Abstract
Physical exercise is known to be beneficial for breast cancer survivors (BCS). However, avoiding nonfunctional overreaching is crucial in this population, as they are in physiological dysregulation. These factors could decrease their exercise capacity or facilitate nonfunctional overreaching, which can increase their risk of additional morbidities and even all-cause mortality. The focus of this study is to evaluate the reliability and validity of the ATOPE+ mHealth system to estimate autonomic balance and specific wellness parameters associated with BCS’ perceived load, thereby informing nonlinear prescriptions in individualized physical exercise programs for BCS.Twenty-two BCS were included in the reliability and validity analysis. Measures were taken for four days, including morning autonomic balance by heart rate variability, self-reported perception of recovery from exercise, sleep satisfaction, emotional distress and fatigue after exertion. Measures were taken utilizing the ATOPE+ mHealth system application. The results of these measures were compared with criterion instruments to assess validity.The reliability results indicated that the intraclass correlation coefficient (ICC) showed an excellent correlation for recovery (0.93; 95% CI 0.85–0.96) and distress (0.94, 95% CI 0.89–0.97) as well as good correlation for the natural logarithm of the mean square root differences of the standard deviation (LnRMSSD) (0.87; 95% CI 0.74–0.94). Sleep satisfaction also showed an excellent correlation with a weighted kappa of 0.83. The validity results showed no significant differences, except for fatigue. ATOPE+ is reliable and valid for remotely assessing autonomic balance, perception of recovery, sleep satisfaction and emotional distress in BCS; however, it is not for fatigue. This highlights that ATOPE+ could be an easy and efficient system used to assess readiness in BCS, and could help to improve their health by supporting the prescription of optimal and safe physical exercise. Trial registration NCT03787966 ClinicalTrials.gov, December 2019 [ATOPE project]. https://clinicaltrials.gov/ct2/show/NCT03787966.
Similar content being viewed by others
Introduction
Background
Physical exercise is already known to mitigate the side effects of cancer and its treatment1, as well as reduce cancer recurrence2,3, and mortality2 in breast cancer survivors (BCS). In general, physical exercise should aim to achieve the desired benefits while balancing the risks of suboptimal loading or overtraining. Avoiding nonfunctional overreaching or insufficient recovery would be important for BCS, as they are in a situation of physiological vulnerability due to cancer and its treatment. Their physiological systems have undergone changes due to treatment, such as increased oxidative stress4, chronic inflammation5, and reduced immune function6; which are similar to the alterations present in overtraining in athletes7. While these alterations are related to treatment side effects, they may also predispose these women to physiological dysregulation which maintained over time, would decrease their physical exercise assimilation capacity or even lead them to overreaching8, and increasing their vulnerability to illness and death9.
In oncology, the conventional prescription is linear, with a progressive and standard increase in intensity, frequency and duration parameters10. However, a nonlinear approach maximises the adaptation to exercise, which has been suggested to fit best to an optimal and safe dose-recovery period10, thus, could be safest for a heterogeneous population such as BCS. Additionally, the presence of nonresponders11, a wide range of adherence12, and patients with comorbidities and higher toxicities13 should be considered in physical exercise programs, which may challenge current physical exercise prescription approaches.
For this matter, nonlinear prescription is usually guided with methods such as heart rate variability (HRV), which allows a better dose adjustment and prevents overtraining14. Nevertheless, this has been commonly used in athletes, but its use is not as common in the clinical population (ClinicalTrials.gov Identifier: NCT03745742), and specifically in the oncological population, where prescription is mostly informed by survivors’ symptoms15. Therefore, it is of great interest to develop a support tool such as ATOPE+16 to assist with a nonlinear prescription, monitor readiness, and control the loading-recovery cycle to allow safe and effective doses following physiological adaptations.
