Abstract
Organic anion transporting polypeptides (OATP), which are encoded by SLCO genes, participate in the hepatic elimination of drugs and xenobiotics. SLCO1B1 is an important pharmacogenomic gene (encoding OATP1B1) associated with response to the uptake of endogenous compounds, such as statin and bilirubin. Ethnicity of the patient modulates the response to these drugs; the frequency and haplotype data for SLCO1B1 genetic variants in the Arab population is lacking. Therefore, we determined the frequencies of two well-characterized SLCO1B1 single nucleotide polymorphisms (SNP) and haplotypes that affect the OATP1B1 drugs transportation activity in Qatari population. Genotyping data for two SLCO1B1 SNPs (c.388A > G, c.521 T > C) were extracted from whole exome data of 1050 Qatari individuals, who were divided into three ancestry groups, namely Bedouins, Persians/South Asians, and Africans. By way of using Fisher's exact and Chi-square tests, we evaluated the differences in minor allele frequency (MAF) of the two functional SNPs and haplotype frequencies (HF) among the three ancestry groups. The OATP1B1 phenotypes were assigned according to their function by following the guidelines from the Clinical Pharmacogenetics Implementation Consortium for SLCO1B1 and Simvastatin-Induced Myopathy.The MAF of SLCO1B1:c.388A > G was higher compared to that of SLCO1B1:c.521 T > C in the study cohort. It was significantly high in the African ancestry group compared with the other two groups, whereas SLCO1B1:c.521 T > C was significantly low in the African ancestry group compared with the other two groups. The SLCO1B1 *15 haplotype had the highest HF, followed by *1b, *1a, and *5. Only the SLCO1B1 *5 haplotype showed no significant difference in frequency across the three ancestry groups. Furthermore, we observed that the OATP1B1 normal function phenotype accounted for 58% of the Qatari individuals, the intermediate function phenotype accounted for 35% with significant differences across the ancestry groups, and the low function phenotype accounted for 6% of the total Qatari individuals with a higher trend observed in the Bedouin group.The results indicate that the phenotype frequencies of the OATP1B1 intermediate and low function in the Qatari population appear at the higher end of the frequency range seen worldwide. Thus, a pharmacogenetic screening program for SLCO1B1 variants may be necessary for the Qatari population.
Similar content being viewed by others
Introduction
Transmembrane protein transporters are involved in the flow of ions, small molecules, and macromolecules across the cell membrane. There are two main groups of proteins known to be involved in the transportation process, namely (a) the solute-linked carrier (SLC) superfamily (influx transporters), and (b) the ATP-binding cassette (ABC) superfamily (efflux transporters)1. The organic anion transporting polypeptide (OATP) transporters, which are expressed on the sinusoidal membrane of human hepatocytes, belong to the SLC superfamily and play an important role in the hepatic elimination of drugs and xenobiotics2. There are 11 members in the human OATP family that are encoded by the SLCO genes. The OATP1B1, that is encoded by SLCO1B1, is the most fully characterized human OATP and is highly polymorphic3.
Single nucleotide polymorphisms (SNP) of the SLCO1B1 gene can alter OATP1B1 activity in vitro and in vivo, and can affect the pharmacokinetics and pharmacodynamics of various drugs4,5,6,7,8. OATP1B1 mediates the uptake of many endogenous substrates and xenobiotics including bilirubin, bile acids, bile salt, thyroid hormones, steroid conjugates of cyclic peptides, antibiotics (such as rifampicin and benzylpenicillin), methotrexate rheumatic arthritis, and natural toxins (such as microcystin and phalloidin)9,10. In addition, OATP1B1 is important for mediating the hepatic clearance of drugs such as 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors (e.g. statins: pravastatin and simvastatin), angiotensin-converting enzyme inhibitors (enalapril), antibiotics (rifampicin), chemotherapeutic agents, endothelin receptor antagonist (bosentan, prostacyclin, and beraprost) anti-inflammatory drug (diclofenac), and antiviral agent (simeprevir)11,12,13,14,15.
