Abstract
The phase angle (PhA), measured via bioelectrical impedance analysis, is considered an indicator of cellular health, where higher values reflect higher cellularity, cell membrane integrity, and better cell function. This study aimed to examine the relationship between PhA and exercise habits or objectively measured physical activity. We included 115 people aged 32–69 years. The body composition and PhA were measured using a bioelectrical impedance device. Physical activity and sedentary behavior (SB) were assessed using a triaxial accelerometer. Exercise habits were also obtained through structured interviews, and participants were categorized into the no exercise habit (No-Ex), resistance training exercise habit (RT), or aerobic training exercise habit (AT) groups. Objectively measured moderate-to-vigorous physical activity or step count significantly correlated with PhA, independent of age, sex, height, percent body fat, body cell mass, and leg muscle power. In contrast, SB was not significant determinants of PhA. People who exercised regularly (RT or AT) had significantly higher PhA values than did those in the No-Ex group. Furthermore, the PhA was not significantly different between the RT and AT groups. Regularly engaging in exercise with moderate-to-vigorous intensity may improve or maintain muscle cellular health and muscle quality.
Similar content being viewed by others
Introduction
Bioelectrical impedance analysis (BIA) measures the impedance of the human body1, which consists of resistance (R) and reactance (Xc). The phase angle (PhA) can be calculated as [arctangent (Xc/R) × 180°/π]2. Raw impedance variables have attracted substantial interest in clinical nutrition3,4,5,6,7,8,9. PhA is considered an indicator of cellular health, with higher values indicating higher cellularity, cell membrane integrity, and better cell function10,11. Previous studies have indicated that PhA decreases during aging12,13 and is correlated with nutritional status11,14,15 and disease status9,14,16,17,18,19, muscle power or strength6,10,20,21, aerobic capacity22 gait ability, and physical fitness2, prospective fall23 and mortality24.
The BIA theories have been established since the 1930s25,26, and BIA has been used to assess human body composition since the 1960s27,28,29,30,31. BIA requires ethnicity-specific, sex-specific, age-specific, or health condition-specific models or equations to estimate the human body composition. However, the PhA is obtained directly from the BIA raw impedance data with the above mentioned equation; thus, the results are not biased by the choice of equations. Because over 90% of the total impedance is obtained from appendicular segments (a leg and an arm) in the whole-body BIA method, in which the electrical path is from the ankle to the wrist, the whole-body PhA mainly reflects the characteristics of the appendicular lean soft tissue (ALST). Because most ALSTs are skeletal muscle cell tissues32, PhA is an indicator of skeletal muscle cell quality. The revised version of the European Working Group on Sarcopenia in Older People notes the importance of muscle quality assessed by PhA obtained by BIA, as well as that assessed by magnetic resonance imaging (MRI) or computed tomography33.
Regular physical activity and limited sedentary behavior (SB) are important factors for the prevention of non-communicable diseases, such as type-2 diabetes, cardiovascular diseases, and breast and colon cancers34,35,36,37,38,39. Regular physical activity and SB contribute to maintaining healthy weight, general well-being, cardiovascular and muscular health. Regular physical activity and SB can be evaluated objectively using accelerometry-based activity monitors or subjectively through interviews or questionnaires40,41,42,43. The above-mentioned cellular health may be related to regular physical activity or SB, but studies examining the association between PhA and physical activity or SB in healthy adults are limited44. To our knowledge, this study is the first to examine the association between PhA and objectively measured physical activity and SB in a healthy population.
We hypothesized that a higher PhA, an indicator of better cellular health, is associated with exercise habits or a longer moderate-to-vigorous intensity physical activity (MVPA) duration and a shorter duration of SB in daily life. Here, we examined the relationship between the PhA and exercise habits, or physical activity and SB, which were objectively assessed by accelerometry-based activity monitors in Japanese adults.
