Abstract
Partially stabilized zirconia (5Y-PSZ) has been widely used to manufacture indirect monolithic restorations, and the effect of finishing procedures on the optical and mechanical properties of these materials are still unclear. The purpose of this study was to evaluate the effect of staining, polishing and glazing on surface roughness, crystalline phase content, microhardness, fracture toughness, dynamic elastic modulus, three-point flexural strength, strain distribution, color (∆E00/∆L/∆a/∆b), and translucency before and after artificial accelerated aging (water spray and ultraviolet) of 5Y-PSZ. Bar-shaped and rectangle-shaped specimens of the 5Y-PSZ were prepared and divided into six groups, according to finishing procedure: GC (control), GS (staining), GG (glazing), GSG (staining and glazing), GP (polishing), GSP (staining and polishing). There was a significant difference between groups for surface roughness (p < 0.05), dynamic elastic modulus (p = 0.007), microhardness (p = < 0.05), ∆E00 (p = 0.010), and ∆a (p = 0.008). GC presented higher cubic phase content, and the stained groups (GS, GSG and GSP) presented higher monoclinic content. The different finishing procedures affected roughness, dynamic elastic modulus, microhardness, and color of 5Y-PSZ; polishing being the finish that provides minors changes to the 5Y- PSZ. Accelerated artificial aging caused color change, regardless of finishing procedure used.
Similar content being viewed by others
Introduction
Dental science is always searching for improvements in optical properties of dental materials. Recently developed monolithic zirconia present lower opacity, greater translucency, and availability of colors for use as a monolithic restorative material1. This is attributed to its ability to provide a natural and harmonious smile with other teeth2,3.
Polycrystalline yttria-stabilized tetragonal zirconia (3Y-TZP) is the most used in dentistry, but partially (4Y-PSZ and 5Y-PSZ) stabilized zirconia, with higher concentrations of yttrium oxide in its composition when compared to 3Y -TZP, 4 mol% for 4Y-PSZ and 5 mol% for 5Y-PSZ4,5, are gaining wider use due to some characteristics. The addition of high concentrations of yttrium oxide promotes an increase in the amount of cubic phase content5,6,7,8,9,10, increasing translucency, since the cubic phase has an index of isotropic refraction, unlike the tetragonal phase8,10,11. These modifications are attributed to reduced light scattering that improves the translucency of the material for clinical use12,13,14.
Zirconia is white and requires color adjustment to mimic the appearance of natural teeth15,16,17,18. There are three techniques available to assign color to zirconia: addition of metal oxides during the manufacture of zirconia blocks, immersion or application of coloring liquids on pre-sintered zirconia, and staining after sintering process12,19,20. These methods can affect the crystalline phase content, which can affect the optical and mechanical properties of zirconia21.
Polishing and glazing are finishing procedures that improve the aesthetics of zirconia22, reducing surface roughness4,23, biofilm accumulation24, and antagonist wear25,26. However, these finishing procedures modify the surface characteristics, and possibly the optical and mechanical properties of the materials, which can reduce the longevity of the indirect restoration27,28,29,30,31,32.
A limited information is available regarding the behavior of 5Y-PSZ after staining and finishing procedures, which are procedures performed routinely in the dental clinic. Therefore, the purpose of this study was to evaluate the effect of staining, polishing, and glazing on surface characteristics and mechanical properties of 5Y-PSZ and the influence of artificial aging on color and translucency. The null hypothesis tested was that staining, polishing, glazing and artificial aging have no influence in evaluated properties of 5Y-PSZ.
Results
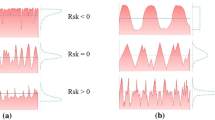
The surface roughness was different in the experimental groups (Fig. 1). GC and GP showed a regular and similar surface roughness. The combination of staining and finishing procedure (GSG and GSP) provided some defects and an irregular surface, and GG and GS groups showed large irregularities.
