Abstract
Anemia is predicted to affect 38% (32 million) of pregnant women worldwide. However, evidence for utilization and compliance with iron supplementation and predictors during pregnancy in low-income countries, including Ethiopia, is sparse and inconclusive. Therefore, we aimed to assess utilization and compliance with iron supplementation and predictors among pregnant women in Robe Town, Southeast Ethiopia. A community-based cross-sectional study was employed among randomly selected 445 pregnant women attending antenatal care at health facilities from May to July 2015. A systematic random sampling was used to select respondents. Data were collected using a pre-tested, interviewer-administered, structured questionnaire. Bivariable and multivariable logistic regression analyses were conducted to identify predictors of compliance with iron supplementation. An odds ratio, along with a 95% confidence interval (CI), was used to estimate the strength of the association. In this study, 54% [95% CI (49.4, 58.4%)], 45.2% [95% CI (40.9, 49.4%)], 4.3% [95% CI (2.5, 6.3%)], and 2.2% [95% CI (1.1, 3.6%)] of women received iron supplements during their first, second, third, and fourth antenatal care visits, respectively. The level of compliance with iron supplementation was 92.4% [95% CI (89.9, 94.6%)]. Having a formal education (AOR = 4.45, 95% CI 1.41, 13.99), being in the high wealth quintile (AOR = 0.18, 95% CI 0.05, 0.68), medium wealth quintile [(AOR = 0.33, 95% CI (0.11, 0.98)], receiving iron supplements for free (AOR = 3.77, 95% CI 1.33, 10.69), not experiencing discomfort related to iron supplements intake (AOR = 2.94, 95% CI 1.17, 7.39), having comprehensive knowledge about anemia (AOR = 2.62, 95% CI 1.02, 6.70), being knowledgeable about iron supplements (AOR = 3.30, 95% CI 1.12, 9.76), having information about importance of iron supplementation during pregnancy (AOR = 2.86; 95% CI 1.04, 7.87), and ever being visited by urban health extension workers (AOR = 0.31; 95% CI 0.12, 0.83) was significantly associated with compliance with iron supplementation during pregnancy. The utilization of iron supplementation during pregnancy was low, with relatively high compliance with the supplements. Thus, comprehensive nutrition education and free provision of iron supplementation are crucial tools to increase utilization and compliance with iron supplementation during pregnancy. Further research with a strong study design using golden standard methods is warranted.
Similar content being viewed by others
Introduction
Iron-deficiency anemia is one of the most common nutritional disorders worldwide, affecting populations in both high-income countries (HICs) and low and middle-income countries (LMICs). Anemia is predicted to affect 38% (32 million) of pregnant women worldwide by 20251. However, the prevalence of anemia is increasing in LMICs with a rate of 35.6–76.7%2,3,4,5. Africa has the highest prevalence of anemia, with 57% of pregnant women6. Several studies carried out in Ethiopia also revealed that the prevalence of anemia among pregnant women ranges from 21 to 54%7,8,9,10,11. Maternal anemia is associated with mortality and morbidity for the mother and baby, including the risk of miscarriages, stillbirths, prematurity, and low birth weight. It impairs children’s development and learning too, further impacting economic productivity and development12.
By 2025, the World Health Organization (WHO) aims to reduce anemia in women of reproductive age by half12. In Ethiopia, nutrition is integrated into the health sector transformation plan in the form of micronutrient interventions to prevent the occurrence of anemia and improve the nutritional condition of mothers during pregnancy13. Maternal and child mortality remain high in Ethiopia, with 412 maternal deaths per 100,000 live births and 67 child deaths per 103 live births reported14. Taking this into account, the Ethiopian government has demonstrated its commitment to averting nutritional problems by adopting food and nutrition policies, strategies, and programs. In addition, the government designed the Seqota declaration to eliminate stunting by 203015. Various factors, such as socio-demographic and health factors, determine the compliance with iron supplementation among pregnant women16. All pregnant women in places where anemia is common should take iron supplements, according to the WHO17. Despite the WHO's recommendation, iron supplementation is nevertheless uncommon in many countries, particularly in those with limited resources18.
The national guideline for the control and prevention of micronutrient deficiencies emphasized the necessity of daily iron supplementation for at least 6 months during pregnancy and 3 months after delivery, in line with WHO recommendations19. By 2015, the national nutrition strategy (NNS) aims to increase to 50% the proportion of women who receive iron supplements for more than 90 days during pregnancy and the postpartum period20.
In the previous 5 years, only 17.3% of women used iron supplements during their most recent pregnancy, and only 0.4% supplemented for 90 days or more. Even though iron supplementation is thought to be an important aspect of prenatal care (ANC), only 37% of women who had ANC received it14. Low adherence has an impact on the level of energy and productivity, cognitive and physical development, and immune function21. Several studies reported that the compliance rate of iron supplements during pregnancy was low. For example, the compliance rates vary from 12 to 93%22,23,24,25,26.
Previous studies have employed a cut-off point of ≥ 90 days to determine adherence to iron supplementation during pregnancy in sub-Saharan Africa (SSA)20,27,28,29,30. However, many women in SSA countries do not take iron supplements because of socio-demographic and economic factors22,27,31,32,33, lack of knowledge about anemia, inadequate supply of iron tablets, poor utilization of ANC services, inability to pay for supplementation, misinformation about the benefit of supplementation, complaints about side effects, forgetfulness, and poor counseling20,27,34,35.
Although prenatal iron supplementation was an integral part of antenatal care and was provided free of charge in Ethiopia, the existing compliance rate of iron supplements varies from 28.1 to 87.6%36,37. Nevertheless, evidence on utilization and compliance with iron supplementation and predictors among pregnant women in low-income countries like Ethiopia, in general, and in the study context, in particular, is sparse and inconclusive. The findings of this study could be used by policymakers to improve utilization and compliance with iron supplementation during pregnancy. Therefore, we aimed to assess the utilization and compliance with iron supplementation and predictors among pregnant women in Robe town, Bale zone, Southeast Ethiopia.