ATOPE+ mHealth system
When working with a vulnerable population such as BCS, it is important to rely on validated tools. For instance, a previous example would be the BENECA application in BCS17, which was successful in terms of reliability17 and efficacy18. BENECA records energy expenditure based on exercise and food ingested and recommends increasing or decreasing physical activity to maintain energy balance. However, ATOPE+ adds further information in prescribing physical exercise by including physiological readiness information in optimizing exercise dose. ATOPE+ is based on assessing autonomic balance with HRV, as it reflects fatigue, stress and other factors that influence exercise assimilation7. However, it has been stated that other internal load parameters are part of novel risks or preclinical alterations preceding overtraining, such as poor sleep, worsened mood, stress, and increased fatigue7. These are especially important in patients with cancer and could mediate HRV on their own; therefore, they are also included in ATOPE+.
The gold standard for autonomic balance is the assessment of HRV with an electrocardiogram (ECG). However, for recovery and fatigue, there is a wide range of blood parameters, such as blood lactate concentration19 and creatine kinase (CK)20; for sleep analysis, it is the use of polysomnography; for stress, cortisol analysis21. However, these are not easily accessible and expensive, and some of them are invasive and time-consuming tests. For these reasons, we selected other instruments validated in previous studies as comparisons to validate ATOPE+, including a Holter monitor22, Perceived Recovery Status Scale23, Sleep Diary24, Emotional Distress Thermometer25, and Borg CR-10 Scale26. ATOPE+ HRV information, complemented with other self-reported parameters, can remotely engage oncological populations. Therefore, ATOPE+ is HRV-guided as well as complemented with other internal load parameters to remotely monitor the oncological population.
Aim
The aim of this study was to evaluate the reliability and validity of the ATOPE+ application to estimate autonomic balance by HRV and wellness parameters to inform nonlinear individualized physical exercise prescription for posttreatment BCS.
Methods
A cross-sectional observational study was conducted to test the reliability and validity of ATOPE+ with 22 BCS.
Participants
Potential participants were identified from the referrals received from the Surgical Unit of the Hospital Universitario Clínico San Cecilio in Granada, Spain, between February and August 2021. BCS were eligible if they had been diagnosed with breast cancer (stages I-III), had to have basic mobile phone capabilities, and had at least one year since the end of oncological treatment (hormonal treatment was not an exclusion criterion). In contrast, potential participants were excluded if they had not finished chemotherapy or radiotherapy at least one year before the study start date, had psychiatric or cognitive disorders that prevented from following the instructions of the protocol given, or did not have access to a smartphone.
Eligible women were asked to come to the CUIDATE group’s facilities. A member of the research group explained the assessment protocol and installed ATOPE+ on their mobile phones. They were asked to use ATOPE+ in the presence of a researcher to ensure correct assessment performance. They were also given the materials needed for remote assessment (i.e., ECG device, chest strap, questionnaires and assessments instructions).
Sample size
A sample size of 20 participants was estimated to be necessary to identify an intraclass correlation coefficient (ICC) of 0.8 between the mean square root differences of the standard deviation (LnRMSSD) assessed with the Polar H10 chest band and the ECG (Gold Standard), 90% power, and an alpha error of 0.527. Considering a potential 10% dropout rate, 22 BCS were recruited for the study.
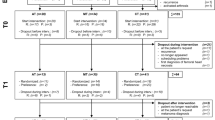
Description of ATOPE+ and data collection
To complete the study, patients had to take measurements with ATOPE+ and their comparison instruments (Table 1): Holter monitor22, Perceived Recovery Status Scale23, Sleep Diary24, Emotional Distress Thermometer25, and Borg CR-10 Scale26, during four consecutive mornings, including one weekend day in order to be as precise to normal routine as possible. Patients were told to follow a normal sleep routine during the study. Once they finished the application protocol, they continued filling out the comparison questionnaires given in paper format and the sleep diary. An overview of the ATOPE+ mHealth system is shown in Fig. 1.
ATOPE+ was developed by the Biomedical (BIO-277) ‘CUIDATE’ research group and the Department of Computer Architecture and Technology, CITIC-UGR Research Centre, both from the University of Granada, Spain. The development of ATOPE+ is part of the ATOPE project28, registration number NCT03787966 ClinicalTrials.gov, December 2019.