The two well-characterized functional SLCO1B1 variants are SLCO1B1*1b (c.388A > G rs2306283) and SLCO1B1*5 (c.521 T > C rs4149056). While the c.388A > G variant is associated with increased OATP1B1 activity, the c.521 T > C variant is associated with reduced transport activity6,16. Decreased hepatic drug clearance is seen in carriers of SLCO1B1*5 variant17. An increase in the transport of pravastatin and ezetimibe has been reported in carriers of SLCO1B1*1b variant in different populations18,19,20. In contrast, reduced uptake of statins, fexofenadine, irinotecan, and repaglinide into hepatocytes is associated with the SLCO1B1*5 polymorphism21,22,23,24,25,26. The SLCO1B1*5 variant is associated with higher plasma concentrations of lopinavir, which is an antiretroviral protease inhibitor used to treat HIV infections27,28.
Many global studies have examined alterations in OATP1B1 transporter activity associated with SNPs from SLCO1B1 in different populations including European29, European American, African American8, Asian3, and North African18; however, there is none or limited data from Arab populations. Arab populations are characterized by a high rate of consanguineous marriages and by a high prevalence of metabolic disorders. In particular, there is a high prevalence of dyslipidaemia, which is a contributing factor to the increase in the cardiovascular disease (CVD)-associated mortality rate in Middle East30. Given that dyslipidaemia is managed by anionic drug that transported OATP1B1, lack of studies from Middle East on pharmacogenomics of OATP1B1 is a concern. Thus, the focus of the current study is to characterize the two well-known SNPs of SLCO1B1 and determine their frequencies in the Qatari population. In addition, pharmacogenetic studies show that there are implications from racial and ancestry variations within the same population on defining genetic profiles for personalised medicine31. Therefore, the current study also examined the three genetic substructures within the Qatari population, namely Bedouin/Arab, Persian/South Asian, and African ancestry groups32.
Results
Minor allele frequencies (MAF) of the two exonic SNPs from the SLCO1B1 gene in the study cohort
We calculated minor allele frequency (MAF) and Hardy–Weinberg equilibrium for the study variants. The study variants passed the tests for Hardy–Weinberg equilibrium (HWE). The MAF for the two exonic SNPs of the SLCO1B1 gene and the HF of SLCO1B1 *1a, *1b, *5, and *15 for the 1050 Qatari individuals across the three ancestry groups are presented in Table 1. The MAF of the SLCO1B1:c.388A > G was significantly higher than that of SLCO1B1:c.521 T > C (p < 0.001) in the full cohort of 1050 Qatari individuals and in each of the three ancestry groups. The MAF of SLCO1B1:c.388A > G was significantly higher (p < 0.001) in the African ancestry group compared with the other two groups, which exhibited similar frequency values. The MAF of SLCO1B1:c.521 T > C was significantly lower (p = 0.007) in the African ancestry group compared with the other two groups, which had similar frequency values.
Haplotype frequencies (HF) of the exonic SNPs from the SLCO1B1 gene
Table 1 shows that the SLCO1B1 *15 haplotype exhibited the highest frequency followed by *1b, *1a, and *5. Only the SLCO1B1 *5 haplotype showed no significant difference in frequencies across the three ancestry groups (p = 0.1195). The frequency of the SLCO1B1 *1a was significantly lower in the African group and that of *1b was significantly higher in the African group. The frequency of the SLCO1B1 *15 haplotype was significantly higher in the Bedouin/Arab group when compared with those in the other two groups. The frequency of the *5 haplotype was as such as small in the whole of the cohort.
Frequency of the OATP1B1 phenotypes
The frequency of the normal function phenotype of the OATP1B1 transporter was highest among the whole cohort (at 58%) while that of the low function was lowest (at 6%). Among the three ancestral groups, the African group exhibited higher frequency for the normal function phenotype while the Bedouin group exhibited higher frequency for the intermediate function phenotype.
Minor allele frequencies (MAF) of the two exonic SLCO1B1 SNPs in global populations
Results of our survey of literature and genotype databases for allele frequencies at the two SLCO1B1 SNPs across different global populations are presented in Table 2. The frequencies exhibit considerable variation among the populations.
