Abstract
Readmission due to chronic obstructive pulmonary disease (COPD) exacerbation contributes significantly to disease burden. Trend in readmission rate among COPD patients in China is not well characterized. We described the secular trend and identify risk factors of COPD-related 30-day readmission in Beijing during 2012–2017. In this retrospective cohort study, we used data from a citywide hospital discharge database in Beijing. We included patients ≥ 40 years with a primary diagnosis of COPD from 2012 to 2017. A total of 131 591 index admissions were identified. COPD-related 30-day readmission was defined as the initial admission with a primary diagnosis of COPD that occurs within 30 days from the discharge date of an index admission. Overall and annual 30-day readmission rates were calculated in the total population and subgroups defined by patient characteristics. We used multivariable logistic models to investigate risk factors for readmission and in-hospital mortality within 30 days. The overall 30-day COPD-related readmission rate was 15.8% (n = 20 808). The readmission rate increased from 11.5% in 2012 to 17.2% in 2017, with a multivariable-adjusted OR (95% CI) for annual change to be 1.08 (1.06–1.09) (P trend < 0.001). The upward trend in readmission rate levelled off at about 17% since 2014. The readmission rate of men was higher and increased faster than women. Comorbid osteoporosis, coronary heart disease, congestive heart failure, and cancer were associated with an increased risk of 30-day COPD-related readmission. The 30-day COPD-related readmission rate in Beijing showed an overall increasing trend from 2012 to 2017. Future efforts should be made to further improve care quality and reduce early readmissions of COPD patients.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a common respiratory disease that has become a leading cause of death and disability in the world1. More than 80% of COPD deaths occurred in low- and middle-income countries (LMIC)2. In China, the prevalence of COPD in adults aged 20 years or older is 8.6%, accounting for 99.9 million people with COPD3. Improving disease management is a priority for such a large number of COPD patients. An important goal for COPD management is to prevent acute exacerbations4,5. COPD exacerbations cause hospitalization and readmission events, contributing significantly to medical expenditures6.
Hospital readmission rate within 30 days after discharge is a marker of health care quality. It was estimated that approximately 20% of COPD patients were readmitted within 30 days7. Some countries have made efforts to reduce excess readmissions8,9,10. The Chinese government implemented policies to reduce medical costs by controlling the mean length of stay. But the quality of care may be affected, and the readmission risk may increase. Consequently, the total expenditures per capita would not decline11. Recent data indicated that the increase in expenditures for COPD exacerbation was mainly driven by the increase in the number of admissions12. Monitoring the 30-day readmission rate using a national or regional representative database is needed to evaluate the care quality and economic burden of COPD patients. The long-term trend pattern of readmission over time is not well characterized in China. Early readmissions may usually be preventable if high-risk patients could be identified7. The number and types of comorbidities have been linked to readmission risk among COPD patients13, but most studies have been conducted in Europeans and Americans. Common comorbidities of COPD may vary across populations, and it is still unclear whether the association between comorbidities and COPD readmission risk differs between populations.
The present study aimed to describe the secular trend in COPD-related 30-day readmissions in Beijing during 2012–2017 based on a population-based citywide representative data. To identify patients at higher risk of 30-day readmission, we also examine risk factors for COPD readmission and in-hospital mortality (IHM) within 30 days.
Methods
Data source
We conducted a retrospective analysis using a hospital discharge database maintained by the Beijing Municipal Health Commission Information Centre. All secondary- and tertiary-level hospitals in Beijing are required to submit a standardized discharge record for each hospitalization. Only secondary- and tertiary-level hospitals admit inpatients in Beijing, therefore the database could capture all hospitalization events in Beijing. The Research Ethics Board of Beijing Chaoyang Hospital approved the study and waived the requirement for informed consent (2018-ke-303). Data were de-identified before analysis. It is impossible to identify patients at an individual level either in this article or in the retrieved database. Given the anonymous and mandatory nature of the data, informed consent was neither required nor necessary. All methods were performed in accordance with the ethical guidelines for human participants.