Methods
Study design, area, and participants
A community-based cross-sectional study design was used among pregnant women attending antenatal care at health facilities in Robe Town, Bale Zone, Southeast Ethiopia from May to July 2015. The majority of the inhabitants were Muslim (48%), Orthodox (45%), and Protestant (6%). There was one government district hospital. Besides, there were 15 private clinics, 12 drug vendors, and one health center. Five of the 12 drug vendors served rural areas. All health facilities provide antenatal care (ANC) visits. There were also primary and secondary schools, a teachers' training college, and Madda Walabu University in the town. The Robe was entirely engulfed by peasant associations. The child-bearing age women counted were 13,685. The estimated number of pregnant women was 214638,39.
All pregnant women who attended the ANC clinic were the source population. All randomly selected pregnant women attending the ANC clinic who fulfilled the inclusion criteria and who received the iron supplement for at least 1 month before the date of interview were included in the study. Pregnant women who did not respond to the interview questions due to severe psychiatric illness, were unable to speak or hear, were excluded from the study.
Sample size determination and sampling techniques
The sample size was calculated using the G-power software version 3.1, assuming an effect size of 0.25, a 95% confidence interval, a precision of 0.05, and a power (1 − β) of 80%40. The computed sample size was 206. Using a design effect of 2 and adding a 10% non-response rate, the final sample size was 454.
The three kebeles (the smallest administrative unit in Ethiopia) were selected at random and their respective numbers of pregnant women were obtained from the study town health office. Then, the sample size was proportionally allocated to each kebele, and the pregnant women were selected using a systematic random sampling technique. In the event that two pregnant women were present in the house, we used the lottery method to select the pregnant women. If a woman was absent from her house during the interview, an eligible pregnant woman in the next house in serial number was interviewed. The house of an absent pregnant woman was revisited the next day.
Data collection
An interviewer-administered, structured questionnaire was used to collect data. The questionnaire was comprised of questions related to socio-demographic and economic factors such as age, marital status, religion, ethnic group, head of household, occupation of the women and husband, educational status of women and husband, wealth index, and family size.
Iron supplements and health-related factors included the experience of discomfort related to iron supplement intake encountered, a dose of iron supplement, knowledge of anemia's causes, symptoms, and prevention, knowledge of iron supplements, beliefs that iron supplement intake may harm the fetus, ever forgotten iron supplement intake, knowledge of anemia, information about iron supplementation, and source of information. Questions related to health care delivery system-related factors were: a source of iron supplement distance from the nearest health facility urban health extension worker visit and ANC services. Obstetric-related factors were also birth order, intended pregnancy, gestational age, the experience of serious pregnancy-related complications, and parity.
To ensure the quality of the data, the questionnaire was initially developed in English and then translated into the local language "Afan Oromo" and back-translated into English by independent language experts to ensure its consistency. The questionnaire was also pretested on 5% of the total estimated sample size, having similar characteristics to the study population in a different adjacent setting. The authors and statistician reviewed the completed questionnaire to ensure its validity in terms of content. Finally, we modified the items in light of the findings of the pre-test and expert reviews. The training was given to data collectors, level IV nurses, and supervisors on the objectives of the study, data collection instruments, and principles of research ethics to minimize interviewers' bias. Data supervisors closely supervised the data collectors daily for the successful completion of the questionnaire and timely action otherwise. The study participants were interviewed at their homes to improve the response rate.
Operational definitions
Utilization of iron supplementation and compliance with iron supplements during pregnancy were outcome variables. In this study, the utilization of iron supplementation during pregnancy was determined by the proportion of pregnant women who had been supplemented previously for at least 1 month before the date of the interview. It was measured by how many pregnant women used iron supplements. Compliance with/adherence to iron supplements during pregnancy was understood in such a way that a pregnant woman was said to be compliant with/adherent to iron supplements if she took the supplement for at least 4 days a week during pregnancy in the previous month preceding the survey; otherwise, they were classified as non-compliant/adherent to iron supplements. Self-report compliance/adherence was estimated by asking a woman how many times she took a supplement per week in the previous time6,41,42.
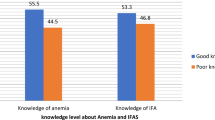
Comprehensive knowledge of anemia during pregnancy was measured in this study in which respondents who were aware of anemia and knew at least one of its major causes, symptoms, and consequences during pregnancy were said to be knowledgeable about anemia. On the contrary, knowledge of iron supplementation was measured based on a set of four questions including (1) awareness of iron supplementation in pregnancy, (2) reasons for iron supplementation, (3) possible side effects of oral iron preparation on women, and (4) possible effects of iron deficiency. Respondents who correctly answered 3 or 4 of the above questions were considered to have good knowledge of anemia during pregnancy, whereas those who answered two or fewer correctly were said to have poor knowledge24.
The knowledge of iron supplementation during pregnancy was based on the participants' responses to a set of four questions, including (1) awareness of iron supplementation in pregnancy, (2) reasons for iron supplementation, (3) possible side effects of oral iron preparation on the women, and (4) possible effects of iron deficiency on pregnancy. Respondents who answered correctly to 3 or 4 of the above questions were considered to have good knowledge of iron supplementation in pregnancy, whereas those who answered correctly to two or fewer were said to have poor knowledge24.
The economic status of respondents was ranked and ordered into tertiles as rich, medium, and poor using the wealth index. The wealth index was assessed by computing principal component analysis using household asset items and other variables14.