Discussion
OATP1B1 (encoded by SLCO1B1) is a well-characterized human OATP and it is highly polymorphic3,8. The genetic variations of the SLCO1B1 gene have been documented for various populations3,8,18,29; however, there is a lack of data regarding these variations in the Arabian countries, including the Gulf Cooperation Council countries. Therefore, we evaluated the genetic variations in the SLCO1B1 among the Qatari population which is comprised of three ethnic groups, namely Bedouins/Arabs, Persians/South Asians, and Africans32. In total, 1050 individuals were examined in this study in which 587 (55.9%) were of Bedouin/Arab ancestry, 387 (36.8%) were of Persian/South Asian ancestry, and 76 (7.2%) were of African ancestry.
Considering that the SLCO1B1 *1b, *5, and *15 are the most-often implicated variants in altering the function and/or intracellular disposition of OATP1B1 substrates14, we focused on these variants in the Qatari population. Previous studies have demonstrated that carriers of the *1b allele exhibit increased transport activity of pravastatin and decreased plasma concentrations of ezetimibe19,20, whereas carriers of the *5 variant show reduced uptake of statins, including pravastatin26,33 and rifampicin34, in hepatocytes, as well as show increased area under the AUC curve for fexofenadine, repaglinide, and irinotecan21,23,24,25. Furthermore, SLCO1B1*5 is strongly associated with myopathy among simvastatin users1,35,36,37,38,39,40,41,42,43,44,45.
The *15 haplotype was shown to be associated with increased plasma concentrations of pitavastatin in Korean subjects46 and had an effect on the systemic exposure and elimination of atorvastatin47,48,49. Moreover, *15 carriers showed a reduction in transport activity and this haplotype was associated with myopathy in patients administered with pravastatin and atorvastatin136,38,45,50.
By way of considering data from literature51,52,53 as well as data extracted from the 1000 Genomes project and gnomAD databases, we compared the minor allele frequencies of the variants from Qatari population with those from global populations. The allele frequency of the c.388A > G variant in the Qatari populations had no similarities with that from other documented populations including Thai, Koreans, Han Chinese, Japanese, African Americans, and European Americans (see Table 2). However, the European, Israeli, Pakistani, Caucasian, Finnish, Turkish, Macedonian, Albanian, and Greek populations exhibited a very similar allele frequency. Data obtained from the gnomAD database also showed a close similarity in allele frequencies from the combined-European, American, Ashkenazi Jewish, Finnish, non-Finish European, and South Asian populations. Moreover, the MAF of c.388A > G in these populations was also similar to that from the Persian/South Asian and Bedouin/Arab ethnic groups from Qatar.
The non-synonymous c.521 T > C SNP, which is associated with reduced OATP1B1 activity, was found in the Qatari population with an allele frequency dissimilar to that of Macedonian, Albanian, Thai, Caucasian, Dutch, Finnish, Algerian, Israeli, Sub-Saharan African, Japanese, Korean, Chinese, African American, European American, Han Chinese, and Turkish populations. However, the frequency from the African ethnic group was similar to that from the European American, Japanese, Chinese, Korean, Thai, and Finnish populations (see Table 2).
Thus, it appears that the minor allele frequencies of both the variants from the Qatari population were dissimilar to those from many Asian countries, particularly the East Asian Countries.
With regard to haplotype frequencies, our data points out that the haplotype frequency for the *5 haplotype in Qataris (HF = 3.81%) is similar to that in the Middle Eastern population (HF = 5%), but higher than that seen in other populations including Thai, Asians, South/central Asians and Indians, Oceania, South/Central Americans, Africans (HF = 0%), and Caucasians (HF = 1%)51. With respect to the Qatari ethnic groups, the frequency of the *5 haplotype in Bedouin/Arab ethnic group (HF = 3.58%) and Persian ethnic group (HF = 4.65%) was also similar to that seen in the Middle Eastern population, whereas that seen in the Persian population was much higher compared with that from the South/Central Asians and Indians (SW Asians) (HF = 0%)51. In addition, the frequency seen in the African ethnic group of Qatar (HF = 1.32%) was higher when compared to that from the natives of Africa51. Regarding the frequency of the *15 haplotype, our results indicated that there are no similarities with global populations, except for the African ethnic group (HF = 21.05%) with the South/Central Americans (HF = 24%)51.
When comparing the frequency of the *1b haplotype from the Qatari population (HF = 34.24%) with those from global populations, similarities were observed with the Middle Eastern (HF = 31%) and South/Central American (HF = 39%) populations. The haplotype frequency of *1b was comparable between the African ethnic group from Qatar (HF = 64.47%) and the Thai (HF = 65%) and Oceania (HF = 66%) populations51.