Methods
Participants
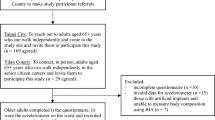
We included 115 people (30 men and 85 women; mean and SD of age were, 55.3 ± 8.0 years old, and range of age was 32–69 years old). Participants were recruited from a longitudinal study at the National Institute of Health and Nutrition, Tokyo45. The inclusion criteria were as follows: (1) anthropometric variables were measured. (2) Physical activity was measured using accelerometer-based activity monitors. (3) Their PhA was measured using bioelectrical impedance spectroscopy (BIS). We excluded the subjects with cardiovascular, respiratory, neurological, metabolic or orthopedic disorders. This studies were reviewed and approved by the Institutional Review Board of the National Institute of Biomedical Innovation, Health and Nutrition (No KENEI-102). The participants provided their written informed consent to participate in this study. All methods were performed in accordance with the relevant guidelines and regulations.
Anthropometry, body composition, and phase angle
Height, weight, and waist circumference were measured, and body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared (kg/m2). The body composition was estimated, and the PhA was measured using the BIS (SFB7, ImpediMed, Pinkenba, Australia) as follows10: Two injectable electrodes were placed on the dorsal surface of the right hand and foot, and detecting electrodes were placed on the dorsum of the right wrist and ankle (Red Dot, 3M Health Care, MN, USA). BIS was measured in the supine position, between 8 and 10 A.M., and before any physical fitness test. Fat-free mass (FFM), body cell mass (BCM), and percent body fat (%fat) were obtained using the BIS software (Bio-imp version 5.5.0.1, ImpediMed). Participants were divided into low and high PhA groups based on the sex-specific median of the PhA results (5.4 for women and 6.5 for men).
Physical activity measurement
A previously validated triaxial accelerometer (Actimarker EW4800, Panasonic, Osaka, Japan) was used to track intensities of physical activity46,47,48,49. All participants were asked to wear a triaxial accelerometer for 20 days. We used the data for 14 days, during which the accelerometer was worn continuously on waking until going to bed. The accelerometer’s technical features and estimated equation were fully detailed46,47. The accelerometer samples the acceleration at a rate of 20 Hz, with a performance of zero to twice the momentum of gravity. It keeps track of the SD of the three-dimensional vector norm of the composite acceleration for a minute. In a study of healthy adults, the vector norm was significantly associated (R2 = 0.86) with oxygen uptake (VO2) during walking and running at seven different paces spanning from 40 to 160 m min−1 and during seven common activities: food preparation, self-care while upright, replacing clothing, cleaning dishes, eating supper, vacuuming, and doing laundry46,50. The metabolic equivalent of tasks (MET) and step counts were was obtained at one-minute intervals. MVPA was defined as MET ≥ 3.0. The light intensity physical activity (LPA) was defined as 1.5 to 2.9 METs, and SB was defined as any waking behavior characterized by ≤ 1.5 METs51,52.
Exercise habits
Engaging in regular exercise habits was interviewed by well-trained staff using the structured method of the National Nutrition Survey in Japan53,54,55. The participants were asked whether they currently exercised (over 30 min per session, twice a week for 3 months). Participants who answered “yes” were classified as having exercise habits (exercised regularly). Participants who answered “no” were classified as participants without exercise habits (non-Ex No-Ex group). Moreover, we divided the participants who have exercise habits into engaging resistance training (RT group) or only aerobic exercises (AT group).
Blood samples
Blood samples were collected from participants following an overnight fast for at least 10 h between 8 and 10 A.M.55. Venous blood withdrawn from the antecubital vein was collected into tubes without additives or EDTA and immediately centrifuged at 3000 rpm for 20 min to obtain serum or plasma. The levels of glucose and glycated hemoglobin (HbA1c) in plasma, total cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides in the serum were determined55.