The ATOPE+ mHealth system is composed of a cross-platform application (Android/iOS) and a centralized secure server. The application provides patients with an interface to record their HRV and to report their wellness through questionnaires. The centralized secure server enables data storage and processing, as well as the generation of tailored exercise prescription according to expert rules. The architecture and usability of ATOPE+ have previously been described16. The registration code of the system is 1710092555522.
Once the research team has installed the application on the participant’s phones and created their personal profiles, patients were ready to start using the application. In the main view, patients were able to read a quick tutorial of how to perform the assessment or start it. The measurement started once they pushed the “Start” button, so they had to be prepared before pushing the button. The assessment of the HRV was first. A notification with sound and vibration alerted the participant that this first step was completed, and the rest of the protocol continued.
Perceived recovery, sleep satisfaction and fatigue were assessed with horizontal continuous Likert scales from 0 to 10 with labels in the values at the extremes and a continuous slider included in ATOPE+. For emotional distress, the scale was positioned vertically. The final part of the assessment consisted of performing 10 repetitions of the "Sit To Stand Test" (STS) and assessing the fatigue perceived after the effort with a rating of perceived exertion scale from 0 to 10. After that, the evaluation was completed. The answers were sent to the server, and the participant received an automatic personalized message about their readiness for either a high-intensity session, a moderate-intensity session, or active recovery. More information about the intervention was published on a previous protocol28.
Comparison instruments
Autonomic balance
Autonomic balance was assessed with ATOPE+ and a Polar H10 chest strap (Polar H10, Polar Electro Oy, Kempele, Finland) connected through Bluetooth and was compared with an ECG (Norav Holter DL800, Braemar Inc, Eagan, EEUU) monitor, which is considered the gold standard. From a 7-min recording, the first and last minutes were cut off to achieve clear and precise interpretations of vagal tone with a 5-min signal, as recommended by the Task Force of the European Society of Cardiology and the North American Society for Pacing and Electrophysiology29. The time domain parameter rMSSD (the square root of the mean squared differences) was analysed.
For ATOPE+ , data were exported to a computer for analysis. As recommended by the Taskforce, all artifacts (ectopic beats, arrhythmic events, and noise effects) in the RR time series were corrected or removed to reduce the chances of substantial deformities that can occur in HRV analysis30. In the case of Holter monitor data, NH300 software (Norav, version 3.0, 2009, Norav Medical Ltd) was used to perform the spectral analysis by using Fast Fourier transform algorithms to remove noise from recordings. The sampling rate was 128 samples/second. The frequency filter was set from 0.05 to 60 Hz. Due to low sampling rate, the software itself applied an interpolation algorithm to improve R peak detection31.
After waking up and emptying their bladder, participants were instructed to moisten and place the chest band and the ECG monitor. Then, lying on their beds facing the ceiling, data recording was performed under the same terms of duration for both devices.
Perception of recovery
The Perception of Recovery Scale was used as a comparison to assess the perception of recovery. It is a subjective self-administered Likert-type scale with scores from 1 to 10 (Table 1) and with a sensitivity and specificity of 0.82 and 0.81, respectively23.
Sleep satisfaction
As a comparison instrument, the subsection of quality of sleep from the consensus sleep diary, a reliable tool for prospectively measuring quality of sleep24, was used. It is a self-reported method that includes quantitative and qualitative aspects related to each night of rest (Table 1). This method, compared to polysomnography, has a kappa coefficient of 0.8732.
Emotional distress
The Emotional Distress thermometer according to “The NCCN Clinical Practice Guidelines in Oncology” was used as a comparison to measure emotional distress. This tool consists of a Likert-type scale with values from 0 to 10, where 0 is "no emotional distress" and 10 constitutes "extreme emotional distress" (Table 1). In the Spanish oncology population, this thermometer has a sensitivity of 0.9 and a specificity of 0.6433.
