I., Essi, I. D. & Kiri, V. A. Survival analysis of under-five mortality and its associated determinants in Nigeria: Evidence from a survey data. Int. J. Stat. Appl. 9(2), 59–66 (2019).
Wegbom, A. I., Edet, C. K. & Kiri, V. A. Prevalence, trends and predictors of small size babies in Nigeria: Analysis of data from two recent Nigeria demographic and health surveys. Int. J. Child Health Nutr. 9(3), 115–124 (2020).
Perin, J. & Walker, N. Potential confounding in the association between short birth intervals and increased neonatal, infant, and child mortality. Glob. Health Action 8(1), 29724. https://doi.org/10.3402/gha.v8.29724 (2015).
National Population Commission (NPC) [Nigeria] & ICF (2019). Nigeria Demographic and Health Survey 2018 Key Indicators Report. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF.
Gebrehiwot, S. W., Abera, G., Tesfay, K. & Tilahun, W. Short birth interval and associated factors among women of child bearing age in northern Ethiopia. BMC Womens Health 19, 85. https://doi.org/10.1186/s12905-019-0776-4 (2019).
Barbosa, R. et al. Factors Associated with Inadequate Birth Intervals in the BRISA Birth Cohort, Brazil Fatores associados a intervalos inadequados de nascimentos na coorte de nascimentos BRISA, Brasil. Rev. Bras. Ginecol. Obs. 42(2), 67–73 (2020).
Akinyemi, J. O., Odimegwu, C. O., Banjo, O. O. & Gbadebo, B. M. Clustering of infant deaths among Nigerian women: Investigation of temporal patterns using dynamic random effects model. Genus 75(1), 12. https://doi.org/10.1186/s41118-019-0058-x (2019).
Fayehun, O., Omololu, F. & Isiugo-Abanihe, U. Sex of preceding child and birth spacing among Nigerian ethnic groups. Afr. J. Reprod. Health 15, 79–89 (2011).
Schwandt, H. M., Skinner, J., Hebert, L. E., Cobb, L., Saad, A. & Odeku, M. Inadequate birth spacing is perceived as riskier than all family planning methods, except sterilization and abortion, in a qualitative study among urban Nigerians. BMC Womens Health 17(01), 80. https://doi.org/10.1186/s12905-017-0439-2
Akinyemi, J. O., Bamgboye, E. A. & Ayeni, O. New trends in under-five mortality determinants and their effects on child survival in Nigeria: A review of childhood mortality data from 1990–2008. Afr. Popul. Stud. 27(1), 25–42 (2013).
Wegbom, A. I., Wokoma, D. S. A., Nnoka, L. C. & Chibo, O. What explains the high rate of infant mortality in rural Nigeria: Biodemographic or socioeconomic factors?. Int. J. Health Sci. Res. 6(8), 317–323 (2016).
Adebowale, S. A., Morakinyo, O. M. & Ana, G. R. Housing materials as predictors of under-five mortality in Nigeria: Evidence from 2013 demographic and health survey. BMC Pediatr. 17, 30 (2017).
Getachew, Y. & Bekele, S. Survival analysis of under-five mortality of children and its associated risk factors in Ethiopia. J. Biosens. Bioelectron. 7(3), 1–10 (2016).
Berhanu, T. W. Socioeconomic, demographic, and environmental determinants of under-5 mortality in Ethiopia: Evidence from Ethiopian Demographic and Health Survey, 2016. Child Dev. Res. https://doi.org/10.1155/2019/1073782 (2019).
Bassey, G., Nyengidiki, T. K. & Dambo, N. D. Determinants of interpregnancy interval among parturient in Port Harcourt, Nigeria. Sahel Med. J. 19, 180–184 (2016).
Owonikoko, K. M., Adeniji, O., Oke, O. F., Fawole, A. A. & Adeniji, A. O. Determinants of interpregnancy interval in Ogbomosho: An unmet need for contraceptive usage. Int. J. Reprod. Contracept. Obstet. Gynecol. 4, 316–321 (2015).
Onubogu, C. U. & Ugochukwu, E. F. Inter-pregnancy interval and pregnancy outcomes among HIV positive mothers in Nnamdi Azikiwe University Teaching Hospital, Nnewi South-East Nigeria, Nigeria. J. Paediatr. 40(3), 264–269 (2013).