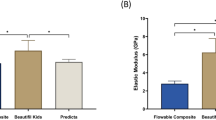
A significant difference between groups was found in the roughness (Sa—µm) (p = < 0.05), dynamic elastic modulus (GPa) (p = 0.007), and microhardness (KHN) (p = < 0.05). There were no statistical differences between groups in three-point flexural strength (MPa) (p = 0.137) and fracture toughness (Kic) (p = 0.129). Table 1 presents the results of the surface characteristics and mechanical tests.
Figure 2 illustrates the crystalline phase content of 5Y-PSZ obtained by X-ray diffraction and shows that staining increases monoclinic phase content while this phase was not found when only finishing procedures were performed (GG and GP). GC had 95.7% of cubic phase, 1.8% of tetragonal phase, and 2.5% of monoclinic phase. When only glazing was performed (GG), it reduced cubic phase (78.6%), increased tetragonal phase (13.3%) and monoclinic phase was not found. Staining (GS) promoted the most increase of monoclinic phase content (30.3%), the lower cubic phase content (37.3%) and 24,1% of tetragonal phase. GP had 70.8% of cubic phase, 20.8% of tetragonal phase, and the monoclinic phase was not found. When a combination of staining and finishing procedure (polishing or glazing) was used, tetragonal phase content was not found. GSG presented 60.3% of cubic phase, 29.2% of monoclinic phase, and GSP presented 79.2% of cubic phase and 20.8% of monoclinic phase.
Figures 3 and 4 illustrated the strain maps for 5Y-PSZ, which showed similar behavior for the different groups during the three-point flexural strength and fracture toughness tests. Compressive strains are presented, represented by cold colors, with the white color corresponding to the neutral zone, and the warm colors representing the tensile forces.
Table 2 shows the average color variation (∆E, ∆L, ∆a, ∆b) of 5Y-PSZ groups. There was a significant difference between the groups. Figure 5 shows the mean and standard deviation of translucency in each group before (T1) and after the accelerated artificial aging (T2). There was no statistical difference observed in the following comparisons: translucency values at T1 and T2 (p = 0.069), groups (p = 0.638), and time*group interaction (p = 0.533).
Discussion
The null hypothesis was rejected because staining and finishing procedures affected the surface morphology and roughness, elastic modulus, microhardness, and color of 5Y-PSZ.
5Y-PSZ is indicated to manufacture monolithic crowns in the anterior region11,33. Finishing procedures for zirconia restorations, such as polishing and glazing, influence surface characteristics of zirconia, and being indicated for better clinical performance and longevity22,23,24. GC and GP showed a lower surface roughness while the highest roughness occurred in the groups that received glazing and staining. Polishing provides high surface smoothness on 5Y-PSZ34 in accordance with Vila-Nova et al.35.
The different surface finishing procedures can directly affect 5Y-PSZ microstructure by introducing residual stresses that can impair its mechanical properties27,29,30,31. The lowest microhardness values were associated with groups that received glazing or staining. A higher microhardness was found in GC, GP and GG. This difference is probably attributed to the introduction of a stain/glaze layer at the surface of 5Y-PSZ, whose microhardness is lower, and this layer of glaze does not interact with bulk 5Y-PSZ because of their different microstructure features.
There was no difference among the groups in the three-point flexural strength and fracture toughness test. The results of the present study corroborated Vila Nova et al. (2020)34, who obtained mean values of flexural strength of 528 MPa on the 5Y-PSZ. The fracture toughness values of 5Y-PSZ are lower than 3Y-TZP and 4Y-PSZ35. This study showed lower toughness values of 5Y-PSZ than other studies with the same methodology, such as: 3.56 MPa33, 2.63 MPa36 and 2.1 MPa37. However, these other studies did not use pre-coloured 5Y-PSZ, which suggests that the introduction of pigments during zirconia block fabrication can lead to a fracture toughness reduction.