Peripheral fatigue
The Borg-CR 10 scale was used as comparison for the evaluation of the perceived level of fatigue after physical exertion. After performing 10 repetitions at a rhythm of 40 beats per minute (marked by a metronome included in ATOPE+) of the STS, a test frequently used as a protocol to induce fatigue in the lower extremities, participants completed this questionnaire, which consists of scores from 0 to 10 ("Not at all" to "Very, very hard", respectively) (Table 1). This scale has a reliability of 0.66 according to the kappa coefficient in the clinical population of women26.
Statistical analysis
A descriptive analysis was performed to summarize sociodemographic and clinical characteristics of participants. Continuous variables are expressed as the mean ± standard deviation, and categorical variables are expressed as numbers and percentages. The normal distribution of the variables was checked by means of the Shapiro-Wilks test. Data that did not follow a normal distribution were transformed into Ln(x) or Ln(x + 1) to enable parametric analysis. All analyses were carried out by a blinded researcher.
IBM SPSS version 24 was used for all analyses (IBM Statistical Program for Social Sciences SPSS Statistic, Corp., Armonk, New York). Bland–Altman analyses were carried out in order to properly establish agreement34 between ATOPE+ methods and Gold Standard methods by using Excel worksheets (Microsoft Excel version 16.55, Microsoft, Washington, EEUU). A 95% Confidence Interval (CI) was established, and significance was set at p < 0.05.
Reliability
For each outcome measure, concordance between comparison instruments and those included in ATOPE+ was calculated. Bearing in mind that Pearson correlation coefficients, paired t test, and Bland–Altman plots are methods for analysing agreement but not ideal in terms of reliability35, interdevice ICC were calculated to reflect relative reliability (Table 2). ICC scores were categorized as poor (< 0.5), moderate (0.5–0.75), good (0.75–0.90) and excellent (> 0.90)36. Weighted kappa was used for categorical variables. The suggested interpretation for agreement is as follows: ≤ 0 poor, 0.01–0.20 slight, 0.21–0.40 fair, 0.41–0.60 moderate, 0.61–0.80 substantial, and 0.81–1 almost perfect37. Additionally, the standard error of measurement was calculated. These calculations identified within subject variation for each method, indicating the magnitude to which repeated measures changed for participants.
Validity
To determine the validity of ATOPE+, paired samples t tests were conducted comparing ATOPE+ measurements versus reliable measurements. Continuous variables were analyzed by Student's t-test in the case of normal parametric variables, and nonparametric variables were analyzed with Wilcoxon test. Considering that they only reflect proportional relationships and can cause erroneous interpretation of measurements, to establish the agreement between the comparison instruments and ATOPE+ methods, Bland–Altman analyses were also carried out, which allowed us to see the difference between two clinical measurement devices against each method’s mean. To obtain further information, sleep satisfaction was treated as a continuous variable for this purpose. To establish interdevice agreement, Cohen's d for effect size was used, with effect sizes categorised as follows: 0 to 0.19, trivial; 0.2 to 0.59, small; 0.6 to 1.19, moderate; 1.2 to 1.99, large; and > 2.0, very large38. The Wilcoxon rank test and effect size were calculated for ordinal variables.
Ethics approval and consent to participate
This study was approved by the ‘Ethics Committee of Biomedical Research of Granada’ (Granada, Spain) (0507-N-18, July 27, 2018). All participants received written and verbal information. Informed consent was obtained from all participants by signing a specific document for this purpose. All methods were carried out in accordance with the Declaration of Helsinki.
Results
Sample description
A total of 22 BCS who had finished oncological treatment at least one year ago were recruited for the study. Of these participants, 1 could not be included in the sample because she was not able to complete the four days of measurement due to personal issues. The mean age of the participants was 49.48 (SD 8.38) years. Tables 3 and 4 summarize demographic and clinical characteristics of the participants. Of the participants, 6 (27.27%) were unemployed. Most participants had stage II breast cancer (36.36%) and had undergone surgery, chemotherapy, and radiotherapy as treatment (63.64%).
Reliability
Interclass correlation
The ICC for each comparison instrument and ATOPE+ methods showed evidence of good reliability, with all values higher than 0.86 (Table 2). Sleep satisfaction showed a strong correlation (weighted kappa = 0.87).
