Abstract
A discrepancy in subjective and objective estimations of sleep duration, which often diverge, could have long-term adverse effects on health outcomes in older adults. Using data from 2674 older adult men (≥ 65 years of age) of the Osteoporotic Fractures in Men Sleep Study, we assessed the longitudinal association between misperception index (MI), calculated as MI = (objective sleep duration – subjective sleep duration)/objective sleep duration, and all-cause mortality. During the follow-up with a mean (standard deviation) of 10.8 (4.2) years, 1596 deaths were observed. As a continuous variable, MI showed a linear relationship with all-cause mortality after adjusting for multiple covariates, including polysomnography-measured objective sleep duration [fully adjusted hazard ratio (HR), 0.69; 95% confidence interval [CI], 0.56–0.84]. As a categorical variable, the lowest MI quartile (vs. the interquartile MI range) was associated with increased mortality (fully adjusted HR, 1.28; 95% CI, 1.12–1.46), whereas the highest MI quartile was not associated with mortality (fully adjusted HR, 0.97; 95% CI, 0.85–1.11). The subjective overestimation of sleep duration may be a risk factor for all-cause mortality in older men. Future studies should examine why subjective overestimation of sleep duration is associated with all-cause mortality from a physiological perspective.
Similar content being viewed by others
Introduction
Older adults have higher prevalence rates of various sleep disorders, including insomnia1, sleep-related breathing2,3, and sleep-related movement disorders4, than other age groups. In addition, inadequate sleep in older adults is associated with an increased risk of developing physical ailments5,6,7, psychiatric disorders8,9,10, and all-cause mortality9,10,11. Therefore, it is a matter of public health to determine ways of optimizing their sleep schedules. While numerous epidemiological studies have relied on subjective measures of sleep duration (e.g., sleep logs or sleep-assessment questionnaires) to investigate various associations between sleep and health outcomes12,13,14,15,16,17,18, there are clear advantages to objective measures, which more accurately reflect the risk of physiological sleep loss. For example, studies using polysomnography (PSG), or actigraphy, have found evidence of frequent mismatches between subjective and objective sleep duration, especially in older adults19,20. Known as subjective–objective discrepancies in sleep duration, these mismatches may have important connotations for sleep physiology.
Such discrepancies are thought to fall along a single dimension ranging from subjective underestimation (subjective sleep duration < objective sleep duration) to subjective overestimation (subjective sleep duration > objective sleep duration)21; both extremes may impact longitudinal health outcomes. For example, subjective underestimation is considered a hallmark of insomnia, the most prominent phenotype of which is paradoxical insomnia, wherein extremely diminished subjective sleep duration is observed without any particular shortening of objective sleep duration22,23,24,25,26,27. Insomnia is of particular concern due to its associations with mental, metabolic, and cardiovascular diseases28,29. Similar physiological characteristics (e.g., cortical activity patterns during rapid eye movement sleep) that could be associated with adverse health outcomes in older adults30 have been reported in individuals with insomnia31 and underestimators of sleep duration in a general population16,32. However, while individuals with insomnia show a significant tendency to underestimate their sleep duration, they do not uniformly do so, and a significant portion of them rather overestimate than underestimate their sleep duration18,33,34, and the distribution of subjective–objective discrepancy resembles that of a general population35. This suggests that underestimation of sleep duration constitutes a distinct entity that involves both those with and without insomnia at large32 and could deteriorate health conditions through different physiological mechanisms in the general population. Thus, it is reasonable to assume that the subjective underestimation of sleep duration is associated with various adverse health outcomes in older adults.
At the other end of the spectrum, there is a lack of epidemiological and clinical knowledge on the subjective overestimation of sleep duration, although evidence suggests it may be associated with psychophysiological factors that are linked to poor health outcomes. Studies have shown that sleep overestimators have an increased propensity for both daytime sleep21,36 and decreased rapid eye movement (REM) activity32. In other research, individuals who reported sufficient amounts of sleep despite sleeping for short durations experienced less REM time than individuals who reported sufficient sleep amounts and objectively slept for long durations37,38. In sum, the literature suggests that overestimators tend to experience less REM sleep. In one case, an overestimator who reported sufficient subjective sleep continued to complain of daytime sleepiness and tiredness for a period lasting more than three years; contrary to the patient’s assumptions, objective measurements revealed short sleep durations and long periods of mid-sleep awakening36, both of which are associated with poor health outcomes14,17,18,39. Moreover, recent investigations have shown that low or “decreased percentage of REM sleep” is associated with a higher risk of all-cause mortality30,40. These findings suggest that subjective overestimations of sleep duration affect longitudinal health outcomes in relation to adverse changes in objective sleep variables that may become more evident in older adults (e.g., reduced sleep continuity and/or diminished REM sleep)41. Although there is scant evidence on gender differences in subjective–objective discrepancies in sleep duration, the subjective overestimation of sleep duration may be more directly influenced by physiological factors in men when compared to women. In a previous study, older men had better perception of their subjective sleep states when compared to older women, but had objectively worse sleep recordings, as evidenced by decreases in PSG-measured total sleep time, sleep efficiency, and the percentage of REM sleep42,43,44. Moreover, overestimation in men has been reported to be less closely associated with psychosocial factors than in women45. For older men, these findings indicate that the tendency to subjectively overestimate sleep despite possible objective deterioration is more directly linked to physiological factors than psychosocial factors. We therefore hypothesize that the subjective overestimation of sleep duration represents poorer current physiological conditions in older men, thus affecting their longitudinal health outcomes.
To test our hypothesis, we assessed longitudinal associations between subjective–objective discrepancies in sleep duration and all-cause mortality in a sample of older men, wherein data were obtained from the Osteoporotic Fractures in Men (MrOS) study46,47 and MrOS Sleep study48,49. In these cases, sleep was measured via both PSG (objective) and subjective perceptions. To assess the underestimation and overestimation of sleep duration, ratios (e.g. misperception index; MI)32,50,51 or differences (e.g. discrepancy index)21,36,45,52 between subjective and objective sleep duration have been utilized in previous studies. While the difference provides an absolute value of time duration and makes it easier to understand intuitively the degree of discrepancy, interindividual differences in sleep duration may influence the degree of discrepancy. To overcome this shortcoming of the discrepancy variables, we utilized the MI, calculated as [objective total sleep time (TST) minus subjective TST] divided by objective TST, which has been globally used as an indicator of subjective and objective discrepancy in sleep duration53,54.