Statistical analysis
Data were checked for completeness, consistency, and accuracy. Then, the data were entered, cleaned, and analyzed using SPSS version 20 computer software. Descriptive statistics such as frequencies, percentages, and means were computed for selected explanatory variables. The normality of the data distribution was assessed using the Kolmogorov–Smirnov test. A bivariable logistic regression analysis was conducted to see the association between each predictor and compliance with iron supplements (Yes = 1, No = 0). Variables with a p-value of ≤ 0.25 were included in multivariable logistic regression analyses to control for all possible confounder effects. Multicollinearity was tested among all independent variables using a correlation matrix (R). The highest correlation between the independent variables was 0.16, which was below the cut-off points. The crude odds ratio (COR) and adjusted odds ratio (AOR) were conducted to estimate the strength of the association between the predictors and the outcome variable. The goodness of fit of the final logistic model was tested using the Hosmer and Lemeshow's test at a p-value of greater than 0.05. The statistical significance of the association was declared at a p-value of less than 0.05.
Ethical considerations
The current study was ethically approved by the Institutional Review Board of Hawassa University before the start of the study (Protocol Number: IRB/07/07). A permission letter was obtained from the Bale Zone and Robe district health offices. All methods were performed in accordance with the relevant tenets of the Helsinki Declaration43. Informed written consent was obtained from each respondent. The privacy of the respondents was respected. Confidentiality was maintained throughout the entire process of data collection and management.
Results
Socio-demographic and economic characteristics
A total of 445 out of 454 pregnant women, were included in the study, yielding a response rate of 98%. Nearly half 214 (48%) of pregnant women were less than or equal to 24 years of age, with a mean (± SD) age of 25 (± 5.42) years. Almost all (98%) of the pregnant women were married, and half of them were Muslims. The majority of the respondents (82.5%) were from the Oromo ethnic group. Half of the households were headed by husbands. More than half (58.4%) of the respondents were housewives, whereas (2.7%) were farmers. The majority of the respondents (94.6%) were literate, and about (30.8%) of the households had high wealth quintiles (Table 1).
Utilization of iron supplements during pregnancy
Out of 445 pregnant women who were enrolled in the study, 54%; 95% CI (49.4, 58.4%), 45.2%; 95% CI (40.9, 49.4%), 4.3%; 95% CI (2.5, 6.3%), and 2.2%; 95% CI (1.1, 3.6%) of women received iron supplements during their first, second, third, and fourth antenatal care visits, respectively. Of 445 pregnant women who were given iron supplements, 46.7%; 95% CI (42.2, 51.5%), 33.9%; 95% CI (29, 37.8%), 18.2%; 95% CI (14.4, 22.2%), and 1.1%; 95% CI (0.2, 2.2%) of them received iron supplements for 30 days, 31–60 days, 61–90 days, and more than 90 days, respectively (Fig. 1).
Compliance with iron supplements during pregnancy
The rate of compliance with iron supplementation during pregnancy was found to be 92.4%; 95% CI (89.9, 94.6%).
Predictors of compliance with iron supplements during pregnancy
In multivariable logistic regression analysis, women’s literacy (AOR = 4.45, 95% CI 1.41, 13.99), the medium (AOR = 0.33, 95% CI 0.11, 0.98), and high (AOR = 0.18, 95% CI 0.04, 0.68) wealth quintiles, absence of discomfort or adverse effects related to iron supplements (AOR = 2.94, 95% CI 1.17, 7.39), women’s having comprehensive knowledge of anemia (AOR = 2.62, 95% CI 1.02, 6.70) and having good knowledge of iron supplements (AOR = 3.30, 95% CI 1.12, 9.76), having information about the importance of iron supplementation (AOR = 2.86, 95% CI 1.04, 7.87), being visited by urban health extension workers (AOR = 0.31, 95% CI 0.12, 0.83) were found to be significant predictors of compliance with iron supplements during pregnancy (Table 2).
Discussion
The objective of this study was to assess utilization and compliance with iron supplementation and predictors among pregnant women. The overall utilization of iron supplementation during pregnancy was low, with a relatively high level of compliance with the supplements. Maternal formal education, knowing anemia and the importance of iron supplementation during pregnancy, not experiencing side effects related to iron tablets, and getting iron for free have positively influenced compliance with iron supplementation during pregnancy. On the other hand, having high/medium wealth quintiles and being visited by urban health extension workers were negatively associated with compliance with iron supplementation during pregnancy.
Accordingly, of pregnant women who were given iron supplements, 46.7%, 33.9%, 18.2%, and 1.1% received iron supplements for 30 days, 31–60 days, 61–90 days, and more than 90 days, respectively. This study’s finding was argued with a study conducted in Ethiopia20. However, fewer than one in twenty pregnant women (3.5%) took the supplements for more than 90 days. Besides, the utilization of iron supplementation was disappointingly low, as only 17.3% of women took the supplements during their most recent pregnancy in the preceding 5 years, and only 0.4% were supplemented for 90 or more days14. This could be due to the difference in the educational status of respondents and access to iron supplements.
In this study, the overall compliance rate of iron supplementation during pregnancy was found to be 92.4%. The current finding was higher than many previous reports in Ethiopia, such as the compliance rate, which varied from 60 to 63.6% in Addis Ababa32,44,45, 87.6% in Ethiopia37, Dire Dawa46, Shalla District47, 43.4% Dilla town48, 38.3% Hadassah28, 51.4% Burin district49, 52.9% Debbie50, 28.1% Denbiya District36, 28.7% Lay Armachiho31, 55% Gondar51, 47.6% Aykal town30, 44% Debre Tabor52, 43% Wollo53 and 74.9% in four regions of Ethiopia20, 67.6% Simada district54, 52.8% Debay Tilat Gen district55, 37.2% Northwestern zone of Ethiopia35, 55.5% Debre Markos town56, 76.9% Dangila, Northern Ethiopia57, 40.9% in Adwa town58, and meta-analyses, 46.15, 46.1, 41.38 and 43.63%59,60,61,62. The present finding was also higher than many others, for example, a meta-analysis in SSA63, Uganda64, Kenya65, Nigeria24, Northwest Tanzania66, Northern Tanzania67, 22 sub-Saharan African countries23, Niger68, West Iran69, Cambodia34, Nepal70,71, India72, and Sri Lanka73. Likewise, the current finding was higher than the study finding conducted in a high-income country (HIC) in which the compliance rate was 85% in Sweden74. However, the current finding was lower than the report from South Africa26 in which the compliance rate was 93%. This might be because of variation in the educational status of respondents and self-reporting as education increases pregnant women’s ability to easily access information dissemination and media outlets.