Study population
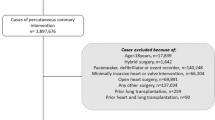
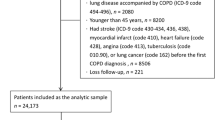
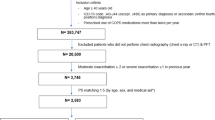
We included patients aged ≥ 40 years who were living in Beijing permanently from 2012 to 2017. During the study period, an index COPD admission was defined as a hospitalization with a primary diagnosis of COPD (International Classification of Diseases 10th Revision, ICD-10: J40-J44) that did not result in in-hospital death. We included bronchitis (J40-J42) and emphysema (J43) because they often co-occurred with COPD, and some COPD patients might be diagnosed as bronchitis or emphysema in practice. We also performed a sensitivity analysis using ICD-10 code J44 to define COPD admissions. If a patient had more than one hospitalization within 30 days, only the first one was counted as an index admission. Discharges against medical advice and those who planned to readmit in 30 days were excluded from index admissions. We excluded December discharges from index admissions because they could not be followed up for 30 days in this year. Finally, a total of 131 591 index admissions were included in our analysis.
Data collection
We obtained the front page of discharge records from the database. This page included demographic characteristics (age and sex), hospital level (secondary or tertiary), date of admission, length of hospital stay (LOHS) (days), the 10th International Classification of Diseases (ICD-10) codes of primary and other discharge diagnoses, use of mechanical ventilation, medical cost in Chinese yuan (CNY), and discharge outcome (alive or dead). Common comorbidities were determined according to discharge diagnoses. Charlson Comorbidity Index was calculated based on 19 categories of diseases14. The frequency of COPD-related hospitalizations (ICD-10: J40-J44) within 1 year prior to the index admission was obtained and categorized into 3 groups: 0, 1, and ≥ 2.
Outcome
The primary outcome of interest was COPD-related 30-day readmission, defined as the initial admission with a primary diagnosis of COPD (ICD-10: J40-J44) that occurs within 30 days from the discharge date of an index admission. The readmission rate was calculated as the number of index admissions with COPD-related 30-day readmission divided by the total number of index admissions (per 100 index admissions). The secondary outcome was IHM for COPD-related 30-day readmission.
Statistical analysis
One patient may have multiple hospitalizations, and all statistical analyses were based on hospitalization instead of a person. Characteristics of index admissions and readmissions in each year during the study period were described and compared. Descriptive statistics are presented as means ± standard deviations or medians for continuous variables and as percentages for categorical variables. Annual 30-day readmission rates were calculated in the total population and subgroups defined by age, sex, hospital level, and Charlson index at index admission. Adjusted annual change of 30-day readmission rate was estimated using logistic models with a random effect to account for multiple hospitalizations of one patient15. Model covariates included age, sex, hospital level, comorbidity index, and use of mechanical ventilation at index admission. We also described the in-hospital outcome (medical cost, use of mechanical ventilation, LOHS, and IHM) of 30-day COPD readmission by sex and year. We used multivariable logistic models to investigate risk factors for COPD readmission risk and IHM within 30 days. Linear models were used to estimate the association of comorbidities with total costs of the index admission and the 30-day COPD readmission. Statistical analyses were performed using Stata 15.0. All P values were two-sided. Statistical significance was set at < 0.05.
Results
Characteristics of index admissions
Between 2012 and 2017, we identified 131 591 index admissions (74 152 patients) submitted by 68 tertiary- and 51 secondary-hospitals, with a primary diagnosis of COPD in Beijing. The mean age of index admissions was 75.2 ± 10.3 years. Compared with 4 011 excluded admissions which occurred in-hospital death, index admissions were more likely to have fewer comorbidities, lower mechanical ventilation rate, and shorter mean LOHS (Table S1). The proportion of men and tertiary-hospital admissions increased over time, and the proportion of mechanical ventilation use showed a decreasing trend (Table S2).
