Abstract
Upper airway collapsibility after anaesthesia induction may be associated with unpredictable difficult airway. However, most works on airway anatomy are tended to morphological description before anaesthesia. This study aimed to evaluate the changes of upper airway after anaesthesia induction and using pre-anesthetic ultrasound measurements to predict Difficult Laryngoscopy (DL). We included 104 eligible subjects with complete data, who were performed tracheal intubations under general anaesthesia in the study. The upper airway changes before and after anaesthesia induction were determined by seven neck ultrasound measurements, included as follow: (1) Distance from skin to under surface of Tongue (DT), (2) Thickness of the thickest part of Tongue body (TT), (3) Hyoid Mental Distance (HMD), (4) Depth of Hyoid (DH), (5) Width of Hyoid (WH), (6) Distance from Skin to Epiglottis (DSE), (7) Depth of the anterior combination of the Vocal Cords (DVC). DL was evaluated with Cormack–Lehane (CL). Data regarding HMD [from 45.3 (42.4–48.5) to 41.1 (38.5–44.9) mm], DH [from 8.7 (6.6–10.9) to 7.0 (5.3–9.1) mm], DSE [from 20.1 (16.6–22.5) to 19.5 (16.5–21.6) mm] and the DVC [from 7.1 (5.7–8.3) to 6.8 (5.7–7.9) mm] were decreased (P < 0.05), while the DT [from 15.9 (13.1–18.4) to 17.4 (14.5–19.8) mm] was increased (P > 0.05) after anaesthesia induction. Additionally, when cut-off value of DSE was 21.25 mm before anaesthesia, it may be better predicted to DL [sensitivity 80.0% (95% CI: 60.7–91.6%) and specificity 83.8% (95% CI: 73.0–91.0%)]. The upper airway after induction showed the propensity of collapsibility by ultrasound measurements. Compared with other indicators, the DSE assessed by ultrasound might be considered to a valuable predictor of DL.
Trial registration: The study was registered in ClinicalTrials.gov on 23th Jan 2019, ChiCTR1900021123.
Similar content being viewed by others
Introduction
Difficult airway management is one of the most relevant issues for practicing emergency physicians, intensivists, and anaesthesiologists, since airway obstruction in an unexpected patient can lead to brain damage even death1,2,3. It is well known that increasing mortality of anaesthesia was connected with collapsibility and obstruction of upper airway4,5. Deficiency of pharyngeal patency may be associated with changes in neck anatomy after anaesthesia induction, because local electromyographic activity abruptly decreases to a nadir6,7. Correct management of airway collapsibility during anaesthesia induction largely depends on an in-depth knowledge of the anatomic changes of upper airway8, because the changes of upper airway after anaesthesia are complicated. However, an accurate evaluation of the airway collapsibility may not be obtained with neck parameters before anaesthesia, and there are less sufficient scientific evidences for detection of upper airway changes after induction of anaesthesia. Robust, prospective evidences were needed to identify the changes of upper airway and predict difficult airway during anaesthesia induction.
Accordingly, point-of-care ultrasound is an effective, non-invasive and widely available tool, which can detect morphologic changes in upper airway with no radiation and little patient preparations9,10,11. It was hypothesized that the airway collapsibility could be described by ultrasonic anatomical parameters in patients under anaesthesia induction(primary outcome) and pre-anesthetic ultrasound measurements in upper airway could predict difficult airway(secondary outcome).
Methods
The study was designed as a prospective observational study. Ethical approval for this study was provided by the ethics committee of the first affiliated hospital of Guangzhou University of Chinese Medicine (NO.ZYYECK (2018) 041), and this trial was registered in the clinical trial registry of China (ChiCTR1900021123). Informed written consent was obtained. The study was conducted in accordance with the guidelines provided by the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Humans, and we confirmed that all experiments were performed in accordance with relevant guidelines and regulations. We recruited patients who had undergone elective surgery with general anaesthesia in the First Affiliated Hospital of Guangzhou University of Chinese Medicine between February 2019 and January 2020. The patients presented with American Society of Anaesthesiologists (ASA) physical status I or II and were aged between 18 and 70 years. Inclusion and exclusion criteria were shown in Table 1.