Educated pregnant women were 4.45 times more compliant with iron supplementation during pregnancy as compared to illiterate pregnant women. The current finding was agreed with studies conducted in Addis Ababa44, Denbiya District36, Lay Armachiho31, Debre Markos Town56, a meta-analysis in Ethiopia61. This might be because educated pregnant women were more likely to appreciate the benefits of iron supplementation in pregnancy and hence more likely to comply with the prescription. Nonetheless, the present study’s results were claimed by a study conducted in Ethiopia20. Similarly, the current study was supported by a study conducted in Burji Districts49. The possible explanation could be for a variety of reasons, despite the pregnant women's living in different settings. Furthermore, the findings of this study agreed with those of 22 subSaharan African23, Nigeria24, West Iran69, Nepal70, and Urban Slum25. This could be because educated pregnant women understand the benefits of iron supplementation as well as the risks that occur in the absence of iron supplementation and are therefore more compliant with iron supplementation in pregnancy. Nevertheless, the current study claims to be a study carried out in India72.
Pregnant women who had high wealth quintiles were 82% less likely to be compliant with iron supplementation as compared to pregnant women who had low wealth quintiles. The present study's results were agreed with those of a study conducted in Ethiopia20. The current study's findings are supported by studies conducted in the Northwest, Ethiopia31, and Nepal70. This could probably be because pregnant women who were socio-economically empowered thought that iron supplement intake affected them or their fetuses. However, this study disagreed with a study carried out in 22 SSA countries23. The possible explanation might be that pregnant women who had high wealth quantiles received information from a media outlet and understood the benefit of iron.
Pregnant women who got free iron supplements from government hospitals or health centers were 3.77 times more likely to be compliant with iron supplementation as compared to those who bought iron supplements from a private pharmacy. This current study’s results agreed with those of a study conducted in Senegal75. This could be because of socioeconomic status.
Pregnant women who had not experienced discomfort related to iron supplement intake were 2.94 times more compliant with iron supplementation during pregnancy as compared to pregnant women who had experienced discomfort related to iron supplement intake. The present finding agrees with a study carried out in Nigeria24. The possible explanation might be that educated pregnant women understand the benefits of iron supplementation and the consequences of anemia during pregnancy.
Nevertheless, this current study result was argued with a study conducted in Bangladesh76, Iran77, and Thailand78 which indicated that gastrointestinal side effects were not significantly associated with compliance. This discrepancy could be because of cultural beliefs.
Pregnant women who had comprehensive knowledge of anemia were 2.62 times more likely to be compliant with iron supplement intake as compared to pregnant women who didn't have comprehensive knowledge of anemia. The present study supported a study conducted in four regions of Ethiopia20. Likewise, the current study findings agreed with several studies carried out in Northwest Ethiopia50, Aykal Town30, North Wollo Zone53, and Ethiopia60,61. The probable reason could be the awareness and educational status of the respondents.
Pregnant women who got free iron supplements from government hospitals or health centers were 3.77 times more likely to be compliant with iron supplementation as compared to those who bought iron supplements from a private pharmacy. This current study’s results agreed with those of a study conducted in Senegal75. This could be because of socioeconomic status.
Pregnant women who had not experienced discomfort related to iron supplement intake were 2.94 times more compliant with iron supplementation during pregnancy as compared to pregnant women who had experienced discomfort related to iron supplement intake. The present finding agrees with a study carried out in Nigeria24. The possible explanation might be that educated pregnant women understand the benefits of iron supplementation and the consequences of anemia during pregnancy.
Nevertheless, this current study result was argued with a study conducted in Bangladesh76, Iran77, and Thailand78 which indicated that gastrointestinal side effects were not significantly associated with compliance. This discrepancy could be because of cultural beliefs.
Pregnant women who had comprehensive knowledge of anemia were 2.62 times more likely to be compliant with iron supplement intake as compared to pregnant women who didn't have comprehensive knowledge of anemia. The present study supported a study conducted in 4 regions of Ethiopia20. Likewise, the current study agreed with several studies carried out in Northwest Ethiopia50, Aykal town30, North Wollo Zone53, and Ethiopia60,61. The probable reasons could be because of the awareness and educational status of the respondents. The current study’s findings were also supported by studies in SSA63, Northwest Tanzania66, and Cambodia34. The possible explanation could be that knowledge helps a woman have a good perception of the advantages of taking an iron supplement.
Pregnant women who had good knowledge of iron supplementation were 3.30 times more likely to be compliant with iron supplements as compared to pregnant women who had poor knowledge of iron supplementation. This current study was agreed with several studies carried out in Burji District49, West Dembia, Ethiopia50, Aykal town30, North Wollo zone53, Debre Tabor52, Debre Markos town56, Ethiopia60,61. Likewise, the current study supported studies conducted in SSA63, Kenya65, Nigeria24, Muntinlupa, and the Philippines79. Pregnant women who had good knowledge of iron supplementation might be more likely to receive information about iron supplements and understand education messages delivered via different media outlets.