Results
Sample characteristics
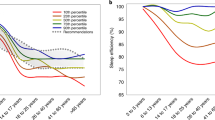
We analyzed a total of 2674 participants with a mean [standard deviation (SD)] age of 76.3 (5.5) years at baseline, followed-up for a mean (SD) of 10.8 (4.2) years. Mean (SD) objective sleep duration (objective total sleep time, oTST) and subjective sleep duration (subjective total sleep time, sTST) were 355.9 (69.0) and 371.9 (91.8) minutes, respectively, both normally distributed. Mean (SD) MI was − 0.07 (0.29), with normal distribution (Fig. 1A). Figure 1B shows correlations between sTST and oTST according to type.
MI details for all participants. (A) MI distribution across the sample; (B) correlations between subjective total sleep duration and objective total sleep duration for each MI group. Low MI is shown in blue (overestimators: Q1, MI ≤ −0.19, n = 678), intermediate MI is shown in green (normoestimators: IQR, −0.19 to < 0.08, n = 1350), and high MI is shown in red (underestimators: Q4, MI > 0.08, n = 646). IQR interquartile range, Q1 lowest quartile, Q4 highest quartile, MI misperception index.
Table 1 lists background, health status, and lifestyle information. The low MI group was older on average and had lower cognitive function and Physical Activity Scale for the Elderly (PASE) scores. Table 2 lists sleep characteristics. For objective assessments, the low MI group tended toward less REM sleep, shorter sleep times, longer sleep wake after sleep onset, shorter sleep efficiency, and more periodic limb movements (PLM); for subjective assessments, they had better sleep evaluations and longer sleep durations. Mean (SD) subjective–objective total sleep time difference was − 90.6 (60.3) in high MI group, 19.6 (27.4) in intermediate MI group, and 110.5 (46.2) in low MI group.
Associations between misperception index and all-cause mortality
A total of 1596 deaths (59.7%) were reported over a mean (SD) follow-up of 10.8 (4.2) years. The regression analyses with MI as a continuous variable consistently showed a linear relationship between MI and all-cause mortality; as MI increased, all-cause mortality decreased [fully adjusted hazard ratio (HR), 0.69; 95% confidence interval (CI), 0.56–0.84]. The regression analyses with MI as a categorical variable showed that low MI (overestimation) was consistently associated with higher mortality when compared to intermediate MI (fully adjusted HR, 1.28; 95% CI, 1.12–1.46), while no such association was found between low MI (underestimation) and mortality (fully adjusted HR, 0.97; 95%CI, 0.85–1.11) (Table 3; Fig. 2).
Sensitivity analysis
We conducted several sensitivity analyses to exclude other possible explanations for the association between MI and all-cause mortality. The sensitivity analyses with MI as a continuous variable consistently showed a linear relationship between increased MI and decreased all-cause mortality; that is, excluding death within two years (fully adjusted HR, 0.72; 95% CI, 0.58–0.89) (Table S1), apnea–hypopnea index scores greater than 30 (fully adjusted HR, 0.68; 95% CI, 0.53–0.85) (Table S2), sleeping pills, benzodiazepines, and/or antidepressants (fully adjusted HR, 0.68; 95% CI, 0.54–0.87) (Table S3), depression (fully adjusted HR, 0.74; 95% CI, 0.59–0.93) (Table S4), objectively short/long sleep durations (fully adjusted HR, 0.53; 95% CI, 0.35–0.82) (Table S5), PSG sleep ratings of extremely poor or better than normal (fully adjusted HR, 0.65; 95% CI, 0.50–0.85) (Table S6), and subjective sleep complaints (fully adjusted HR, 0.60; 95% CI, 0.42–0.85) (Table S7). Across the sensitivity analyses with MI as a categorical variable, low MI was consistently associated with higher mortality when compared to intermediate MI, while no such association was found between high MI and mortality (Tables S1-S7). With MI divided into quintiles, including Q’1 (≤ −0.23), Q’2 (−0.23 to ≤ −0.11), Q’3 (−0.11 to ≤ −0.01), Q’4 (−0.01 to ≤ 0.12), and Q’5 (> 0.12), the lowest quintile was significantly associated with higher mortality when compared to the intermediate quintile (Q’3) (fully adjusted HR, 1.29; 95% CI, 1.09–1.53) (Table S8).
Finally, the regression analyses with data supplemented via multiple imputation for missing values were consistent with MI, both in continuous and categorical form (Table S9).
Discussion
We found a negative association between MI and all-cause mortality in a longitudinal cohort of older men. After dividing participants into subgroups by quartiles/quintiles, those with low (vs. intermediate) MI (overestimation) showed consistent associations with increased mortality, while those with high MI (underestimation) did not, thus indicating an increased mortality risk among sleep overestimators. The observed associations between MI and mortality persisted through a series of sensitivity analyses, suggesting that MI influenced mortality independent of the end-of-life functional change, sleep apnea, sleeping pills, depression, objective long/short sleep duration, extreme dissatisfaction/satisfaction with sleep during PSG, and/or subjective sleep complaints. In sum, low MI (the overestimation of sleep duration) may indicate a higher risk of mortality in older men.
Following previous studies, MI was normally distributed in this sample, with the extremes representing the subjective underestimation and overestimation of sleep duration. Subjective–objective sleep discrepancies have primarily been investigated through studies on subjective underestimations of sleep duration in insomniacs, which therein constitutes a behavioral hallmark known as sleep state misperception22. For example, Mercer et al. found that individuals with insomnia underestimated total sleep while overestimating wake compared to good sleepers55. Similarly, Manconi et al. found that insomniacs tended to underestimate sleep times while healthy counterparts gave accurate estimates51. On the other hand, Attarian et al. reported on overestimated sleep durations in older adult women, conceptualizing this as “reverse” sleep state misperception, thus providing important clues for future research into subjective–objective discrepancies36. Trajanovic et al. proposed that such discrepancies spanned a continuum ranging from underestimation to overestimation21. Here, the subjective overestimation of sleep duration may represent a distinct condition that can appear in healthy individuals and insomniacs25,35,50,51,56. These findings support the idea that MI reaches both ends of the continuum, thus suggesting the clinical and epidemiological importance of subjective overestimations.