Shallo, S. A. & Gobena, T. Duration of birth interval and associated factors among married women in Dodota Woreda, Arsi Zone, Ethiopia. J. Health Educ. Res. Dev. 7, 292 (2019).
Berg, V., Miettinen, A., Jokela, M. & Rotkirch, A. Shorter birth intervals between siblings are associated with increased risk of parental divorce. PLoS ONE 15(1), 8237. https://doi.org/10.1371/journal.pone.0228237 (2020).
Nisha, M. K., Alam, A., Islam, M. T., Huda, T. & Raynes-Greenow, C. Risk of adverse pregnancy outcomes associated with short and long birth intervals in Bangladesh: Evidence from six Bangladesh Demographic and Health Surveys, 1996–2014. BMJ Open 9(2), 24392 (2019).
Molitoris, J., Barclay, K. & Kolk, M. When and where birth spacing matters for child survival: An international comparison using the DHS. Demography 56(4), 1349–1370 (2019).
Islam MZ, Islam MM, Rahman MM, Khan MN. Prevalence and risk factors of short birth interval in Bangladesh: Evidence from the linked data of population and health facility survey. medRxiv. https://doi.org/10.1101/2021.07.05.21259952v1
Damtie Y, Kefale B, Yalew M, Arefaynie M, Adane B. Short birth spacing and its association with maternal educational status, contraceptive use, and duration of breastfeeding in Ethiopia. A systematic review and meta-analysis. PLoS ONE 16(2), e0246348 (2021). https://doi.org/10.1371/journal.pone.0246348
Fayehun, F. Contraceptive use in Nigeria is incredibly low. A lack of knowledge may be why (2017). https://theconversation.com
Hailu, D. & Gulte, T. Determinants of short interbirth interval among reproductive age mothers in Arba Minch district, Ethiopia. Int. J. Reprod. Med. https://doi.org/10.1155/2016/6072437 (2016).
Begna, Z., Assegid, S., Kassahun, W. & Gerbaba, M. Determinants of inter birth interval among married women living in rural pastoral communities of southern Ethiopia: A case control study. BMC Pregnancy Childbirth 13, 116–121 (2013).
Asifa, K. & Muhammad, K. P. Determinants of higher order birth intervals in Pakistan. J. Stat. 19, 54–82 (2012).
ICPD & MDGs. Working as One Fifteen-Year Review of the Implementation of the ICPD PoA in Africa ICPD (2009). http://esaro.unfpa.org/webdav/site/africa/users/africa_admin/public/ICPD%2015%20Report.pdf.
Abdel-Fattah, M., Hifnawy, T., El-Said, T. I., Moharam, M. M. & Mahmoud, M. A. Determinants of birth spacing among Saudi women. J. Fam. Community Med. 14(3), 103–111 (2007).
Chernet, A. G., Shebeshi, D. S. & Banbeta, A. Determinant of time-to-first birth interval after marriage among Ethiopian women. BMC Womens Health 19, 157. https://doi.org/10.1186/s12905-019-0858-3 (2019).
Islam, M. S. Differential determinants of birth spacing since marriage to first live birth in rural Bangladesh. Pertanika J. Soc. Sci. Hum. 17(1), 1–6 (2009).
Wang, W., Sarah, S., Rebecca, W. & Courtney A. Women’s marital status, contraceptive use, and unmet need in Sub-Saharan Africa, Latin America, and the Caribbean. DHS Comparative Reports No. 44. Rockville, Maryland, USA: ICF (2017).
Author information
Authors and Affiliations
Contributions
A.W. and C.E. contributed to conception and study design. A.W., A.B., C.K.E., K.I.G., L.S. and A.F.F. authors performed the statistical analysis and interpretation of results and the drafting of the manuscripts. All authors reviewed the statistical analysis and revised the manuscript draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wegbom, A.I., Bademosi, A., Edet, C.K. et al. Rural–urban disparities in birth interval among women of reproductive age in Nigeria. Sci Rep 12, 17488 (2022). https://doi.org/10.1038/s41598-022-22142-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-22142-y
This article is cited by
-
Multilevel analysis of early resumption of sexual intercourse among postpartum women in sub-Saharan Africa: evidence from Demographic and Health Survey Data
BMC Public Health (2023)
-
Suboptimal birth spacing practice and its predictors among reproductive-age women in Sub-Saharan African countries: a multilevel mixed-effects modeling with robust Poisson regression
Reproductive Health (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.