Thus, it appears that the SLCO1B1 HFs from Qatar are similar to those seen in Middle Eastern population and that the results from Qatar are extendable to the whole of Middle Eastern countries. In summary, the SLCO1B1 HFs in Qataris are unique from global populations.
As regards SLCO1B1 diplotypes, the phenotype frequency (PF) of the OATP1B1 transporter accounts for 58.19% with normal function and 35.33% for intermediate function (see Table 3), These phenotype frequencies of the Qatari population are within the global PF range (55–88% and 11–36%, respectively). Compared with other populations (including the Thai, Koreans, Chinese, and Vietnamese) both the intermediate and normal function-encoding diplotypes were higher in Qatar51,52. However, the phenotype frequency of the SLCO1B1 diplotypes encoding low function OATP1B1 was higher in Qatar than the global range (0–6%), whereas the PF values for all of the ethnic groups of normal and intermediate function were within the global range. Hence, it can be concluded that the phenotypic frequency of the intermediate and the low OATP1B1 function phenotypes in the Qatari population appear at either the top end of the global range or even higher. This warrants a large-level pharmacogenetic screening of the Qatari population for SLCO1B1 variants to guide clinical decisions regarding the above-mentioned drugs and xenobiotics (see the “Introduction” section).
Further, it is reiterated that the OATP1B1 transporter intermediate function has a significant variability across the three Qatari ethnic groups—this observation is important to consider in personalized medicine approach where the genomic sequence of every patient determines the best therapy and dosage regimen suited to the patient. The same conclusion has been drawn in a previous study that investigated South African ethnic populations including Zulu and Cape admixture groups31.
The current study is limited to only two functional SNPs from SLCO1B1 that are used to clinically classify/predict OTAB1 phenotype profile. However, it is to be noted that this is the first study of pharmacogenomic aspects of SLCO1B1 variations in Arab populations and it is important to restrict the study to only the variants that are globally well-characterized for clinical outcome following the use of drugs. Nevertheless, we hope that our work will pave the way to follow-up works by other researchers on patients to study the impact of SNPs on key transporter proteins, which may hinder drug efficacy in vitro, in vivo, and clinical setting.
Conclusion
Based on the observations from our study, we predict that the Qatari population, along with the different ethnic groups of the Bedouin/Arab ancestry, Persian/South Asian ancestry, and African ancestry, is at an increased risk of haplotype-mediated inter-individual variations in drug disposition and, therefore, is prone to elevated toxicity levels compared with other populations. However, since there is no previously published data on association of these variants in the Middle Eastern population, particularly the Qatari population, in a clinical setting, we highly recommend that a pharmacogenetic screen should be conducted on a large scale for this population in a clinical setting.
Materials and methods
Ethics statement
This study was approved by the Institutional Ethical Review Committee at the Dasman Diabetes Institute, Kuwait, in accordance with the Declaration of Helsinki. Genomic information on the study subjects is publicly available from the National Center for Biotechnology Information Sequence Read Archive (NCBI-SRA). Informed consent from the recruited participants had been obtained as part of the original studies32,54 using protocols approved by the institutional review boards of the Hamad Medical Corporation and Weill Cornell Medical College in Qatar.
Study samples
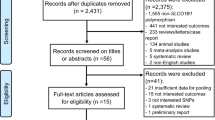
Next-generation sequence data of whole exomes and genomes from individuals living in Qatar32,54 are publicly available at the NCBI-SRA server (accession numbers SRP060765, SRP061943, and SRP061463). These exomes and genomes were sequenced on the Illumina platform with library kits of differing coverage of the human consensus-coding sequence regions. Further, some of these individuals were not natives of Qatar and some of them were of ad-mixed ethnicities. To address these concerns, we short-listed only those native individuals who adhered to one of the three ancestry-components of Qatar, namely Bedouins, Persian/South Asians and Africans32,54. Further, we ignored those individuals who were sequenced on low-coverage library kits, such as Agilent version V4 (Agilent Technologies Inc., USA). This led to the short-listed sample set of 958 exomes and 92 genomes.