Random number table was used to select two eligible patients every day. To reduce the risk of bias, only one anaesthetist using ultrasound device (Navi series, Shenzhen Wisonic Medical Technologies, Shenzhen, China) proficiently was responsible for measurement and data record. Preoperative evaluation was performed the day before surgery, and informed consent was obtained from each subject. The demographic characteristics and clinical screening tests including gender, BMI, mouth opening, thyromental distance, neck circumference and modified Mallampati grade were collected. After routine fasting (no solids ≥ 8 h; no water ≥ 2 h), patients were sent to operating rooms (OR) and positioned supine on the operating tables with their heads in sniffing position7,12. The ECG, SpO2, noninvasive blood pressure, capnography and accelerometric neuromuscular monitoring of train-of-four (TOF) were employed.
To compare the changes in upper airway during induction of anaesthesia and assess DL, a cranio-caudal scan of the neck with the probe placed in the transverse and longitudinal axis was performed and 7 kinds of distances from 5 ultrasound images were measured as follows:
-
(1)
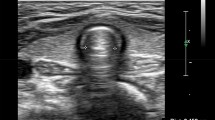
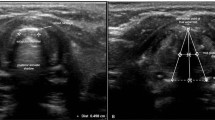
Distance from skin to under surface of Tongue (Depth of Tongue, DT), Fig. 1A13.
Figure 1 Patient positioning and transducer placement for measuring (left), anatomical (middle) and ultrasonography views (right) at the level of the tongue surface (A), tongue body (B), hyoid (C), epiglottis (D) and vocal cords (E), before anaesthetic induction. Consent to publish the figure was obtained from the patient.
-
(2)
Thickness of the thickest part of Tongue body (Tongue Thickness, TT) and Hyoid-Mental Distance (HMD), Fig. 1B14,15.
-
(5)
Depth of the anterior commissure of the Vocal Cords (DVC), Fig. 1E14. The images had been stored on the hard drive of the ultrasound device (Fig. 1).
To obtain the upper airway data after induction in safety, the processes of ultrasound measurements and face mask ventilation were carried out alternately every 3 min. The general anaesthesia was performed by two attending anaesthetists in a standard protocol with a combination of 0.003 to 0.004 mg·kg−1 fentanyl, 0.1 mg·kg−1 vecuronium, and 1 to 2 mg·kg−1 propofol. Depth of anaesthesia was measured by a Narcotrend-Compact monitor (MT MonitorTechnik GmbH & Co.KG, Helsinki, Germany). Pre-oxygenation were lasting for 3 min through a facemask with 100% oxygen (5–6 L·min−1). Face mask ventilation was continuously administered to the patient for 5 min till the anaesthetic plane was deep enough (Narcotrend D, train-of-four, TOF ¼ 0). Then, face mask was removed and the same ultrasound device was used to quickly measure the seven kinds of distances of upper airway above when patients were anaesthetised. SpO2 changes should be paid more attention during measurement. The process would be stopped if SpO2 < 93%. Face mask ventilation was performed until SpO2 increased. All procedures would be completed in the duration of SpO2 > 93%. If an unpredicted emergency airway was encountered, anaesthetist would instantly asked for help from the airway management team. A non-invasive airway tool or method such as a laryngeal mask airway (LMA) should be used to ensure ventilation. If ventilation was failed, a surgical airway must immediately be established to rescue the patient’s life3.
Once all measurements came to an end, face mask ventilation was performed for 5 min again. The conventional direct laryngoscopy with a Macintosh blade was performed to evaluate the Cormack–Lehane grades (CL grades) by another attending anaesthetist who was blinded to the results of the previous ultrasound data. According to a modified version of the CL classification system17,18, the patients were designated as Non-Difficult Laryngoscopy group (NDL, CL grades < 2b) and Difficult Laryngoscopy group (DL, CL grades ≥ 2b), respectively19.