Trends in COPD-related 30-day readmissions
There were 20 808 COPD-related readmissions within 30 days of index discharge, and the overall 30-day readmission rate was 15.8%. Of all COPD-related readmissions, 20.1% occurred at on first day after index discharge, and 49.9% occurred within 7 days after index discharge. The number of COPD-related readmissions stabilized after day 2 among women, while a readmission peak at day 7 was observed for men (Fig. 1). Table 1 presented characteristics and in-hospital outcomes of readmitted patients by calendar year. Mechanical ventilation use, LOHS, and median medical cost of readmitted patients showed decreasing trends from 2012 to 2017. Female patients were older and were more likely to have comorbidities than male patients. The proportion of mechanical ventilation use and median medical cost were higher in women than in men among patients readmitted to tertiary hospitals (Table S3).
The secular trend in annual COPD-related readmission rate was presented in Fig. 2. Overall, the readmission rate increased from 11.5% in 2012 to 17.2% in 2017 (Ptrend < 0.001). The adjusted OR (95% CI) for the annual change in the 30-day readmission rate was 1.08 (1.06–1.09) (Ptrend < 0.001). The readmission rate increased significantly from 2012 to 2014 (11.5% to 17.5%) and then remained almost unchanged at around 17% from 2014 to 2017. Men (19.9%) had a higher readmission rate than women (8.5%), with different trend patterns from women. The change of readmission rate over time in men was similar to the overall trend, with an adjusted OR (95% CI) for annual change to be 1.10 (1.08–1.12) (Ptrend < 0.001). Whereas in women, the readmission rate did not change significantly during the study period (Ptrend = 0.852). No significant differences in secular trends were found between subgroups by age, sex, Charlson index, and hospital level (Table S4). When using ICD-10 code J44 to define COPD, a total of 121 149 index admissions were identified, and the overall 30-day readmission rate was 16.3%. The secular trend of 30-day readmission rate under the J44 definition was similar to the main results (Fig. S1).
Gender-specific trends in 30-day COPD readmission rates during 2012–2017. ORs (95% CIs) for change in readmission rates per year were calculated using logistic regression models. Covariates included age, sex (for total population), hospital level, Charlson index, length of hospital stay, and use of mechanical ventilation at index admission.
In-hospital mortality of 30-day readmissions
Among 20 808 COPD-related readmissions, 709 (3.4%) in-hospital deaths occurred. Women had higher IHM than men (6.0% vs. 2.8%). The crude IHM of 30-day readmission decreased from 4.2% in 2012 to 2.8% in 2017. After multivariable adjustment, the IHM did not change significantly during 2012–2017 (OR for change per year: 0.99, 95% CI 0.93–1.07) (Fig. S2).
Risk factors for readmission and in-hospital mortality within 30 days
Compared with hospitalizations without 30-day COPD-related readmission, those who readmitted are more likely to be male, hospitalized for COPD in the previous year, from tertiary hospitals at index admission, have a higher proportion of mechanical ventilation, have higher medical costs, and have longer LOHS. The prevalence of common comorbidities differed between those with and without 30-day readmissions (Table 2).
Multivariable analyses showed that risk factors collected at index admission for 30-day readmission risk included male (OR = 1.89, 95% CI 1.78–2.00), hospitalized for COPD in the previous year, admitted to tertiary-hospital (OR = 1.10, 95% CI 1.04–1.16), Charlson index ≥ 3 (OR = 1.09, 95% CI 1.01–1.16), mechanical ventilation use (OR = 1.74, 95% CI 1.57–1.92), LOHS longer than 10 days, and having the following comorbidities: osteoporosis (OR = 1.14, 95% CI 1.02–1.27), coronary heart disease (OR = 1.16, 95% CI 1.10–1.22), congestive heart failure (OR = 1.09, 95% CI 1.02–1.16), and cancer (OR = 1.29, 95% CI 1.16–1.44) (Table 3). Using ICD-10 code J44 to define COPD did not change the results substantially (Table S5). Similar results were observed for IHM within 30 days (Table S6). Comorbid diabetes, coronary heart disease, cerebral vascular disease, congestive heart failure, and cancer were associated with 900 (642–1 158) CNY, 1 288 (1 076–1 500) CNY, 1 589 (1 359–1 818) CNY, 3 427 (3 161–3 693) CNY, and 2 392 (1 902–2 882) CNY higher costs of the index admission and 30-day COPD readmission, respectively (Table S7).