Pregnant women who had information about the importance of iron supplementation during pregnancy were 2.86 times more compliant with iron supplementation as compared to pregnant women who had not gotten information about the importance of iron supplementation during pregnancy. The current study agreed with the studies conducted in Akaki Kality32, Hawassa28, Debre Tabor52, Aykal Town30, North Wollo zone53, meta-analyses in Ethiopia59,60,61, a study of four regions of Ethiopia20, and Adwa Town58. The possible explanation might be that pregnant women who received information about iron supplements have increased their knowledge, attitude, and behavior.
A study conducted in SSA63, Uganda22, North West Tanzania66, and Iran77 found that most women received information on anemia and iron supplementation from health workers rather than other information sources such as the media, but their knowledge was still low regardless of the training.
Strength and limitations
This study used a community-based cross-sectional study, and it was representative of the source population. On the other hand, recall bias might occur due to self-reporting because the gold standard (like biochemical and stool tests) had not been used, and this might have underestimated or overestimated the utilization and compliance with iron supplementation during pregnancy. The findings of this study might not be representative of the country. Since this study used a cross-sectional study, it could not establish a cause-effect relationship.
Conclusion
This study demonstrated that the utilisation of iron supplementation during pregnancy was low, with a high level of compliance with the supplements. It was also revealed that the most common types of discomfort experienced by pregnant women who took iron supplements were gastric burning and headaches. The study also identified that being literate women, being free of charge iron supplements, not experiencing discomfort related to iron supplement intake, having comprehensive knowledge of anemia, having good knowledge of iron supplementation, and information about the importance of iron supplementation during pregnancy were factors significantly affecting compliance with iron supplementation during pregnancy. However, high wealth quintiles, medium wealth quintiles, and ever being visited by urban health extension workers were less likely to be associated with compliance with iron supplementation during pregnancy. The proper delivery of training to pregnant women on anemia causes, symptoms, consequences, and prevention, as well as the benefits of iron supplementation, is crucial. There should be a continuous and timely provision of iron supplements for health facilities. The findings of this study have implications for clinicians and policymakers. Further research with a strong study design using golden standard methods is warranted.
Data availability
All the relevant information is within this manuscript.
References
Organization, W. H. The global prevalence of anaemia in 2011. (World Health Organization, 2015).
Haider, B. A. et al. Anaemia, prenatal iron use, and risk of adverse pregnancy outcomes: Systematic review and meta-analysis. BMJ 346, f3443. https://doi.org/10.1136/bmj.f3443 (2013).
Fowkes, F. J. I. et al. Iron deficiency during pregnancy is associated with a reduced risk of adverse birth outcomes in a malaria-endemic area in a longitudinal cohort study. BMC Med. 16, 156. https://doi.org/10.1186/s12916-018-1146-z (2018).
Adam, I., Ibrahim, Y. & Elhardello, O. Prevalence, types and determinants of anemia among pregnant women in Sudan: A systematic review and meta-analysis. BMC Hematol. 18, 31. https://doi.org/10.1186/s12878-018-0124-1 (2018).
Fite, M. B., Assefa, N. & Mengiste, B. Prevalence and determinants of Anemia among pregnant women in sub-Saharan Africa: A systematic review and Meta-analysis. Arch. Public Health 79, 219. https://doi.org/10.1186/s13690-021-00711-3 (2021).
Organization, W. H. Guideline: Daily iron and folic acid supplementation in pregnant women. (World Health Organization, 2012).
Kefiyalew, F., Zemene, E., Asres, Y. & Gedefaw, L. Anemia among pregnant women in Southeast Ethiopia: Prevalence, severity and associated risk factors. BMC Res. Notes 7, 771. https://doi.org/10.1186/1756-0500-7-771 (2014).
Getahun, W., Belachew, T. & Wolide, A. D. Burden and associated factors of anemia among pregnant women attending antenatal care in southern Ethiopia: Cross sectional study. BMC Res. Notes 10, 276. https://doi.org/10.1186/s13104-017-2605-x (2017).
Alem, M. et al. Prevalence of anemia and associated risk factors among pregnant women attending antenatal care in Azezo Health Center Gondar town, Northwest Ethiopia. J. Interdiscip. Histopathol. 1, 137–144 (2013).
Getachew, M., Yewhalaw, D., Tafess, K., Getachew, Y. & Zeynudin, A. Anaemia and associated risk factors among pregnant women in Gilgel Gibe dam area, Southwest Ethiopia. Parasit Vectors 5, 296. https://doi.org/10.1186/1756-3305-5-296 (2012).
Obse, N., Mossie, A. & Gobena, T. Magnitude of anemia and associated risk factors among pregnant women attending antenatal care in Shalla Woreda, West Arsi Zone, Oromia Region, Ethiopia. Ethiop. J. Health Sci. 23, 165–173 (2013).
Organization, W. H. (WHO/NMH/NHD/14.4)[cited 2020 Feb 20]. Available at: https://apps.who.int).
The Federal Democratic Republic of Ethiopia. Ministry of Health. Health sector Transformation Plan, 2015/16-2019/20.
Federal Democratic Republic of Ethiopia, Central Statistical Agency Ethiopia Demographic and Health Survey, Addis Ababa, Ethiopia. The DHS Program ICF Rockville, Maryland, USA, 2017.
Ministry of Health, F. D. R. O. E. National Nutrition Program Multi-sectoral Implementation Guide. Addis Ababa: 2016. (2016).
Leung, B. M. & Kaplan, B. J. Perinatal depression: Prevalence, risks, and the nutrition link—A review of the literature. J. Am. Diet. Assoc. 109, 1566–1575 (2009).
Organization, W. H. Weekly Iron-Folic Acid Supplementation (WIFS) in women of reproductive age: Its role in promoting optimal maternal and child health. (World Health Organization, 2009).