The strain distribution during the fracture toughness test showed similar behavior to feldspathic ceramic, lithium disilicate, leucite reinforced ceramic, and nanofilled resin material, and the highest stress concentration occurred on the notch, as the load gradually increased during the test until fracture38,39. Staining procedure reduced the dynamic elastic modulus, if compared with GC, that presented highest values. This reduction can probably be caused by metallic salts and oxides present in the stains18. There is a similarity between the values of the dynamic modulus of elasticity of 5Y-PSZ with other studies with 4Y-PSZ (210GPa)40 and 3Y-TZP (202GPa)41.
All groups showed a reduction in the cubic phase content after staining and finishing procedures. Although staining promoted an increase the monoclinic phase content in GS, GSG, and GSP of pre-coloured 5Y-PSZ, the mechanical behavior was not improved. These results are different from Shah et al.42, which reported that oxides that give color to 3Y-TZP change the grain size of zirconia and increase the monoclinic phase content, which can improve the mechanical behavior of the material. However, it is necessary to consider differences of 3Y-TZP used in the previous study and 5Y-PSZ of the present study. In addition, the oxides present in the stains can reduce grains, affecting mechanical properties18.
Zirconia staining occurs in chromatic reproduction and dental mimicry21,43,44,45. All finishing protocols showed a color change ∆E00, perceptible by the human eye with accelerated artificial aging simulating 1 year of clinical service46,47,48. The lower color stability of zirconia is influenced by the properties and qualities of the surface49. Differences in color variations may arise from the composition of the material and stain liquids22. 5Y-PSZ presents a stable translucency, independent of staining, surface finishing procedures and accelerated artificial aging.
Stains are used in 5Y-PSZ monolithic restorations when color requires adjustment. When stains are necessary, the use of glaze layer to protect stain is important and color change is lower than polishing after stain. However, sometimes color is ideal and stain is not necessary. Then, color stability of polishing is better than glaze. These results are important to guide the dentist in the choice of the ideal finishing procedures in clinical practice.
The study showed that the mechanical behavior of 5Y-PSZ is affected by staining and surface finishing procedures, which are routine laboratory and clinical procedures in the finalization of restorations, exhibiting good results when subjected to the polishing, which is indicated as the best protocol for finishing 5Y-PSZ indirect restorations. Accelerated artificial aging does not affect the translucency of 5Y-PSZ, but changes the color of the material, regardless of the surface finishing procedure. However, the limitations of this study were: design of the specimens was different from dental prostheses, staining was performed in a single layer, using only one color of stain, accelerated artificial aging does not simulate all factors present in the oral cavity, such as pH variation, biofilm formation. In addition, 12 months of clinical service is considered a short period when measuring clinical success of the materials. Clinical studies using staining and surface finishing procedures in 5Y-PSZ indirect restorations are necessary to establish longevity.
Conclusions
Based on the findings of this in vitro study, the following conclusions were drawn:
-
Staining and surface finishing procedures applied on 5Y-PSZ promoted changes in the surface roughness, dynamic elastic modulus, and microhardness.
-
Three-point flexural strength and fracture toughness did not differ significantly; polishing promoted minor changes in the mechanical properties of 5Y-PSZ.
-
All groups showed crystallographic phase transformation and staining promoted an increase of monoclinic phase content.
-
Accelerated artificial aging changes color of 5Y-PSZ, regardless of surface finishing procedure used. Translucency was not affected.
Methods
Partially stabilized zirconia (5Y-PSZ) blocks (pre-coloured in color A2) (Table 3) were used to manufacture specimens. Bars of two dimensions (30 × 4.4 × 2 mm and 25 × 3 × 4 mm), and rectangle-shaped specimens (5 × 6 × 2 mm) were obtained using a precision saw, with the aid of a diamond disc under water cooling, and manually finished with sandpaper using a sequential granulation of 320, 400, 600, and 1200. Before sintering, the specimens were cleaned or washed in an ultrasonic bath with distilled water, and after sintered in a furnace, according to the manufacturer's recommendations. The specimens were randomly divided into 6 groups: GC (control), GS (staining), GG (glazing), GSG (staining and glazing), GP (polishing), GSP (staining and polishing).