Thus, the study sample set included a total of 1050 individuals, of which 449 individuals were males (43%) and 601 were females (57%).
Variant calling for the SLCO1B1 gene
Illumina raw paired-end reads from the whole genome and exome sequencing were mapped to the human genome reference assembly, GRCh37, by the Burrows–Wheeler Aligner version v07-1755. The mapped data were converted to BAM files in which duplicate reads were removed using SAMtools56 and Picard software tool version 2.20.21 (http://picard.sourceforge.net). The Genome Analysis Toolkit (GATK) version v3.8-1-057 was used for local realignment of the reads around insertion–deletion mutations, for recalibration of base quality, and for variant calling for the SLCO1B1 variants (rs2306283; c.388A > G and rs4149056; c.521 T > C).
OATP1B1 transport phenotypes assignment with SLCO1B1 genotypes
The assignment of the OATP1B1 phenotypes into three groups of normal, intermediate, and low function was done by following the guidelines of the Clinical Pharmacogenetics Implementation Consortium for SLCO1B1 and Simvastatin-Induced Myopathy: 2014 update and the star (*) allele nomenclature58.
Statistical analysis
The frequency of the two functional SNPs within the SCLO1B1 (c.388A > G, c.521 T > C) gene was assessed for deviation from the Hardy–Weinberg equilibrium (HWE) using R software (version 3.6.2) (https://www.R-project.org/). Differences in minor alleles frequencies and haplotype frequencies across the three Qatari ancestry groups were characterized using Fisher's exact and Chi-square tests using IBM SPSS Statistics Version 25 software. A p-value of < 0.05 was considered statistically significant.
Data availability
The next-generation sequencing data used in this study are available from the NCBI-SRA with accession numbers SRP060765, SRP061943, and SRP061463.
References
Gong, I. Y. & Kim, R. B. Impact of genetic variation in OATP transporters to drug disposition and response. Drug Metab. Pharmacokinet. 28, 4–18 (2013).
Hagenbuch, B. & Meier, P. J. Organic anion transporting polypeptides of the OATP/SLC21 family: Phylogenetic classification as OATP/SLCO superfamily, new nomenclature and molecular/functional properties. Pflug. Arch-Eur. J. Physiol. 447, 653–665 (2004).
Jada, S. R. et al. Pharmacogenetics of SLCO1B1: Haplotypes, htSNPs and hepatic expression in three distinct Asian populations. Eur. J. Clin. Pharmacol. 63, 555–563 (2007).
Nies, A. T. et al. Genetics is a major determinant of expression of the human hepatic uptake transporter OATP1B1, but not of OATP1B3 and OATP2B1. Genome Med 5, 1–13 (2013).
Chigutsa, E. et al. The SLCO1B1 rs4149032 polymorphism is highly prevalent in South Africans and is associated with reduced rifampin concentrations: Dosing implications. Antimicrob. Agents Chemother. 55, 4122–4127 (2011).
Kameyama, Y., Yamashita, K., Kobayashi, K., Hosokawa, M. & Chiba, K. Functional characterization of SLCO1B1 (OATP-C) variants, SLCO1B1*5, SLCO1B1*15 and SLCO1B1*15+C1007G, by using transient expression systems of HeLa and HEK293 cells. Pharmacogenet. Genomics 15, 513–522 (2005).
Niemi, M. et al. High plasma pravastatin concentrations are associated with single nucleotide polymorphisms and haplotypes of organic anion transporting polypeptide-C (OATP-C, SLCO1B1). Pharmacogenetics 14, 429–440 (2004).
Tirona, R. G., Leake, B. F., Merino, G. & Kim, R. B. Polymorphisms in OATP-C—Identification of multiple allelic variants associated with altered transport activity among European- and African-Americans. J. Biol. Chem. 276, 35669–35675 (2001).
Gribble, M. O. et al. SLCO1B1 variants and urine arsenic metabolites in the strong heart family study. Toxicol. Sci. 136, 19–25 (2013).
Hagenbuch, B. & Meier, P. J. The superfamily of organic anion transporting polypeptides. BBA-Biomembranes 1609, 1–18 (2003).
Oshida, K., Shimamura, M., Seya, K., Ando, A. & Miyamoto, Y. Identification of transporters involved in beraprost sodium transport in vitro. Eur. J. Drug Metab. Pharmacokinet. 42, 117–128 (2017).