Grip strength
Grip strength tests were conducted after BIA measurements. Maximal GS was measured using a Smedley Hand Dynamometer (Grip-D, TKK5401; Takei Scientific Instruments, Niigata, Japan), as described elsewhere56. When performing the measurement, subjects were instructed to maintain a standard bipedal position for the duration of the test. The involved arm was placed in complete extension with the dynamometer not touching any other part of the body, except the hand being measured. The width of the handle was adjusted to ensure that, when the subject held the dynamometer, the second phalanx was against the inner stirrup. Two trials, separated by a brief rest, were allowed for each hand alternately, and the highest value was recorded as the result. Subjects were encouraged to exert themselves maximally during each effort.
Statistical analyses
The results are presented as the mean ± SDs. One-way analysis of variance (ANOVA) and analysis of covariance (ANCOVA) was used to compare physical characteristics and physical activities between the low and high PhA groups. Age and sex were set as covariates for the ANCOVA. Pearson’s correlation coefficients were calculated, and partial correlation coefficients were calculated between the PhA and other variables, with age and sex as control variables. Correlations presenting coefficients between, 0.00–0.29, 0.30–0.49, 0.50–0.69, 0.70–0.89, and 0.90–1.0, were considered “negligible”, “low”, “moderate”, “high” and “very high”, respectively57. Multiple linear regression analyses were conducted with PhA as the objective variable and age, sex, height, %fat, BCM, leg muscle power, MVPA, step counts, or regular exercise habits as the explanatory variables while avoiding multicollinearity (< 5 variance inflation factor [VIF]). An alpha of 0.05 was used for statistical significance for all analyses. All analyses were performed using SPSS 22.0 (IBM Inc., USA).
Results
The physical characteristics and activities of the participants are presented in Table 1. The ANOVA results showed that the high PhA group was younger and had higher BMI, BCM, calf circumference, leg muscle power, MVPA, and step counts than the low PhA group (P < 0.05). In addition, men had higher PhA values than women (6.5° ± 0.7° vs. 5.4 ± 0.5°, P < 0.001). The ANCOVA results show that the high PhA group had higher values of weight, BMI, FFM, BCM, calf circumference, handgrip strength, leg muscle power, MVPA, and step counts than the low PhA group after adjustment for age and sex (P < 0.05). Higher BMI in the higher PA group was due to higher body cell mass (P < 0.01), but not due to percent body fat difference (P > 0.4).
Table 2 shows the Pearson and partial correlation coefficients between PhA and other variables. The PhA was negatively and significantly correlated with age (r = − 0.361, P < 0.001). BMI, percent body fat, FFM, BCM, leg muscle power, MVPA, and step counts were significantly correlated with PhA in both Pearson and partial correlation analyses (P < 0.05). The relationship between PhA and leg muscle power, MVPA, and step count is shown in Fig. 1. In addition, we compared the PhA values between the No-Ex, AT, and RT groups using ANCOVA and found that the AT and RT groups had significantly higher PhA (P < 0.05) than the No-Ex group, even after adjustment for age and sex (Fig. 1). In contrast, there was no significant difference between the AT and RT groups (P > 0.05).
The results of multiple regression analyses are shown in Table 3. All variables in both models have < 5. BCM, leg muscle power, MVPA, step counts, and regular exercise habits were selected as significant predictors of the between-individual difference in PhA, independent of age, sex, height, and percent body fat (P < 0.05).
Discussion
In the present study, daily MVPA, step count, and exercise habits, FFM, BCM, calf circumference, handgrip strength, and leg muscle power are associated with PhA. The objectively measured MVPA or step count was significantly associated with PhA in healthy adults, independent of age, sex, height, percent body fat, BCM, and leg muscle power. Conversely, SB and LPA were not significant determinants of PhA. Moreover, people who exercised had significantly higher PhA values than those in the No-Ex group. Furthermore, the PhA value was not significantly different between the RT and AT groups in our study.