Alveolar recruitment manoeuvres were performed immediately after orotracheal intubation. Mechanical ventilation was carried out with tidal volume of 8–10 ml·kg−1, respiration rate of 10–12 times·min−1, and PetCO2 of 30–35 mmHg. Subsequent anaesthesia maintenance and surgery were performed as usual.
Outcomes
The primary outcomes were the changes of the seven neck ultrasound measurements in upper airway before and after anaesthetic induction. The ultrasound measurement was used to evaluate the seven tissue structures: DT, TT, HMD, DH, WH, DSE and DVC. The secondary outcomes included laryngoscopy results of CL grades (early prediction for difficult airway) and correlation between CL grades and each indicator (clinical screening tests and ultrasound measurement data).
Statistical analysis
According to the literature16, the DSE measured by ultrasound might be used to predict DL. Therefore, a pilot study of 20 subjects was carried out to estimate sample size. The change in DSE before and after anaesthesia induction was 0.22 cm ± 0.55 (mean ± standard) in pilot study. Furthermore, the ratio between NDL and DL groups was 3:1 (non-difficult: difficult = 3:1). Pass 11.0 software showed that at least 100 patients would be necessary to obtain statistically significant differences between two groups, when accepting an alpha error of 0.05 and a beta error of 0.20.
The IBM Statistical Package for the Social Sciences (SPSS) V.25.0.was used for data analysis. The measurement data were presented as the means ± standard deviation or median (P25–P75), and the categorical variable data were presented as numbers. The Kolmogorov–Smirnov test was used to verify the normality of all ultrasound measurement data. Mann–Whitney U test or χ2 was used for variables comparison of demographic characteristics and clinical screening tests. According to distribution sets, changes before and after anaesthesia induction were analyzed by the Wilcoxon rank test. The Medcalc software was used for comparison of the area under (AUC) the receiver-operating characteristic curves (ROC curves) determined the correlation between each indicator and the CL grade, included clinical screening tests and perioperative sonographic data. The Youden index (the maximal difference between sensitivity and 1-specificity) was used to determine the optimal cut-off scores for significant indices, then, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the predictive indicators were calculated by QuickCalcs software. For all analyses, P value < 0.05 would be considered significantly.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the ethics committee of the first affiliated hospital of Guangzhou University of Chinese Medicine (NO.ZYYECK (2018) 041), and this trial was registered in the clinical trial registry of China (ChiCTR1900021123).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Results
A total of 110 patients were enrolled. Important missing values occurred in four patients, and two patients were excluded because of cancellation of the operation. Thus, 104 subjects with complete data were successfully included for analysis in this study. The flowchart of this trial was provided in Fig. 2.
There were 48 men (46.15%) and 56 women (53.85%). Participant characteristics are described in Table 2.
We sequentially obtained 5 ultrasound views in the neck. Compared with the data before anaesthesia, the HMD, DH, DSE and the DVC were decreased (P < 0.05), while the DT (P < 0.05) was increased after anaesthesia induction. All data are shown in Table 3.
Seventy-four patients (71.15%) were classified as NDL group (CL < 2b), while 30 patients (28.85%) were classified as DL group (CL ≥ 2b) in direct laryngoscopy. The ROC curve analysis showed the AUC of each predictor. Sensitivity, specificity, PPV and NPV were shown in Table 4.
Table 2 showed there were statistical differences between NDL and DL groups in BMI, thyromental distance, neck circumference, modified Mallampati grade and DSE. However, Table 4 confirmed that only three variables of neck circumference, modified Mallampati grade and DSE might have diagnostic value in DL prediction (AUC was more than 0.7). The ROC curve of significant variables of neck circumference, modified Mallampati grade and DSE were demonstrated in Fig. 3.