Low MI (the overestimation of sleep duration) was significantly associated with increased all-cause mortality, independent of objective sleep variables that were also associated with increased mortality. Several mechanisms are assumed to exist for this relationship. While physiological sleep need may decrease with age, there is no clear reduction in time in bed57, suggesting excessive time in bed relative to physiological sleep need in older adults. Epidemiological evidence suggests that objective longer time in bed is associated with higher total mortality in older adults independent of objective sleep duration per se17,58. In addition, there is evidence linking objective long time in bed and self-reported long sleep duration59. Thus, overestimation could be associated with mortality through such discrepancy between physiological and behavioral (hygienic) sleep durations.
Moreover, overestimators may have several objectively poor sleep states, which may lead to increased mortality particularly via cardiovascular disease. First, it has been suggested that in the general population, overestimation of sleep duration is associated with decreased REM activity32, increased severity of obstructive sleep apnea60, and decreased sleep efficiency34. Meanwhile, in patients with sleep disorders, it has been suggested that the mean sleep latency in the multiple sleep latency test was significantly shorter in overestimators21 and the frequency of PLM was higher in the overestimators with insomnia50. Consistent with a range of previous reports, the low MI group showed comparatively lower rates of REM sleep, shorter sleep durations, lower sleep efficiency, and more PLM in the present sample. Furthermore, these objective factors have been reported to be associated with all-cause mortality. Objectively shorter sleep duration61, lower rates of REM sleep30, and more PLM62 have been associated with cardiovascular mortality, and higher AHI63 has been associated with cardiovascular and cerebrovascular mortality. Although the present study does not allow clarification of the causal mechanisms of the observed association, it is speculated that these physiological changes (e.g., decreased REM rate and sleep efficiency) may occur in the background in overestimators, leading to increased total mortality. Further physiological studies are needed to elucidate the mechanisms that underly overestimation of sleep duration in the general population in more detail. Unveiling the underlying mechanisms may further allow the chance to test whether a certain intervention to optimize the perception of sleep duration reduces mortality in the epidemiological setting.
Contrary to our hypothesis, the subjective underestimation of sleep duration was not associated with an increased risk of mortality. It is possible that underestimation of sleep duration was not associated with an increased risk of all-cause mortality because the underestimators in this study did not fully reflect the underestimators in the previous study. First, we did not analyze any data from older women, who appear more likely to complain of subjective sleep disturbances even when their objective sleep states are better than those of older men42,43,44. Thus, older women with high MI may experience more subjective sleep disturbances, which is suggestive of insomnia. Therefore, our null findings on the relationship between high MI and mortality may have differed if older women were included. This negative finding may also be attributable to the nonclinical characteristics of sleep abnormalities in the current sample. Clearly, the high MI group did not wholly represent chronic insomnia, as its members did not necessarily have sleep difficulties. Moreover, the definition for subjectively underestimated sleep duration is not confined to the context of chronic insomnia. Indeed, a previous review reported that underestimation was associated with other health problems, including depression and irritable bowel syndrome24. However, there is scant evidence that paradoxical insomnia, which can be a form of chronic insomnia that can be characterized by extremely high MI25, is independently associated with poor long-term health outcomes. Meanwhile, in examining the relationship between underestimation and poor health outcomes, it is also necessary to examine the mechanisms that cause underestimation. As objective factors involved in high MI, NREM and REM activity have been shown to be higher in the extreme underestimation group in the general population32. However, in the present study, there was no clear trend toward lower REM% in the low subject-object ratio group compared to the intermediate estimation group. Other findings in the general population are scant, but in their findings on insomnia, Parrino et al. reported higher arousal index in paradoxical insomniacs with extreme underestimation compared to healthy controls64. Furthermore, sleep duration underestimation is also important for mental health status, and is thought to be common in depression65 and insomnia35. Fernandez-Mendoza et al. also suggested that the insomnia underestimation group showed higher scores in depression and anxiety scales34. In the present study, in the general population, the underestimator group had a higher arousal index and slightly higher scores on the Geriatric Depression Scale (GDS) and Pittsburgh Sleep Quality Index (PSQI) than the intermediate estimator group. This is consistent with previous studies and may be associated with underestimation. Future studies should investigate the association between high MI and health outcomes and background physiological mechanism, particularly in individuals with chronic insomnia disorder as well as those without insomnia in the general older adult population.
Strengths and limitations
This study investigated a large prospective cohort using a combination of validated objective/subjective sleep variables and PSG. Moreover, our results remained robust after adjusting for multiple confounders and conducting sensitivity analyses. However, there were also some limitations. First, the majority of participants were older Caucasians with preserved activities of daily living registered from the community, which limits generalizability. There may also be residual confounding factors such as sex, especially considering that older men and women may have different sociological background factors that are associated with the overestimation of sleep duration45. Second, we cannot completely exclude the influence of the first-night effect on both the objective and subjective estimation of sleep duration66,67,68, although this does not always occur with single-night PSG69. Further, reports involving consecutive PSG nights suggest that objective sleep duration does not always change significantly across recordings70. We also controlled for the effects of subjective sleep wellness on the PSG night as a covariate in the survival group, thus finding consistent results; our findings do not appear problematized by the first-night effect. Although further investigations are needed in other samples to determine the long-term adverse effects of subjective and objective discrepancy in sleep duration on health outcomes, this cohort study found an association between the subjective overestimation of sleep duration and all-cause mortality, thus positioning MI as an important determinant of longitudinal health outcomes in a sample of older men. Moreover, these findings challenge the efficacy of approaches that rely on basic sleep duration as a measure for improving public health.