In the present study, age was negatively associated with PhA, and men (mean ± SD; 6.5 ± 0.7) had a higher PhA than women (5.4 ± 0.5) (Table 3). The results was consistent with previous studies5,13. Moreover, the leg muscle power was positively associated with PhA even after controlling for age and sex. These observations were consistent with previous studies5,13. PhA was also positively associated with BCM and FFM and negatively associated with body fat percentage in the current population. The range of PhA was 4.2 to 8.2 which was also consistent with previous studies2,5.
Regular physical activity was assessed via objective and subjective methods. For objective assessment, a previously validated triaxial accelerometer was used to assess daily step counts, MVPA, LPA, and SB46,47,48,49. We found that step counts and MVPA was significantly and positively correlated with PhA, even after adjusting for age, sex, height, percent body fat, BCM, and leg muscle power. In contrast, SB was not significantly associated with PhA. As a subjective method, the exercise habits were assessed by the interview based on the structured method of the National Nutrition Survey in Japan53,54,55. In addition to step count or MVPA, subjectively assessed exercise habits were also significantly associated with PhA (Table 3, Model 3). Furthermore, the exercise modality (RT or AT) did not affect the results of the PhA (Fig. 1).
Mundstock reviewed previous studies examining the association between PhA and physical activity44. In the healthy adult population review, most of the previous studies applied a randomized controlled trial design with RT mode and subjective physical activity assessment. Ribeiro et al. found that 8-week RT significantly improved the PhA58, and Souza et al. also found that 12-week RT improved PhA59. Most recently, Otsuka et al. examined the effect of 24-wk moderate-intensity RT on thigh PhA in middle-aged and older adults and found that moderate-intensity RT also improved PhA (+ 0.3°)60. In addition, the change in PhA significantly correlated with the change in thigh muscle cross-sectional area (CSA) measured by MRI. Otsuka et al.60 also found that PhA is correlated with the ratio between intermuscular adipose tissue and thigh muscle CSA, suggesting that PhA reflects muscle quality. Thus, RT, which induces muscle hypertrophy, improves the PhA in the segments. The present study also showed that people who engaged in regular RT had significantly higher PhA than those who did not have any exercise habits.
Several researches have assessed the effect of daily physical activity on PhA61,62. In addition, Cupisti et al. examined 50 hemodialysis patients and found that the daily energy expenditure estimated using the SenseWear Armband was positively related to PhA (r = 0.40, P < 0.01)63. In the healthy adult population, we found that MVPA and daily step counts were positively associated with PhA (r = 0.388 and r = 0.409, respectively; P < 0.001). The current results are consistent with those findings.
PhA was not significantly different between the RT and AT groups in participants who exercised regularly in the present study. No other study has compared the effects of RT and AT on the PhA; therefore, further studies are required. In addition, the present study has some limitations. This is a cross-sectional study; thus, cause-and-effect logic is not clear. Hence, longitudinal and intervention studies are also required. Furthermore, the current sample size is small and further large cohort study are required. Nevertheless, our results suggest that regularly engaging in exercises with moderate-to-vigorous intensities may improve or maintain muscle cellular health. However, PhA was not significantly correlated with SB or LPA, which may indicate that preventing SB by engaging in LPA is not sufficient to improve muscle cellular health.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Schoeller, D. A. Bioelectrical impedance analysis. What does it measure?. Ann. N. Y. Acad. Sci. 904, 159–162 (2000).
Yamada, Y. et al. Association of bioelectrical phase angle with aerobic capacity, complex gait ability and total fitness score in older adults. Exp. Gerontol. https://doi.org/10.1016/j.exger.2021.111350 (2021).
Norman, K. et al. Cutoff percentiles of bioelectrical phase angle predict functionality, quality of life, and mortality in patients with cancer. Am. J. Clin. Nutr. 92(3), 612–619. https://doi.org/10.3945/ajcn.2010.29215 (2010) (Epub 2010/07/16).
Kuchnia, A. J. et al. Phase angle and impedance ratio: Reference cut-points from the United States National Health and Nutrition Examination Survey 1999–2004 from bioimpedance spectroscopy data. JPEN J. Parenter. Enteral Nutr. 41(8), 1310–1315. https://doi.org/10.1177/0148607116670378 (2017) (Epub 2016/09/28).