The ROC curves of DSE (blue line), neck circumference (green line) and modified Mallampati grade (red line), the AUC > 0.7 were showed. Asterisk: comparison with the AUC of the other 2 airway assessment tests, there were significant differences between DSE and other predictors (P < 0.05). Calculated by nonparametric test.
The cut-off value of the DSE prediction criterion for DL determined by Youden index was 21.25 mm. The AUC of the DSE (AUC: 0.868) was bigger than other predictors. The sensitivity and specificity of DSE predicting DL were 80.0% (95% CI: 60.7–91.6%) and 83.8% (95% CI: 73.0–91.0%), respectively.
Hyoid bone is a bone structure of the upper airway and the width of it will not change after anaesthesia induction. In this study, the width of hyoid bone was 10.8 (9.8–12.3) mm and 11.2(10.1–12.5) mm before and after anaesthesia induction, respectively. There was no significant difference of hyoid bone between two states (P = 0.089 > 0.05), which showed good accuracy and repetitive stability of our results.
Discussion
This study examined the changes of upper airway parameters before and after induction of anaesthesia by ultrasound device. The major findings of the study were (1) that the DT was deeper after induction of anaesthesia, while HMD, DH, DSE and the DVC were decreased, suggesting the propensity for the upper airway collapsibility was tongue drops close to hand palate and cartilaginous structures came-up with muscle relax, and (2) that data of the DSE measured by ultrasound device before anaesthesia may be a better predictor for DL.
The assessing devices for morphology changes of upper airway before and after induction of anaesthesia include rulers, radiography equipment, computerized tomography, magnetic resonance imaging and so on20,21,22. Compared with the aforementioned methods, ultrasound plays an important role in various diagnostic or therapeutic purposes in the operating theatre and critical care settings, especially the increasing use in airway management in the last decade23. In some studies24,25, ultrasound could be used for the care of pediatric and obstetric airway, confirmation of proper laryngeal mask airway position and evaluation of full stomach26,27. Emanuela Roldi et al28 found that ultrasound measurement of tracheal diameter could assist with the choice of the size of left double-lumen tube. To our knowledge, however, studies that involved ultrasound measurements for morphology changes of upper airway after anaesthesia induction were less reported. Our findings extend the application of this technique to managing airways undergoing general anaesthesia. This study indicated that it was relatively simple to identify the different airway structures with the ultrasound image. We also found that the propensity for the upper airway to collapse after muscular relaxation obtained by ultrasound was consistent with previous studies4,29, and similar to Simons JC30, this collapsibility of airway after induction of anaesthesia was stable. In all of these studies, the authors observed upper airway closing pressure (PCLOSE) and genioglossus muscle electromyography to endpoints29,30,31, while we visibly recorded changes of upper airway before and after anaesthesia induction by ultrasound device, it might show a high degree of accuracy by “your eyes”. Identification the changes in upper airway after anaesthesia induction is conducive to airway management, especially if upper airway collapsibility occurs in outdoor anaesthesia, such as ERCP and gastro-endoscope. Therefore, when it comes to this, the results of this study suggest that it is crucial to avoid tongue blocking laryngeal and restore muscle tension in the neck as soon as possible.
In this study, compared with that before anaesthesia, we found the DT was deeper, while HMD and DH were decreased, which could be partly explained by the decrease of related muscle activity and lung volume under anaesthesia induction30. On the one hand, the inhibitory effects on central drive to genioglossus activity in propofol anaesthesia will lead to loss of support on pharyngeal in humans4, the animal studies32 in cats also showed electromyographic activity of the genioglossus muscle and hypoglossal nerve activity decreased in during halothane anaesthesia. On the other hand, inspiratory and respiratory pump muscles inhibited after anaesthesia induction could also contribute to the observed changes in upper airway collapsibility. Lung volume decreased caused by such inhibitory effects on muscles after anaesthesia, could also result in upper airway collapsibility by virtue of longitudinal tension within the airway wall and a decreased caudal traction on the upper airway33.