Methods
Participants
As a community-based longitudinal observational investigation, the MrOS study was conducted among 5,994 participants from six centers in the United States between 2000 and 2002. All participants were at least 65 years of age and could walk independently. The study details have been previously published46,47. Of those participants, 3135 engaged in the ancillary MrOS Sleep study between 2003 and 2005, which included a comprehensive sleep assessment with in-home PSG recordings48,49. However, 224 had missing PSG data (i.e., 179 with no PSG recordings and 45 who failed to record PSG), which resulted in 2911 valid observations. In this study, we only included participants with verified survival or known causes of death through August 2019, which reduced the sample to 2675 subjects. Finally, one participant did not have data on subjective sleep time from the morning survey, which ultimately reduced the analyzed sample to 2674 subjects (Fig. S1). All analyzed data (including vital data) are available on the Internet, from both the National Sleep Research Resource website (http://sleepdata.org. [November 20, 2019])40 and MrOS online (https://mrosdata.sfcc-cpmc.net. [April 2, 2020]). For the MrOS study, ethical approval was obtained from the relevant local institutional review boards and all participants provided informed consent. The current study was approved by the Ethics Committee of the National Center of Neurology and Psychiatry, Tokyo, Japan and conducted in line with the principles of the Declaration of Helsinki.
Measures
Objective sleep duration
An unattended, portable in-home PSG (Safiro, Compumedics, Inc., Melbourne, Australia) was recorded at baseline, with scoring based on the American Academy of Sleep Medicine rules71. Standard PSG characteristics were also assessed48,49. We defined PSG-measured total sleep time as oTST.
Subjective sleep duration
Following the night of their in-home PSG recordings, participants completed a morning survey, which asked “How much time do you think you actually slept last night?” to rate their subjective sleep duration in terms of the number of perceived hours and minutes achieved (sTST). Subjective responses to PSG recordings were evaluated via morning surveys in which participants evaluated their preceding night’s sleep along a 5-point scale ranging from “poor = 1” to “good = 5” (compared to habitual sleep).
Primary exposure
The primary exposures were the overestimation and underestimation of sleep duration, as compared to the intermediate estimation of sleep duration. As a measure of subjective–objective discrepancy in sleep duration, we used the misperception index, calculated as MI = (objective sleep duration – subjective sleep duration)/objective sleep duration, as continuous variable. In addition, we divided MI into three groups using quartiles, therein defining the lowest (Q1 ≤ −0.19) and highest MI quartiles (Q4 > 0.08) as high MI (underestimation) and low MI (overestimation), respectively; the interquartile range of MI (IQR; Q2–Q3, −0.19 to ≤ 0.08) served as the reference category (normal estimation). Participants with high MI (Q4 > 0.08) and low MI (Q1 ≤ −0.19) were considered underestimators and overestimators, respectively, while those with intermediate MI (IQR) were considered normoestimators.
Mortality outcome
Participants or their next of kin were contacted every four months after baseline to confirm survival30. Reported deaths were validated via death certificates46,47.
Other covariates
Participants reported a variety of baseline characteristics through self-administered questionnaires, interviews, and clinical examinations. Specific items included education, race/ethnicity, body mass index (BMI), smoking history, daily caffeine intake, and alcohol consumption. Medication use and medical history were assessed via questionnaire; medications included antidepressants, sleeping pills, and benzodiazepines that may affect sleep/sleep structure, while medical history included clinically diagnosed hypertension, stroke, myocardial infarction, transient ischemic attack, heart failure, type 2 diabetes, and chronic obstructive pulmonary disease (COPD). In addition, participants completed the 15-item GDS72, Modified Mini-Mental State Examination73, and PASE74. Self-administered sleep questionnaires included the Epworth Sleepiness Scale75, and PSQI76. Circadian sleep timing was evaluated based on PSQI-derived habitual bed times and wake-up times over the previous month77,78,79.
Statistical analysis
Of the 2674 participants, 81 (3.03%) had missing values. We first conducted analyses in complete cases, then compared the results with those of the multiple assignment method. We used Cox proportional hazard models to evaluate the longitudinal associations between high MI (underestimation) or low MI (overestimation) and all-cause mortality. We first assessed MI as a continuous variable, since no categorical definitions were provided for the underestimation or overestimation of PSG-measured total sleep time. We then assessed MI as a categorical variable, therein defining the lowest (Q1 ≤ −0.19) and highest MI quartiles (Q4 > 0.08) as low MI (overestimation) and high MI (underestimation), respectively; the interquartile range of MI (IQR; Q2–Q3, −0.19 to ≤ 0.08) served as the reference category (normal estimation).
Cox models were run in the unadjusted model, age-adjusted model, and other two models (Model 1 and Model 2) using known covariates for adverse health outcomes. For Model 1, we used demographic covariates, including age, race/ethnicity, education, BMI, smoking status, alcohol, caffeine, medication use (sleeping pills, benzodiazepine, and/or antidepressants), and study sites. For Model 2, adding to Model 1 variables, we used health and sleep covariates, including circadian sleep timing (habitual bed times and wake-up times), Epworth Sleepiness Scale scores, PSQI score33,34, Teng Modified Mini-Mental State Examination scores, PASE scores, Geriatric Depression Scale scores, history of congestive heart failure, COPD, diabetes, hypertension, heart attack, and stroke, and PSG variables, including the overall arousal index, percentage of sleep time oxygen saturation below 80%, percentages of Stage N2, Stage REM%, wake after sleep onset, total sleep time, PLM index, and apnea–hypopnea index30; we also included the percentage of Stage N3, which may affect the perception of sleep duration32,80, and subjective sleep wellness on the PSG night81. The results were presented as HRs with 95% CIs. The proportional hazards assumptions were assessed using log minus log survival curve. All analyses were performed using SPSS Statistics, version 23 (IBM Japan, Tokyo), with significance set at a standard two-sided level of 5%.
Sensitivity analysis
We conducted several analyses to exclude other possible explanations for the association between MI and all-cause mortality. First, participants with deaths within two years were excluded82,83,84. Second, participants with apnea–hypopnea index scores greater than 30 were excluded. Third, participants who used sleeping pills, benzodiazepines, and/or antidepressants were excluded. Fourth, depressed participants were excluded (i.e., Geriatric Depression Scale scores > 4 or antidepressant use). Fifth, the confounding effects of objectively short and long sleep durations were excluded, as represented by the lowest and highest quartiles, respectively (objective total sleep time < 317.0 min or ≥ 400.0 min from polysomnography). Sixth, participants who rated their sleep during PSG as extremely poor or far better than normal were excluded, as either rating may represent excessive responses to monitoring. Seventh, participants who complained of sleep disturbance (i.e., PSQI scores ≥ 6) were excluded so that the sample being examined was free from sleep complaints. To ensure that the association between MI and mortality did not solely depend on the definitions for high/low MI, we conducted another sensitivity analysis with MI as a categorical variable (quintiles).