Validity
Validity analysis outcomes are shown in Table 5. The paired sample T-test revealed significant differences for fatigue (p < 0.001). The strongest parameter agreement for ATOPE+ compared to comparison instruments was the mean Emotional Distress, with a Pearson correlation of 0.91. In contrast, the weakest parameter agreement with a Pearson correlation of 0.80 was found in LnRMSSD (Table 5).
Bland–Altman plots were also generated (Fig. 2a–e), as a graphical representation to depict the difference and limits of agreement between ATOPE+ mean measurement methods and comparison instruments mean measurement methods. Bland-Altman bias, with 95% limits of agreement (LOA), 95% CIs and effect sizes are shown in Table 5. The effect size was small for all variables except for fatigue, which was large.
Discussion
Our findings showed that ATOPE+ is reliable and valid for assessing autonomic balance, perception of recovery, sleep satisfaction and emotional distress in BCS, with the exception of detecting fatigue. These results highlight that ATOPE+ could be an easy and efficient system to measure tailored readiness in BCS and a tool to improve health by helping professionals to prescribe optimal and safe exercise doses. Moreover, ATOPE+ may provide reliable data-driven analysis with machine learning algorithms, as originally described in its architecture16.
Comparison with prior work
The majority of previous work is not oriented to the clinical population but to athletes39 to avoid overtraining14 and increase performance40. In the clinical population, to our knowledge, a similar tool has not been developed, although there is an ongoing one on post myocardial infarction (ClinicalTrials.gov Identifier: NCT03745742), with less demanding purpose but more oriented to improve functional capacities and reduce fatigue. To our knowledge, there is not an application that has yet been specialized in the oncological population, particularly in women with breast cancer, that has HRV as the principal assessment but complemented with other internal load parameters.
Regarding the validity observed in HRV parameters, the results from ATOPE+ were similar to those in the literature39,41. On the one hand, these positive results in ATOPE+ regarding HRV were expected, as the Polar H10 chest band already has had excellent results in the literature measuring this specific outcome42. In the study by Gilgen-Ammann et al.42, they found that it has excellent validity compared to an ECG monitor and recommended it as gold standard, especially during exercise, as it surpassed the ECG in terms of inducing less recording noise. In addition, good results in our study could have been due to the patients being instructed that it was of great importance to empty their bladder, to remain still during the measurement, to breathe normally, and to have a comfortable environment without distractions. Nevertheless, the correlation was expected to be higher. These results could be obtained because the software that automatically analyses ECG data could not be using the same interpolation methods or selection of outliers or ectopic beats. On the other hand, for the Bland–Altman analysis, previous studies39,41 obtained a higher percentage of values of HRV outside the limits of agreement. ATOPE+ reduced percentage of values outside the levels of agreement for HRV, which could have been the result of the application having a timer that told participants where to stop both devices at the same time, as longer samples had been identified to modify HRV indices29.
Considering the rest of the parameters, we found significant differences between the fatigue measured with ATOPE+ and the Borg CR-10 Scale, but not for the rest of the internal load parameters. Therefore, it may not be useful for detecting fatigue. Patients were instructed to immediately complete the questionnaires on paper, however, the time in between could explain the differences because as time passes, the perceived fatigue decreases43. Another possible hypothesis is that the ATOPE+ fatigue scale may be completed with more verbal anchors, facilitating patients’ answers, or it could be due to differences in the formats used. Therefore, we still wanted to address that even if criteria validity was not met, analysis was performed until the end and found excellent correlation results. In the future, we could add more anchor words or turn the scale horizontal to try to investigate this difference. However, as recovery could be seen as inversely proportional to fatigue, it could be still recognised that having the recovery data may be sufficient from a clinical point of view.