Barbosa-Silva, M. C., Barros, A. J., Wang, J., Heymsfield, S. B. & Pierson, R. N. Jr. Bioelectrical impedance analysis: Population reference values for phase angle by age and sex. Am. J. Clin. Nutr. 82(1), 49–52 (2005) (Epub 2005/07/09).
Yamada, M. et al. Phase angle is a useful indicator for muscle function in older adults. J. Nutr. Health Aging. 23(3), 251–255. https://doi.org/10.1007/s12603-018-1151-0 (2019) (Epub 2019/03/02).
Piccoli, A., Pillon, L. & Dumler, F. Impedance vector distribution by sex, race, body mass index, and age in the United States: Standard reference intervals as bivariate Z scores. Nutrition 18(2), 153–167 (2002) (Epub 2002/02/15).
Norman, K., Stobäus, N., Pirlich, M. & Bosy-Westphal, A. Bioelectrical phase angle and impedance vector analysis–clinical relevance and applicability of impedance parameters. Clin. Nutr. 31(6), 854–861. https://doi.org/10.1016/j.clnu.2012.05.008 (2012) (Epub 2012/06/16).
Gupta, D. et al. Bioelectrical impedance phase angle in clinical practice: Implications for prognosis in advanced colorectal cancer. Am. J. Clin. Nutr. 80(6), 1634–1638. https://doi.org/10.1093/ajcn/80.6.1634 (2004) (Epub 2004/12/09).
Yamada, Y. et al. Electrical properties assessed by bioelectrical impedance spectroscopy as biomarkers of age-related loss of skeletal muscle quantity and quality. J. Gerontol. A Biol. Sci. Med. Sci. 72(9), 1180–1186. https://doi.org/10.1093/gerona/glw225 (2017).
Lukaski, H. C., Kyle, U. G. & Kondrup, J. Assessment of adult malnutrition and prognosis with bioelectrical impedance analysis: Phase angle and impedance ratio. Curr. Opin. Clin. Nutr. Metab. Care. 20(5), 330–339. https://doi.org/10.1097/mco.0000000000000387 (2017) (Epub 2017/05/27).
Bosy-Westphal, A. et al. Phase angle from bioelectrical impedance analysis: Population reference values by age, sex, and body mass index. JPEN J. Parenter. Enteral Nutr. 30(4), 309–316. https://doi.org/10.1177/0148607106030004309 (2006) (Epub 2006/06/29).
Mattiello, R., Amaral, M. A., Mundstock, E. & Ziegelmann, P. K. Reference values for the phase angle of the electrical bioimpedance: Systematic review and meta-analysis involving more than 250,000 subjects. Clin. Nutr. 39(5), 1411–1417. https://doi.org/10.1016/j.clnu.2019.07.004 (2020) (Epub 2019/08/12).
Marra, M. et al. Bioelectrical impedance phase angle in constitutionally lean females, ballet dancers and patients with anorexia nervosa. Eur. J. Clin. Nutr. 63(7), 905–908 (2009).
Grundmann, O., Yoon, S. L. & Williams, J. J. The value of bioelectrical impedance analysis and phase angle in the evaluation of malnutrition and quality of life in cancer patients—A comprehensive review. Eur. J. Clin. Nutr. 69(12), 1290–1297. https://doi.org/10.1038/ejcn.2015.126 (2015).
Machado, F. V. C. et al. Relationship between body composition, exercise capacity and health-related quality of life in idiopathic pulmonary fibrosis. BMJ Open Respir. Res. 8(1), e001039. https://doi.org/10.1136/bmjresp-2021-001039 (2021).
Gupta, D. et al. Bioelectrical impedance phase angle as a prognostic indicator in breast cancer. BMC Cancer 8, 249. https://doi.org/10.1186/1471-2407-8-249 (2008) (Epub 2008/08/30).