Finally, we evaluated missing values. As such instances were considered random, we created 20 datasets and assigned missing values via the multiple assignment method, mainly using the chain method85,86. We then compared these results with those from the complete case analysis86.
Data availability
The data analyzed in this article are available through the National Sleep Research Resource website (http://sleepdata.org) and MrOS online (https://mrosonline.ucsf.edu).
References
Ohayon, M. M. Epidemiology of insomnia: What we know and what we still need to learn. Sleep Med. Rev. 6, 97–111. https://doi.org/10.1053/smrv.2002.0186 (2002).
Young, T. et al. Predictors of sleep-disordered breathing in community-dwelling adults: The Sleep Heart Health Study. Arch. Intern. Med. 162, 893–900. https://doi.org/10.1001/archinte.162.8.893 (2002).
Young, T., Peppard, P. E. & Gottlieb, D. J. Epidemiology of obstructive sleep apnea: A population health perspective. Am. J. Respir. Crit. Care Med. 165, 1217–1239. https://doi.org/10.1164/rccm.2109080 (2002).
Iranzo, A. Parasomnias and sleep-related movement disorders in older adults. Sleep Med. Clin. 13, 51–61. https://doi.org/10.1016/j.jsmc.2017.09.005 (2018).
Nakakubo, S. et al. Sleep duration and progression to sarcopenia in Japanese community-dwelling older adults: A 4 year longitudinal study. J. Cachexia Sarcopenia Muscle. 12, 1034–1041. https://doi.org/10.1002/jcsm.12735 (2021).
Garfield, V., Llewellyn, C. H., Steptoe, A. & Kumari, M. Investigating the bidirectional associations of adiposity with sleep duration in older adults: The English Longitudinal Study of Ageing (ELSA). Sci. Rep. 7, 40250. https://doi.org/10.1038/srep40250 (2017).
Eguchi, K., Hoshide, S., Ishikawa, S., Shimada, K. & Kario, K. Short sleep duration is an independent predictor of stroke events in elderly hypertensive patients. J. Am. Soc. Hypertens. 4, 255–262. https://doi.org/10.1016/j.jash.2010.09.001 (2010).
Jackowska, M. & Poole, L. Sleep problems, short sleep and a combination of both increase the risk of depressive symptoms in older people: A 6-year follow-up investigation from the English Longitudinal Study of Ageing. Sleep Med. 37, 60–65. https://doi.org/10.1016/j.sleep.2017.02.004 (2017).
Ohara, T. et al. Association between daily sleep duration and risk of dementia and mortality in a Japanese community. J. Am. Geriatr. Soc. 66, 1911–1918. https://doi.org/10.1111/jgs.15446 (2018).
Robbins, R. et al. Examining sleep deficiency and disturbance and their risk for incident dementia and all-cause mortality in older adults across 5 years in the United States. Aging (Albany NY). 13, 3254–3268. https://doi.org/10.18632/aging.202591 (2021).
He, M., Deng, X., Zhu, Y., Huan, L. & Niu, W. The relationship between sleep duration and all-cause mortality in the older people: An updated and dose-response meta-analysis. BMC Public Health 20, 1179. https://doi.org/10.1186/s12889-020-09275-3 (2020).
Itani, O., Jike, M., Watanabe, N. & Kaneita, Y. Short sleep duration and health outcomes: A systematic review, meta-analysis, and meta-regression. Sleep Med. 32, 246–256. https://doi.org/10.1016/j.sleep.2016.08.006 (2017).
Jike, M., Itani, O., Watanabe, N., Buysse, D. J. & Kaneita, Y. Long sleep duration and health outcomes: A systematic review, meta-analysis and meta-regression. Sleep Med. Rev. 39, 25–36. https://doi.org/10.1016/j.smrv.2017.06.011 (2018).
Bertisch, S. M. et al. Insomnia with objective short sleep duration and risk of incident cardiovascular disease and all-cause mortality: Sleep Heart Health Study. Sleep https://doi.org/10.1093/sleep/zsy047 (2018).
Fernandez-Mendoza, J., He, F., Vgontzas, A. N., Liao, D. & Bixler, E. O. Interplay of objective sleep duration and cardiovascular and cerebrovascular diseases on cause-specific mortality. J. Am. Heart Assoc. 8, e013043. https://doi.org/10.1161/jaha.119.013043 (2019).
Li, Y. et al. Association between total sleep time and all cancer mortality: Non-linear dose-response meta-analysis of cohort studies. Sleep Med. 60, 211–218. https://doi.org/10.1016/j.sleep.2019.03.026 (2019).
Kripke, D. F., Langer, R. D., Elliott, J. A., Klauber, M. R. & Rex, K. M. Mortality related to actigraphic long and short sleep. Sleep Med. 12, 28–33. https://doi.org/10.1016/j.sleep.2010.04.016 (2011).
Vgontzas, A. N. et al. Insomnia with short sleep duration and mortality: The Penn State cohort. Sleep 33, 1159–1164. https://doi.org/10.1093/sleep/33.9.1159 (2010).
McCrae, C. S. et al. Sleep complaints, subjective and objective sleep patterns, health, psychological adjustment, and daytime functioning in community-dwelling older adults. J. Gerontol. B. 60, P182–P189. https://doi.org/10.1093/geronb/60.4.P182 (2005).
Williams, J. M., Kay, D. B., Rowe, M. & McCrae, C. S. Sleep discrepancy, sleep complaint, and poor sleep among older adults. J. Gerontol. B. Psychol. Sci. Soc. Sci. 68, 712–720. https://doi.org/10.1093/geronb/gbt030 (2013).
Trajanovic, N. N., Radivojevic, V., Kaushansky, Y. & Shapiro, C. M. Positive sleep state misperception—A new concept of sleep misperception. Sleep Med. 8, 111–118. https://doi.org/10.1016/j.sleep.2006.08.013 (2007).
Harvey, A. G. & Tang, N. K. (Mis)perception of sleep in insomnia: A puzzle and a resolution. Psychol. Bull. 138, 77–101. https://doi.org/10.1037/a0025730 (2012).
Nishikawa, K. et al. Effects of cognitive behavioral therapy for insomnia on subjective-objective sleep discrepancy in patients with primary insomnia: A small-scale cohort pilot study. Int. J. Behav. Med. 28, 715–726. https://doi.org/10.1007/s12529-021-09969-x (2021).