Discussion
In this 6-year trend analysis of a city-wide representative database in Beijing, we found that the overall 30-day readmission rate for COPD increased at an adjusted annual rate of 8% during 2012–2017. The readmission rate of men was higher and increased faster than women. Having comorbid osteoporosis, coronary heart disease, congestive heart failure, and cancer were associated with increased risk of 30-day COPD-related readmission.
As a result of poor inpatient care and discharge management, early readmissions frequently occur in COPD patients. An analysis of the US Health Cost and Utilization Project (HCUP) database found that 18.9% of COPD index hospitalizations had at least one 30-day readmission in 201316. Another study in London reported a 30-day readmission rate of 10.2% between 2006 and 20109. In the present study, we restricted the analysis to COPD-related readmissions (defined by primary diagnosis) and found that the overall 30-day readmission rate was 15.8% in Beijing between 2012 to 2017. Variability in rates of COPD readmissions between countries might be explained by differences in study methodology, ethnicity, disease diagnosis, and care quality. Nearly a half of 30-day COPD readmissions occurred within 1 week after discharge in our study. Previous studies also found that most readmissions occurred on the first day after discharge16,17. Early readmissions were thought to be more preventable and amenable to hospital-based interventions18. The relatively high readmission rates and a large proportion of early readmissions indicated the need for improving the quality of care and treatment received during and immediately after hospitalization.
Reducing readmissions for acute exacerbation of COPD has become a global challenge. COPD readmission within 30 days is associated with a higher economic burden and subsequent mortality risk19,20. In response, several countries developed policies linking payments to reducing readmissions. For example, the US Hospital Readmissions Reduction Program (HRRP) penalized hospitals with excess readmissions for targeted conditions including COPD21. Policy-related interventions to reduce hospital readmissions have shown variable temporal trends in 30-day readmission rates after COPD hospitalization in different countries. The 30-day readmission rate showed a modest decline trend from 2006 to 2014 in the US22,23,24. During the same period, a Spanish study based on a national discharge database found a significant reduction in COPD readmissions from 2006 to 201225. By contrast, the 30-day readmission rate in Beijing increased significantly from 11.5% in 2012 to 17.2% in 2017. The upward trend in readmission rate and the accompanying downward trend in IHM might partly reflect better access to hospital care and better treatment modalities during hospitalization for COPD in China. In addition, the severity of inpatients with COPD declined, which might also result in better survival rates26. But readmissions are responsible for most of the expenses related to the disease27,28, and many of them could be prevented with strategies to improve the quality of care29.
Moreover, early readmission rates for COPD could be reduced by some interventions including early follow-up care and care bundle after hospital discharge30. The care bundle includes continuity of care with a primary care physician or pulmonologist, optimization of medication, supervision of inhaler use, assessment and management of comorbidities, smoking cessation, and referral to pulmonary rehabilitation4. In addition, COPD self-management is essential in preventing readmissions, especially for high-risk subgroups such as female and older patients. Future research could evaluate the application of the COPD care bundle in China.