In other recent studies, Weidong et al.34 performed sonographic measurements of mandibular condylar mobility to predict DL, and Yadav et al.35 showed ultrasound measurements of soft tissue thickness of the anterior neck and tongue thickness along with the clinical assessment of airway could be useful in predicting DL. Only one or two ultrasound parameters were recorded in these studies, while clinical screening tests and other seven ultrasonography parameters to compare the diagnosis value for DL were systematically collected in our study. We compared clinical screening tests including BMI, mouth opening, thyromental distance, neck circumference, modified Mallampati grade and six selected upper airway ultrasound parameters such as DT, TT, HMD, DH, DSE and the DVC. Our data demonstrated that the AUC of the DSE was 0.868 which was significantly bigger than the other(P < 0.05) predictors. Additionally, when the DSE exceeded 21.25 mm, the sensitivity and specificity of predicting DL were 80.0% (95% CI: 60.7–91.6%) and 83.8% (95% CI: 73.0–91.0%), respectively. Pinto16 and Martinez-Garcia36 also found that the DSE was associated to DL, but the cut-off values were not the same, which could be explained by small sample sizes and different areas where subjects came from. In our observational study, we expanded the sample size and compared the DSE measured by ultrasound device with other 11 indicators, which trying to get a more complete understanding of the DSE prediction DL. Increasing thickness at the level of the pre-epiglottic space could affect the ability to visualise the glottis with a Macintosh blade at direct laryngoscopy19. It could explain that a higher upwards concavity of the oropharyngeal curve would not overlap with pharyngo-glottic-tracheal curve, which lead to bad glottic visualization when both curves were not aligned with the visual axis37. The incidence of DL was 28.85% in our study, which was higher than others which defined CL grades ≥ 3 as DL36 (we defined DL as CL grades ≥ 2b), In our study, the incidence of DL was 28.85%, it was higher than other studies which defining CL grades ≥ 3 as DL36, (we defined CL grades ≥ 2b as DL), because some researchers believed that DL might have occurred on the condition of novice anaesthetists when the CL grade was 2b17,19.
Our study has several limitations. Potential selection bias might be existed since we excluded patients with obviously difficult intubation. On the one hand, it was a concern for the safety of the patients, on the other hand, we thought it might allow us to evaluate changes of upper airway in normal patients and use ultrasound measurements to predict unknown DL. The total time to measure all the sonographic variables was approximately 10 min in each patient before and after induction of anaesthesia, which was more time-consuming than other studies34,35,36. Our purposes were to identify the changes of upper airway via more variables, and screened out which variable might have the maximum correlation with the laryngoscopic view. Although seven distances from five ultrasound images were measured in our study, it was still difficult in fully displaying the upper airway changes during anaesthesia induction when compared with MRI and CT20,21, while they were more time-consuming and expensive. Furthermore, all measurements were performed within the images in store, not in real time, more data of upper airway structures should be collected during dynamic motion.
Finally, it has been suggested that the thickness of the base of the tongue (SBL) and hyoid mental distance with hyperextension of the head and subluxation of the mandible (DIMs) could effectively predict difficult mask ventilation, which may be caused by thick tongue could be displaced more posteriorly after anaesthesia, and reduced the air space also at the level of the oropharynx and hypopharynx limiting the airflow coming11. However, our study did not include difficult mask ventilation into the outcomes, because other studies suggested that mask ventilation could be facilitated by muscle relaxation after anaesthesia in adults38,39, it was quite controversial. Although our study found that parameters such as SBL and hyoid mental distance have no predictive value for difficult laryngoscopy, it was not discussed whether these ultrasound measurements could show values in difficult mask ventilation prediction, so we will further expand the sample size and include difficult mask ventilation as one of the outcomes in the follow-up research to obtain more complete results.