Limitations and strengths
The system is aimed at BCS and not patients with other types of cancer. Patients had to have basic mobile phone capabilities. In addition, ATOPE+ may be restricted to the available technology and, even if not particularly expensive, could not be accessible for everyone (Polar H10 chest band). The system is only supported in smartphones, not in tablets or computers, and some sight problems in elderly patients could demand family support. In addition, Spanish is the only available language of the system. Additionally, a limitation is that we did not include biomarkers that could support the results, as we wanted a fully noninvasive assessment. In the future, we could establish new tools for different cancer types, have English as an available language, and include photoplethysmography for greater accessibility to the population. To improve individualized physical exercise prescription and to find concordance between subjetctive methods (such as perceived rating of exertion or perceived fatigue, repetitions in reserve) and objective methods (such as heart rate) to control physical exercise intensity, we think it may be interesting the inclusion of invasive biomarkers such as exerkines (specifically, lactate), CK, or maximal oxygen comsumption (VO2max) as an optional complement to ATOPE+ .
ATOPE+ also presents some strengths. The system could be a very powerful tool for professionals, as it may guarantee safe exercise doses. Additionally, it saves time, as readiness or recovery could be assessed remotely. In addition, it is a step toward health monitoring and requires patients to be part of it, which may help them learn to regulate recovery. Additionally, it is a friendly, easy-to-install and easy-to-use application compatible with both Android and IOS systems, so it can reach a population with fewer mobile phone capabilities.
Clinical implications
ATOPE+ can be an excellent support tool for exercise programs in BCS, optimising physical exercise and improving adherence and safety. Additionally, it offers professionals a single, easy, remote and validated tool that assesses several parameters related to different systems and could identify risk profiles and target interventions to a particular problem. Lastly, it can be used together with other complementary tools, as it is not time-consuming and does not require patients to wear any device.
Conclusion
ATOPE+ is a reliable and valid tool to monitor readiness in BCS, which could help rehabilitation professionals prescribe safer and optimal doses of exercise. This ensures that BCS have an adequate recovery period to induce compensation to meet the principles of training. As a new technology, it offers a more easy, efficient and inexpensive way of doing so. ATOPE+ is a realiable and valid tool to assess autonomic balance, sleep satisfaction, emotional distress in BCS. Therefore, it could be an excellent tool to support physical exercise programs in cancer survivor populations.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ATOPE+:
-
ATOPE+ mHealth system
- BCS:
-
Breast Cancer Survivors
- CK:
-
Creatine Kinase
- ECG:
-
Electrocardiogram
- HRV:
-
Heart Rate Variability
- ICC:
-
Intraclass correlation coefficient
- Ln:
-
Natural logarithm
- LnRMSSD:
-
Natural logarithm of the mean square root differences of the standard derivation
- RMSSD:
-
Mean square root differences of the standard derivation
- VO2max:
-
Maximal oxygen consumption
References
Patel, A. V. et al. American college of sports medicine roundtable report on physical activity, sedentary behavior, and cancer prevention and control. Med. Sci. Sport. Exerc. 51, 2391–2402 (2019).
Morishita, S. et al. Effect of exercise on mortality and recurrence in patients with cancer: A systematic review and meta-analysis. Integr. Cancer Ther. 19, 153473542091746 (2020).
Biganzoli, E., Desmedt, C. & Demicheli, R. Does physical activity have an impact on recurrence dynamics in early breast cancer patients?. J. Clin. Med. 10, 831 (2021).
Conklin, K. A. Chemotherapy-associated oxidative stress: Impact on chemotherapeutic effectiveness. Integr. Cancer Ther. 3, 294–300 (2004).
Bower, J. E. Cancer-related fatigue—Mechanisms, risk factors, and treatments. Nat. Rev. Clin. Oncol. 11, 597–609 (2014).
Zitvogel, L., Apetoh, L., Ghiringhelli, F. & Kroemer, G. Immunological aspects of cancer chemotherapy. Nat. Rev. Immunol. 8, 59–73 (2008).
Cadegiani, F. A. & Kater, C. E. Novel insights of overtraining syndrome discovered from the EROS study. BMJ Open Sport Exerc. Med. 5, e000542 (2019).
Angeli, A., Minetto, M., Dovio, A. & Paccotti, P. The overtraining syndrome in athletes: A stress-related disorder. J. Endocrinol. Investig. 27, 603–612 (2004).
