Abstract
Adolescent mental health problems have been recognised as a major issue in low-income countries including India. Through a meta-analytic approach, the present review delineate the overall prevalence of each of the most discussed mental health problems among rural adolescents in India, comprising depression, anxiety disorders, generalised anxiety disorder, panic disorder, separation anxiety, social anxiety disorder, suicidality, hyperactivity, emotional problems, conduct problems and peer problems. The review also presents the potential determinants of such mental health problems. Using PRISMA guidelines, a total of thirty-five studies were finalized from databases such as PubMed, Science Direct, JSTOR, Web of Science, Google Scholar and ProQuest. From the findings, it is observed that male and female adolescents does not differ significantly in the prevalence of most mental health problems. However, social anxiety was found to be more prevalent among females when compared to males. In meta-regression, factors like tools used (screening tools vs diagnostic interviews), sample size, setting (school-based vs community-based), sampling technique and year of publication were found to influence the prevalence rates of certain mental health problems, reported in the studies. Major determinants influencing the prevalence of mental health problems in rural adolescents were age, socio-economic status, academic and family environment. Individual factors such as social media usage, physical activity, and substance use also contribute to mental health problems. As India accounts for one-fifth of the world's adolescent population, the findings of this review can have global implications.
Similar content being viewed by others
Introduction
‘Psychiatric epidemiology’ studies the causes and prevalence of mental health problems in society1. Ever since the establishment of the Diagnostic and Statistical Manual of Mental Disorders (DSM)2, numerous psychiatric epidemiological studies have been conducted across the world3. Due to a lack of awareness about mental health disorders in countries like India, those struggling with psychiatric issues remain unnoticed and neglected4. Psychiatric epidemiological studies address this issue by identifying people with psychiatric problems and by finding new occurrences of a particular mental health problem1.
World Health Organization (WHO) defines adolescents as those in the 10–19 age range5. Most unidentified mental health problems develop during adolescence phase6,7, many of which are life-long disorders8. Empirical evidence emphasises that adolescents are more vulnerable to recurrent anxiety, depression, mood disorders, and cognitive and behavioural issues as they grow up9,10. Mental health problems account for 45% of the burden and dysfunctionalities in the adolescent population11,12. If left unnoticed and untreated, such mental problems become more complicated with the transition of adolescents into adulthood. The most serious consequence of concern is a suicide, which has been a major predictor of the rising number of adolescent deaths13,14.
Adolescent mental health problems have been recognised as a major issue in low-income countries including India15,16. As per the 2011 Census, 21% of the Indian population consists of adolescents, with an estimated count of 253 million. However, there exists an incongruency between the needs and services for mental issues of adolescents in India17,18,19. The current Indian adolescent health initiatives do not acknowledge adolescent mental health with due importance. Lack of understanding about mental health problems in the country leads to adolescents experiencing their needs as incapacitated20.
Compared to western countries, epidemiological studies done on adolescent mental health problems in India can be found less in number21. Of the epidemiological studies done in India on adolescents, a wide variation in the prevalence of mental health problems from 2 to 63% can be noted22,23. However, inadequate description of the case, non-uniform diagnostic methods, type of area and variation in the set of mental health problems under consideration, use of non-representative samples, small sample size and discontinuation of participants after screening were some of the limitations that could be seen across the studies. The healthcare infrastructure, insufficient resources, stigma towards mental illnesses and sociocultural aspects of India limit the generalisability of the research findings conducted in other developed countries16,19. A meta-analysis helps systematically synthesise the results of many studies to give an overall estimate24. The present meta-analysis aims to provide an exact figure on the prevalence of the major mental health problems reported among adolescents in India. India has the largest number of adolescents, comprising one-fifth of the world's adolescent population16,25. Thus, the results of the present meta-analysis can have global implications.
The majority of the adolescent population in India resides in rural areas26. Previous studies have claimed that rural adolescents have more mental health issues than urban adolescents15,16,23,27. This can be attributed to the different lifestyles and environmental factors of the two areas28. Adolescents living in rural areas are neglected and exploited. They can be considered more vulnerable to mental health problems for many reasons, including their lack of access to health facilities, illiteracy, sudden exposure to metro-cities, supernatural beliefs, high prevalence of substance abuse, less preventive health screening, hostile family environments, low socioeconomic status and so on29,30,31. Venkaiah et al.,32 pointed out the undernutrition issue among India's rural adolescents. Poor nutritional status causes stunted growth, thus making this population more vulnerable to mental deterioration32. Not much-consolidated information about mental health problems of rural adolescent students could be found through literature search. As rural adolescents are a vulnerable group with many unique stressors, there is an urgency for more reliable information regarding the mental health status of rural adolescents, which will contribute to planning the necessary resources as well as preventive and control strategies for this group.
Socially constructed characteristics of women and men help understand the concept of ‘Gender’33. It may be a factor influencing one’s mental health10 as researches have shown that gender affects one's control over the determinants of socioeconomic status, access to various resources, health and many other essential aspects of life34. It was claimed in certain studies that the majority of the mental health problems other than emotional issues are more prevalent in boys than girls16; while in some studies, rural adolescent girls were found to be more mentally affected35 owing to the high frequency of early marriage and child-bearing in rural India, lack of autonomy, becoming a victim of marital violence, dropping out from education which in turn influence future employment, decreased social mobility and so on36,37,38,39,40,41. Reasonable cross-cultural differences exist regarding the prevalence of many mental disorders42. Contemporary research initiatives should address the lack of national statistics on mental health of adolescents43. The present meta-analysis gives wider clarity regarding such claims by analysing whether the prevalence of each mental health problem under study varies across gender (and other variables) or not.
The present study is the first meta-analysis in the literature that comprehensively reviews the prevalence of mental health problems among rural adolescents in India published across the 1990–2021 time period. The present study has considered a larger spectrum of mental health problems experienced by rural adolescents using selected studies that had used appropriate diagnostic measures. The following were the primary objectives:
-
1.
To analyse the pooled prevalence of each of the mental health problems among rural adolescents in India, including depression, anxiety disorders (AD), Generalised Anxiety Disorder (GAD), panic disorder (PD), separation anxiety (SeA), social anxiety disorder (SoA), suicidality, hyperactivity, emotional problems, conduct problems and peer problems.
-
2.
To explore variation (if any) in the prevalence of the investigated mental health problems among rural adolescents with respect to gender, year of publication, sample size, study setting, sampling technique and tools used.
-
3.
To systematically review the included studies to identify the determinants of the investigated mental health problems among rural adolescents in India.