Maina-Gathigi, L., Omolo, J., Wanzala, P., Lindan, C. & Makokha, A. Utilization of folic acid and iron supplementation services by pregnant women attending an antenatal clinic at a regional referral hospital in Kenya. Matern. Child Health J. 17, 1236–1242 (2013).
Federal Ministry of Health, Ethiopia. Guidelines for the prevention and control of micronutrient deficiencies (2016).
Gebremedhin, S., Samuel, A., Mamo, G., Moges, T. & Assefa, T. Coverage, compliance and factors associated with utilization of iron supplementation during pregnancy in eight rural districts of Ethiopia: A cross-sectional study. BMC Public Health 14, 1–8 (2014).
Rahmati, S., Delpisheh, A., Parizad, N. & Sayehmiri, K. Maternal anemia and pregnancy outcomes: A systematic review and meta-analysis. Int. J. Pediatr. 4, 3323–3342 (2016).
Kiwanuka, T. S., Ononge, S., Kiondo, P. & Namusoke, F. Adherence to iron supplements among women receiving antenatal care at Mulago National Referral Hospital Uganda-cross-sectional study. BMC Res. Notes 10, 510. https://doi.org/10.1186/s13104-017-2834-z (2017).
Ba, D. M. et al. Adherence to iron supplementation in 22 Sub-Saharan African countries and associated factors among pregnant women: A large population-based study. Curr. Dev. Nutr. 3, nzz120. https://doi.org/10.1093/cdn/nzz120 (2019).
Ugwu, E., Olibe, A., Obi, S. & Ugwu, A. Determinants of compliance to iron supplementation among pregnant women in Enugu, Southeastern Nigeria. Niger. J. Clin. Pract. 17, 608–612 (2014).
Dutta, A. J., Patel, P. & Bansal, R. Compliance to iron supplementation among pregnant women: A cross sectional study in urban slum. Natl. J. Commun. Med. 5, 457–462 (2014).
Mbhenyane, X. & Cherane, M. Compliance with the consumption of iron and folate supplements by pregnant women in Mafikeng local municipality, North West province, South Africa. Afr. Health Sci. 17, 657–670. https://doi.org/10.4314/ahs.v17i3.8 (2017).
Titilayo, A., Palamuleni, M. E. & Omisakin, O. Sociodemographic factors influencing adherence to antenatal iron supplementation recommendations among pregnant women in Malawi: Analysis of data from the 2010 Malawi Demographic and Health Survey. Malawi Med. J. 28, 1–5. https://doi.org/10.4314/mmj.v28i1.1 (2016).
Kassa, Z. Y., Awraris, T., Daba, A. K. & Tenaw, Z. Compliance with iron folic acid and associated factors among pregnant women through pill count in Hawassa city, South Ethiopia: A community based cross-sectional study. Reprod. Health 16, 1–8 (2019).
Haile, M., Jeba, A. & Hussen, M. Compliance to prenatal iron and folic acid supplement and associated factors among women during pregnancy in South East Ethiopia: A cross-sectional study. J. Nutr. Health Food Eng. 7, 272–277 (2017).
Assefa, H., Abebe, S. M. & Sisay, M. Magnitude and factors associated with adherence to Iron and folic acid supplementation among pregnant women in Aykel town, Northwest Ethiopia. BMC Pregnancy Childbirth 19, 1–8 (2019).
Agegnehu, G., Atenafu, A., Dagne, H. & Dagnew, B. Adherence to iron and folic acid supplement and its associated factors among antenatal care attendant mothers in lay armachiho health centers, Northwest, Ethiopia, 2017. Int. J. Reprod. Med. 2019, 5863737. https://doi.org/10.1155/2019/5863737 (2019).
Gebreamlak, B., Dadi, A. F. & Atnafu, A. High adherence to iron/folic acid supplementation during pregnancy time among antenatal and postnatal care attendant mothers in Governmental Health Centers in Akaki Kality Sub City, Addis Ababa, Ethiopia: Hierarchical negative binomial poisson regression. PLoS ONE 12, e0169415 (2017).
Warvadekar, K., Reddy, J., Sharma, S., Dearden, K. A. & Raut, M. K. Socio-demographic and economic determinants of adherence to iron intake among pregnant women in selected low and lower middle income countries in Asia: Insights from a cross-country analyses of global demographic and health surveys. Int. J. Commun. Med. Public Health 5, 1552–1569 (2018).
Lacerte, P., Pradipasen, M., Temcharoen, P., Imamee, N. & Vorapongsathorn, T. Determinants of adherence to iron/folate supplementation during pregnancy in two provinces in Cambodia. Asia Pac. J. Public Health 23, 315–323 (2011).
Gebre, A., Mulugeta, A. & Etana, B. Assessment of factors associated with adherence to iron-folic acid supplementation among urban and rural pregnant women in North Western Zone of Tigray, Ethiopia: Comparative Study. Int. J. Nutr. Food Sci. 4, 161 (2015).
Tarekegn, M., Wubshet, M., Atenafu, A., Derso, T. & Woretaw, A. Antenatal care and mothers’ education improved iron-folic acid adherence at Denbiya district health centers, Northwest Ethiopia: Using pills count method. Arch. Public Health 77, 30. https://doi.org/10.1186/s13690-019-0356-y (2019).
Tadesse, A. W., Aychiluhm, S. B. & Mare, K. U. Individual and community-level determinants of iron-folic acid intake for the recommended period among pregnant women in Ethiopia: A multilevel analysis. Heliyon 7, e07521. https://doi.org/10.1016/j.heliyon.2021.e07521 (2021).
The National Regional Government of Oromia Bureau of Finance and Economic Development. Condensed Physical Geography of Oromia (2012).
Robe Town Health Office. Robe Health Office Annual Report (2016).