We observed that the 30-day readmission rate levelled off from 2014 to 2017 in Beijing. Several factors may contribute to this stable trend. First, the regional integrated care alliances were established in Beijing in 2013. To improve the quality and efficiency of healthcare services, the Beijing Municipal Health Commission promoted collaboration between secondary/tertiary hospitals and primary care institutions. Since 2013, a mutual referral system was gradually established across the city. Under this system, patients would seek primary care first before hospitalization, and inpatients would be referred to the primary health care institutions to receive subsequent treatment once their conditions are stable31. Second, the stable trend in readmission rate since 2014 might be benefited from improvements in air quality in Beijing during 2013–2017 as a result of the Air Pollution Prevention and Control Action Plan (APPCAP)32. Third, the decline in smoking prevalence after the implementation of the Beijing Tobacco Control Regulation in 2015 may also partly have contributed to the stable trend33.
Identifying patient-level risk factors is important in preventing COPD-related readmissions. LOHS, Charlson index, and use of mechanical ventilation are proxies of disease severity, and they have been used to predict 30-day readmission risk13. But limited and inconsistent results have been reported in the Chinese population34,35. We confirmed these predictors using a larger database that virtually covers all admissions in Beijing. These factors were also associated with increased risk of IHM at 30-day readmission. In concordance with previous results36, we observed a higher risk of 30-day readmission among male patients. But female readmitted patients appeared to be more severe and presented higher IHM than male readmitted patients. This finding may reflect gender disparities in disease phenotype, treatment, and management of COPD37. We should pay attention to improving healthcare services and reducing IHM in female readmitted patients.
COPD often coexists with other diseases, particularly in the elderly. Comorbidity is associated with poor outcomes of COPD. Congestive heart failure, osteoporosis, and cancer are established risk factors for exacerbation readmission13, and the results hold in this Chinese population. The association between comorbid coronary heart disease (CHD) and COPD-related readmission risk was still not clear. A large study in Canada found that ischaemic heart disease only predicted 1-year COPD readmission in women38. Other smaller studies reported inconsistent findings35,39. In our study, the prevalence of CHD in COPD hospitalized patients was high (49.6%), and patients with CHD were at higher risk of 30-day readmission. Interventions to reduce COPD readmissions need to target high-risk subgroups identified by comorbidities. In consistent with previous studies40,41, we also found that many comorbidities were associated with significantly higher costs in COPD inpatients. The prevention and management of comorbidities may contribute to reducing the economic burden of COPD.
The major strength of this study is the large representative sample in Beijing, the capital of China. Hospitalization information was collected from an administrative database, and the data quality had been strictly controlled by the government. The readmission plan was available on the front page of the discharge record since 2012, which facilitated us to exclude planned readmissions within 30 days. There are also several limitations. First, the findings of readmission rates and trends could not be generalized to other parts of China because of regional variations in disease spectrum and healthcare quality. Second, some covariates were not available, such as smoking status, medication use, lung function, and severity of COPD exacerbation. These factors were also associated with readmission risk36. Third, COPD-related readmissions could not capture symptom-based exacerbations, which may also reflect the quality of care. However, hospital readmission could be more accurately assessed using a discharge database.
In conclusion, the 30-day COPD-related readmission rate in Beijing showed an overall increasing trend from 2012 to 2017. Comorbid conditions were associated with the risk of 30-day readmission. These findings can guide future efforts to improve hospital treatment and post-discharge management in COPD patients. Preventing early readmissions after COPD hospitalizations would help reduce the significant disease burden in China.
Data availability
The data that support the findings of this study are available from Beijing Municipal Health Commission Information Centre but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Beijing Municipal Health Commission Information Centre.
References
GBD Chronic Respiratory Disease Collaborators. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir. Med. 8, 585 (2020).
WHO. WHO Global Health Estimates. Updated 2020. Available at: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed 5 Oct 2021.
Wang, C. et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): A national cross-sectional study. Lancet 391, 1706 (2018).
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2022 Report). Available at: https://goldcopd.org/2022-gold-reports-2/. Accessed 20 Nov 2021.
COPD Group of Chinese Thoracic Society. COPD Committee of Chinese Association of Chest Physician. [Guidelines for the diagnosis and management of chronic obstructive pulmonary disease (revised version 2021)]. Zhonghua Jie He He Hu Xi Za Zhi 44(3), 170–205 (2021).