Methods
Inclusion criteria
Quantitative studies published between 1990 and 2021 were selected for pooling. Studies conducted among rural adolescents in India were included, in which the sample participants were aged between 10–19 years. In order to be included, the studies should have reported the prevalence of at least one of the following mental health problems: depression, anxiety disorders, general anxiety disorder, panic disorder, separation anxiety, social anxiety, suicidality, hyperactivity, emotional problems, conduct disorders and peer problems. Studies having adequate information to calculate the prevalence of these mental health problems, were also included.
The studies conducted on both urban and rural settings were also included if the study mentioned separate results for rural participants regarding their mental health problems; In the case of rural–urban combined results, prevalence estimates were taken if more than 60% of the participants were from the rural area. Only studies published in the English language were considered.
Exclusion criteria
Studies with no full text available were excluded. Studies that did not use standardised tools/measurement scales or a structured psychiatric diagnostic interview, as part of the survey methodology were excluded. Studies in particular settings such as psychiatric wards in hospitals and studies conducted following any particular natural disaster etc., were excluded. Studies with ambiguous methodology or results were excluded. Conference abstracts, reviews, case studies, letters, commentaries, conceptual papers, editorials and books were excluded.
Information sources and search strategy
A systematic search of the databases such as PubMed, Science Direct, JSTOR, Web of Science, ProQuest and Google Scholar, was conducted to identify relevant studies. The search was completed by the end of 2021, collecting all english-language publications since 1990. The search strategy was decided based on a preliminary recursive search of research databases by the first, second and third authors, which was later validated by the rest of the authors.
The following search strategy was applied: (Adolescent OR Teenager OR Adolescents OR Youth OR Adolescence OR rural adolescents) AND (India OR rural India) AND (“mental health problems" OR Anxiety OR depression OR "generalised anxiety disorder" OR "panic disorder" OR "social anxiety disorder" OR suicidality OR hyperactivity OR “mental health”) AND (Prevalence OR rate OR incidence).
The reviewers then expanded the search by identifying further studies from the references of the screened full-texts. In addition, the reviewers ran a manual search in other organisational websites to identify potentially eligible studies that could not be retrieved from the database searches. Because of the small number of papers that met the eligibility criteria during the first search, an additional search was conducted. Before final analysis, the search strategy was re-run to check for missed records (if any) that met the inclusion criteria. The search strategy used in each of the databases have been uploaded as supplementary file (“supplementary information”).
Study selection and data extraction
The search findings were downloaded into Zotero software (Corporation for Digital Scholarship, Virginia, USA), and duplicate references were removed. The remaining studies were analysed following preferred reporting items for systematic reviews and meta-Analyses (PRISMA) guidelines44. Primary screening was done by checking the title and abstract of each study to identify and select the studies which met the inclusion and exclusion criteria. Subsequently, a secondary screening was done where the full text of articles was read and assessed by each reviewer independently based on the eligibility criteria. Reasons for exclusion were noted down at every stage.
After finalising the articles, relevant information like study characteristics (first author’s name, design of the study, year of publication, location of the study, sample size, instruments or tools used), sampling technique used, setting of the study (school-based or community-based), participant characteristics (age, community- rural or urban, gender) and outcomes (mental health problems and their prevalence rates) were retrieved. If a particular study selected did not directly report results using prevalence, then it was computed using the available information. Information regarding determinants of mental health problems among rural adolescents in India was collected for the purpose of systematic review. The collected data was entered into Google sheets. The disagreements and doubts about studies were cleared through group discussion.
Quality assessment
Two of the reviewers assessed the quality of the studies independently using the JBI critical appraisal checklist for prevalence studies45, published by the Joanna Briggs Institute in 2017. The evaluation criteria were: (1) appropriateness of the sample frame; (2) appropriateness of recruitment procedure; (3) adequacy of the sample size; (4) sufficiency in description of subjects and setting; (5) coverage of the identified sample; (6) validity of the methods used to identify the mental health problems; (7) reliability of the methods used to identify mental health problems symptoms or disorders; (8) adequacy of statistical analyses; and (9) appropriateness in management of response rate. Each item was assessed by scoring in the following way: yes = 1; no, unclear or not applicable = 0. Disagreements between the two authors, about the qualitative evaluation of studies were settled by seeking validation from other authors, complemented by the calculation of the inter-judge agreement index. Total quality scores of less than 5, 5 to 7 and greater than 7 were interpreted as low, moderate and high quality, respectively.
Data analysis
Pooled prevalence rates of mental health problems were calculated in the meta-analyses using the random-effects model, weighted by the inverse of the variance. The pooled prevalence was reported with 95% confidence intervals: Lower Limit − Upper Limit (CI: LL − UL). The "metaprop" command of the Stata software (version 17.0) was used for the analyses.
Heterogeneity was assessed by the I2 statistic, which describes the percentage of variation across studies due to heterogeneity rather than chance46. It is a ratio that ranges between 0 and 100%47. The higher the I2 value/ percentage, the greater the heterogeneity between the studies. Values of 25%, 50% and 75% represented cut-off points for low, moderate and high degrees of heterogeneity, respectively. Results were considered to be statistically significant only if p value was less than or equal to 0.05.
Subgroup analyses stratified by gender, year of publication, sample size, setting (school-based vs community-based), sampling method (probability sampling vs non-probability sampling) and tools used (screening tool vs diagnostic interview) were conducted to investigate potential sources of heterogeneity between subgroups. Subgroup differences were tested by meta-regression analysis (STATA V.17.0 ‘metareg’ command).
Besides a visual inspection of the funnel plot, potential publication bias was assessed through Egger’s test (checking the small study effects), with the results indicating publication bias when p value was less than or equal to 0.05. Sensitivity analysis was also done to confirm the consistency of prevalence estimates.
A systematic review to identify the determinants of the investigated mental health problems in rural adolescents in India was completed through a narrative synthesis of the included studies.
Results
Search flow and study characteristics
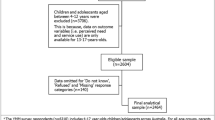
The initial search identified 2776 records through database searching using the mentioned keywords. On removal of 1214 duplicates, 1562 articles were selected for title/abstract reading. Consequently, 128 articles were selected based on inclusion criteria, and the remaining 1448 articles were excluded. Full texts of 2 articles could not be retrieved.
After a full-text screening of retrieved articles, 96 articles were removed based on reasons such as unavailability of full-texts, lack of differentiation between urban and rural adolescents, absence of prevalence rates mentioned and having prevalence estimates indicating combined results of children and adolescents. Studies with a special population were also removed, i.e., patients in psychiatric hospitals or survivors of natural disasters as participants. Duplicates and review papers were also removed. By the end of the full-text screening, 30 studies were included.