Rezaie, L., Fobian, A. D., McCall, W. V. & Khazaie, H. Paradoxical insomnia and subjective-objective sleep discrepancy: A review. Sleep Med. Rev. 40, 196–202. https://doi.org/10.1016/j.smrv.2018.01.002 (2018).
Castelnovo, A. et al. The paradox of paradoxical insomnia: A theoretical review towards a unifying evidence-based definition. Sleep Med. Rev. 44, 70–82. https://doi.org/10.1016/j.smrv.2018.12.007 (2019).
Rezaie, L., Vakili-Amini, Y., Paschall, E. & Khazaie, H. Personality profiles in paradoxical insomnia: A case–control study. Sleep Sci. 13, 242–248. https://doi.org/10.5935/1984-0063.20190148 (2020).
Feige, B. et al. Event-related potentials in insomnia reflect altered perception of sleep. Sleep https://doi.org/10.1093/sleep/zsab137 (2021).
Lin, C. L., Chien, W. C., Chung, C. H. & Wu, F. L. Risk of type 2 diabetes in patients with insomnia: A population-based historical cohort study. Diabetes Metab. Res. Rev. https://doi.org/10.1002/dmrr.2930 (2018).
Khan, M. S. & Aouad, R. The effects of insomnia and sleep loss on cardiovascular disease. Sleep Med. Clin. 12, 167–177. https://doi.org/10.1016/j.jsmc.2017.01.005 (2017).
Leary, E. B. et al. Association of rapid eye movement sleep with mortality in middle-aged and older adults. JAMA Neurol. 77, 1241–1251. https://doi.org/10.1001/jamaneurol.2020.2108 (2020).
Zhao, W. et al. EEG spectral analysis in insomnia disorder: A systematic review and meta-analysis. Sleep Med. Rev. 59, 101457. https://doi.org/10.1016/j.smrv.2021.101457 (2021).
Lecci, S. et al. Electroencephalographic changes associated with subjective under- and overestimation of sleep duration. Sleep https://doi.org/10.1093/sleep/zsaa094 (2020).
Fernandez-Mendoza, J. et al. Insomnia with objective short sleep duration is associated with deficits in neuropsychological performance: A general population study. Sleep 33, 459–465. https://doi.org/10.1093/sleep/33.4.459 (2010).
Fernandez-Mendoza, J. et al. Sleep misperception and chronic insomnia in the general population: Role of objective sleep duration and psychological profiles. Psychosom. Med. 73, 88–97. https://doi.org/10.1097/PSY.0b013e3181fe365a (2011).
Means, M. K., Edinger, J. D., Glenn, D. M. & Fins, A. I. Accuracy of sleep perceptions among insomnia sufferers and normal sleepers. Sleep Med. 4, 285–296. https://doi.org/10.1016/s1389-9457(03)00057-1 (2003).
Attarian, H. P., Duntley, S. & Brown, K. M. Reverse sleep state misperception. Sleep Med. 5, 269–272. https://doi.org/10.1016/j.sleep.2003.10.014 (2004).
Webb, W. B. & Agnew, H. W. Jr. Sleep stage characteristics of long and short sleepers. Science (New York NY). 168, 146–147. https://doi.org/10.1126/science.168.3927.146 (1970).
Aeschbach, D., Cajochen, C., Landolt, H. & Borbély, A. A. Homeostatic sleep regulation in habitual short sleepers and long sleepers. Am. J. Physiol. 270, R41–R53. https://doi.org/10.1152/ajpregu.1996.270.1.R41 (1996).
Wallace, M. L. et al. Which sleep health characteristics predict all-cause mortality in older men? an application of flexible multivariable approaches. Sleep https://doi.org/10.1093/sleep/zsx189 (2018).
Zhang, G. Q. et al. The National Sleep Research Resource: Towards a sleep data commons. J. Am. Med. Inform. Assoc. 25, 1351–1358. https://doi.org/10.1093/jamia/ocy064 (2018).
Ohayon, M. M., Carskadon, M. A., Guilleminault, C. & Vitiello, M. V. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep 27, 1255–1273. https://doi.org/10.1093/sleep/27.7.1255 (2004).
Vitiello, M. V., Larsen, L. H. & Moe, K. E. Age-related sleep change: Gender and estrogen effects on the subjective-objective sleep quality relationships of healthy, noncomplaining older men and women. J. Psychosom. Res. 56, 503–510. https://doi.org/10.1016/s0022-3999(04)00023-6 (2004).
Unruh, M. L. et al. Subjective and objective sleep quality and aging in the sleep heart health study. J. Am. Geriatr. Soc. 56, 1218–1227. https://doi.org/10.1111/j.1532-5415.2008.01755.x (2008).
van den Berg, J. F. et al. Sex differences in subjective and actigraphic sleep measures: A population-based study of elderly persons. Sleep 32, 1367–1375. https://doi.org/10.1093/sleep/32.10.1367 (2009).
Park, S. et al. Psychosocial factors affecting sleep misperception in middle-aged community-dwelling adults. PLoS ONE 15, e0241237. https://doi.org/10.1371/journal.pone.0241237 (2020).
Orwoll, E. et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study—A large observational study of the determinants of fracture in older men. Contemp. Clin. Trials. 26, 569–585. https://doi.org/10.1016/j.cct.2005.05.006 (2005).
Blank, J. B. et al. Overview of recruitment for the osteoporotic fractures in men study (MrOS). Contemp. Clin. Trials. 26, 557–568. https://doi.org/10.1016/j.cct.2005.05.005 (2005).
Blackwell, T. et al. Associations between sleep architecture and sleep-disordered breathing and cognition in older community-dwelling men: The Osteoporotic Fractures in Men Sleep Study. J. Am. Geriatr. Soc. 59, 2217–2225. https://doi.org/10.1111/j.1532-5415.2011.03731.x (2011).
Mehra, R. et al. Prevalence and correlates of sleep-disordered breathing in older men: Osteoporotic fractures in men sleep study. J. Am. Geriatr. Soc. 55, 1356–1364. https://doi.org/10.1111/j.1532-5415.2007.01290.x (2007).