Kraft, T. S. et al. Multi-system physiological dysregulation and ageing in a subsistence population. Philos. Trans. R. Soc. B Biol. Sci. 375, 2019 (2020).
Sasso, J. P. et al. A framework for prescription in exercise-oncology research. J. Cachexia Sarcopenia Muscle 6, 115–124 (2015).
Pickering, C. & Kiely, J. Do non-responders to exercise exist—And if so, what should we do about them?. Sport. Med. 49, 1–7 (2019).
Spence, R. R., Sandler, C. X., Newton, R. U., Galvão, D. A. & Hayes, S. C. Physical activity and exercise guidelines for people with cancer: Why are they needed, who should use them, and when?. Semin. Oncol. Nurs. 36, 151075 (2020).
Bruce, J. et al. Exercise versus usual care after non-reconstructive breast cancer surgery (UK PROSPER): Multicentre randomised controlled trial and economic evaluation. BMJ 375, e066542 (2021).
Singh, N. et al. Heart rate variability: An old metric with new meaning in the era of using mhealth technologies for health and exercise training guidance. Part two: Prognosis and training. Arrhythm. Electrophysiol. Rev. 7, 1 (2018).
Kirkham, A. A. et al. ‘Chemotherapy-periodized’ exercise to accommodate for cyclical variation in fatigue. Med. Sci. Sport. Exerc. 52, 278–286 (2020).
Moreno-Gutierrez, S. et al. ATOPE+: An mHealth system to support personalized therapeutic exercise interventions in patients with cancer. IEEE Access 9, 16878–16898 (2021).
Lozano-Lozano, M. et al. Monitoring energy balance in breast cancer survivors using a mobile app: Reliability study. JMIR mHealth uHealth 6, 1–10 (2018).
Lozano-Lozano, M. et al. Mobile health and supervised rehabilitation versus mobile health alone in breast cancer survivors: Randomized controlled trial. Ann. Phys. Rehabil. Med. 63, 316–324 (2020).
Billat, V. L., Sirvent, P., Py, G., Koralsztein, J.-P. & Mercier, J. The concept of maximal lactate steady state. Sports Med. 33, 407–426 (2003).
Hecksteden, A. et al. Blood-borne markers of fatigue in competitive athletes—Results from simulated training camps. PLoS ONE 11, e0148810 (2016).
Levine, A., Zagoory-Sharon, O., Feldman, R., Lewis, J. G. & Weller, A. Measuring cortisol in human psychobiological studies. Physiol. Behav. 90, 43–53 (2007).
Shaffer, F., Ginsberg, J. P. & Shaffer, F. An overview of heart rate variability metrics and norms. Front. Public Health 5, 1–17 (2017).
Laurent, C. M. et al. A practical approach to monitoring recovery: Development of a perceived recovery status scale. J. Strength Cond. Res. 25, 620–628 (2011).
Carney, C. E. et al. The consensus sleep diary: Standardizing prospective sleep self-monitoring. Sleep 35, 287–302 (2012).
Cutillo, A. et al. The distress thermometer: Cutoff points and clinical use. Oncol. Nurs. Forum 44, 329–336 (2017).
Soriano-Maldonado, A. et al. Validity and reliability of rating perceived exertion in women with fibromyalgia: Exertion-pain discrimination. J. Sports Sci. 33, 1515–1522 (2015).
de Vet, H. C. W., Terwee, C. B., Mokkink, L. B. & Knol, D. L. Measurement in Medicine (Cambridge University Press, 2011).
Postigo-Martin, P. et al. Attenuating treatment-related cardiotoxicity in women recently diagnosed with breast cancer via a tailored therapeutic exercise program: Protocol of the ATOPE trial. Phys. Ther. 101, pzab014 (2021).
Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Task force of the european society of cardiology and the North American society of pacing and electrophysiology. Circulation 93, 1043–1065 (1996).
Umair, M., Chalabianloo, N., Sas, C. & Ersoy, C. HRV and stress: A mixed-methods approach for comparison of wearable heart rate sensors for biofeedback. IEEE Access 9, 14005–14024 (2021).