Five more studies which met the inclusion criteria were added in the final stage through a manual search of other websites, complemented by searching for citations from included studies. Thus, 35 studies were selected for the qualitative synthesis (systematic review), and 34 studies were included for quantitative synthesis (meta-analysis). Figure 1 shows the PRISMA flowchart depicting the study selection process.
The 35 studies provided prevalence data for common mental health problems for 17,514 participants. The participants were adolescents between the ages of 10–19 years. Five studies reported prevalence estimates for female adolescents and three reported prevalence for male adolescents only. The remaining 27 studies mentioned the prevalence estimates for both males and females (combined or separately). There were 13 studies done in South India (Karnataka (6), Kerala (4), Tamil Nadu, Puducherry, Andhra Pradesh) and 22 studies done in North India (Haryana (5), Maharashtra (2), Jharkhand (4) Uttar Pradesh (2), Jammu& Kashmir, Gujarat (2), Punjab, West Bengal (2), Rajasthan, Chandigarh, Assam).
Out of the 35 studies, 24 were school-based and the remaining 11 were community-based. Fifteen studies used probability sampling, while 20 studies used non-probability sampling methods.
All studies that reported the prevalence of emotional, conduct, and peer problems had used the Strengths and Difficulties Questionnaire (SDQ) for screening. The tools used to screen all the remaining mental health problems varied across the selected studies.
The articles were all cross-sectional studies, and were conducted between the years 1990–2021 in various rural areas within India. Table 1 depicts the characteristics of the 35 studies in detail.
Quality of studies and publication bias
Using JBI quality appraisal criteria, all included studies were evaluated for their quality. Twelve studies were found to have moderate risk of bias/moderate quality9,16,20,35,48,49,50,51,52,53,54,55 while the rest 23 studies had a low risk of bias/high quality15,22,23,26,27,28,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72. The inter-judge agreement index (κ) was calculated to be 0.88, indicating a high agreement between the judges about the quality of the studies. Most studies did not meet the following three parameters: (1) appropriateness of recruitment procedure, (2) adequacy of the sample size, and (3) appropriateness in management of response rate. Many studies employed non-probability sampling techniques, which do not yield a representative sample of the target population. Very few studies provided evidence that the respective authors determined an adequate sample size and used a small sample size using sample size calculation. Details of response rate was not reported in majority of the studies.
Considering the insufficiency of data for certain mental health problems, the assessment of publication bias could be done only for depression, anxiety disorders, social anxiety and suicidality. The visual inspection of the funnel plot of studies and Egger's test revealed an absence of publication bias (p > 0.05).
Determinants of mental health problems among rural adolescents in India
Factors such as gender, age, socio-economic status, academic environment and family environment influence the prevalence of mental health problems among rural adolescents. Individual factors such as social media usage, physical activity and substance use also affect the prevalence of mental health problems.
Table 2 summarizes the results reported on the prevalence of mental health problems among rural adolescents in India. Sensitivity analysis conducted by sequentially removing each study proved the stability in the prevalence estimate of each mental health problem.
Depression
Seventeen studies reported the prevalence of depression among rural adolescents in India. The pooled prevalence of depression across the 17 studies was found to be 27% (95% CI: 17–38%, I2 = 99.08%). The prevalence of depression varied from 3.5% to 88.3% across the studies15,20,22,23,26,27,35,50,54,55,58,59,60,63,64,69,71.
In subgroup analyses, the heterogeneity remained high. It was observed that the prevalence of depression is higher in studies that used screening tools compared to diagnostic tools (34% vs 8%) and in school-based studies than in community-based studies (34% vs 9%) and in studies with a sample size of less than 500, compared with those with sample size equal to or greater than 500 (31% vs 9%).
The meta-regression analysis found no significant between-group difference for gender, year of publication, sample size and sampling (all p > 0.05). Significant between-group difference was found for tools used (p = 0.04) and setting (p = 0.05).
Anxiety disorders (AD)
Nine studies reported the prevalence of anxiety disorders among rural adolescents in India. The pooled prevalence of anxiety disorders was found to be 26% (95% CI: 16–37%, I2 = 97.82%). The prevalence of anxiety disorders ranged from 12.4% to 60% across the nine studies20,22,26,35,50,51,56,67,72.
In subgroup analyses, the heterogeneity remained high, and it was observed that the prevalence of anxiety disorders is higher in studies that used screening tools compared to diagnostic tools (31% vs 16%) and in studies that used non-probability sampling than those that used probability sampling (29% vs 18%). The prevalence was higher in school-based studies than community-based studies (30% vs 19%) and in studies with a sample size of less than 500, compared with those with a sample size equal to or greater than 500 (30% vs 19%).
In the meta-regression analysis, no significant between-group difference was found for gender, year of publication, sample size, setting, sampling and tool used (all p > 0.05).
Generalised anxiety disorder (GAD)
Four studies reported the prevalence of generalised anxiety disorder, which ranged from 7.2% to 37.2% across the studies51,56,67,72. The pooled prevalence of generalised anxiety disorder was found to be 16% (95% CI: 7–28%, I2 = 97.73%). Subgroup analyses, meta-regression, and tests for publication bias were not performed for generalised anxiety disorder due to the small number of studies and insufficient data.
Panic disorder (PD)
Four studies reported the prevalence of the panic disorder, which ranged from 6.6% to 55.2% across the studies51,56,67,72. The pooled prevalence of panic disorder could be seen as 20% (95% CI: 6–41%, I2 = 98.99%). Due to the small number of studies and inadequate data, subgroup analyses, meta-regression and tests for publication bias were not performed for panic disorder.
Separation anxiety (SeA)
Four studies reported the prevalence of separation anxiety disorder, which ranged from 2.1% to 74% across the studies51,56,67,72. The pooled prevalence of separation anxiety was found to be 18% (95% CI: 1–47%, I2 = 99.50%). Subgroup analyses, meta-regression and tests for publication bias were not performed for separation anxiety because of inadequate data and small number of studies.
Social anxiety disorder (SoA)
The pooled prevalence of social anxiety disorder was found to be 23% (95% CI: 17–30%, I2 = 96.53%). The prevalence ranged from 8.4% to 39.7% across the eight studies51,55,56,59,65,66,67,72.
In subgroup analyses, the heterogeneity remained high. It was observed that the social anxiety disorder prevalence is higher among females than males (28% vs 16%) and in studies with a sample size of less than 500, compared with those with a sample size equal to or greater than 500 (37% vs 17%).