Bar-shaped specimens (30 × 4.4 × 2 mm) (n = 60) were used to evaluate surface roughness, crystalline phase content, dynamic elastic modulus, and three-point flexural strength. Other bar-shaped specimens (25 × 3 × 4 mm) (n = 60) were used for the fracture toughness test while rectangular-shaped ones (n = 66) were subjected to the Knoop microhardness test, color and translucency before and after accelerated artificial aging.
Staining and finishing procedures were performed by a single operator (A.O.S.) after sintering. Glaze (Glaze InSync, InSync, USA) and/or stain (Stain InSync Orange, InSync, USA) was applied using a brush, in a single layer, and fired according to manufacturer’s recommendations. Polishing was performed with diamond polishers in two steps. Initially, samples were polished with a medium-grain diamond polisher (Diacera W16DCmf, Eve Ernst Vetter GmbH, Germany), and after with a fine-grained diamond polisher (Diacera W16DC, Eve Ernst Vetter GmbH, Germany). For this, specimens were positioned in a metallic matrix (Fig. 6). The matrix with specimen and the rotary instrument were positioned in a device that ensures parallelism and standardization of the applied load on all specimens50, and polishing was performed using diamond polishers in low speed handpiece at 7000–12,000 rpm.
A confocal laser microscope (LEXT OLS4000, Olympus, Japan) was used to evaluate the surface roughness. A representative image of the surface in each group was chosen based on the repetitive pattern found. The surface roughness (Sa) (n = 21) was calculated with software (LEXT 3D Measuring Laser Microscope OLS4000; Olympus) which analyzed the entire scanned surface and calculated a mean roughness. The dynamic elastic modulus was a non-destructive method characterized by the impulse excitation technique, using specific equipment (Sonelastic, ATCP Engenharia Física, Brazil) and software (Sonelastic v. 2.2, ATCP Engenharia Física, Brazil), according to ASTM E-1876. X-ray diffraction (XRD) was performed using a diffractometer (D2 Phaser, Bruker AXS Corporation, USA), and the relative amount of the crystalline phase content was obtained through Rietveld refinement using software (TOPAS V4.2, Bruker AXS Corporation, USA).
The three-point flexural strength test was performed in a universal testing machine (Biopdi, São Carlos, Brazil) using a 100 kgf load cell at a 0.5 mm/min speed, in accordance with ISO 687251. The fracture toughness was calculated using the single-edge V-notch beam method in accordance with ISO 6872:201651. The notch was performed using a diamond disc (0.25 mm rigid sintered diamond, Odontomega, Brazil), having a depth ranging between 0.8 and 1.2 mm. The notches were then finished with a polishing paste (Lunar diamond paste, Odontomega, Brazil) and a razor blade (Navalha, Wilksonnson Sword, United Kingdom). The notches were examined under an optical microscope (S8AP0, Leica, Germany) prior to the test to determine the notching depth between 0.8 and 1.2 mm. The specimens were supported by two rollers with a distance of 20 mm between them. The notched surface was positioned downwards, and loaded under 0.5 mm/min speed in an universal testing machine until the fracture. The digital image correlation was used to qualitatively analyze the strain distribution in the 5Y-PSZ bars during the three-point flexural strength and fracture toughness tests. The Knoop microhardness was evaluated using a microhardness tester (HMV-2, Shimadzu Corp., Japan) under a load of 3 N for 15 s (five indentation were applied for each specimen at five different locations)52. Color and translucency were evaluated using a spectrophotometer (Delta Vista 2.0, Delta Color, Brazil) at room temperature according to the formulas described by Sharma et al. and Nassary et al.33,53. Color and translucency were evaluated before (T1) and after (T2) artificial aging. Artificial aging was performed using the Accelerated Aging System for C-UV non-metallics (Conexim Matérias Primas Ltda, São Paulo, Brazil), with condensation water spray with saturated air-vapor mixture and UV-B light with radiation concentrated between 280 and 320 nm. The program consisted of 4 h exposure to UV-B light at 50 °C and 4 h condensation at 50 °C for a period of 300 h. This aging procedure corresponds to 1 year of clinical service48,49,50.