Editorial, L. R. M. Reducing COPD readmissions-a personal and political priority. Lancet Respir. Med. 1(5), 347 (2013).
Shah, T., Press, V. G., Huisingh-Scheetz, M. & White, S. R. COPD readmissions: Addressing COPD in the era of value-based health care. Chest 150, 916 (2016).
Buhr, R. G. et al. Readmission rates for chronic obstructive pulmonary disease under the hospital readmissions reduction program: An interrupted time series analysis. J. Gen. Intern. Med. 35, 3581 (2020).
Harries, T. H. et al. Hospital readmissions for COPD: A retrospective longitudinal study. NPJ Prim. Care Respir. Med. 27, 31 (2017).
Hakim, M. A., Garden, F. L., Jennings, M. D. & Dobler, C. C. Performance of the LACE index to predict 30-day hospital readmissions in patients with chronic obstructive pulmonary disease. Clin. Epidemiol. 10, 51 (2018).
Gao, C., Xu, F. & Liu, G. G. Payment reform and changes in health care in China. Soc. Sci. Med. 111, 10 (2014).
Liang, L. et al. Trends in hospitalization expenditures for acute exacerbations of COPD in Beijing from 2009 to 2017. Int. J. Chron. Obstruct. Pulmon. Dis. 15, 1165 (2020).
Kong, C. W. & Wilkinson, T. Predicting and preventing hospital readmission for exacerbations of COPD. ERJ Open Res. 6, 5550 (2020).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 40, 373 (1987).
Twisk, J. W. R. Applied Longitudinal Data Analysis for Epidemiology: A Practical Guide (Cambridge University Press, 2003).
Chatterjee, K., Goyal, A. & Joshi, M. Thirty-day readmissions in adults hospitalized for COPD or bronchiectasis: Findings from the nationwide readmission database 2013. Chest 151, 943 (2017).
Jacobs, D. M. et al. Early hospital readmissions after an acute exacerbation of chronic obstructive pulmonary disease in the nationwide readmissions database. Ann. Am. Thorac. Soc. 15, 837 (2018).
Graham, K. L. et al. Preventability of early versus late hospital readmissions in a national cohort of general medicine patients. Ann. Intern. Med. 168, 766 (2018).
Guerrero, M. et al. Readmission for acute exacerbation within 30 days of discharge is associated with a subsequent progressive increase in mortality risk in COPD patients: A long-term observational study. PLoS ONE 11, e150737 (2016).
Press, V. G., Konetzka, R. T. & White, S. R. Insights about the economic impact of chronic obstructive pulmonary disease readmissions post implementation of the hospital readmission reduction program. Curr. Opin. Pulm. Med. 24, 138 (2018).
Zuckerman, R. B., Sheingold, S. H., Orav, E. J., Ruhter, J. & Epstein, A. M. Readmissions, observation, and the hospital readmissions reduction program. N. Engl. J. Med. 374, 1543 (2016).
Goto, T. et al. Trends in 30-day readmission rates after COPD hospitalization, 2006–2012. Respir. Med. 130, 92 (2017).
Ford, E. S. Hospital discharges, readmissions, and ED visits for COPD or bronchiectasis among US adults: Findings from the nationwide inpatient sample 2001–2012 and Nationwide Emergency Department Sample 2006–2011. Chest 147, 989 (2015).
Jiang, X., Xiao, H., Segal, R., Mobley, W. C. & Park, H. Trends in readmission rates, hospital charges, and mortality for patients with chronic obstructive pulmonary disease (COPD) in Florida from 2009 to 2014. Clin. Ther. 40, 613 (2018).
de Miguel-Diez, J. et al. Readmissions following an initial hospitalization by COPD exacerbation in Spain from 2006 to 2012. Respirology 21, 489 (2016).