Ouwerkerk-Mahadevan, S., Snoeys, J., Peeters, M., Beumont-Mauviel, M. & Simion, A. Drug-drug interactions with the NS3/4A protease inhibitor simeprevir. Clin. Pharmacokinet. 55, 197–208 (2016).
Zhang, Y. et al. Diclofenac and its acyl glucuronide: Determination of in vivo exposure in human subjects and characterization as human drug transporter substrates in vitro. Drug Metab. Dispos. 44, 320–328 (2016).
Nakanishi, T. & Tamai, I. Genetic polymorphisms of OATP transporters and their impact on intestinal absorption and hepatic disposition of drugs. Drug Metab. Pharmacokinet. 27, 106–121 (2012).
Treiber, A., Schneiter, R., Haeusler, S. & Stieger, B. Bosentan is a substrate of human OATP1B1 and OATP1B3: Inhibition of hepatic uptake as the common mechanism of its interactions with cyclosporin A, rifampicin and sildenafil. Drug Metab. Dispos. 35, 1400–1407 (2007).
Mwinyi, J., Johne, A., Bauer, S., Roots, I. & Gerloff, T. Evidence for inverse effects of OATP-C (SLC21A6) *5 and *1b haplotypes on pravastatin kinetics. Clin. Pharmacol. Ther. 75, 415–421 (2004).
Pasanen, M. K., Neuvonen, M., Neuvonen, P. J. & Niemi, M. SLCO1B1 polymorphism markedly affects the pharmacokinetics of simvastatin acid. Pharmacogenet. Genomics 16, 873–879 (2006).
Mwinyi, J., Koepke, K., Schaefer, M., Roots, I. & Gerloff, T. Comparison of SLCO1B1 sequence variability among German, Turkish and African populations. Eur. J. Clin. Pharmacol. 64, 257–266 (2008).
Oswald, S. et al. Disposition of ezetimibe is influenced by polymorphisms of the hepatic uptake carrier OATP1B1. Pharmacogenet. Genomics 18, 559–568 (2008).
Maeda, K. et al. Effects of organic anion transporting polypeptide IBI haplotype on pharmacokinetics of pravastatin, valsartan and temocapril. Clin. Pharmacol. Ther. 79, 427–439 (2006).
Han, J.-Y., Lim, H.-S., Lee, S. Y., Kim, H. T. & Lee, J. S. Influence of the organic anion transporting polypeptide 1B1 (OATP1B1) polymorphisms on irinotecan-pharmacokinetics and clinical outcome of patients with advanced non-small cell lung cancer. J. Thorac. Oncol. 2, S485–S485 (2007).
Kalliokoski, A., Neuvonen, M., Neuvornen, P. J. & Niemi, M. Different effects of SLCO1B1 polymorphism on the pharmacokinetics and pharmacodynamics of repaglinide and nateglinide. J. Clin. Pharmacol. 48, 311–321 (2008).
Niemi, M., Pasanen, M. K. & Neuvonen, P. J. SLCO1B1 polymorphism and sex affect the pharmacokinetics of pravastatin but not fluvastatin. Clin. Pharmacol. Ther. 80, 356–366 (2006).
Niemi, M. et al. Polymorphic organic anion transporting polypeptide 1B1 is a major determinant of repaglinide pharmacokinetics. Clin. Pharmacol. Ther. 77, 468–478 (2005).
Niemi, M. et al. Fexofenadine pharmacokinetics are associated with a polymorphism of the SLCO1B1 gene (encoding OATP1B1). Br. J. Clin. Pharmacol. 59, 602–604 (2005).
Nishizato, Y. et al. Polymorphisms of OATP-C (SLC21A6) and OAT3 (SLC22A8) genes: Consequences for pravastatin pharmacokinetics. Clin. Pharmacol. Ther. 73, 554–565 (2003).
Hartkoorn, R. C. et al. HIV protease inhibitors are substrates for OATP1A2, OATP1B1 and OATP1B3 and lopinavir plasma concentrations are influenced by SLCO1B1 polymorphisms. Pharmacogenet. Genomics 20, 112–120 (2010).