Statistical analyses were performed using IBM SPSS statistics software (20.0, IBM, USA), after the Shapiro–Wilk normality test, data from all assays presented normal distribution. The surface characteristics, mechanical properties and color were evaluated by one-way analysis of variance (ANOVA) and post-hoc Tukey test (α = 5%). Translucency was evaluated by the linear model of repeated measures and Bonferroni's test.
Data availability
Data supporting the results of this study are available in the article and can be requested from the corresponding author.
References
Wang, F., Takahashi, H. & Iwasaki, N. Translucency of dental ceramics with different thicknesses. J. Prosthet. Dent. 110(1), 14–20. https://doi.org/10.1016/S0022-3913(13)60333-9 (2013).
Sen, N. & Us, Y. O. Mechanical and optical properties of monolithic CAD-CAM restorative materials. J. Prosthet. Dent. 119(4), 593–599. https://doi.org/10.1016/j.prosdent.2017.06.012 (2018).
Baldissara, P. et al. Translucency of IPS e.max and cubic zirconia monolithic crowns. J. Prosthet. Dent. 120(2), 269–275. https://doi.org/10.1016/j.prosdent.2017.09.007 (2018).
Zhang, Y. & Lawn, B. R. Novel zirconia materials in dentistry. J. Dent. Res. 97(2), 140–147. https://doi.org/10.1177/0022034517737483 (2018).
Carrabba, M. et al. Translucent zirconia in the ceramic scenario for monolithic restorations: A flexural strength and translucency comparison test. J. Dent. 60, 70–76. https://doi.org/10.1016/j.jdent.2017.03.002 (2017).
Camposilvan, E. et al. Aging resistance, mechanical properties and translucency of different yttria-stabilized zirconia ceramics for monolithic dental crown applications. Dent. Mater. 34(6), 879–890. https://doi.org/10.1016/j.dental.2018.03.006 (2018).
Ghodsi, S. & Jafarian, Z. A review on translucent zirconia. Eur. J. Prosthodont. Restor. Dent. 26(2), 62–74. https://doi.org/10.1922/EJPRD_01759Ghodsi13 (2018).
Zhang, Y. & Lawn, B. R. Evaluating dental zirconia. Dent. Mater. 35(1), 15–23. https://doi.org/10.1016/j.dental.2018.08.291 (2018).
Shahmiri, R., Standard, O. C., Hart, J. N. & Sorrell, C. C. Optical properties of zirconia ceramics for esthetic dental restorations: A systematic review. J. Prosthet. Dent. 119(1), 36–46. https://doi.org/10.1016/j.prosdent.2017.07.009 (2018).
Inokoshi, M. et al. Crystallographic and morphological analysis of sandblasted highly translucent dental zirconia. Dent. Mater. 34(3), 508–518. https://doi.org/10.1016/j.dental.2017.12.008 (2018).
Mao, L. et al. Graded ultratranslucent zirconia (5Y-PSZ) for strength and functionalities. J. Dent. Res. 97(11), 1222–1228. https://doi.org/10.1177/0022034518771287 (2018).
Zhang, Y. Making yttria-stabilized tetragonal zirconia translucent. Dent. Mater. 30(10), 1195–1203. https://doi.org/10.1016/j.dental.2014.08.375 (2014).
Eldwakhly, E., Ahmed, D. R. M., Soliman, M., Abbas, M. M. & Bodrawy, W. Color and tranlucency stability of novel restorative CAD/CAD materials. Dent. Med. Probl. 56(4), 349–356. https://doi.org/10.17219/dmp/111400 (2019).