In summary, our study shown a new measurement process of upper airway after induction of anaesthesia. Our data measured by ultrasound device demonstrated that the propensity of upper airway collapsibility was tongue drops close to the hard palate and cartilaginous structures came-up after induction of anaesthesia. These results might provide a systematic investigation in upper airway, and we found the DSE assessed by ultrasound may be crucial to predict DL when compared with other indicators. Moreover, establishing a further prediction of difficult Laryngoscopy is required to reduce the incidence of the false negatives and the false positives, it can ensure patients’ safety and make the best use of resources.
Data availability
All data generated or analysed during this study are included in this published article [and its Supplementary Information files].
References
Heidegger, T. Management of the difficult airway. N. Engl. J. Med. 384(19), 1836–1847. https://doi.org/10.1056/NEJMra1916801 (2021).
Frerk, C. et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br. J. Anaesth. 115(6), 827–848. https://doi.org/10.1093/bja/aev371 (2015).
Kornas, R. L., Owyang, C. G., Sakles, J. C., Foley, L. J. & Mosier, J. M. Evaluation and management of the physiologically difficult airway: Consensus recommendations from Society for Airway Management. Anesth. Analg. 132(2), 395–405. https://doi.org/10.1213/ane.0000000000005233 (2021).
Eastwood, P. R., Platt, P. R., Shepherd, K., Maddison, K. & Hillman, D. R. Collapsibility of the upper airway at different concentrations of propofol anesthesia. Anesthesiology 103(3), 470–477. https://doi.org/10.1097/00000542-200509000-00007 (2005).
Norton, J. R. et al. Differences between midazolam and propofol sedation on upper airway collapsibility using dynamic negative airway pressure. Anesthesiology 104(6), 1155–1164. https://doi.org/10.1097/00000542-200606000-00009 (2006).
Hillman, D. R. et al. Evolution of changes in upper airway collapsibility during slow induction of anesthesia with propofol. Anesthesiology 111(1), 63–71. https://doi.org/10.1097/ALN.0b013e3181a7ec68 (2009).
Dong, F., Wang, Y., Wang, X., Zhao, H. & Ma, W. Changes in the upper airway following induction of anaesthesia: A prospective observational study protocol to determine the use of ultrasound in the assessment of a difficult airway in China. BMJ Open 9(7), e029782. https://doi.org/10.1136/bmjopen-2019-029782 (2019).
Gómez-López, L. et al. Ultrasound measurement of anatomical parameters of the upper airway in adults. Rev. Esp. Anestesiol. Reanim. (Engl. Ed.) 65(9), 495–503. https://doi.org/10.1016/j.redar.2018.05.007 (2018).
Austin, D. R., Chang, M. G. & Bittner, E. A. Use of handheld point-of-care ultrasound in emergency airway management. Chest 159(3), 1155–1165. https://doi.org/10.1016/j.chest.2020.09.083 (2021).
Gottlieb, M., Holladay, D., Burns, K. M., Nakitende, D. & Bailitz, J. Ultrasound for airway management: An evidence-based review for the emergency clinician. Am. J. Emerg. Med. 38(5), 1007–1013. https://doi.org/10.1016/j.ajem.2019.12.019 (2020).
Bianchini, A., Nardozi, L., Nardi, E. & Scuppa, M. F. Airways ultrasound in predicting difficult face mask ventilation. Minerva Anestesiol. 87(1), 26–34. https://doi.org/10.23736/s0375-9393.20.14455-9 (2021).
Mendonca, C., Ungureanu, N., Nowicka, A. & Kumar, P. A randomised clinical trial comparing the “sniffing” and neutral position using channelled (KingVision(®)) and non-channelled (C-MAC(®)) videolaryngoscopes. Anaesthesia 73(7), 847–855. https://doi.org/10.1111/anae.14289 (2018).