Kohlrausch, F. B., de Estrela, R. C., Barroso, P. F. & Suarez-Kurtz, G. The impact of SLCO1B1 polymorphisms on the plasma concentration of lopinavir and ritonavir in HIV-infected men. Br. J. Clin. Pharmacol. 69, 95–98 (2010).
Pasanen, M. K., Backman, J. T., Neuvonen, P. J. & Niemi, M. Frequencies of single nucleotide polymorphisms and haplotypes of organic anion transporting polypeptide 1B1 SLCO1B1 gene in a Finnish population. Eur. J. Clin. Pharmacol. 62, 409–415 (2006).
Al Rasadi, K. et al. Dyslipidaemia in the Middle East: Current status and a call for action. Atherosclerosis 252, 182–187 (2016).
Hoosain, N., Pearce, B., Jacobs, C. & Benjeddou, M. Mapping SLCO1B1 genetic variation for global precision medicine in understudied regions in Africa: A focus on Zulu and Cape admixed populations. Omics J. Integr. Biol. 20, 546–554 (2016).
Fakhro, K. A. et al. The Qatar genome: A population-specific tool for precision medicine in the Middle East. Human genome variation 3, 16016–16016 (2016).
Zhang, W. et al. SLCO1B1 521T >C functional genetic polymorphism and lipid-lowering efficacy of multiple-dose pravastatin in Chinese coronary heart disease patients. Br. J. Clin. Pharmacol. 64, 346–352 (2007).
He, Y.-J. et al. Rifampicin alters atorvastatin plasma concentration on the basis of SLCO1B1 521T>C polymorphism. Clin. Chim. Acta 405, 49–52 (2009).
Link, E. et al. SLCO1B1 variants and statin-induced myopathy—A genomewide study. N. Engl. J. Med. 359, 789–799 (2008).
Ghatak, A., Faheem, O. & Thompson, P. D. The genetics of statin-induced myopathy. Atherosclerosis 210, 337–343 (2010).
Mammen, A. L. & Amato, A. A. Statin myopathy: A review of recent progress. Curr. Opin. Rheumatol. 22, 644–650 (2010).
Sirtori, C. R., Mombelli, G., Triolo, M. & Laaksonen, R. Clinical response to statins: Mechanism(s) of variable activity and adverse effects. Ann. Med. 44, 419–432 (2012).
Hu, M., Mak, V. W. L. & Tomlinson, B. Intronic variants in SLCO1B1 related to statin-induced myopathy are associated with the low-density lipoprotein cholesterol response to statins in Chinese patients with hyperlipidaemia. Pharmacogenet. Genomics 22, 803–806 (2012).
Rallidis, L. S., Fountoulaki, K. & Anastasiou-Nana, M. Managing the underestimated risk of statin-associated myopathy. Int. J. Cardiol. 159, 169–176 (2012).
Sathasivam, S. Statin induced myotoxicity. Eur. J. Intern. Med. 23, 317–324 (2012).
Bhardwaj, S., Selvarajah, S. & Schneider, E. B. Muscular effects of statins in the elderly female: A review. Clin. Interv. Aging 8, 47–59 (2013).
Dandona, S. Cardiovascular drugs and the genetic response. Methodist Debakey Cardiovasc. J. 10, 13–17 (2014).
Albayda, J. & Christopher-Stine, L. Identifying statin-associated autoimmune necrotizing myopathy. Clevel. Clin. J. Med. 81, 736–741 (2014).
Maeda, K. Organic anion transporting polypeptide (OATP)1B1 and OATP1B3 as important regulators of the pharmacokinetics of substrate drugs. Biol. Pharm. Bull. 38, 155–168 (2015).
Chung, J. Y. et al. Effect of OATPIBI (SLCOIBI) variant alleles on the pharmacokinetics of pitavastatin in healthy volunteers. Clin. Pharmacol. Ther. 78, 342–350 (2005).
Lee, Y. J., Lee, M. G., Lim, L. A., Jang, S. B. & Chung, J. Y. Effects of SLCO1B1 and ABCB1 genotypes on the pharmacokinetics of atorvastatin and 2-hydroxyatorvastatin in healthy Korean subjects. Int. J. Clin. Pharmacol. Ther. 48, 36–45 (2010).