Longhini, D. et al. Mechanical behavior of ceramicc monolithic systems with different thicknesses. Oper. Dent. 44(5), 244–253. https://doi.org/10.2341/18-083-L (2019).
Kim, H. K., Kim, S. H., Lee, J. B., Han, J. S. & Yeo, I. S. Effect of polishing and glazing on the color and spectral distribution of monolithic zircônia. J. Adv. Prosthodont. 5(3), 296–304. https://doi.org/10.4047/jap.2013.5.3.296 (2013).
Tuncel, I., Eroglu, E., Sari, T. & Usumez, A. The effect of coloring liquids on the translucency of zirconia framework. J. Adv. Prosthodont. 5(4), 448–451. https://doi.org/10.4047/jap.2013.5.4.448 (2013).
Orhun, E. The effect of coloring liquid dipping time on the fracture load and color of zirconia ceramics. J. Adv. Prosthodont. 9(1), 67–73. https://doi.org/10.4047/jap.2017.9.1.67 (2017).
Tabatabaian, F. Color aspect of monolithic zirconia restorations: A review of the literature. J. Prosthodont. 28, 276–287. https://doi.org/10.1111/jopr.12906 (2019).
Ahangari, A. T., Torabi Ardakani, K., Mahdavi, F. & Torabi Ardakani, M. The effect of two shading techniques on value of zirconia-based crowns. J. Dent. (Shiraz) 16, 129–133 (2015).
Kim, H. K. Optical and mechanical properties of highly translucent dental zirconia. Materials (Basel) 13(15), 3395. https://doi.org/10.3390/ma13153395 (2020).
Sulaiman, T. A. et al. The effect of staining and vacuum sintering on optical and mechanical properties of partially and fully stabilized monolithic zirconia. Dent. Mater. 34(5), 605–610. https://doi.org/10.4012/dmj.2015-054 (2015).
Alp, G., Subasi, G. M., Seghi, R. R., Johnston, W. M. & Yilmaz, B. Effect of shading technique and thickness on color stability and translucency of new generation translucent zircônia. J. Dent. 73, 19–23. https://doi.org/10.1016/j.jdent.2018.03.011 (2018).
Huh, Y. H., Yang, E. C., Park, C. J. & Cho, L. R. In vitro evaluation of the polishing effect and optical properties of monolithic zirconia. J. Prosthet. Dent. 119(6), 994–999. https://doi.org/10.1016/j.prosdent.2017.06.015 (2018).
Haralur, S. B. Evaluation of efficiency of manual polishing over autoglazed and overglazed porcelain and its effect on plaque accumulation. J. Adv. Prosthodont. 4(4), 179–186. https://doi.org/10.4047/jap.2012.4.4.179 (2012).
Ghazal, M. & Kern, M. The influence of antagonistic surface roughness on the wear of human enamel and nanofilled composite resin artificial teeth. J. Prosthet. Dent. 101(5), 342–349. https://doi.org/10.1016/S0022-3913(09)60068-8 (2009).
Mitov, G. et al. Wear behavior of dental Y-TZP ceramic against natural enamel after different finishing procedures. Dent. Mater. 28(8), 909–918. https://doi.org/10.1016/j.dental.2012.04.010 (2012).
Sundh, A., Molin, M. & Sjögren, G. Resistance to fracture of pure ceramic bridges of zirconia partially stabilized with yttrium oxide after coating and mechanical fatigue tests. Dent. Mater. 21(5), 476–482. https://doi.org/10.1016/j.dental.2004.07.013 (2005).
Nothdurft, F. P., Merker, S. & Pospiech, P. R. Fracture behavior of implant-implant and implant-tooth-supported all-ceramic fixed dental prostheses utilizing zirconium dioxide implant abutments. Clin. Oral. Investig. 15(1), 89–97. https://doi.org/10.1007/s00784-009-0359-0 (2011).