Adhikari, S. et al. Pilot study to determine the utility of point-of-care ultrasound in the assessment of difficult laryngoscopy. Acad Emerg. Med. 18(7), 754–758. https://doi.org/10.1111/j.1553-2712.2011.01099.x (2011).
Petrisor, C., Dîrzu, D., Trancă, S., Hagău, N. & Bodolea, C. Preoperative difficult airway prediction using suprahyoid and infrahyoid ultrasonography derived measurements in anesthesiology. Med. Ultrason. 21(1), 83–88. https://doi.org/10.11152/mu-1764 (2019).
Chen, J. W., Chang, C. H., Wang, S. J., Chang, Y. T. & Huang, C. C. Submental ultrasound measurement of dynamic tongue base thickness in patients with obstructive sleep apnea. Ultrasound Med. Biol. 40(11), 2590–2598. https://doi.org/10.1016/j.ultrasmedbio.2014.06.019 (2014).
Pinto, J. et al. Predicting difficult laryngoscopy using ultrasound measurement of distance from skin to epiglottis. J. Crit. Care 33, 26–31. https://doi.org/10.1016/j.jcrc.2016.01.029 (2016).
Cook, T. M. A new practical classification of laryngeal view. Anaesthesia 55(3), 274–279. https://doi.org/10.1046/j.1365-2044.2000.01270.x (2000).
Sajayan, A., Wicker, J., Ungureanu, N., Mendonca, C. & Kimani, P. K. Current practice of rapid sequence induction of anaesthesia in the UK—A national survey. Br. J. Anaesth. 117(Suppl 1), i69–i74. https://doi.org/10.1093/bja/aew017 (2016).
Falcetta, S. et al. Evaluation of two neck ultrasound measurements as predictors of difficult direct laryngoscopy: A prospective observational study. Eur. J. Anaesthesiol. 35(8), 605–612. https://doi.org/10.1097/eja.0000000000000832 (2018).
Gupta, K. & Gupta, P. K. Assessment of difficult laryngoscopy by electronically measured maxillo-pharyngeal angle on lateral cervical radiograph: A prospective study. Saudi J. Anaesth. 4(3), 158–162. https://doi.org/10.4103/1658-354x.71572 (2010).
Wani, T. M. et al. Age-based analysis of pediatric upper airway dimensions using computed tomography imaging. Pediatr. Pulmonol. 51(3), 267–271. https://doi.org/10.1002/ppul.23232 (2016).
Feng, Y. et al. Dynamic upper airway imaging during wakefulness in obese subjects with and without sleep apnea. Am. J. Respir. Crit. Care Med. 198(11), 1435–1443. https://doi.org/10.1164/rccm.201711-2171OC (2018).
Dalesio, N. M. et al. Age-related changes in upper airway anatomy via ultrasonography in pediatric patients. Pediatr. Emerg. Care https://doi.org/10.1097/pec.0000000000001821 (2019).
Daniel, S. J., Bertolizio, G. & McHugh, T. Airway ultrasound: Point of care in children—The time is now. Paediatr. Anaesth. 30(3), 347–352. https://doi.org/10.1111/pan.13823 (2020).
Zheng, B. X., Zheng, H. & Lin, X. M. Ultrasound for predicting difficult airway in obstetric anesthesia: Protocol and methods for a prospective observational clinical study. Medicine (Baltimore) 98(46), e17846. https://doi.org/10.1097/md.0000000000017846 (2019).
Wojtczak, J. A. & Cattano, D. Laryngo-tracheal ultrasonography to confirm correct endotracheal tube and laryngeal mask airway placement. J. Ultrason. 14(59), 362–366. https://doi.org/10.15557/JoU.2014.0037 (2014).
El-Boghdadly, K., Wojcikiewicz, T. & Perlas, A. Perioperative point-of-care gastric ultrasound. BJA Educ. 19(7), 219–226. https://doi.org/10.1016/j.bjae.2019.03.003 (2019).