Edinger, J. D. & Fins, A. I. The distribution and clinical significance of sleep time misperceptions among insomniacs. Sleep 18, 232–239. https://doi.org/10.1093/sleep/18.4.232 (1995).
Manconi, M. et al. Measuring the error in sleep estimation in normal subjects and in patients with insomnia. J. Sleep Res. 19, 478–486. https://doi.org/10.1111/j.1365-2869.2009.00801.x (2010).
Van Den Berg, J. F. et al. Disagreement between subjective and actigraphic measures of sleep duration in a population-based study of elderly persons. J. Sleep Res. 17, 295–302. https://doi.org/10.1111/j.1365-2869.2008.00638.x (2008).
Dittoni, S. et al. Psychological functioning measures in patients with primary insomnia and sleep state misperception. Acta Neurol. Scand. 128, 54–60. https://doi.org/10.1111/ane.12078 (2013).
Normand, M. P., St-Hilaire, P. & Bastien, C. H. Sleep spindles characteristics in insomnia sufferers and their relationship with sleep misperception. Neural Plast. 2016, 6413473. https://doi.org/10.1155/2016/6413473 (2016).
Mercer, J. D., Bootzin, R. R. & Lack, L. C. Insomniacs’ perception of wake instead of sleep. Sleep 25, 564–571 (2002).
Vanable, P. A., Aikens, J. E., Tadimeti, L., Caruana-Montaldo, B. & Mendelson, W. B. Sleep latency and duration estimates among sleep disorder patients: Variability as a function of sleep disorder diagnosis, sleep history, and psychological characteristics. Sleep 23, 71–79 (2000).
Ohayon, M. M. & Roth, T. Place of chronic insomnia in the course of depressive and anxiety disorders. J. Psychiatr. Res. 37, 9–15 (2003).
Yoshiike, T. et al. Mortality associated with nonrestorative short sleep or nonrestorative long time-in-bed in middle-aged and older adults. Sci. Rep. 12, 189. https://doi.org/10.1038/s41598-021-03997-z (2022).
Kline, C. E. et al. Self-reported long sleep in older adults is closely related to objective time in bed. Sleep Biol. Rhythms. 8, 42–51. https://doi.org/10.1111/j.1479-8425.2009.00422.x (2010).
Takahashi, N. et al. Differences between subjective and objective sleep duration according to actual sleep duration and sleep-disordered breathing: The Nagahama Study. J. Clin. Sleep Med. 18, 851–859. https://doi.org/10.5664/jcsm.9732 (2022).
Vgontzas, A. N., Liao, D., Bixler, E. O., Chrousos, G. P. & Vela-Bueno, A. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep 32, 491–497. https://doi.org/10.1093/sleep/32.4.491 (2009).
Alessandria, M. & Provini, F. Periodic limb movements during sleep: A new sleep-related cardiovascular risk factor?. Front. Neurol. 4, 116. https://doi.org/10.3389/fneur.2013.00116 (2013).
Wang, X. et al. Obstructive sleep apnea and risk of cardiovascular disease and all-cause mortality: a meta-analysis of prospective cohort studies. Int. J. Cardiol. 169, 207–214. https://doi.org/10.1016/j.ijcard.2013.08.088 (2013).
Parrino, L., Milioli, G., De Paolis, F., Grassi, A. & Terzano, M. G. Paradoxical insomnia: the role of CAP and arousals in sleep misperception. Sleep Med. 10, 1139–1145. https://doi.org/10.1016/j.sleep.2008.12.014 (2009).
Rotenberg, V. S., Indursky, P., Kayumov, L., Sirota, P. & Melamed, Y. The relationship between subjective sleep estimation and objective sleep variables in depressed patients. Int. J. Psychophysiol. 37, 291–297. https://doi.org/10.1016/s0167-8760(00)00110-0 (2000).
Agnew, H. W. Jr., Webb, W. B. & Williams, R. L. The first night effect: An EEG study of sleep. Psychophysiology 2, 263–266. https://doi.org/10.1111/j.1469-8986.1966.tb02650.x (1966).
Curcio, G., Ferrara, M., Piergianni, A., Fratello, F. & De Gennaro, L. Paradoxes of the first-night effect: A quantitative analysis of antero-posterior EEG topography. Clin. Neurophysiol. 115, 1178–1188. https://doi.org/10.1016/j.clinph.2003.12.018 (2004).
Tamaki, M., Nittono, H., Hayashi, M. & Hori, T. Examination of the first-night effect during the sleep-onset period. Sleep 28, 195–202. https://doi.org/10.1093/sleep/28.2.195 (2005).
Quan, S. F. et al. Short-term variability of respiration and sleep during unattended nonlaboratory polysomnography-The Sleep Heart Health Study (corrected). Sleep 25, 843–849 (2002).
Le Bon, O. et al. The first-night effect may last more than one night. J. Psychiatr. Res. 35, 165–172. https://doi.org/10.1016/s0022-3956(01)00019-x (2001).
Berry, R.B.B.R.G.C. et al. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Version 2.4. (American Academy of Sleep Medicine, 2017).
Yesavage, J. A. Geriatric Depression Scale. Psychopharmacol. Bull. 24, 709–711 (1988).
Teng, E. L. & Chui, H. C. The Modified Mini-Mental State (3MS) examination. J. Clin. Psychiatry. 48, 314–318 (1987).
Washburn, R. A., Smith, K. W., Jette, A. M. & Janney, C. A. The physical activity scale for the elderly (PASE): Development and evaluation. J. Clin. Epidemiol. 46, 153–162. https://doi.org/10.1016/0895-4356(93)90053-4 (1993).
Johns, M. W. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 15, 376–381. https://doi.org/10.1093/sleep/15.4.376 (1992).
Buysse, D. J., Reynolds, C. F. 3rd., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213. https://doi.org/10.1016/0165-1781(89)90047-4 (1989).
Knutson, K. L. & von Schantz, M. Associations between chronotype, morbidity and mortality in the UK Biobank cohort. Chronobiol. Int. 35, 1045–1053. https://doi.org/10.1080/07420528.2018.1454458 (2018).
Borbély, A. A., Daan, S., Wirz-Justice, A. & Deboer, T. The two-process model of sleep regulation: A reappraisal. J. Sleep Res. 25, 131–143. https://doi.org/10.1111/jsr.12371 (2016).