No significant between-group difference was found for year of publication, setting, and sampling (p > 0.05) in the meta-regression analysis. Significant between-group difference was found only for gender (p = 0.05) and sample size (p = 0.00).
Suicidality
Across the nine studies investigating suicidality, the pooled prevalence was 9% (95% CI: 5–13%, I2 = 95.27%). The prevalence ranged from 2.1% to 34.2% across the studies9,15,22,49,50,52,53,64.
In subgroup analyses, the heterogeneity remained high, and it was observed that the prevalence of suicidality is higher in studies published between 2009 and 2015 compared to those published between 2016 and 2021 (17% vs 6%) and in studies that used probability sampling than that used non-probability sampling (18% vs 5%). However, this might be a result of the study by Kumar et al.,50 that reported a much greater prevalence of suicidality than all the other included studies.
In the meta-regression analysis, no significant between-group difference was found for the year of publication and sample size (p > 0.05). Significant between-group difference was observed only for setting (p = 0.04) and sampling method (p = 0.02).
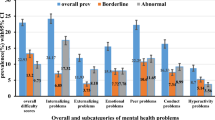
Hyperactivity
The pooled prevalence of hyperactivity was found to be 7% (95% CI: 2–14%, I2 = 97.15%). Seven studies investigated hyperactivity and the prevalence ranged from 2% to 22.7% across the studies16,22,28,48,61,62,68.
The heterogeneity remained high, and it was observed that the prevalence of hyperactivity is higher in studies published between 2009 and 2015 compared to those published between 2016 and 2021 (21% vs 4%) in the sub-group analysis. In the meta-regression analysis, no significant between-group difference was found for sample size and sampling (p > 0.05). However, a significant between-group difference was observed only for the year of publication (p = 0.00).
Emotional, conduct and peer problems
Six studies reported the prevalence of emotional, conduct, and peer problems. The pooled prevalence of emotional problems, conduct problems and peer problems was found to be 9% (95% CI: 6–13%, I2 = 89.90%), 19% (95% CI: 11–29%, I2 = 97.00%), and 15% (95% CI: 2–36%, I2 = 97.00%) respectively. Across the six studies, the prevalence of emotional problems, conduct problems and peer problems ranged from 5.12% to 20%, 7.06% to 53.3% and 6% to 45.9% respectively16,28,48,61,62,68. Due to the small number of studies and inadequate data, subgroup analyses, meta-regression and tests for publication bias were not performed for emotional, conduct and peer problems.
Discussion
The adolescent period is marked by reliance on friends more than family for mental support. Adolescents can be encouraged to spend more time and effort with friends to prevent them from experiencing issues of peer problems, conduct problems and other consequent emotional troubles16. Since the finalised studies in this review incorporated participants from various regions of India, the overall population of 17,514 can be regarded as an equitable representation of rural adolescents in India. The rates of morbidity, malnutrition and mortality reported in the rural areas of India are higher than what is being reported among the Indian population at large73. The present analysis shows that many rural adolescents in India are affected by mental health problems. Given the dearth of government-funded mental health treatments currently available, prevalence estimates for the mental health problems examined in this study highlight the need for enhanced mental health care74.
The high prevalence of depression found through meta-analysis re-validates the claims made by Steptoe et al., (2007) asserting Asian countries to have high levels of depression. It was interesting to see that, unlike the other types of anxiety disorders, social anxiety disorder was more prevalent among females when compared to males. As reported by previous empirical findings, female vulnerability to social anxiety might have genetic determinants besides the environmental aspects. The pooled prevalence of hyperactivity in the present study is higher than the worldwide prevalence of ADHD for adolescents, i.e., 5.2975. This suggests that adolescents in India's rural areas need to pay greater attention to the problem of hyperactivity. The prevalence of suicidality reported in the present meta-analysis is higher when compared to the estimates reported by the latest meta-analysis on suicidal behaviour among adolescents (rural and urban taken together) in India, which found the pooled prevalence of suicidal ideation in a lifetime as 5.458%76. In addition, the pooled prevalence estimates for suicidality reported in the present study is also higher than that reported across other Asian countries77.
The high heterogeneity between the individual studies could be due to the variation in sample size, sampling techniques, tools used and the study settings. Variables like tools used (screening tools vs diagnostic interviews), sample size, setting (school-based vs community-based) and year of publication were found to influence the prevalence rates reported in the studies.
Gender-wise comparison made in some studies reveal that females are more likely than males to experience depression, emotional issues, anxiety disorders, generalised anxiety disorder, panic disorder, social anxiety, and separation anxiety16,20,28,35,51,56,59,63,67,72. Males were found to have more hyperactivity, conduct and peer problems than females16,20. But some other studies found no significant association of gender with depression and/or anxiety disorders26,35,50,57,71. However, the present meta-analysis shows gender to have a significant association with social anxiety disorder only and not with other mental health problems.
The prevalence of depression, generalised anxiety disorder, panic disorder and suicidality increased with age56,57,60,63,69,70,71. There were mixed results regarding the relationship of age with anxiety disorders, emotional problems, conduct problems and peer problems respectively16,20,26,35,56,61. Social anxiety was found to be more prevalent in early and middle adolescence65,66.
Several comorbid conditions were also identified in the rural adolescents. The common psychiatric comorbidities with depression were found to be anxiety disorders, panic disorder, generalised anxiety disorder, separation anxiety58, conduct disorder in the past year, oppositional defiant disorder (ODD) in the past six months, attention deficit hyperactivity disorder (ADHD) in the past six months71, suicidal ideation23,49,55,71 and social anxiety59. Adolescent boys with anxiety and depressive disorder were identified to be in the high-risk group for suicidal behaviour47.
Students of government schools had a greater prevalence of depression. However, a lesser prevalence of anxiety disorders was observed in students from government schools than those from private schools23,56,60. In a study by Shukla et al., (2017), it was interesting to notice that adolescent girls studying in Hindi medium schools were about 12 times more preponderate for depression26.
Family factors such as a report of parental discord23,69, harsh parenting and strained family relationships26 were significantly associated with higher depression and anxiety rates. Sharing a living room with siblings, death of a family member in the recent past, presence of a family member with serious medical or psychiatric illness71, alcoholism or substance abuse in the family23, financial constraints and altercations in the family due to it23, were some of the identified determinants of depression among rural adolescents. Also, adolescents in joint families had a significantly higher prevalence of depression and social anxiety20,65. The majority of the studies reported a higher prevalence of depression and anxiety disorders in adolescents belonging to families of lower socioeconomic status20,22,23,60,67,69.