Gupta, D. et al. Bioelectrical impedance phase angle in clinical practice: Implications for prognosis in stage IIIB and IV non-small cell lung cancer. BMC Cancer 9, 37. https://doi.org/10.1186/1471-2407-9-37 (2009) (Epub 2009/01/30).
Schwenk, A. et al. Phase angle from bioelectrical impedance analysis remains an independent predictive marker in HIV-infected patients in the era of highly active antiretroviral treatment. Am. J. Clin. Nutr. 72(2), 496–501. https://doi.org/10.1093/ajcn/72.2.496 (2000).
Wada, O., Kurita, N., Yamada, M. & Mizuno, K. Structural severity, phase angle, and quadriceps strength among patients with knee osteoarthritis: The SPSS-OK study. Clin. Rheumatol. 39(10), 3049–3056. https://doi.org/10.1007/s10067-020-05056-w (2020) (Epub 2020/04/29).
Yoshida, T. et al. Intracellular-to-total water ratio explains the variability of muscle strength dependence on the size of the lower leg in the elderly. Exp. Gerontol. 113, 120–127. https://doi.org/10.1016/j.exger.2018.09.022 (2018) (Epub 2018/09/30).
Custódio Martins, P., de Lima, T. R., Silva, A. M. & Santos Silva, D. A. Association of phase angle with muscle strength and aerobic fitness in different populations: A systematic review. Nutrition 93, 111489. https://doi.org/10.1016/j.nut.2021.111489 (2022) (Epub 2021/10/24).
Uemura, K., Yamada, M. & Okamoto, H. Association of bioimpedance phase angle and prospective falls in older adults. Geriatr. Gerontol. Int. 19(6), 503–507. https://doi.org/10.1111/ggi.13651 (2019) (Epub 2019/04/09).
Garlini, L. M. et al. Phase angle and mortality: A systematic review. Eur. J. Clin. Nutr. 73(4), 495–508. https://doi.org/10.1038/s41430-018-0159-1 (2019).
Barnett, A. & Bagno, S. The physiological mechanisms involved in the clinical measure of phase angle. Am. J. Physiol. Legacy Content. 114(2), 366–382. https://doi.org/10.1152/ajplegacy.1935.114.2.366 (1935).
Horton, J. W. & VanRavenswaay, A. C. Electrical impedance of the human body. J. Franklin Inst. 220(5), 557–572. https://doi.org/10.1016/S0016-0032(35)90038-2 (1935).
Thomasset, A. Bioelectrical properties of tissue impedance measurements. Lyon Medical. 207, 107–118 (1962).
Hoffer, E. C., Meador, C. K. & Simpson, D. C. Correlation of whole-body impedance with total body water volume. J. Appl. Physiol. 27(4), 531–534 (1969).
Kanai, H., Sakamoto, K. & Haeno, M. Electrical measurement of fluid distribution in human legs: Estimation of extra- and intra-cellular fluid volume. J. Microw. Power. 18(3), 233–243 (1983).
Lukaski, H. C., Johnson, P. E., Bolonchuk, W. W. & Lykken, G. I. Assessment of fat-free mass using bioelectrical impedance measurements of the human body. Am. J. Clin. Nutr. 41(4), 810–817. https://doi.org/10.1093/ajcn/41.4.810 (1985) (Epub 1985/04/01).
Kushner, R. F. & Schoeller, D. A. Estimation of total body water by bioelectrical impedance analysis. Am. J. Clin. Nutr. 44, 417–424 (1986).
Heymsfield, S. B. et al. Phenotypic differences between people varying in muscularity. J. Cachexia Sarcopenia Muscle. https://doi.org/10.1002/jcsm.12959 (2022) (Epub 2022/02/17).
Cruz-Jentoft, A. J. et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing. 48(1), 16–31. https://doi.org/10.1093/ageing/afy169 (2019) (Epub 2018/10/13).