Pereira, G. K. R. et al. The effect of grinding on the mechanical behavior of Y-TZP ceramics: A systematic review and meta-analyses. J. Mech. Behav. Biomed. Mater. 63, 417–442. https://doi.org/10.1016/j.jmbbm.2016.06.028 (2016).
Canneto, J. J. et al. Grinding damage assessment on four high-strength ceramics. Dent. Mater. 32(2), 171–182. https://doi.org/10.1016/j.dental.2015.11.028 (2016).
Moris, I. C. M. et al. Fracture loads and failure modes of customized and non-customized zirconia abutments. Dent. Mater. 34(8), e197–e204. https://doi.org/10.1016/j.dental.2018.04.005 (2018).
Go, H., Park, H., Lee, J., Seo, H. & Lee, S. Effect of various polishing burs on surface roughness and bacterial adhesion in pediatric zirconia crowns. Dent. Mater. J. 38(2), 311–316. https://doi.org/10.4012/dmj.2018-106 (2019).
Nassary Zadeh, P., Lümkemann, N., Sener, B., Eichberger, M. & Stawarczyk, B. Flexural strength, fracture toughness, and translucency of cubic/tetragonal zirconia materials. J. Prosthet. Dent. 120(6), 948–954. https://doi.org/10.1016/j.prosdent.2017.12.021 (2018).
Carvalho, I.H.G., Silva, N.R., Vila-Nova, T.E.L., Almeida, L.F.D., Veríssimo, A.H., Melo, R.M., Zhang, Y., Souza, R.O.A. Effect of finishing/polishing techniques and aging on topography, C. albicans adherence, and flexural strength of ultra-translucent zirconia: na in situ study. Clin. Oral Investig. 26(1):889–900. DOI: https://doi.org/10.1007/s00784-021-04068-3 (2021).
Vila-Nova, T. E. L. et al. Effect of finishing/polishing techniques and low temperature degradation on the surface topography, phase transformation and flexural strength of ultra-translucent ZrO2 ceramic. Dent. Mater. 36, e126–e139. https://doi.org/10.1016/j.dental.2020.01.004 (2020).
Jerman, E. et al. Evaluation of translucency, Marten’s hardness, biaxial flexural strength and fracture toughness of 3Y-TZP, 4Y-TZP and 5Y-TZP materials. Dent. Mater. 37(2), 212–222. https://doi.org/10.1016/j.dental.2020.11.007 (2021).
Liu, H., Zhao, W. Y., Ji, J., Cui, Y. & Chu, P. Determination of fracture toughness of zirconia ceramics with different yttria concentrations by SEVNB method. Ceram. Int. 43(13), 10572–10575. https://doi.org/10.1016/j.ceramint.2017.04.064 (2017).
Porto, T. et al. Mechanical properties and DIC analyses of CAD/CAM materials. J. Clin. Exp. Dent. 8(5), e512–e516. https://doi.org/10.4317/jced.53014 (2016).
Porto, T. S. et al. Brittleness index and its relationship with materials mechanical properties: Influence on the machinability of CAD/CAM materials. Braz. Oral Res 33, 026. https://doi.org/10.1590/1807-3107bor-2019.vol33.0026 (2019).
Alghazzawi, T. F. et al. Influence of low-temperature environmental exposure on the mechanical properties and structural stability of dental zirconia. J. Prosthodont. 21(5), 363–369. https://doi.org/10.1590/1807-3107bor-2019.vol33.0026 (2012).
Fiorin, L., Moris, I. C. M., Faria, A. C. L., Ribeiro, R. F. & Rodrigues, R. C. S. Effect of different grinding protocols on surface characteristics and fatigue behavior of yttria-stabilized zirconia polycrystalline: An in vitro study. J. Prosthet. Dent. 124(4), 486.e1-486.e8. https://doi.org/10.1016/j.prosdent.2020.03.016 (2020).