Depression was significantly higher in adolescents with illiterate parents and in adolescents whose parents were unemployed27, while no association was found between parents' occupation status and anxiety disorder in the child51. Feeling pressurised by parents to perform well in exams69, lack of supportive environment in school, spending lesser number of hours studying and lack of participation in cultural activities and/or sports in school23,64 were some factors associated with higher levels of depression, emotional, peer and conduct problems in adolescents. Prevalence of anxiety and depression was higher among students with unsatisfactory academic performance23,26. After-school entertainment like watching movies and spending time with friends had a favourable effect on mental health16. Also, individual resilience, supportive family and school environments and yoga were identified as protective factors23,65,71.
Adolescents smoking cigarettes or chewing tobacco and those who had experienced adverse events in the recent past, had significantly higher depression and anxiety26. Spending more time on social media sites was related to lesser depression and having a romantic partner23 was found to be linked to higher levels of depression. Adolescents with a long-term medical illness and/or impaired body image were more vulnerable to having depression71.
Mixed results were observed for the association of physical activity with emotional, conduct and peer problems respectively. However, hyperactivity was found to be less prevalent among adolescents with sedentary behaviour16,28,61.
The present review highlights the need for screening, early identification, monitoring and treatment of mental health problems. Improving awareness and coordination among parents, teachers and community workers can significantly help achieve this9,20,59,60,68,69. Some studies emphasized the development of psychosocial care, targeted interventions and mental health education programs for adolescents15,23,62,63. Life skill education was suggested to deal with mental health issues16,61. Yoga, sports and other recreational activities must be encouraged to improve mental well-being28. Present meta-analysis results emphasise the importance of giving vigilant supervision and careful attention to rural adolescents to prevent them from getting involved in anti-social behaviours (drug abuse, stealing and so on) and attempting suicide2,78.
De-limitations, limitations and scope for future research
Though the heterogeneity value across studies was high for most mental health problems, subgroup analysis investigating the reason for heterogeneity could not be explored for some mental health problems due to the insufficiency of empirical studies that met the inclusion criteria. For a few mental health problems for which subgroup analyses were done, variables like gender (male/female), year of publication (2009–2015/2016-2021), sample size (< 500/≥ 500), setting (school-based/community-based), sampling (probability vs non-probability sampling) and tools used (screening tool/diagnostic interview) could not account for the heterogeneity. However, considering the commonality of these limitations in other similar meta-analysis studies76,79, less variability in the pooled prevalence estimate level, and consistency with similar prevalence estimates reported by other meta-analysis results on particular mental health problems, interpretability of the present review's prevalence rates can be considered as valid.
The majority of the mental health problems were found to be identified using different screening methods, which would have caused variation in the prevalence estimate range obtained across the finalized studies. This, in turn, would have affected the present meta-analysis results. In addition, certain studies have used self-report measures to identify the prevalence of certain mental health problems. When disorders are self-reported, it sometimes becomes impossible to identify the isolated, sub-threshold, mild or short-lived cases that can be diagnosed and cured in the early stages. The authors of multiple studies mentioned that the 'social desirability' factor could have impacted the subject's responses, especially when questions were asked about substance abuse or the family and home atmosphere. Hence it would have influenced the accuracy of results reported in such studies.
The samples selected for some of the finalised studies focused majorly on specific regions or towns and did not provide a true representation of that particular study's population. Therefore, more empirical studies should provide results for a wider geographical area by taking larger samples that gives more generalisable and practical findings.
Since all of the included studies had used cross-sectional designs, inferences regarding the lifetime prevalence of each mental health problem could not be made in the present review. Therefore, there exists a scope for more research on this aspect of the topic. In addition to this, most of the included studies were school-based studies. As school-based studies are known for higher prevalence than community studies, this could have influenced the overall prevalence rates reported in the present review.
The search for appropriate literature was limited to only English indexed papers and journals. Access to certain published articles could not be gained as they were unavailable online. Despite all the limitations, the fact that there is a dire need to build, focus and implement psychological care services in rural India stays undisputed.
Implications
Finding the prevalence of mental health problems in the adolescent population of rural India aids in planning and distributing the nation's mental health resources appropriately. The study results would encourage public health planners, private health sectors, educational sectors and parents to take active measures to address adolescent mental health issues. This is very important as adolescence is the most vulnerable, yet developing stage of life. Timely addressing and management of affected rural adolescents can potentially smoothen their transition from adolescence to adulthood, hence, helping to adapt better to the complexities and consequences they may face in later phases of life. This study emphasises the importance of implementing appropriate primary mental health care services in the country's rural areas and the proves the necessity to include mental health awareness in education policies. Present meta-analysis results contribute to monitoring the effectiveness of new mental health policies and programs. High prevalence rates of mental health problems in rural adolescents of the country point out the urgency for reforming the public health policies, thereby facilitating more appropriate interventions and quality counselling services to be put in place for the better mental health of future adults. This, in turn, helps the development of the rural areas too.
Also, the study suggests placing teaching staff or trained professionals who can identify potential behaviours in students, that may lead to psychological disturbances later. Such students can be sent to experts in the field to be diagnosed and given adequate support at a very preliminary stage itself. Considering all the given points, it is not wrong to say that finding the prevalence of mental health issues is an indirect way to assess the success of mental health reform in the country.
Conclusion
Though meta-analysis is to be conducted once every 10 years, there has not been a meta-analysis that comprehensively reviews the prevalence of mental health problems among rural adolescents in India for the past 30 years. The current review provides accurate prevalence estimates for a range of mental health problems that affect adolescents in rural areas. The findings show that adolescents in rural India have a significant incidence of mental health problems. Therefore, the Indian government must expand and enhance the current national mental health services to cater to the requirements of adolescents living in rural areas of the nation.
Data availability
The datasets generated during and/or analysed during the current review paper, are available from the corresponding author on reasonable request.
References
Malhotra, S. & Patra, B. N. Prevalence of child and adolescent psychiatric disorders in India: A systematic review and meta-analysis. Child Adolesc. Psychiatry Ment. Health 8(1), 1–9. https://doi.org/10.1186/1753-2000-8-22 (2014).
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Steel, Z. et al. The global prevalence of common mental disorders: A systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 43(2), 476–493. https://doi.org/10.1093/ije/dyu038 (2014).
Math, S. B. & Srinivasaraju, R. Indian psychiatric epidemiological studies: Learning from the past. Indian J. Psychiatry. 52(Suppl1), S95. https://doi.org/10.4103/0019-5545.69220 (2010).