World Health O. WHO Guidelines on Physical Activity and Sedentary Behaviour 2020 (World Health Organization, 2020).
Owen, N. et al. Adults’ sedentary behavior: Determinants and interventions. Am. J. Prev. Med. 41(2), 189–196 (2011).
Lavie, C. J., Ozemek, C., Carbone, S., Katzmarzyk, P. T. & Blair, S. N. Sedentary behavior, exercise, and cardiovascular health. Circ. Res. 124(5), 799–815 (2019).
Lynch, B. M. Sedentary behavior and cancer: A systematic review of the literature and proposed biological mechanisms. Cancer Epidemiol. Prev. Biomark. 19(11), 2691–2709 (2010).
Owen, N., Healy, G. N., Matthews, C. E. & Dunstan, D. W. Too much sitting: The population-health science of sedentary behavior. Exerc. Sport Sci. Rev. 38(3), 105 (2010).
Warburton, D. E., Nicol, C. W. & Bredin, S. S. Health benefits of physical activity: The evidence. CMAJ 174(6), 801–809 (2006).
Troiano, R. P. et al. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 40(1), 181 (2008).
Sallis, J. F. & Saelens, B. E. Assessment of physical activity by self-report: Status, limitations, and future directions. Res. Q. Exerc. Sport 71(sup2), 1–14 (2000).
Hallal, P. C. et al. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 380(9838), 247–257 (2012).
Craig, C. L. et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35(8), 1381–1395 (2003).
Mundstock, E. et al. Association between phase angle from bioelectrical impedance analysis and level of physical activity: Systematic review and meta-analysis. Clin. Nutr. 38(4), 1504–1510. https://doi.org/10.1016/j.clnu.2018.08.031 (2019) (Epub 2018/09/19).
Tripette, J. et al. Effect of a 1-year intervention comprising brief counselling sessions and low-dose physical activity recommendations in Japanese adults, and retention of the effect at 2 years: A randomized trial. BMC Sports Sci. Med. Rehabil. 13(1), 133. https://doi.org/10.1186/s13102-021-00360-7 (2021) (Epub 2021/10/27).
Yamada, Y. et al. Light-intensity activities are important for estimating physical activity energy expenditure using uniaxial and triaxial accelerometers. Eur. J. Appl. Physiol. 105(1), 141–152. https://doi.org/10.1007/s00421-008-0883-7 (2009) (Erratum in: 16(6):1279).
Yamada, Y. et al. Validity of a triaxial accelerometer and simplified physical activity record in older adults aged 64–96 years: A doubly labeled water study. Eur. J. Appl. Physiol. 118(10), 2133–2146. https://doi.org/10.1007/s00421-018-3944-6 (2018) (Epub 2018/07/19).
Murakami, H. et al. Accuracy of 12 wearable devices for estimating physical activity energy expenditure using a metabolic chamber and the doubly labeled water method: Validation study. JMIR mHealth uHealth. 7(8), e13938. https://doi.org/10.2196/13938 (2019) (Epub 2019/08/04).
Murakami, H. et al. Accuracy of wearable devices for estimating total energy expenditure: Comparison with metabolic chamber and doubly labeled water method. JAMA Intern. Med. 176(5), 702–703. https://doi.org/10.1001/jamainternmed.2016.0152 (2016) (Epub 2016/03/22).
Matsumura, Y. et al. High-accuracy physical activity monitor utilizing three-axis accelerometer. Natl. Tech. Rep. 56(2), 60–66 (2008).
Gibbs, B. B., Hergenroeder, A. L., Katzmarzyk, P. T., Lee, I.-M. & Jakicic, J. M. Definition, measurement, and health risks associated with sedentary behavior. Med. Sci. Sports Exerc. 47(6), 1295 (2015).
Aoyama, T. et al. Association between age at onset of independent walking and objectively measured sedentary behavior is mediated by moderate-to-vigorous physical activity in primary school children. PLoS ONE 13(9), e0204030 (2018).