Robbins, R. et al. Self-reported sleep duration and timing: A methodological review of event definitions, context, and timeframe of related questions. Sleep Epidemiol. https://doi.org/10.1016/j.sleepe.2021.100016 (2021).
Aritake, S. et al. Time estimation during nocturnal sleep in human subjects. Neurosci. Res. 49, 387–393. https://doi.org/10.1016/j.neures.2004.04.006 (2004).
Hublin, C., Partinen, M., Koskenvuo, M. & Kaprio, J. Sleep and mortality: A population-based 22-year follow-up study. Sleep 30, 1245–1253. https://doi.org/10.1093/sleep/30.10.1245 (2007).
Teno, J. M., Weitzen, S., Fennell, M. L. & Mor, V. Dying trajectory in the last year of life: Does cancer trajectory fit other diseases?. J. Palliat. Med. 4, 457–464. https://doi.org/10.1089/109662101753381593 (2001).
Castro-Costa, É. et al. Association between sleep duration and all-cause mortality in old age: 9-year follow-up of the Bambuí Cohort Study, Brazil. J. Sleep Res. 20, 303–310. https://doi.org/10.1111/j.1365-2869.2010.00884.x (2011).
da Silva, A. A. et al. Sleep duration and mortality in the elderly: A systematic review with meta-analysis. BMJ Open 6, e008119. https://doi.org/10.1136/bmjopen-2015-008119 (2016).
Li, P., Stuart, E. A. & Allison, D. B. Multiple imputation: A flexible tool for handling missing data. JAMA 314, 1966–1967. https://doi.org/10.1001/jama.2015.15281 (2015).
Sterne, J. A. et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ (Clin. Res. Ed.) 338, 2393. https://doi.org/10.1136/bmj.b2393 (2009).
Acknowledgements
We obtained data from the Osteoporotic Fractures in Men (MrOS) Study, which was funded by the National Institutes of Health via the National Institute on Aging (NIA) and the National Center for Advancing Translational Sciences (NCATS) (grant numbers R01 AG066671 and UL1 TR000128). The National Heart, Lung, and Blood Institute funded the ancillary MrOS Sleep Study titled “Outcomes of Sleep Disorders in Older Men” (grant numbers R01 HL071194, R01 HL070848, R01 HL070847, R01 HL070842, R01 HL070841, R01 HL070837, R01 HL070838, and R01 HL070839). The National Sleep Research Resource was supported by the National Heart, Lung, and Blood Institute (R24 HL114473, 75N92019R002). We thank Ryusei Iijima, MT, MHSc for helping us prepare the datasets analyzed in this study.
Funding
This study received a grant-in-aid for scientific research from the Ministry of Health, Labor and Welfare, Government of Japan (grant numbers #19FA1009 and #21FA1002). The funder had no role in the study design or procedures, including data collection, management, analysis, and interpretation, nor was there any such involvement in the manuscript preparation, review, approval, or decision to submit for publication.
Author information
Authors and Affiliations
Contributions
K.K. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: K.K., T.Y., T.U., S.A.O.; acquisition, analysis, or interpretation of data: T.U., K.K., T.Y., Y.K., S.A.O., K.M., K.N., K.S., R.O., M.Su.; drafting of the manuscript: T.U., T.Y., K.K.; critical revision of the manuscript for important intellectual content: K.K., T.Y., T.U., S.A.O., Y.K., K.M., K.N., K.S., R.O., M.Sh., M.Su.; statistical analysis: T.Y., T.U.; obtained funding: K.K.; administrative, technical, or material support: S.A.O.; supervision: K.K., T.Y. All authors have read and approved the submitted manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. Utsumi reports payments for lectures outside the submitted work, including services at speakers bureaus from Eisai. Dr. Yoshiike reports payments for lectures outside the submitted work, including services at speakers bureaus from MSD and Takeda Pharmaceutical. Dr. Kaneita has no relevant conflicts of interest to declare. Dr. Aritake-Okada reports several items outside the submitted work, namely expert testimony from Idorsia Pharma, grants from the Kao Corporation, payments for lectures, including services at speakers bureaus from MSD, as well as services at speakers bureaus and payments for the development of educational presentations from Takeda Pharmaceutical and payments for the development of educational presentations from NIHON SOYAKU. Dr. Matsui reports payments for lectures outside the submitted work, including services at speakers bureaus from Eisai, Meiji Seika Pharma, MSD, Otsuka Pharmaceutical, Takeda Pharmaceutical, and Yoshitomi Pharmaceutical. Dr. Nagao reports payments for lectures outside the submitted work, including services at speakers bureaus from Takeda Pharmaceutical and Sumitomo Dainippon Pharm. Dr. Saitoh reports personal fees received from Yoshitomi Pharmaceutical outside the submitted work. Dr. Otsuki reports no relevant conflicts of interest. Dr. Shigeta has no relevant conflicts of interest to declare. Dr. Suzuki reports grants and payments for lectures outside the submitted work, including services at speakers bureaus from Dainippon Sumitomo, Eisai, Mochida Pharmaceutical, Otsuka Pharmaceutical, and Takeda Pharmaceutical, grants from Novartis, and payments for lectures and services at speakers bureaus from EA Pharma, Meiji Seika Pharma, MSD, Pfizer, Yoshitomi Pharmaceutical, and Viatris. Dr. Kuriyama reports items outside the submitted work, including grants from Otsuka Pharmaceutical, Mitsubishi Tanabe Pharma, Shionogi Pharma, and Pfizer, as well as grants and personal fees from Meiji Seika Pharma, Eisai, MSD, Takeda Pharmaceutical, Tsumura, and Eli Lilly, and personal fees from Yoshitomi Pharmaceutical and Sumitomo Pharma. There are no other disclosures to report including non-financial interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Utsumi, T., Yoshiike, T., Kaneita, Y. et al. The association between subjective–objective discrepancies in sleep duration and mortality in older men. Sci Rep 12, 18650 (2022). https://doi.org/10.1038/s41598-022-22065-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-22065-8
This article is cited by
-
Objective sleep quality predicts subjective sleep ratings
Scientific Reports (2024)
-
A prospective study of the association of weekend catch-up sleep and sleep duration with mortality in middle-aged adults
Sleep and Biological Rhythms (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.