Dick, B. & Ferguson, B. J. Health for the world’s adolescents: A second chance in the second decade. J. Adolesc. Health 56(1), 3–6. https://doi.org/10.1016/j.jadohealth.2014.10.260 (2015).
Patton, G. C. et al. The prognosis of common mental disorders in adolescents: A 14-year prospective cohort study. Lancet 383(9926), 1404–1411. https://doi.org/10.1016/S0140-6736(13)62116-9 (2014).
Rushton, J. L., Forcier, M. & Schectman, R. M. Epidemiology of depressive symptoms in the National Longitudinal Study of Adolescent Health. J. Am. Acad. Child Adolesc. Psychiatry 41(2), 199–205. https://doi.org/10.1097/00004583-200202000-00014 (2002).
Zuckerbrot, R. A. & Jensen, P. S. Improving recognition of adolescent depression in primary care. Arch. Pediatr. Adolesc. Med. 160(7), 694–704. https://doi.org/10.1001/archpedi.160.7.694 (2006).
Ahir, R., Singhal, Y. K., Dhaked, M. S. & Sharma, P. A comparative study on protective factors, mental health and violence among male adolescents students of urban and rural school of Udaipur (Rajasthan), India. Int. J. Community Med. Public Health. 2(4), 421–424. https://doi.org/10.18203/2394-6040.ijcmph20150910 (2015).
Patel, V. Reducing the burden of depression in youth: What are the implications of neuroscience and genetics on policies and programs?. J. Adolesc. Health 52(2), S36–S38. https://doi.org/10.1016/j.jadohealth.2012.04.016 (2013).
Gore, F. M. et al. Global burden of disease in young people aged 10–24 years: A systematic analysis. Lancet 377(9783), 2093–2102. https://doi.org/10.1016/S0140-6736(11)60512-6 (2011).
Kieling, C. et al. Child and adolescent mental health worldwide: Evidence for action. Lancet 378(9801), 1515–1525. https://doi.org/10.1016/S0140-6736(11)60827-1 (2011).
Kessler, R. C. et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. General Psychiatry. 62(6), 593–602. https://doi.org/10.1001/archpsyc.62.6.593 (2005).
Centers for Disease Control and Prevention. (2005). National center for injury prevention and control. in Web-based injury statistics query and reporting system (WISQARS), 2013. https://www.cdc.gov/injury/wisqars.
Beattie, T. S. et al. Prevalence and correlates of psychological distress among 13–14 years old adolescent girls in North Karnataka, South India: A cross-sectional study. BMC Public Health 19(1), 1–12. https://doi.org/10.1186/s12889-018-6355-z (2019).
Nair, S., Ganjiwale, J., Kharod, N., Varma, J. & Nimbalkar, S. M. Epidemiological survey of mental health in adolescent school children of Gujarat, India. BMJ Paediatr. Open. https://doi.org/10.1136/bmjpo-2017-000139 (2017).
Roy, K. et al. India’s response to adolescent mental health: A policy review and stakeholder analysis. Soc. Psychiatry Psychiatr. Epidemiol. 54(4), 405–414. https://doi.org/10.1007/s00127-018-1647-2 (2019).
Sharan, P. & Sagar, R. Mental health policy for children and adolescents in developing countries. J. Indian Assoc. Child Adolesc. Mental Health. 3(1), 1–4 (2007).
Saxena, S., Thornicroft, G., Knapp, M. & Whiteford, H. Resources for mental health: Scarcity, inequity, and inefficiency. Lancet 370(9590), 878–889. https://doi.org/10.1016/S0140-6736(07)61239-2 (2007).
Mishra, S. K., Srivastava, M., Tiwary, N. K. & Kumar, A. Prevalence of depression and anxiety among children in rural and suburban areas of Eastern Uttar Pradesh: A cross-sectional study. J. Family Med. Primary Care. 7(1), 21–26. https://doi.org/10.4103/jfmpc.jfmpc_248_17 (2018).
Reddy, V. E. N. K. A. T. A. S. H. I. V. A. (2019). Mental health issues and challenges in India: A review. Int. J. Social Sci. Manag. Entrepreneurship (IJSSME). 3(2). Retrieved on 19th November, 2021 from http://mail.sagepublishers.com/index.php/ijssme/article/view/52
Satyanarayana, P. T., Prakash, B., Kulkarni, P., Kishor, M. & Renuka, M. A comparative study of prevalence of mental abnormalities among high school children in tribal, rural and urban Mysuru district, Karnataka, India. Int. J. Community Med. Public Health. 4, 809–813. https://doi.org/10.18203/2394-6040.ijcmph20170763 (2017).
Singh, M. M., Gupta, M. & Grover, S. Prevalence & factors associated with depression among schoolgoing adolescents in Chandigarh, north India. Indian J. Med. Res. 146(2), 205. https://doi.org/10.4103/ijmr.IJMR_1339_15 (2017).
Hedges, L. V. & Olkin, I. Statistical Methods for Meta-analysis (Academic Press, 2014).
Institute of Applied Manpower Research. Manpower Profile India 4th edn. (Manak Publications Yearbook, 1996).
Shaikh, B. M., Doke, P. P. & Gothankar, J. S. Depression, anxiety, stress, and stressors among rural adolescents studying in Pune and a rural block of Nanded district of Maharashtra, India. Indian J. Public Health 62(4), 311–314. https://doi.org/10.4103/ijph.IJPH_174_17 (2018).
Shukla, M., Ahmad, S., Singh, J. V., Shukla, N. K. & Shukla, R. Factors associated with depression among school-going adolescent girls in a district of northern India: A cross-sectional study. Indian J. Psychol. Med. 41(1), 46–53. https://doi.org/10.4103/IJPSYM.IJPSYM_211_18 (2019).
Dwivedi, M., Paria, B. & Roy, S. K. Study on adolescent health and associated factors: Comparison between rural and urban areas of West Bengal. Int. J. Med. Sci. Public Health 9(6), 348–352. https://doi.org/10.5455/ijmsph.2020.12342201916062020 (2020).
Balgir, R. S. (2004). Dimensions of rural tribal health, nutritional status of Kondh tribe and tribal welfare in Orissa: A biotechnological approach. in Proceedings of the UGC Sponsored National Conference on Human Health and Nutrition: A Biotechnological Approach (Lead Lecture), 47–57.
Meng, H., Li, J., Loerbroks, A., Wu, J. & Chen, H. Rural/urban background, depression and suicidal ideation in Chinese college students: A cross-sectional study. PLoS ONE 8(8), e71313. https://doi.org/10.1371/journal.pone.0071313 (2013).