Shah, K., Holloway, J. A. & Denry, I. L. Effect of coloring with various metal oxides on the microstructure, color, and flexural strength of 3Y-TZP. J. Biomed. Mater. Res. B Appl. Biomater. 87(2), 329–337. https://doi.org/10.1002/jbm.b.31107 (2008).
Sedda, M. et al. Influence of coloring procedure on flexural resistance of zirconia blocks. J. Prosthet. Dent. 114(1), 98–102. https://doi.org/10.1016/j.prosdent.2015.02.001 (2015).
Dal Piva, A. M. O. et al. Three-body wear effect on different CAD/CAM ceramics stainig durability. J. Mech. Behav. Biomed. Mater. 103, 103579. https://doi.org/10.1016/j.jmbbm.2019.103579 (2020).
Giti, R., Haghdoost, S. & Ansarifard, E. Effect of different coloring techniques and surface treatment methods on the surface roughness of monolithic zirconia. Dent. Res. J. (Isfahan) 17(2), 152–161 (2020).
Heydecke, G., Zhang, F. & Razzoog, M. E. In vitro color stability of double layer veneers after accelerated aging. J. Prosthet. Dent. 85, 551–557. https://doi.org/10.1067/mpr.2001.115385 (2014).
Turgut, S., Bagis, B., Turkaslan, S. S. & Bagis, Y. H. Effect of ultraviolet aging on translucency of resin cemented ceramic veneers: An in vitro study. J. Prosthodont. 23, 39–44. https://doi.org/10.1111/jopr.12061 (2014).
Kurt, M. & Bal, B. T. Effects of accelerated artificial aging on the translucency and color stability of monolithic ceramics with different surface treatments. J. Prosthet. Dent. 121(4), 712.e1-712.e8. https://doi.org/10.1016/j.prosdent.2019.01.014 (2019).
Subasi, M. G., Alp, G., Johnston, W. M. & Yilmaz, B. Effect of thickness on optical properties of monolithic CAD-CAM ceramics. J. Dent. 71, 38. https://doi.org/10.1016/j.jdent.2018.01.010 (2018).
Hatanaka, G. R., Polli, G. S. & Adabo, G. L. The mechanical behaviour of high-tranlucent monolithic zirconia. J. Prosthet. Dent. 123(2), 330–337. https://doi.org/10.1016/j.prosdent.2018.12.013 (2020).
ISO 6872. Dentistry—Ceramic Materials. International Organ Stand, (2015).
Lima, R. S., Kucuk, A. & Berndt, C. C. Bimodal distribuition os mechanical properties on plasma sprayed nanostructured partially stabilized zirconia. Mater. Sci. Eng. A 327(2), 224–232 (2002).
Sharma, G., Wu, W. & Dalal, E. N. The CIEDE2000 Color difference formula: Implementation notes, supplemental test data, and mathematical observations. Color. Res. Appl. 30(1), 21–30. https://doi.org/10.1002/COL.20070 (2005).
Acknowledgements
This work was supported by the São Paulo Research Foundation FAPESP [research grant # 2019/18367-4] and Agency for the High-Standard Promotion of Graduate Courses, Brazil (CAPES) for the support for Oral Rehabilitation Graduate Program and scholarship grant.
Author information
Authors and Affiliations
Contributions
A.O.S: methodology, data collection and interpretation, drafting the paper, final review of the manuscript. L.F.: conceptualization, methodology, final review of the manuscript. A.C.L.F.: monitored the tests in the laboratory, statistical analysis, final review of the manuscript. R.F.R.: project associate researcher, data interpretation, drafting the paper, final review of the manuscript. R.C.S.R.: researcher and project coordinator, conceptualization, data interpretation, final review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
da Silva, A.O., Fiorin, L., Faria, A.C.L. et al. Translucency and mechanical behavior of partially stabilized monolithic zirconia after staining, finishing procedures and artificial aging. Sci Rep 12, 16094 (2022). https://doi.org/10.1038/s41598-022-20120-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-20120-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.