Ikeda, N., Takimoto, H., Imai, S., Miyachi, M. & Nishi, N. Data resource profile: The Japan National Health and nutrition survey (NHNS). Int. J. Epidemiol. 44(6), 1842–1849 (2015).
Ishikawa-Takata, K. & Takimoto, H. Current protein and amino acid intakes among Japanese people: Analysis of the 2012 National Health and Nutrition Survey. Geriatr. Gerontol. Int. 18(5), 723–731. https://doi.org/10.1111/ggi.13239 (2018).
Gando, Y. et al. Cardiorespiratory fitness suppresses age-related arterial stiffening in healthy adults: A 2-year longitudinal observational study. J. Clin. Hypertens. 18(4), 292–298. https://doi.org/10.1111/jch.12753 (2016) (Epub 2015/12/15).
Kimura, M., Mizuta, C., Yamada, Y., Okayama, Y. & Nakamura, E. Constructing an index of physical fitness age for Japanese elderly based on 7-year longitudinal data: Sex differences in estimated physical fitness age. Age 34(1), 203–214. https://doi.org/10.1007/s11357-011-9225-5 (2012) (Epub 2011/03/23).
Mukaka, M. M. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med. J. 24(3), 69–71 (2012) (Epub 2013/05/03).
Ribeiro, A. S. et al. Resistance training prescription with different load-management methods improves phase angle in older women. Eur. J. Sport Sci. 17(7), 913–921. https://doi.org/10.1080/17461391.2017.1310932 (2017) (Epub 2017/04/11).
Souza, M. F. et al. Effect of resistance training on phase angle in older women: A randomized controlled trial. Scand. J. Med. Sci. Sports. 27(11), 1308–1316. https://doi.org/10.1111/sms.12745 (2017) (Epub 2016/08/20).
Otsuka, Y. et al. Effects of resistance training intensity on muscle quantity/quality in middle-aged and older people: A randomized controlled trial. J. Cachexia Sarcopenia Muscle. https://doi.org/10.1002/jcsm.12941 (2022) (Epub 2022/02/22).
Di Vincenzo, O., Marra, M. & Scalfi, L. Bioelectrical impedance phase angle in sport: A systematic review. J. Int. Soc. Sports Nutr. 16(1), 49. https://doi.org/10.1186/s12970-019-0319-2 (2019).
Marra, M., Di Vincenzo, O., Sammarco, R., Morlino, D. & Scalfi, L. Bioimpedance phase angle in elite male athletes: A segmental approach. Physiol. Meas. 41(12), 125007. https://doi.org/10.1088/1361-6579/abcb5c (2021).
Cupisti, A., Capitanini, A., Betti, G., D’Alessandro, C. & Barsotti, G. Assessment of habitual physical activity and energy expenditure in dialysis patients and relationships to nutritional parameters. Clin. Nephrol. 75(3), 218–225. https://doi.org/10.5414/cnp75218 (2011) (Epub 2011/02/19).
Acknowledgements
We wish to thank Mr. Yuki Nishida for the BIS measurements. This study was funded by Health and Labour Sciences Research Grant (200825016B and 201222028B) to MM and Japan Society for the Promotion of Science (JSPS) KAKENHI (18H03164) to YY. The authors declare no competing financial interest.
Author information
Authors and Affiliations
Contributions
M.M., H.M., Y.Y. designed research; Y.Y., T.Y., H.M., R.K., Y.G., H.O., K.T., K.K., J.T., E.K., M.M. conducted research (data collection); Y.Y., T.N., H.N. analyzed data or performed statistical analysis; Y.Y., M.M. data interpretation; Y.Y. wrote paper and had primary responsibility for final content. All authors read, reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yamada, Y., Yoshida, T., Murakami, H. et al. Phase angle obtained via bioelectrical impedance analysis and objectively measured physical activity or exercise habits. Sci Rep 12, 17274 (2022). https://doi.org/10.1038/s41598-022-21095-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-21095-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.