Letvak, S. The importance of social support for rural mental health. Issues Ment. Health Nurs. 23(3), 249–261. https://doi.org/10.1080/016128402753542992 (2002).
Venkaiah, K., Damayanti, K., Nayak, M. U. & Vijayaraghavan, K. Diet and nutritional status of rural adolescents in India. Eur. J. Clin. Nutr. 56(11), 1119–1125. https://doi.org/10.1038/sj.ejcn.1601457 (2002).
Patel, V. et al. Gender disadvantage and reproductive health risk factors for common mental disorders in women: A community survey in India. Arch. General Psychiatry. 63(4), 404–413. https://doi.org/10.1001/archpsyc.63.4.404 (2006).
World Health Organization. (2000). Women's Mental Health: An Evidence-based Review.
Prabha, V. S., Rao, V. B. & Kanakabushanam, G. V. V. S. A comparative study of anxiety and depression among adolescents from rural and urban areas. J. Med. Sci. Res. 5(1), 29–32. https://doi.org/10.17727/JMSR.2017/5-6 (2017).
Roest, J. Child marriage and early child-bearing in India: Risk factors and policy implications. Young Lives Policy Paper 10, 12–34 (2016).
Ramanaik, S. et al. Education, poverty and" purity" in the context of adolescent girls’ secondary school retention and dropout: A qualitative study from Karnataka, southern India. PLoS ONE 13(9), e0202470. https://doi.org/10.1371/journal.pone.0202470 (2018).
Unicef, U. N. (2014). Progress and prospects. End Child Marriage Prog. Prospect UNICEF [Internet]. 1–8.
Raj, A., Saggurti, N., Balaiah, D. & Silverman, J. G. Prevalence of child marriage and its effect on fertility and fertility-control outcomes of young women in India: A cross-sectional, observational study. Lancet 373(9678), 1883–1889. https://doi.org/10.1016/S0140-6736(09)60246-4 (2009).
Raj, A., Saggurti, N., Lawrence, D., Balaiah, D. & Silverman, J. G. Association between adolescent marriage and marital violence among young adult women in India. Int. J. Gynecol. Obstet. 110(1), 35–39. https://doi.org/10.1016/j.ijgo.2010.01.022 (2010).
Warrington, M. & Kiragu, S. “It makes more sense to educate a boy”: Girls ‘against the odds’ in Kajiado, Kenya. Int. J. Educ. Dev. 32(2), 301–309. https://doi.org/10.1016/j.ijedudev.2011.05.004 (2012).
Marques, S. C., Pais-Ribeiro, J. L. & Lopez, S. J. Use of the “Mental Health Inventory–5” with Portuguese 10–15 years old. Spanish J. Psychol. 14(1), 478–485. https://doi.org/10.5209/rev_SJOP.2011.v14.n1.43 (2011).
Gururaj, G., Varghese, M., Benegal, V., Rao, G.N., Pathak, K., Singh, L.K., et al. National Mental Health Survey of India, 2015–16: Prevalence, patterns and outcomes. Bengaluru: National Institute of Mental Health and Neuro Sciences, NIMHANS; 2016. Publication No.:129. Retrieved on 25th November, 2021 from http://indianmhs.nimhans.ac.in/Docs/Report2.pdf
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372, n71. https://doi.org/10.1136/bmj.n71 (2021).
Munn, Z., Moola, S., Lisy, K., Riitano, D. & Tufanaru, C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int. J. Evid. Based Healthc. 13, 147–153. https://doi.org/10.1097/xeb.0000000000000054 (2015).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21(11), 1539–1558. https://doi.org/10.1002/sim.1186 (2002).
Borenstein, M., Hedges, L. V., Higgins, J. P. & Rothstein, H. R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synthesis Methods 1(2), 97–111. https://doi.org/10.1002/jrsm.12 (2010).
Dhoundiyal, M. & Venkatesh, R. The psychological world of adolescence: A comparative evaluation between rural and urban girls. Indian J. Psychol. Med. 31(1), 35–38. https://doi.org/10.4103/0253-7176.53313 (2009).
Samanta, A., Mukherjee, S., Ghosh, S. & Dasgupta, A. Mental health, protective factors and violence among male adolescents: A comparison between urban and rural school students in West Bengal. Indian J. Public Health 56(2), 155 (2012).
Kumar, S., Dixit, V., Chaudhury, S. & Kenswar, D. K. Racial differences in suicidal ideation among school going adolescents. Ind. Psychiatry J. 22(2), 118. https://doi.org/10.4103/0972-6748.132924 (2013).
Manuel, D., John, M. & Rekha, N. S. A study on the prevalence of anxiety related disorders among adolescents in rural Kerala. J. Evid. Based Med. Healthc. 3(58), 3077–3079. https://doi.org/10.18410/jebmh/2016/670 (2016).
Yadav, S. K. & Sengar, K. S. Prevalence of psychosocial problems in tribal school going adolescents. Indian J. Clin. Psychol. 149(2), 118–123 (2017).
Rai, S. K. et al. Mental health, bullying, and violent injuries among adolescents—A cross-sectional study. Int. J. Med. Sci. Public Health 8(11), 928–931. https://doi.org/10.5455/ijmsph.2019.0822620082019 (2019).
Chopra, R. & Sangwan, S. Differences in depression level among rural and urban adolescents of Haryana. India. Int. J. Curr. Microbiol. Appl. Sci. 9(9), 3391–3398. https://doi.org/10.20546/ijcmas.2020.909.421 (2020).
Rajamani, S. Prevalence of social phobia and depression among adolescent girls in selected schools in rural areas of Panipat. Haryana. Int. J. Adv. Nursing Manag. https://doi.org/10.52711/2454-2652.2021.00067 (2021).
Nair, M. K. C. et al. ADad 3: The epidemiology of Anxiety Disorders among adolescents in a rural community population in India. Indian J. Pediatr. 80(Suppl 2), S144-148. https://doi.org/10.1007/s12098-013-1097-5 (2013).
Russell, P. S. S. et al. ADad 9: Suicidal behavior in Anxiety Disorders among adolescents in a rural community population in India. Indian J. Pediatr. 80(Suppl 2), S175-180. https://doi.org/10.1007/s12098-013-1122-8 (2013).
Russell, P. S. S. et al. ADad 7: Relationship between depression and Anxiety Disorders among adolescents in a rural community population in India. Indian J. Pediatr. 80(Suppl 2), S165-170. https://doi.org/10.1007/s12098-013-1232-3 (2013).