Faul, F., Erdfelder, E., Lang, A. G. & Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39, 175–191. https://doi.org/10.3758/bf03193146 (2007).
Prevention., C. f. D. C. a. Pregnancy risk assessment monitoring system (PRAMS), phase 5 standard questions. http://www.prams.org.com/ (2007).
Organization, W. H. Developing and validating an iron and folic acid supplementation indicator for tracking progress towards global nutrition monitoring framework targets: Final report June 2018. (2018).
World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. Jama 310, 2191–2194. https://doi.org/10.1001/jama.2013.281053 (2013).
Nasir, B. B., Fentie, A. M. & Adisu, M. K. Adherence to iron and folic acid supplementation and prevalence of anemia among pregnant women attending antenatal care clinic at Tikur Anbessa Specialized Hospital, Ethiopia. PLoS ONE 15, e0232625. https://doi.org/10.1371/journal.pone.0232625 (2020).
Tegodan, E., Tura, G. & Kebede, A. Adherence to iron and folic acid supplements and associated factors among pregnant mothers attending ANC at gulele sub-city government health centers in addis ababa, Ethiopia. Patient Prefer Adher. 15, 1397–1405. https://doi.org/10.2147/ppa.S301630 (2021).
Solomon, Y., Sema, A. & Menberu, T. Adherence and associated factors to iron and folic acid supplementation among pregnant women attending antenatal care in public hospitals of Dire Dawa, Eastern Ethiopia. Eur. J. Midwifery 5, 35. https://doi.org/10.18332/ejm/138595 (2021).
Kedir Obsa, A., Tegene, Y. & Gebretsadik, A. Iron and folic acid supplementation compliance and associated factors among pregnant women attending antenatal clinic in Shalla District, Southwest Ethiopia: A cross-sectional Study. J. Nutr. Metab. 2021, 6655027. https://doi.org/10.1155/2021/6655027 (2021).
Mamo, T. T., Ashenafi, E., Gube, A. A. & Bekele, T. Adherence to prenatal iron–folic acid supplementation and associated factors among pregnant women attending antenatal care services in Dilla town, South Ethiopia. Med. @ Access Point Care 5, 23992026211008804 (2021).
Boti, N. et al. Adherence to iron-folate supplementation and associated factors among pastoralist’s pregnant women in Burji districts, Segen area People’s zone, southern Ethiopia: Community-based cross-sectional study. Int. J. Reprod. Med. 2018, 1 (2018).
Molla, T., Guadu, T., Muhammad, E. A. & Hunegnaw, M. T. Factors associated with adherence to iron folate supplementation among pregnant women in West Dembia district, northwest Ethiopia: A cross sectional study. BMC. Res. Notes 12, 1–6 (2019).
Birhanu, T. M., Birarra, M. K. & Mekonnen, F. A. Compliance to iron and folic acid supplementation in pregnancy, Northwest Ethiopia. BMC Res. Notes 11, 1–5 (2018).
Gebremariam, A. D., Tiruneh, S. A., Abate, B. A., Engidaw, M. T. & Asnakew, D. T. Adherence to iron with folic acid supplementation and its associated factors among pregnant women attending antenatal care follow up at Debre Tabor General Hospital, Ethiopia, 2017. PLoS ONE 14, e0210086 (2019).
Demis, A., Geda, B., Alemayehu, T. & Abebe, H. Iron and folic acid supplementation adherence among pregnant women attending antenatal care in North Wollo Zone northern Ethiopia: Institution based cross-sectional study. BMC. Res. Notes 12, 1–7 (2019).
Mekonnen, A., Alemnew, W., Abebe, Z. & Demissie, G. D. Adherence to iron with folic acid supplementation among pregnant women attending antenatal care in public health centers in Simada District, Northwest Ethiopia: Using health belief model perspective. Patient Prefer. Adher. 15, 843–851. https://doi.org/10.2147/ppa.S299294 (2021).
Demisse, B., Temesgen, H., Dessie, B. & Kassa, G. M. Adherence status to iron with folic acid supplementation and associated factors among pregnant women receiving antenatal care at public health facilities in Northwest Ethiopia. SAGE Open Med. 9, 20503121211049936 (2021).
Mekonnen, B. A., Dessie, Y., Baraki, N., Oumer, A. & Gebru, M. Adherence to iron and folic acid supplementation and associated factors among antenatal care attendants in Northwest Ethiopia. Int. J. Public Health Sci. 9, 20–28. https://doi.org/10.11591/ijphs.v9i1.20385 (2020).
Asres, A. W., Hunegnaw, W. A., Ferede, A. G. & Azene, T. W. Compliance level and factors associated with iron-folic acid supplementation among pregnant women in Dangila, Northern Ethiopia: A cross-sectional study. SAGE Open Med. 10, 20503121221118988. https://doi.org/10.1177/20503121221118989 (2022).
Gebremichael, T. G. & Welesamuel, T. G. Adherence to iron-folic acid supplement and associated factors among antenatal care attending pregnant mothers in governmental health institutions of Adwa town, Tigray, Ethiopia: Cross-sectional study. PLoS ONE 15, e0227090. https://doi.org/10.1371/journal.pone.0227090 (2020).
Desta, M. et al. Adherence of iron and folic acid supplementation and determinants among pregnant women in Ethiopia: A systematic review and meta-analysis. Reprod. Health 16, 182. https://doi.org/10.1186/s12978-019-0848-9 (2019).
Fite, M. B. et al. Compliance with iron and folic acid supplementation and associated factors among pregnant women in Ethiopia: A systematic review and meta-analysis. Int. J. Sci. Rep. 6, 514. https://doi.org/10.18203/issn.2454-2156.IntJSciRep20205031 (2020).