Roldi, E. et al. Use of tracheal ultrasound combined with clinical parameters to select left double-lumen tube size: A prospective observational study. Eur. J. Anaesthesiol. 36(3), 215–220. https://doi.org/10.1097/eja.0000000000000939 (2019).
Mishima, G. et al. Upper-airway collapsibility and compensatory responses under moderate sedation with ketamine, dexmedetomidine, and propofol in healthy volunteers. Physiol. Rep. 8(10), e14439. https://doi.org/10.14814/phy2.14439 (2020).
Simons, J. C. et al. Effects of depth of propofol and sevoflurane anesthesia on upper airway collapsibility, respiratory genioglossus activation, and breathing in healthy volunteers. Anesthesiology 125(3), 525–534. https://doi.org/10.1097/aln.0000000000001225 (2016).
Eikermann, M. et al. The influence of aging on pharyngeal collapsibility during sleep. Chest 131(6), 1702–1709. https://doi.org/10.1378/chest.06-2653 (2007).
Ochiai, R., Guthrie, R. D. & Motoyama, E. K. Effects of varying concentrations of halothane on the activity of the genioglossus, intercostals, and diaphragm in cats: An electromyographic study. Anesthesiology 70(5), 812–816. https://doi.org/10.1097/00000542-198905000-00018 (1989).
Rowley, J. A., Permutt, S., Willey, S., Smith, P. L. & Schwartz, A. R. Effect of tracheal and tongue displacement on upper airway airflow dynamics. J. Appl. Physiol. (1985) 80(6), 2171–2178. https://doi.org/10.1152/jappl.1996.80.6.2171 (1996).
Yao, W. et al. Can mandibular condylar mobility sonography measurements predict difficult laryngoscopy?. Anesth. Analg. 124(3), 800–806. https://doi.org/10.1213/ane.0000000000001528 (2017).
Yadav, N. K., Rudingwa, P., Mishra, S. K. & Pannerselvam, S. Ultrasound measurement of anterior neck soft tissue and tongue thickness to predict difficult laryngoscopy—An observational analytical study. Indian J. Anaesth. 63(8), 629–634. https://doi.org/10.4103/ija.IJA_270_19 (2019).
Martínez-García, A., Guerrero-Orriach, J. L. & Pino-Gálvez, M. A. Ultrasonography for predicting a difficult laryngoscopy. Getting closer. J. Clin. Monit. Comput. 35(2), 269–277. https://doi.org/10.1007/s10877-020-00467-1 (2021).
Greenland, K. B. Airway assessment based on a three column model of direct laryngoscopy. Anaesth. Intensive Care 38(1), 14–19. https://doi.org/10.1177/0310057x1003800104 (2010).
Engelhardt, T. & Weiss, M. Difficult mask ventilation and muscle paralysis. Anesthesiology 118(4), 994. https://doi.org/10.1097/ALN.0b013e3182874659 (2013).
Richardson, M. G. & Litman, R. S. Ventilation before paralysis: Crossing the Rubicon, slowly. Anesthesiology 117(3), 456–458. https://doi.org/10.1097/ALN.0b013e318266868f (2012).
Funding
This study was supported by grants from the National Natural Science Foundation of China (82074357), Guangzhou Municipal Science and Technology Bureau, China (202102080036).
Author information
Authors and Affiliations
Contributions
Study conception and design: X.W., W.-H.M. Acquisition of the data: X.W., Y.W. Analysis and interpretation of the data: X.W., Z.-W.Z., Y.-R.L. Drafting of the manuscript: X.W., Z.-W.Z., Y.-R.L. Critical revision: Y.W., W.-H.M. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the images in Fig. 1.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, X., Wang, Y., Zheng, ZW. et al. Ultrasound measurements for evaluation of changes in upper airway during anaesthesia induction and prediction difficult laryngoscopy: a prospective observational study. Sci Rep 12, 18564 (2022). https://doi.org/10.1038/s41598-022-21695-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-21695-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.