Rodrigues, A. C. et al. Pharmacogenetics of OATP transporters reveals that SLCO1B1 c.388A > G variant is determinant of increased atorvastatin response. Int. J. Mol. Sci. 12, 5815–5827 (2011).
Pasanen, M. K., Fredrikson, H., Neuvonen, P. J. & Niemi, M. Different effects of SLCO1B1 polymorphism on the pharmacokinetics of atorvastatin and rosuvastatin. Clin. Pharmacol. Ther. 82, 726–733 (2007).
Shitara, Y. et al. Clinical significance of organic anion transporting polypeptides (OATPs) in drug disposition: Their roles in hepatic clearance and intestinal absorption. Biopharm. Drug Dispos. 34, 45–78 (2013).
Nakorn, C. N. et al. Genetic variations and frequencies of the two functional single nucleotide polymorphisms of SLCO1B1 in the Thai population. Front. Pharmacol. 11, 728 (2020).
Kim, E.-Y. et al. Duplex pyrosequencing assay of the 388A > G and 521T > C SLCO1B1 polymorphisms in three Asian populations. Clin. Chim. Acta 388, 68–72 (2008).
Namgoong, S. et al. Comparison of genetic variations of the SLCO1B1, SLCO1B3 and SLCO2B1 genes among five ethnic groups. Environ. Toxicol. Pharmacol. 40, 692–697 (2015).
Rodriguez-Flores, J. L. et al. Indigenous Arabs are descendants of the earliest split from ancient Eurasian populations. Genome Res. 26, 151–162 (2016).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25, 1754–1760 (2009).
Li, H. et al. The Sequence alignment/Map format and SAMtools. Bioinformatics 25, 2078–2079 (2009).
McKenna, A. et al. The genome analysis toolkit: A mapreduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303 (2010).
Ramsey, L. B. et al. The clinical pharmacogenetics implementation consortium guideline for SLCO1B1 and Simvastatin-induced myopathy: 2014 Update. Clin. Pharmacol. Ther. 96, 423–428 (2014).
Xu, L. Y. et al. Organic anion transporting polypeptide-1B1 haplotypes in Chinese patients. Acta Pharmacol. Sin. 28(10), 1693–1697 (2007).
Pasanen, M. K., Neuvonen, P. J. & Niemi, M. Global analysis of genetic variation in SLCOIB1. Pharmacogenomics 9, 19–33 (2008).
Lee, E. et al. Rosuvastatin pharmacokinetics and pharmacogenetics in white and Asian subjects residing in the same environment. Clin. Pharmacol Ther. 78(4), 330–341 (2005).
Yang, G. P. et al. Lack of effect of genetic polymorphisms of SLCO1B1 on the lipid-lowering response to pitavastatin in Chinese patients. Acta Pharmacol. Sin. 31(3), 382–386 (2010).
Grapci, D. A. et al. Frequencies of single-nucleotide polymorphisms and haplotypes of the SLCO1B1 gene in selected populations of the Western Balkans. Balk. J. Med. Gene. 18, 5–21 (2015).
Giannakopoulou, E. et al. No impact of SLCO1B1 521T > C, 388A > G and 411G > A polymorphisms on response to statin therapy in the Greek population. Mol. Biol. Rep. 41, 4631–4638 (2014).
Brunham, L. R. et al. Differential effect of the rs4149056 variant in SLCO1B1 on myopathy associated with simvastatin and atorvastatin. Pharmacogenomics J. 12, 233–237 (2012).
Acknowledgements
The authors acknowledge the institutional funding by the Kuwait Foundation for Advancement of the Sciences (KFAS). The authors thank Dr Juan Rodriguez-Flores for sharing the data on ancestry classification of the participants from the study cohort.
Author information
Authors and Affiliations
Contributions
M.D., F.A-M., and T.A.T. designed and performed the study and wrote the manuscript. M.D. and A.A-M. performed the data analyses. A.C. participated in data analysis. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dashti, M., Al-Matrouk, A., Channanath, A. et al. Frequency of functional exonic single-nucleotide polymorphisms and haplotype distribution in the SLCO1B1 gene across genetic ancestry groups in the Qatari population. Sci Rep 12, 14858 (2022). https://doi.org/10.1038/s41598-022-19318-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-19318-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.