Sendeku, F. W., Azeze, G. G. & Fenta, S. L. Adherence to iron-folic acid supplementation among pregnant women in Ethiopia: A systematic review and meta-analysis. BMC Pregnancy Childbirth 20, 1–9 (2020).
Workineh, Y., Semachew, A., Ayalew, E. & Temesgen, W. A. Compliance to iron-folic acid supplementation and its association with the number of ANC visits in Ethiopia: Systematic review and meta-analysis. Adv. Prev. Med. 2019, 3602585. https://doi.org/10.1155/2019/3602585 (2019).
Fite, M. B., Roba, K. T., Oljira, L., Tura, A. K. & Yadeta, T. A. Compliance with iron and folic acid supplementation (IFAS) and associated factors among pregnant women in Sub-Saharan Africa: A systematic review and meta-analysis. PLoS ONE 16, e0249789. https://doi.org/10.1371/journal.pone.0249789 (2021).
Nimwesiga, C., Murezi, M. & Taremwa, I. M. Adherence to iron and folic acid supplementation and its associated factors among pregnant women attending antenatal care at bwindi community hospital, Western Uganda. Int. J. Reprod. Med. 2021, 6632463. https://doi.org/10.1155/2021/6632463 (2021).
Kamau, M. W., Mirie, W. & Kimani, S. Compliance with Iron and folic acid supplementation (IFAS) and associated factors among pregnant women: Results from a cross-sectional study in Kiambu County, Kenya. BMC Public Health 18, 1–10 (2018).
Lyoba, W. B., Mwakatoga, J. D., Festo, C., Mrema, J. & Elisaria, E. Adherence to iron-folic acid supplementation and associated factors among pregnant women in Kasulu communities in North-Western Tanzania. Int. J. Reprod. Med. 2020, 3127245. https://doi.org/10.1155/2020/3127245 (2020).
Ogundipe, O. et al. Factors associated with prenatal folic acid and iron supplementation among 21,889 pregnant women in Northern Tanzania: A cross-sectional hospital-based study. BMC Public Health 12, 1–10 (2012).
Begum, K. et al. Prevalence of and factors associated with antenatal care seeking and adherence to recommended iron-folic acid supplementation among pregnant women in Zinder, Niger. Matern. Child Nutr. https://doi.org/10.1111/mcn.12466 (2018).
Siabani, S. et al. Determinants of compliance with iron and folate supplementation among pregnant women in West Iran: A population based cross-sectional study. J. Family Reprod. Health 12, 197–203 (2018).
Neupane, N., Sharma, S. & Kaphle, H. P. Factors affecting compliance of iron and folic acid among pregnant women attaining Western Regional Hospital, Pokhara, Nepal. Int. J. Res. Curr. Dev. 1, 43–47 (2015).
Yadav, K. D., Yadav, U. N., Wagle, R. R., Thakur, D. N. & Dhakal, S. Compliance of iron and folic acid supplementation and status of anaemia during pregnancy in the Eastern Terai of Nepal: Findings from hospital based cross sectional study. BMC Res Notes 12, 127. https://doi.org/10.1186/s13104-019-4167-6 (2019).
Debi, S. et al. Compliance to iron-folic-acid supplementation and associated factors among pregnant women: A cross-sectional survey in a district of West Bengal, India. J. Family Med. Primary Care 9, 3613–3618. https://doi.org/10.4103/jfmpc.jfmpc_392_20 (2020).
Pathirathna, M. L., Wimalasiri, K. M. S., Sekijima, K. & Sadakata, M. Maternal compliance to recommended iron and folic acid supplementation in pregnancy, Sri Lanka: A hospital-based cross-sectional study. Nutrients 12, 3266. https://doi.org/10.3390/nu12113266 (2020).
Wulff, M. & Ekström, E. C. Iron supplementation during pregnancy in Sweden: To what extent is the national recommendation followed? Acta Obstet, Gynecol, Scand, 82, 628–635. https://doi.org/10.1034/j.1600-0412.2003.00186.x (2003).
Seck, B. C. & Jackson, R. T. Determinants of compliance with iron supplementation among pregnant women in Senegal. Public Health Nutr. 11, 596–605 (2008).
Hyder, S. Z., Persson, L. Å., Chowdhury, A. & Ekström, E.-C. Do side-effects reduce compliance to iron supplementation? A study of daily-and weekly-dose regimens in pregnancy. J. Health Popul. Nutr. 20, 175–179 (2002).
Yekta, Z., Ayat, E. H., Pourali, R. & Farzin, A. Predicting factors in iron supplement intake among pregnant women in urban care setting. J. Res. Health Sci. 8, 39 (2008).
Winichagoon, P. Prevention and control of anemia: Thailand experiences. J. Nutr. 132, 862S-866S (2002).
Yamashita, T. et al. Maternal knowledge associated with the prevalence of iron and folic acid supplementation among pregnant women in muntinlupa, Philippines: A cross-sectional study. Patient Prefer Adher. 15, 501–510. https://doi.org/10.2147/ppa.S291939 (2021).
Acknowledgements
Our heartfelt appreciation and thanks extend to supervisors, data collectors, respondents, and individuals who enormously engaged in the study.
Funding
We didn’t receive a specific fund for this study.
Author information
Authors and Affiliations
Contributions
G.B.: Participated in the conception, design, data analysis, and writing up of the manuscript. B.L.: Participated in the conception, design, and finalizing of the manuscript. T.B.: Participated in the conception, design, data analysis, and finalizing of the manuscript. G.E.: Participated in the conception, design, data analysis, and finalizing of the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Beressa, G., Lencha, B., Bosha, T. et al. Utilization and compliance with iron supplementation and predictors among pregnant women in Southeast Ethiopia. Sci Rep 12, 16253 (2022). https://doi.org/10.1038/s41598-022-20614-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-20614-9
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.