Liang, L. et al. Long-term trends in hospitalization and outcomes in adult patients with exacerbation of chronic obstructive pulmonary disease in Beijing, China, from 2008 to 2017. Int. J. Chron. Obstruct. Pulmon. Dis. 15, 1155 (2020).
Khakban, A. et al. Ten-year trends in direct costs of COPD: A population-based study. Chest 148, 640 (2015).
Deniz, S., Sengul, A., Aydemir, Y., Celdir, E. J. & Ozhan, M. H. Clinical factors and comorbidities affecting the cost of hospital-treated COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 11, 3023 (2016).
Jian, W. et al. Quality of care in large Chinese hospitals: An observational study. BMJ Qual. Saf. 28, 963 (2019).
Ospina, M. B. et al. A systematic review of the effectiveness of discharge care bundles for patients with COPD. Thorax 72, 31 (2017).
WHO. People's Republic of China health system review. Manila: WHO Regional Office for the Western Pacific (2015).
Liang, L. et al. Associations between daily air quality and hospitalisations for acute exacerbation of chronic obstructive pulmonary disease in Beijing, 2013–17: An ecological analysis. Lancet Planet Health 3, e270 (2019).
Li, Y. Q., Shi, J. H., Cao, Y., Qi, L. & Liu, X. R. One year after the implementation of 2015 Tobacco Control Regulation on persons aged 15 years and over tobacco use in Beijing. Zhonghua Liu Xing Bing Xue Za Zhi 39, 1188 (2018).
Chan, F. W. et al. Risk factors of hospitalization and readmission of patients with COPD in Hong Kong population: Analysis of hospital admission records. BMC Health Serv. Res. 11, 186 (2011).
Lin, J. et al. Risk factors associated with chronic obstructive pulmonary disease early readmission. Curr. Med. Res. Opin. 30, 315 (2014).
Alqahtani, J. S. et al. Risk factors for all-cause hospital readmission following exacerbation of COPD: A systematic review and meta-analysis. Eur. Respir. Rev. 29, 558 (2020).
Jia, G., Lu, M., Wu, R., Chen, Y. & Yao, W. Gender difference on the knowledge, attitude, and practice of COPD diagnosis and treatment: A national, multicenter, cross-sectional survey in China. Int. J. Chron. Obstruct. Pulmon. Dis. 13, 3269 (2018).
Chen, Y., Li, Q. & Johansen, H. Age and sex variations in hospital readmissions for COPD associated with overall and cardiac comorbidity. Int. J. Tuberc. Lung Dis. 13, 394 (2009).
Nantsupawat, T., Limsuwat, C. & Nugent, K. Factors affecting chronic obstructive pulmonary disease early rehospitalization. Chron. Respir. Dis. 9, 93 (2012).
Shah, C. H. et al. Economic burden of comorbidities among COPD patients hospitalized for acute exacerbations: An analysis of a commercially insured population. Expert. Rev. Pharmacoecon. Outcomes Res. 22, 683 (2022).
Perera, P. N., Armstrong, E. P., Sherrill, D. L. & Skrepnek, G. H. Acute exacerbations of COPD in the United States: Inpatient burden and predictors of costs and mortality. COPD 9, 131 (2012).
Acknowledgements
We appreciate the data collection team from the Beijing Municipal Health Commission Information Centre.
Funding
This work was supported by grants from the Beijing Municipal Science & Technology Commission (No. Z201100005520028) and the Beijing Municipal Administration of Hospitals Incubating Program (PX2020014). The funders had no role in the study design, data collection, data analysis and interpretation, writing of the report, or the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
L.L., Z.T., and J.L. designed the study. S.C., H.R., L.F., D.Z., S.C., and H.J. acquired or interpreted the data. J.L. and L.L. did the statistical analysis. J.L. drafted the manuscript, and L.L. revised the manuscript. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, J., Liang, L., Cao, S. et al. Secular trend and risk factors of 30-day COPD-related readmission in Beijing, China. Sci Rep 12, 16589 (2022). https://doi.org/10.1038/s41598-022-20884-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-20884-3
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.