Caro-Morán, E. et al. Heart rate variability in breast cancer survivors after the first year of treatments: A case-controlled study. Biol. Res. Nurs. 18, 43–49 (2016).
Rogers, A. E., Caruso, C. C. & Aldrich, M. S. Reliability of sleep diaries for assessment of sleep/wake patterns. Nurs. Res. 42, 368–372 (1993).
Martínez, P., Galdón, M. J., Andreu, Y. & Ibáñez, E. The distress thermometer in Spanish cancer patients: Convergent validity and diagnostic accuracy. Support. Care Cancer 21, 3095–3102 (2013).
Hughes, D. C. et al. Using rating of perceived exertion in assessing cardiorespiratory fitness in endometrial cancer survivors. Physiother. Theory Pract. 33, 0–765 (2017).
Koo, T. K. & Li, M. Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 15, 155–163 (2016).
Portney, L. G. Foundations of Clinical Research : Applications to Practice. (Davis, F A, 2020).
Landis, J. R. & Koch, G. G. The measurement of observer agreement for categorical data. Biometrics 33, 159–174 (1977).
Hopkins, W. G., Marshall, S. W., Batterham, A. M. & Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 41, 3–12 (2009).
Perrotta, A. S., Jeklin, A. T., Hives, B. A., Meanwell, L. E. & Warburton, D. E. R. Validity of the elite HRV smartphone application for examining heart rate variability in a field-based setting. J. Strength Cond. Res. 31, 2296–2302 (2017).
Manresa-Rocamora, A., Sarabia, J. M., Javaloyes, A., Flatt, A. A. & Moya-Ramón, M. Heart rate variability-guided training for enhancing cardiac-vagal modulation, aerobic fitness, and endurance performance: A methodological systematic review with meta-analysis. Int. J. Environ. Res. Public Health 18, 10299 (2021).
Boos, C. J. et al. A comparison of two methods of heart rate variability assessment at high altitude. Clin. Physiol. Funct. Imaging 37, 582–587 (2017).
Gilgen-Ammann, R., Schweizer, T. & Wyss, T. RR interval signal quality of a heart rate monitor and an ECG Holter at rest and during exercise. Eur. J. Appl. Physiol. 119, 1525–1532 (2019).
Tibana, R. A. et al. Validity of session rating perceived exertion method for quantifying internal training load during high-intensity functional training. Sports 6, 2–9 (2018).
Acknowledgements
This work is part of PPM’s doctoral work at the Clinical Medicine and Public Health Doctoral Studies of the University of Granada, Spain. The authors express their gratitude to the participants for their participation in the evaluation of ATOPE+.
Funding
This study was funded by the Spanish Ministry of Economy and Competitiveness (Plan Estatal de I + D + I 2013–2016), the Fondo de Investigación Sanitaria del Instituto de Salud Carlos III (PI18/01840), the Fondos Estructurales de la Unión Europea (FEDER), the European Social fund the Carlos III Health Institute (FI19/00230) and the Spanish Ministry of Education Cultura y Deporte (FPU17/00939, FPU16/04201, FPU18/0357). Additional funding is provided by the European Regional Development Fund (ERDF, SOMM17/6107/UGR).
Author information
Authors and Affiliations
Contributions
P.P.M., I.C.V., M.A.M., and S.M.G. conceptualized the study and wrote the manuscript. A.G.S., M.L.G., and R.G.G. performed statistical analyses and wrote the manuscript. P.P.M., M.L.G., and A.G.S. recruited and measured patients with cancer and healthy matched controls. P.P.M. and S.M.G. created the database. All the authors analysed and interpreted the data and revised and edited the manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Postigo-Martin, P., Gil-Gutiérrez, R., Moreno-Gutiérrez, S. et al. mHealth system (ATOPE+) to support exercise prescription in breast cancer survivors: a reliability and validity, cross-sectional observational study (ATOPE study). Sci Rep 12, 15217 (2022). https://doi.org/10.1038/s41598-022-18706-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-18706-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.