Waghachavare, V., Quraishi, S., Dhumale, G. & Gore, A. A cross-sectional study of correlation of body image anxiety with social phobia and their association with depression in the adolescents from a rural area of Sangli District in India. Int. J. Preventive Med. 5(12), 1626–1629 (2015).
Vashisht, A. et al. Prevalence of depression & assessment of risk factors among school going adolescents. Indian J. Community Health. 26(2), 196–199 (2014).
Kharod, N. & Kumar, D. Mental health status of school going adolescents in rural area of Gujarat. Indian J. Youth Adolesc. Health 2, 17–21 (2015).
Ali, A. & Eqbal, S. Mental health status of tribal school going adolescents: A study from rural community of Ranchi, Jharkhand. Telangana J. Psychiatry. https://doi.org/10.18231/j.tjp.2019.036 (2016).
Chakraborty, T. et al. Prevalence of depression amongst adolescents in rural area of South India—A school based cross sectional study. Public Health Rev. Int. J. Public Health Res. 30, 3 (2016).
Bahl, R. & Kumari Sandeepa, R. Mental health profile of urban and rural adolescents in Jammu District of J&K. JK Sci. 18(4), 221–224 (2016).
Archana, S., Prasad, K. N. & Jabeen, B. Prevalence of social anxiety disorder and its determinants in school going adolescents in rural population of Ramnagara district. Int. J. Med. Sci. Public Health 6(8), 1308–1313. https://doi.org/10.5455/ijmsph.2017.0513413062017 (2017).
Yuvaraj, K. et al. Prevalence and associated factors for social phobia among school-going adolescents in a rural area of Puducherry, South India. Int. J. Adolesc. Med. Health. https://doi.org/10.1515/ijamh-2018-0037 (2018).
Madasu, S. et al. Anxiety disorders among adolescents in a rural area of northern India using Screen for Child Anxiety-Related Emotional Disorders tool: A Community-based Study. Indian J. Community Med. 44(4), 317. https://doi.org/10.4103/ijcm.IJCM_359_18 (2019).
Edlina, K., Arif, A., Nilesh, G. M. & Sonia, D. P. Prevalence of emotional, behavioural problems and ego resilience among tea tribe adolescents living in Dibrugarh district of Assam. Clin. Epidemiol. Glob. Health 8(1), 190–193. https://doi.org/10.1016/j.cegh.2019.06.012 (2020).
Hanspal, I. et al. How prevalent is depression among rural school-going adolescents: A cross-sectional study in South Karnataka. J. Indian Assoc. Child Adolesc. Mental Health. 15(2), 124–139 (2019).
Rose-Clarke, K. et al. Adolescent girls’ health, nutrition and wellbeing in rural eastern India: A descriptive, cross-sectional community-based study. BMC Public Health 19(1), 1–11. https://doi.org/10.1186/s12889-019-7053-1 (2019).
Mohta, A. et al. Depression among adolescents in a rural community of north India: A cross-sectional study. J. Family Med. Primary Care 9(11), 5671. https://doi.org/10.4103/jfmpc.jfmpc_1152_20 (2020).
Priyanga, S. (2020). A Study to Screen for Various Types of Anxiety Disorders in Higher Secondary School Students in Rural Areas using Scared Scale (Doctoral dissertation, Government Mohan Kumaramangalam Medical College, Salem). Retrieved on 9th November, 2021 from http://repository-tnmgrmu.ac.in/id/eprint/13591
International Institute of Population Sciences. National Family Health Survey 2, 1998–1999. Retrieved on 2nd January, 2022 from www.nfhsindia.org/india2.html
Ministry of Health and Family Welfare. 2002. National Health Policy.
Polanczyk, G., De Lima, M. S., Horta, B. L., Biederman, J. & Rohde, L. A. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. Am. J. Psychiatry. 164(6), 942–948. https://doi.org/10.1176/ajp.2007.164.6.942 (2007).
Ganesan, R., Radhakrishnan, S. & Rajamanickam, R. Prevalence and predictors of suicidal behaviour among adolescents in India: A systematic review and meta-analyses. J. Crit. Rev. 7(19), 8754–8770. https://doi.org/10.31838/jcr.07.19.981 (2020).
Cao, X. L. et al. Prevalence of suicidal ideation and suicide attempts in the general population of China: A meta-analysis. Int. J. Psychiatry Med. 49(4), 296–308. https://doi.org/10.1177/0091217415589306 (2015).
Kessler, R. C. et al. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Arch. General Psychiatry. 69(4), 372–380. https://doi.org/10.1001/archgenpsychiatry.2011.160 (2012).
Joseph, J. K. & Devu, B. K. Prevalence of attention-deficit hyperactivity disorder in India: A systematic review and meta-analysis. Indian J. Psychiatric Nursing. 16(2), 118. https://doi.org/10.4103/IOPN.IOPN_31_19 (2019).
Funding
The authors have received no funding for this research.
Author information
Authors and Affiliations
Contributions
E.R.—Idea, supervised the work progress, proofread the manuscript, and contributed substantially to the discussion. N.V.S.K. and G.J.J.—Method, data selection and extraction, quality appraisal, analysis, writing, drafting and revising of the review paper and contributed substantially to the discussion. P.K.R.—Helped with data extraction, validated the work done by N.V.S.K. & G.J.J. in study selection and quality appraisal and contributed substantially to the discussion. M.M.—Helped with data extraction, validated the work done by N.V.S.K. & G.J.J. in study selection and quality appraisal and contributed substantially to the discussion. R.R.D.—Helped with data extraction, validated the work done by N.V.S.K. & G.J.J. in study selection and quality appraisal and contributed substantially to the discussion. D.R.—Helped with data extraction, validated the work done by N.V.S.K. & G.J.J. in study selection and quality appraisal and contributed substantially to the discussion. G.C.—Helped with data extraction, validated the work done by N.V.S.K & G.J.J. in study selection and quality appraisal and contributed substantially to the discussion. J.R.—Helped with data extraction, validated the work done by N.V.S.K. & G.J.J. in study selection and quality appraisal and contributed substantially to the discussion. J.G.A.—Reviewed and edited the manuscript, contributed substantially to discussion J.A.—Reviewed and edited the manuscript and contributed substantially to the discussion. A.M.J.—Reviewed and edited the manuscript and contributed substantially to the discussion.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rajkumar, E., Julia, G., Sri Lakshmi K., N.V. et al. Prevalence of mental health problems among rural adolescents in India: A systematic review and meta-analysis. Sci Rep 12, 16573 (2022). https://doi.org/10.1038/s41598-022-19731-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-19731-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.